Introduction
The Australian College of Rural and Remote Medicine (ACRRM)1 is accredited by the Australian Medical Council for setting professional standards for training, assessment, certification and professional development in the specialty of general practice, especially in rural and remote medicine.
The recruitment and retention of doctors in rural areas has been linked to their professional support2,3. ACRRM supports rural doctors through training in clinical assessment, rural practice, professional and legal topics using theory, scenario-based learning and facilitated group discussions4.
Context
Whether doctors, particularly those in rural areas, were sufficiently prepared by medical education courses to deliver remote care using telehealth services during the COVID-19 pandemic has been questioned in recent studies of medical students’ educational experiences5,6. Other studies have reviewed the provision of education in the use of video consultations in rural settings7 and the need for general practitioners to follow well-defined procedures when undertaking remote consultations8.
Training of doctors in remote consultations
One of the reasons postulated for the slow growth in video consultations9 is that doctors may not have the knowledge and skills to perform a remote consultation to a standard that they and the patient would be comfortable with10. The need for training was confirmed by an online survey of ACRRM members in early 2021. Members were concerned about how to conduct consultations, screening patients to ensure that a video consultation is appropriate, indirect physical examinations, patient-assisted physical examinations and the safety of telephone consultations. In response to this need, ACRRM developed a Telehealth Clinical Skills Program (TCSP), intended to improve the acceptance and use of telehealth services by rural and remote doctors, with funding by the Australian Digital Health Agency.
The anticipated outcomes of the TCSP were that doctors’ competencies in conducting a remote (phone or video) consultation, and confidence in their ability to meet the expectations of the patient, carer or other health professional participating in these consultations would improve.
Methods
Design of the intervention
The TCSP aimed to improve doctors’ competence in conducting remote (phone or video) consultations, and confidence in their ability to meet the expectations of the patient, carer or other health professional participating in these consultations. The assessment modelled a ACRRM mini-clinical evaluation exercise (mini-CEX)11, which is a tool for assessing trainees’ performance in the workplace12, and is used throughout the ACRRM curriculum13. The TCSP included a simulated consultation, and education on use of peripheral devices, accessing medical records, making referrals, ordering tests and medication.
Trainees participated in a 90-minute session where one of two 30-minute clinical scenarios were enacted, supplemented by discussions with the trainees. Each session included feedback opportunities, and an additional education component covering all aspects of telehealth services, including:
• how to manage privacy and security
• the value and benefits of video compared to telephone consultation
• how to make a diagnosis remotely
• how to incorporate use of shared health records
• use of other digital tools such as diagnostic devices (eg a tele-stethoscope).
Recorded simulations began with the use of the audio component only of a videoconferencing platform to enable assessment of the key criteria for good telephone consultations. Subsequently, the video component was enabled to assess the value of progressing to video consultations.
In the first scenario the doctor receives a call from an Aboriginal Health Worker who is in a small community often serviced on a daily basis by doctors who reside in other locations. They then interact with an Aboriginal Health Worker or remote area nurse who is physically at the clinic with the patient and carers. The second scenario models a direct interaction between a GP and a regular patient calling from their farming property (a 2-hour drive away), leading into a video consultation.
For each of the two scenarios, separate scripts and a summary of the patient’s history were provided to the medical educator, the training candidate and an actor. The medical educator provided diagnostic results and other clinical details at the trainee’s request. The actor worked to simulate authentic patient–doctor interactions.
Evaluation methods and tools
During the implementation of the TCSP the authors worked within a team to design and evaluate its outcomes using pre- and post-intervention surveys focused on trainee competence and confidence in undertaking remote consultations and analysis of recordings of each simulation (with permission from the trainee). The pre-intervention survey asked about the extent to which trainees had used telehealth and ancillary services such as the ACRRM tele-dermatology service14. The medical educator asked trainees to self-rate, on a 10-point scale, their confidence and competence in undertaking telephone and video consultations, and the additional value of using video compared with the telephone. At the end of each session the medical educator repeated the same questions to determine changes to the initial ratings. ACRRM also undertook a follow-up survey to validate the study results: trainees were asked to confirm if their levels of confidence and competence had improved after the training.
To understand the competencies acquired by trainees in the TCSP, a process of open thematic coding15 of recordings, informed by the desired competencies, was used to assess the contribution of the TCSP. The desired competencies included communication, history taking, physical examination (online), clinical management, professionalism and an overall assessment. For example, competency measures included the checking of patient e-health records, advising on communication problems and building patient rapport. Competency in physical examination included considering if an adequate examination could be done, using an optimal mode for the examination (eg video instead of telephone, use of adjuncts), capturing visual or auditory information (eg coming closer to a camera/microphone), taking a photo, noting relevant symptoms and undertaking a logical, organised assessment.
Program participants
Trainees were introduced to the TCSP by an email requesting consent to participate in the program and its subsequent evaluation. Eleven doctors working in rural or remote areas enrolled, with five participating in the first scenario and six in the second scenario. In this report each trainee is referred to by a code (eg P001).
Ethics approval
Flinders University Human Ethics Low Risk Panel approved this research (Project 4563).
Results
Confidence and competence in remote consulting
The majority of trainees had experience of using telephone and video technologies for remote consultations. Those who had provided few video consultations felt that their ability to use video technology was low. Most trainees had not previously received training in the use of video. Many were unsure about accessing state or national patient e-health records, and the possibilities of digital photography.
At the commencement and completion of each session, trainees were asked to rate their confidence and competence in undertaking remote consultations overall, in telephone and video consultations specifically, and about the additional value of using video compared with the telephone. Table 1 summarises the average improvements in confidence and competence reported by trainees during a training session.
The final post-intervention trainee survey confirmed a similar improvement in competence and confidence, from about five to seven points on a 10-point scale.
Table 1: Medical trainee confidence and competence (on a 10-point scale) in undertaking remote consultations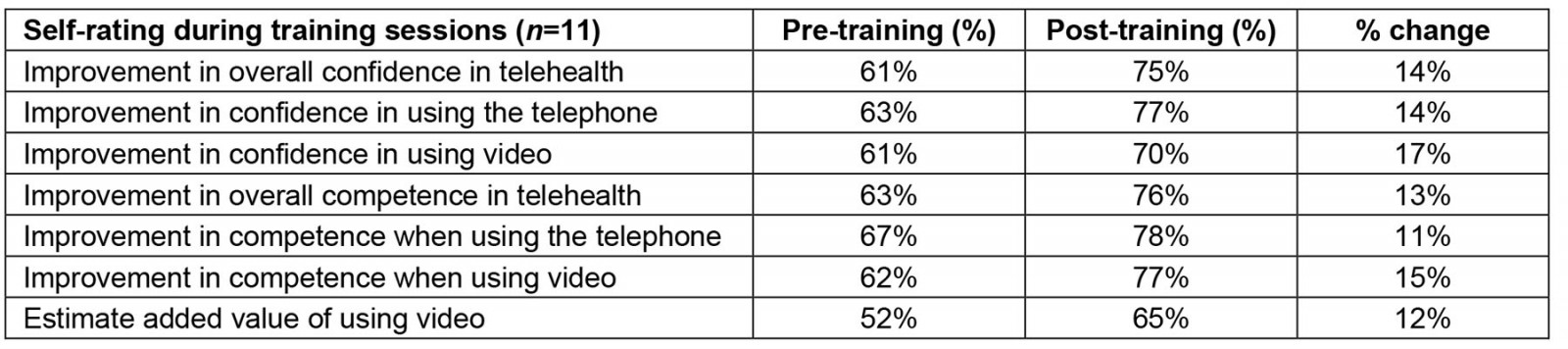
Competencies assessed within the Telehealth Clinical Skills Program
Most trainees displayed good communications skills including patient-centred communication, empathy and respect, consideration of cultural values, and attitudes and beliefs. All trainees obtained a clinical history and discussed the impact of the clinical presentation on patient function.
All trainees considered that an adequate physical examination for these scenarios could be done through video, and the majority of trainees conducted organised, logical consultations, capturing relevant signs and symptoms and possible differential diagnoses. It was observed that many trainees would benefit from further training when using video, such as in the use of the camera.
Discussions between the medical educator and the participants covered many desirable skills that had not been evident during the simulation, including the need to confirm patient identity, obtain consent, and ensure privacy or confidentiality. For instance, the medical educator asked one trainee ‘who’s at the other end of the phone? … is there anyone else in the room because you don’t have a view of who else is in the room’.
The medical educator focused on simple techniques for capturing visual, auditory or movement information; use of digital photography and peripheral digital devices such as otoscopes and stethoscopes; and how to assist the patient or heath worker with the physical examination. This was not always a straightforward process: one trainee recalled that when the internet connection was poor they had a nurse take a photo using their mobile phone, who then called to say ‘it looks really good’. However, when the photo of the wound arrived they realised ‘actually that looks really, really weird’ (P002).
Often simple solutions that could improve the quality of remote physical examinations had not occurred to trainees. For instance, the medical educator advised several trainees that:
If you ever had to do an oral exam ... the secret is to have a good torchlight … so you can get pretty good images of throats … you can use a spoon or a tongue depressor, so that if someone else has got the camera … [they] can get some pretty good pictures.
Trainees particularly welcomed instruction on how to organise consultations and conduct remote clinical examinations, with one commenting, ‘you’ve given me a few ideas about examinations, … and the lighting (and) getting the receptionist to make sure we’ve got a landline, mobile and an email address’ (P010).
Participants’ views on overall benefits of the Telehealth Clinical Skills Program
Trainees in both simulation scenarios felt that their competencies to undertake telehealth consultations had improved. For instance, trainees stated:
Well, I think I would definitely ask … for the nurse or the health worker [to do] more examination. (P001)
I think I’ve been learning how to better direct the (patient) examination. (P003)
I think I would be able to do a lot of the examinations. (P006)
… certain things in examination. I can ask them to do it (now). (P007)
During the educational component of each session, trainees were stimulated to explore new ideas for their practice. One trainee commented, ‘I’m going to go and check it out, about the equipment that you mentioned there, for the video, the scope [otoscope] and the virtual stethoscopes’ (P003).
Awareness of e-health services was strengthened. A trainee acknowledged that 'access to the patient records is invaluable because then you don't have to ask questions that you have the answer in front of you and then you can concentrate on other matters’ (P003).
There was a consistent improvement in the trainees’ self-rating scores of confidence and competence in telehealth overall and use of visual input (sending photography or short videos). The improvement in ratings for audio calls alone was not so evident.
Discussion
Following completion of the TCSP the self-reported confidence and competence of trainees improved by between 8 and 17 percentage points, and trainees felt empowered to improve their practice of telehealth using both telephone and video. All trainees rated video consultations as providing significant additional value.
Each simulation included assessment of a core set of skills for the conduct of any remote consultation, including trainee communication, history taking, physical examination, clinical management and professional competencies. There is evidence that some doctors were reluctant to attempt online physical examinations during the COVID-19 pandemic16. Other studies have concluded that assessment of physical examination skills can be successfully conducted online17. The outcomes of the TCSP support the feasibility of online assessment of physical examination skills. A key mechanism in assessing and improving the confidence and competencies of trainees in conducting common types of remote physical examinations in general practice proved to be discussions between the medical educator and trainees.
Reluctance to attempt online physical examinations may be linked to explanations for the lower use of video consultations, which has been discussed by several researchers18-20 and mentioned by some trainees. These include:
- lack of access to and training in video technology platforms including hardware, software, peripherals and connectivity
- lack of clinical governance standards
- interoperability between technologies
- difficulties integrating video consultations in administrative and clinical workflows.
Decisions about technology platforms or networks being suitable for video consultations or offering supporting technology such as e-health records or electronic prescriptions can hamper how trainees can put what they have learnt from this program into practice. Therefore, ACRRM recommends education and support for organisations (as well as individuals) to improve the operation and usability of technology.
Trainees felt they could extend or adapt their current practice because they were able to deal with potential risks, were more aware of the capabilities of technologies and could assist the nurse (with the patient) to do the examination. In contrast to the conclusions of some studies that practical skills and clinical examination skills cannot be assessed reliably online within remote consultations21,22, the TCSP showed it was possible to assess some of these skills online. However, trainees continued to express concerns about set-up time, technical quality, privacy and confidentiality, interaction with and examination of patients, and maintaining the option to do telephone consultations.
Limitations and validation
The conclusions of this study should be treated with caution due to the small number of participants in this pilot program. ACRRM undertook a follow-up survey to confirm the study results, in which most trainees indicated that their levels of confidence and competence had improved by attending the simulation. Two trainees stated that their already high level of confidence in telehealth consultations had not changed.
Because the one-on-one simulations offered in this pilot are resource intensive, in a future program group sessions based on a single scenario may be especially valuable for health professionals who work for the same service or organisation.
Conclusion
As a result of participating in the program, the self-reported confidence and competence of trainees improved. Not only did confidence levels improve and the ability to conduct remote examinations remotely increase, but also trainees were stimulated to explore new practices. Offering an active, simulated environment in addition to traditional passive, written learning enabled doctors to practise and demonstrate their skill levels.
The simulation scenarios used in the program successfully reflected real-life situations for remote consultations and physical examinations. The educational component contributed towards significant improvement in self-reported confidence and competence in conducting remote examinations, and trainees were stimulated to explore new ideas for their practice.
Acknowledgements
Thank you to Dr Kambiz Bahaadinbeigy for reviewing previous manuscript drafts.
Funding
The ACRRM approved and funded the online survey of its members and evaluation of the pilot TCSP by the lead author.
Conflicts of interest
The authors report no conflicts of interest for this study.
References
You might also be interested in:
2016 - Household structure, maternal characteristics and childhood mortality in rural sub-Saharan Africa



