Context
Australia’s medical workforce problem is primarily one of maldistribution, with both the geographic distribution of doctors and the relative supply of medical specialities not currently meeting the health needs of Australian rural communities1. Despite policies designed to increase the medical workforce in rural and remote Australia, geographic disparities remain in patient access to care and in health outcomes2,3.
The Australian Government funds a network of University Departments of Rural Health (UDRHs), Rural Clinical Schools (RCSs) and Regional Training Hubs (RTHs), facilitating stronger rural training for nursing and allied health students, medical students and junior doctors, respectively. This network is distributed with geographical intent, with each providing clinical placement activity within a particular rural region of Australia4. The activity location of each UDRH, RCS and RTH is described contractually by the current Rural Health Multidisciplinary Training (RHMT) program using major clinical placement locations, with the intention that these are surrounded by a network of smaller sites5. Over time, a local network of established relationships and geographic area of placement activity for each university develops as an activity ‘footprint’. This footprint represents an appropriate focus for a university’s recruitment of rural students and priority workforce responsibilities; however, it lacks a precise definition that can be applied for these purposes.
Situated in western and south-western Victoria, Deakin University operates an RCS, UDRH and RTH. Western Victoria experiences health inequities relative to metropolitan areas of the state. Western Victoria Primary Health Network (PHN) residents experience more years of life lost (42.0) compared with those in metropolitan Victoria (31.9) for avoidable deaths caused by a wide range of disease types6. In 2021, only 6.5% of the state’s 7718 GPs were providing services in rural areas of the Western Victoria PHN, with 60% of these GPs aged 45 years or more7. Thirty-three percent (10 648) of Victoria’s Indigenous Peoples live in the Western Victoria PHN, representing 1.5% of the PHN population6. A subanalysis of the data presented by Versace et al (2021) highlights how socioeconomic status (SES) in rural areas of the PHN is low relative to metropolitan areas, with 63 435 (91.6%) of residents in the Western Victoria PHN residing in medium rural towns classed as deciles 1–5 using the Index of Relative Socio-economic Advantage and Disadvantage8.
Deakin’s 4-year graduate entry Doctor of Medicine (MD) Program includes RCS sites in Ballarat (Modified Monash (MM) category 2), Warrnambool (MM 3) and a network of smaller surrounding sites constituting the Rural Community Clinical School (Fig1)9,10. To date, all MD students have completed two pre-clinical years at a central campus in Geelong (MM 1), prior to commencing their two clinical years at one of the rural or metropolitan clinical schools. To address the medical workforce needs of rural Western Victoria, a rural strategy working group was established (2020) to design a Rural Training Stream (RTS) for the MD10. The working group included representatives of the RCS, UDRH, RTH, course team, health services, professional staff and students. The aim of the RTS was to increase access to the MD for local rural students and provide them with extended rural training in the region, to improve local graduate retention.
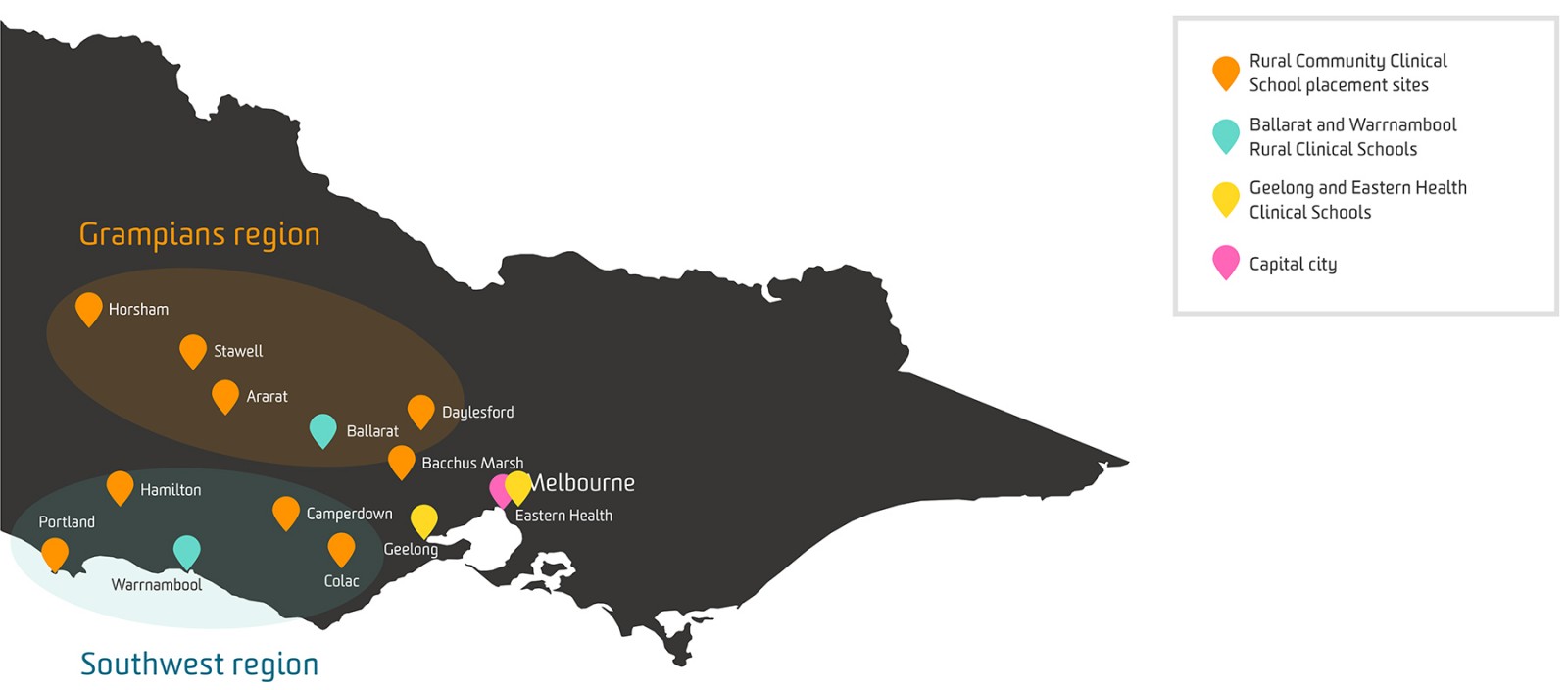 Figure 1: Deakin School of Medicine Clinical School locations.
Figure 1: Deakin School of Medicine Clinical School locations.
Issue
With a few exceptions, strategies to increase the admission of rural background students to Australian medical courses have adopted a binary approach, assigning rural background status to applicants meeting the RHMT program definition of 5 years continuous or 10 years cumulative residence in a rural location as defined by Australian Statistical Geography Standard Remoteness Areas (ASGS-RA) 2–5 or MM 2–711. Applicants fulfilling this criterion are equally eligible for preferential rural entry streams and admission quotas across the country, resulting in many undertaking training removed from their area of rural origin, frequently in metropolitan locations.
Commonly, workforce outcomes for Australian health professional graduates have been reported using either the ASGS-RA or MM classifications, but without reference to a specific geographic region12. More recently, a small number of published studies have investigated the return of graduates to practise in their region of origin or training, using different methodologies to define these regions of interest. A single university study described five areas within Victoria using health workforce planning regions, identifying two of these aligning with its program’s footprint13. A 2021 national-scale study described 54 regions across all of Australia using Australian Bureau of Statistics (ABS) Statistical Area (SA) boundaries (SA3/4), chosen to align closely with the structure of Queensland’s Hospital and Health Service boundaries and New South Wales Local Health District boundaries14. Studies from Australian universities that prioritised recruiting students from the state or territory in which they are located have reported workforce outcomes through the same jurisdiction-based measure15,16. These studies demonstrated promising results of a ‘grow your own’ workforce strategy, with students who grew up and also trained in the region being up to 17 times as likely to work in the same region after graduation14.
With growing evidence supporting strategic ‘grow your own’ approaches to recruiting, training and retaining health professionals from and for underserviced rural communities13-17, there is a need for sound methodologies by which universities with a social accountability mandate can accurately describe their region of rural focus. This article describes the process, outcomes and lessons learned through a project undertaken during 2020–21 to describe Deakin University’s rural health activity footprint formally. Deakin’s Rural Strategy working group identified early the need to define the rural footprint clearly. The working group met monthly online from the beginning of 2020 and completed the footprint definition process within 12 months. The definition was used to select the inaugural RTS cohort (2021).
Step 1: Defining the regional boundaries
Australia has a network of 31 PHNs that closely align with areas of activity of state and territory hospital networks18. Our project identified that Deakin University’s clinical placement and RTH activity is broadly aligned with the Western Victoria PHN (Fig2), thus we chose to utilise this boundary to define the outer limits of our footprint. However, given the PHN area includes locations of varying levels of rurality, from metropolitan centres (Geelong, MM 1) to more rural locations, it could not exclusively describe our rural footprint.
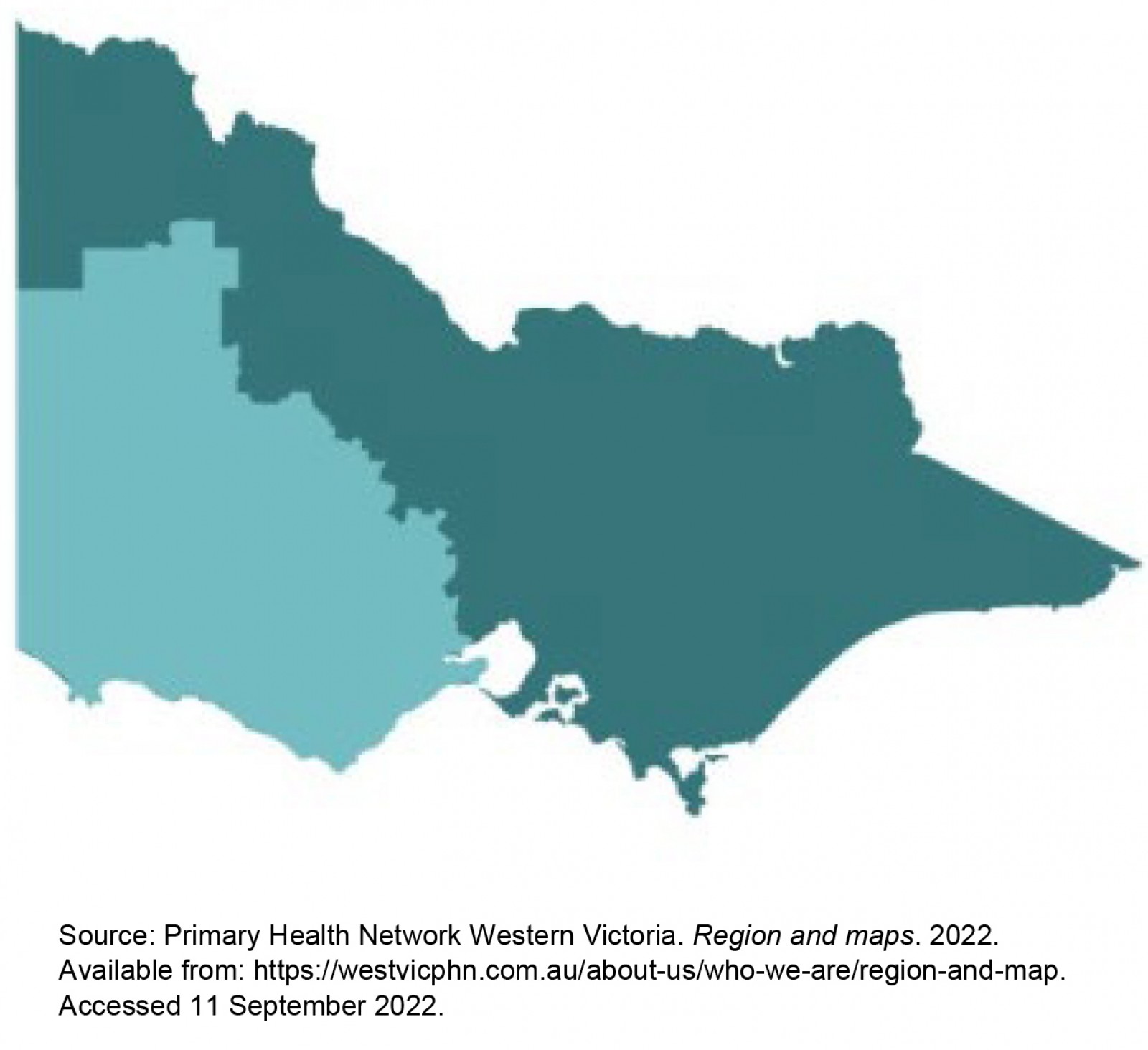 Figure 2: Western Victoria Primary Healthcare Network outline.
Figure 2: Western Victoria Primary Healthcare Network outline.
Step 2: Defining ‘rural’ within the footprint
Having defined the broad boundary of our region of interest using the Western Victoria PHN in step 1, we needed to identify further, within this zone, the areas that we considered to be our rural focus. For this purpose, ABS and non-ABS structures were considered.
Option 1 – Australian Statistical Geography Standard Remoteness Areas (ASGS-RA): The ASGS-RA is an ABS structure that utilises statistical area data to define rurality according to five classes of remoteness based on proximity to services (RA1 – Major Cities of Australia, RA2 – Inner Regional Australia, RA3 – Outer Regional Australia, RA4 – Remote Australia, RA5 – Very Remote Australia)11. Commonly, RA2–5 is used to define ‘rural’ locations and RA1 metropolitan. Although classifications within the region of interest outlined by the Western Victorian PHN are in the range of RA1–4 (Fig3), we found that applying RA2–4 to describe the rural footprint was inclusive of locations considered too close to metropolitan centres (particularly those on the fringes of City of Greater Geelong, population >250 000, RA1). Alternatively, specifying RA3–4 as the inclusion criterion excluded a significant portion of our rural clinical placement locations and one of our major rural training centres (Ballarat, RA2).
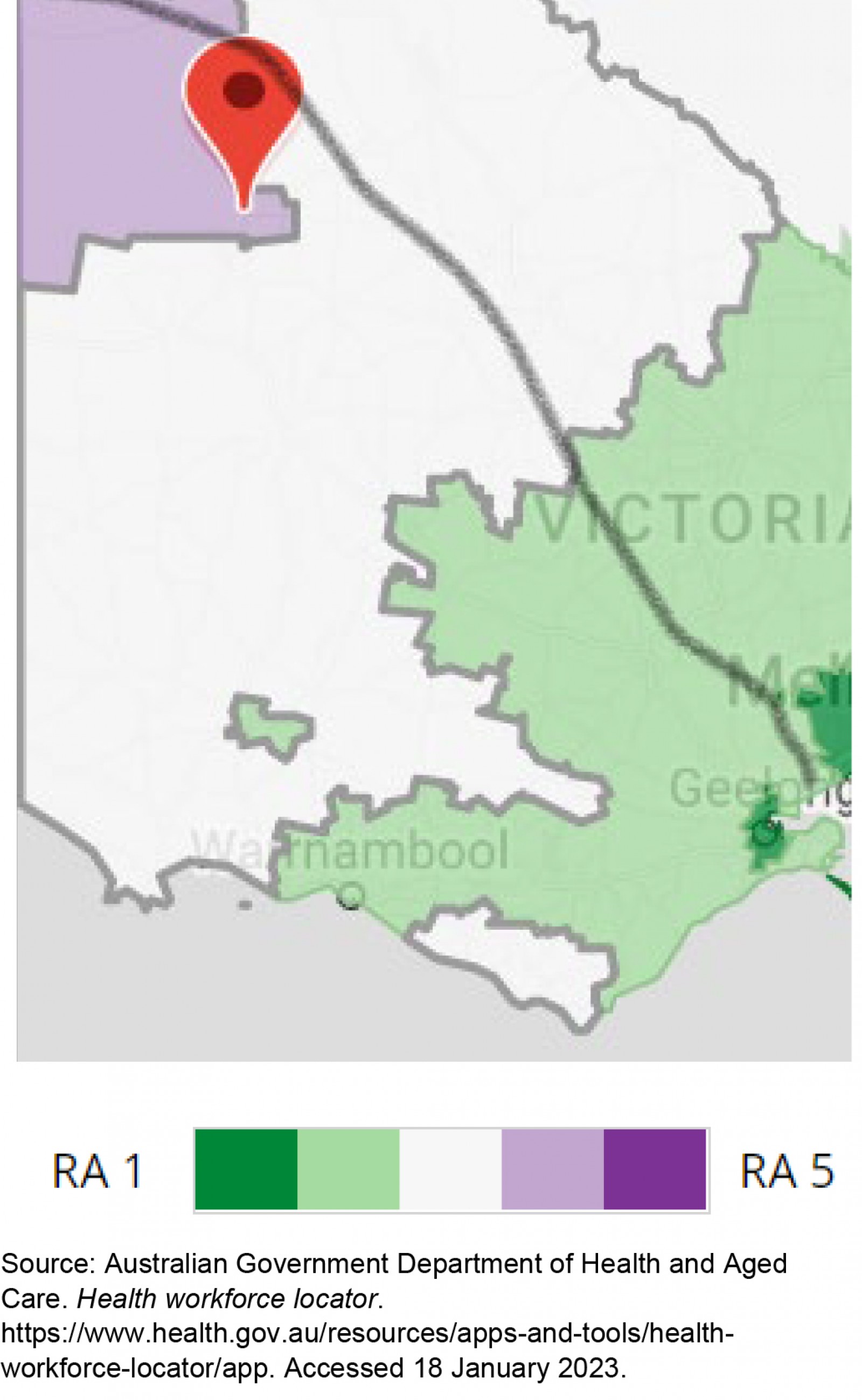 Figure 3: Australian Statistical Geography Standard Remoteness Areas classification applied to rural footprint.
Figure 3: Australian Statistical Geography Standard Remoteness Areas classification applied to rural footprint.
Option 2 – Modified Monash Model (MMM): The MMM has been adopted as the standard in the health sector for defining rural locations within Australia, underpinning the 2021–2031 National Medical Workforce Strategy and, from 2022, employed to define rural areas for the RHMT program9. The MMM describes rurality using seven categories, building on the ASGS-RA framework but with greater emphasis on the local community’s population size.
With reference to our area of activity, the MM compared to the ASGS-RA provided increased granularity and differentiated the rurality within the PHN. A significant proportion of our rural placement activity area comprised MM 5 (Fig4). However, there were limitations again in using the MMM as a filter to describe our rural footprint, as use of MM 3–6 excluded Ballarat (MM 2), while MM 2–6 included locations on the urban fringe of Geelong that were agreed not to be priority rural communities. In addition, a small area at the end of the Bellarine Peninsula was classified as MM 3 and 4 (eg communities of Queenscliff, Point Lonsdale, Portarlington, St Leonards), but again due to their proximity to Geelong (approximately 30 minutes by car) these areas were not considered an area of rural activity focus and required exclusion from the final rural footprint definition.
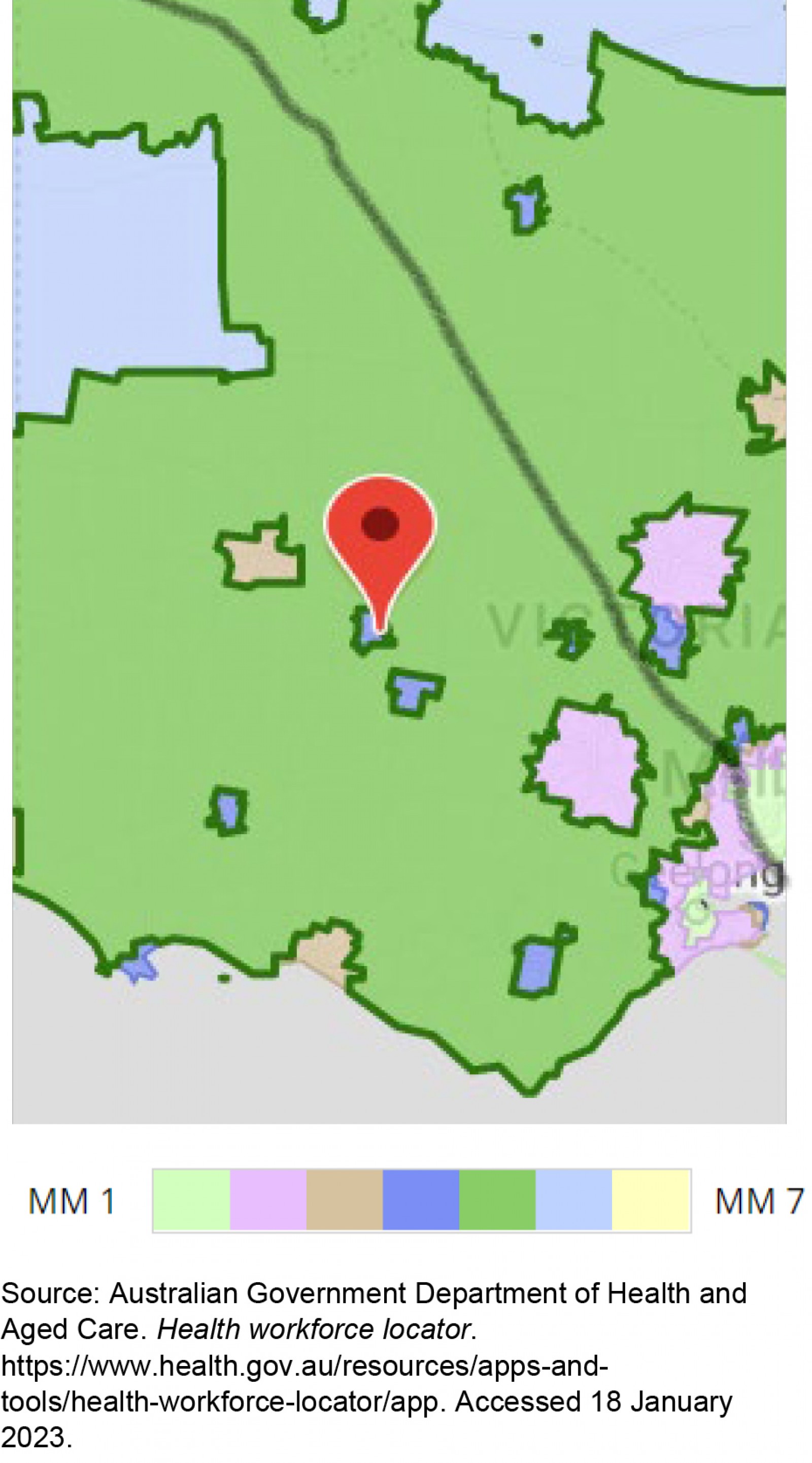 Figure 4: Modified Monash Model applied to rural footprint.
Figure 4: Modified Monash Model applied to rural footprint.
Option 3 – Local Government Areas: Local Government Areas (LGAs) are non-ABS structures that describe local council areas of activity19. The territory of a PHN consists of a number of LGAs, so the inclusion and exclusion of specific LGAs has the potential to classify areas of focus (Fig5). However, within LGAs there are significant differences in rurality, with some LGAs adjoining Geelong including locations ranging from MM 1 to MM 5 (eg Golden Plains)20. Furthermore, LGAs are not currently assigned as part of course applicant’s admission process, making these impractical to apply.
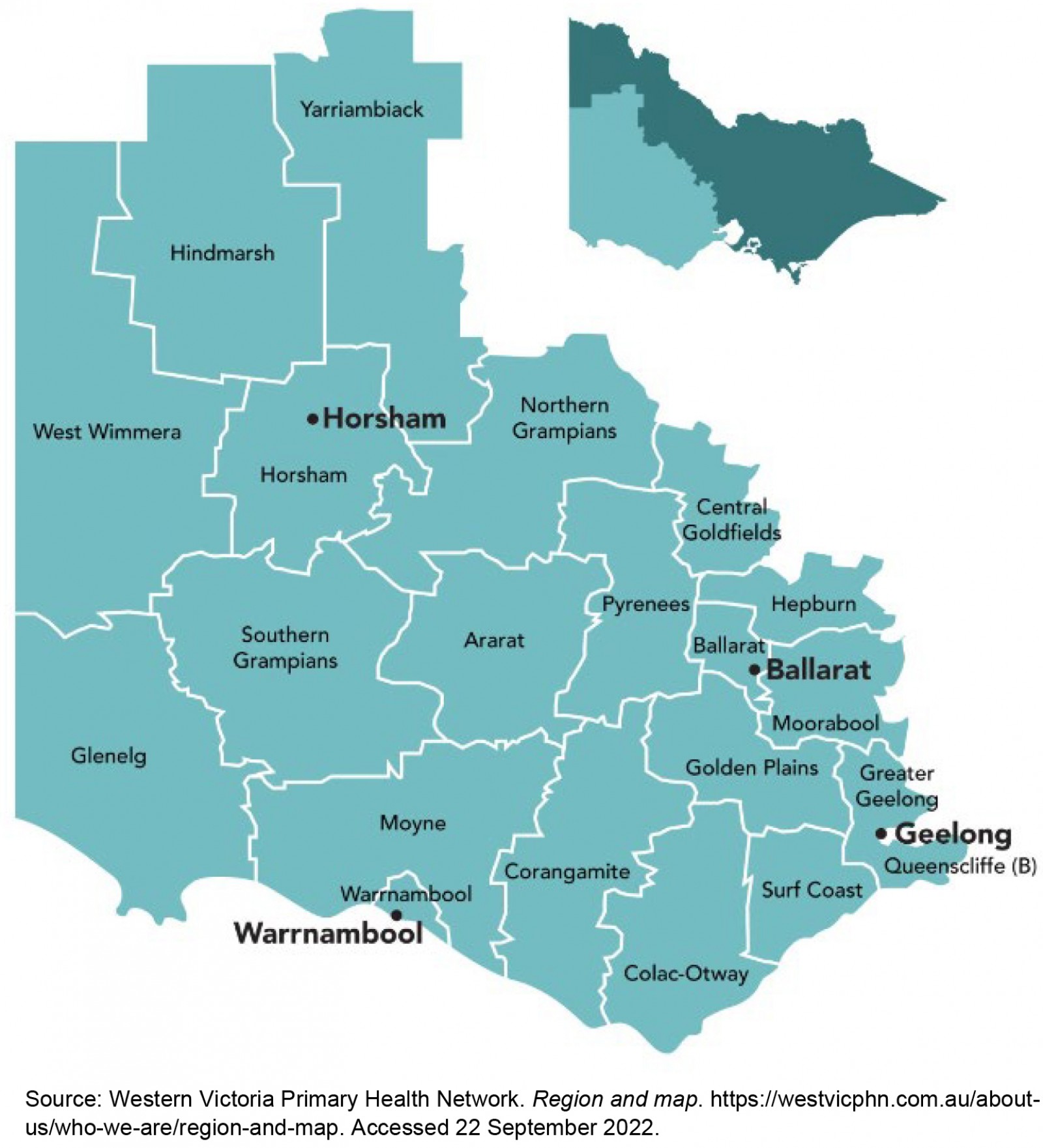 Figure 5: Local Government Areas in Western Victoria Primary Health Network.
Figure 5: Local Government Areas in Western Victoria Primary Health Network.
Option 4 – Postcodes: Postcodes were reviewed as a way of subdividing the PHN19. This information is collected as part of all course applications and could be readily utilised during course admission to identify applicants from the rural footprint. However, postcode territories become very large in rural areas and some were found to cross the boundaries of the PHN significantly. Furthermore, postcodes may include locations of significantly different rurality. For example, postcode 3340 includes both Balliang (MM 4) and Bacchus Marsh (MM 1), limiting their utility in the identification of rural students.
Option 5 – Statistical Areas: We considered the usage of level 2 Statistical Areas (SA-2) to subdivide the PHN, as these areas have been designed to describe communities that interact socially and economically19. However, Statistical Areas were not collected during the admissions process, nor are they practical to collect prospectively, so could not be readily utilised.
Lessons learned
It became evident that there was no single geographical or rural framework that (1) accurately described our area of activity, (2) accurately described our desired workforce focus, (3) was practical to apply during the admissions process. We ultimately settled on a bespoke approach, resulting in the working rural footprint definition (Box 1). This relies heavily on the Western Victoria PHN boundary and MMM but required the additional inclusion and exclusion of specific locations.
Although complex, this working definition allowed us to create a list of 965 locations that comprise our rural activity footprint. This has become a living reference document that can be updated periodically to reflect new or reclassified locations. The development of an accurately described rural footprint has several utilities and applications.
Box 1: Working definition of Deakin University’s rural footprint.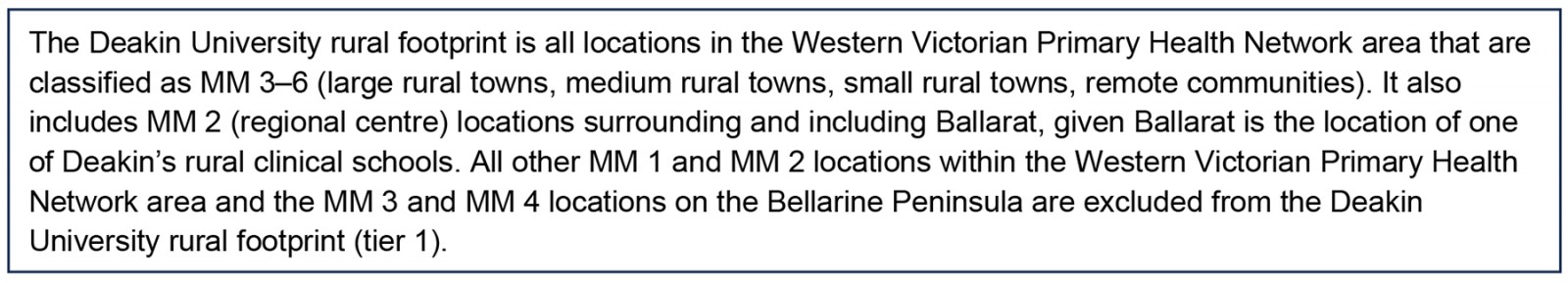
Application 1: Student selection
To adopt a more geographically focused ‘recruit, train and retain in the region’ strategy, it is necessary to admit students preferentially from a more limited geographical area. One of the primary stimuli for this project was the establishment of the RTS within Deakin’s MD course, with a primary aim of increasing access to the course for applicants from communities within our rural footprint. Our definition allows us to do this, using each applicant’s provided rural background location (according to the RHMT program definition5) to assign a MMM classification followed by a rurality tier. To be considered tier 1, applicants must meet the RHMT definition for a location within the rural footprint to be eligible for priority entry to the RTS. Tier 2 applicants meet the rural background definition of Victorian rural locations (MM 2–6) not included in tier 1, and tier 3 comprises the rest of rural Australia (MM 2–7). In addition to these administrative data, applicants complete a written statement that includes a description of their connection to their rural community. To date, this approach has been successfully applied to admission of our first three RTS cohorts.
Application 2: Graduate workforce outcomes
Having our region of rural workforce focus accurately described allows us to evaluate the retention or return of graduates to our specific region. As we continue to track our graduates throughout pre-vocational training and onto later practice locations, we will examine the training pathways followed by those originating from our rural footprint and their future work locations. This will provide valuable information regarding the workforce impact of the RTS and add to the literature on the effectiveness of ‘grow your own’ approaches.
A regionalised approach also increases our ability to focus on the health needs of local communities and evaluate progress towards our longer term goals of improving the health and wellbeing of the communities we serve. The baseline data available for the Western Victorian PHN provides a useful reference point; however, we are engaged in further work to describe socioeconomic and health service access data at the address level within our footprint21.
Application 3: Stakeholder relationships
Rural clinical placements are underpinned by partnership arrangements with health services, including hospitals, general practices, allied health facilities, Aboriginal Community Controlled Health Organisations and community health services. These relationships are symbiotic, sharing a common goal to provide quality clinical placements to train future local rural healthcare practitioners. In the context of the current national rural health workforce crisis, supervision and placement capacity is fragile, with rural clinicians often concurrently responsible for multiple medical learners at a range of levels for various durations. In this context, the ability to demonstrate targeted selection of students from the region and return to the region of training is critically important to maintaining and strengthening these partnership relationships.
Application 4: RHMT reporting
Annual reporting of placement activity is required as part of the RHMT program. This reporting captures the activity within each university’s footprint, rather than including placements outside the footprint, such as remote electives. Accurate reporting requires an activity footprint to be precisely described, which this definition enables. This approach could potentially be transferable to other RHMT program participants to clarify geographic areas and identify any potential for overlapping counting of placements.
Furthermore, evaluation of graduate outcomes using the MMM achieves RHMT policy relevance and allows our graduate outcomes to be reported by each category of MMM and included in multi-site meta-analyses, an approach recommended in the recent literature to improve RCS outcome research, and in health research more broadly22,23.
Conclusion
Although the Australian context has a strong influence on this work, the principles and potential applications are relevant to international health professional education programs wishing to focus their activities on a geographical region. With growing interest in socially accountable medical education and evidence supporting place-based selection and training of students, this article provides an example of how a rural activity footprint has been accurately described in the Australian context and successfully employed in recruiting medical students. Future program evaluation will include an analysis of workforce outcomes with the ability to report on graduate outcomes both from and for a specific geographic region.
Acknowledgements
We acknowledge Deakin School of Medicine Rural Strategy Working Group members involved in this project.
Conflicts of interest
The authors declare no conflicts of interest.
Funding
A number of the authors are funded as academics under the Australian Government Rural Health Multidisciplinary Training program to undertake this work.
References
You might also be interested in:
2020 - ‘It’s mostly about the job’ – putting the lens on specialist rural retention





