Introduction
The most common spinocerebellar ataxia worldwide1, MJD has the highest estimated prevalence in affected Aboriginal communities of the Top End of Australia2-5, including Groote Eylandt and Ngukurr in the Northern Territory. MJD, or spinocerebellar ataxia 3 (SCA3)6, is a rare autosomal dominant neurodegenerative disease that leads to progressive ataxia resulting in loss of coordination of all motor functions, and there is no cure7. Within 5–10 years of symptoms first emerging, individuals typically become wheelchair dependent and require full assistance for all activities of daily living8, with a mean life expectancy of 20 years from symptom onset. MJD can occur around 8–10 years earlier than in the previous generation due to genetic anticipation9,10.
The Staying Strong Toolbox is a physical activity and lifestyle program designed by Aboriginal families living in Groote Eylandt and Ngukurr, to keep their families walking and moving around. Families with MJD in these communities who were concerned about their declining mobility11 partnered with the MJD Foundation and university researchers to co-design the Staying Strong Toolbox12, based on their experiences11 and what is known from MJD research10,13.
Whether the program can be carried out as families with MJD intended, and whether participants can engage, adhere and perceive benefits of the program without serious adverse events14 is, logically, the next issue to address. The co-design process provided foundations for a feasible program because it was community-initiated, informed by families’ lived experiences of MJD11,15 and drew on support workers accepted by the community12,16. Whether the program could be implemented in a real-world setting, in harmony with the unique culture and lifestyle of Aboriginal families with MJD living in the remote Northern Australian environment, is examined in this article. It was believed that exploring feasibility would inform program implementation and program evaluation in any future efficacy trials.
Physical activity programs responsive to the culture and lifestyle of families with MJD and those with degenerative ataxias more broadly are scarce in Australia and internationally, despite calls for person-centred rehabilitation programs17,18. For Aboriginal people and other First Nations Peoples internationally, programs are found to fail when views, lifestyle and concepts of cultural and traditional practices are not taken into account11,19. Research on the benefits of any physical activity programs for individuals with MJD is challenging, limiting the available evidence13,20. Particular challenges arise because MJD is a rare disease that affects families in small clusters around the world, with marked clinical heterogeneity between individuals20. Additionally, conduct of randomised clinical trials to demonstrate intervention efficacy can be problematic21, in the face of small sample sizes, and high variability of and social barriers to trial procedures such as randomisation and blinding, particularly for interventions that defy standardisation, because they must be tailored, individualised and flexible to individual needs17,18. Notwithstanding these challenges, opportunities are created to consider innovative research designs22, to richly describe novel interventions in preparation for real-world application, to develop useful insights for clinicians and support workers to draw from, and for families to learn from23. To address some of these challenges, and to take advantage of these opportunities, this study used a mixed-methods, multiple case study design to determine the feasibility and impact of the Staying Strong Toolbox program on walking and moving around for Aboriginal families with MJD in the Top End of Australia.
Methods
Design
A pragmatic approach, drawing from Indigenous and participatory methodologies, formed the overarching methodology for this work and the development of the Staying Strong Toolbox Program10-13. A mixed-methods, multiple case study design was chosen to allow multiple individuals (cases) to be studied to illustrate feasibility and program impact24-26. Each individual who participated in the program was defined as a single case. Case study design provides a flexible, culturally responsive approach for individuals to individually tailor and pilot their own program in a real-life context27-29. Case study design can accommodate variability in functional levels between individuals20 and it allowed for a rich description of the program from the small group of participants with MJD27. The mixed-methods design allows qualitative findings to be used to explain quantitative findings and for these findings to be integrated to strengthen Toolbox design and implementation29-31.
Feasibility of the Staying Strong Toolbox was determined by documenting program participation, adherence to program activity32, cost, and program acceptability from the perspective of participants. Program participation and activity were recorded in a single research diary for the project. Acceptability was explored through semi-structured, in-depth interviews with participants33. Impact on walking and moving around was determined using outcome measures of mobility, ataxia severity, quality of life (QOL), wellbeing, goal attainment and self-perceived impression of change32. Participant perspectives on their performance further reflected program impact. In the absence of specific reporting guidelines for mixed-methods case studies the CONSIDER statement checklist for health research involving Indigenous peoples34 and STROBE statement checklist for reporting of observational studies were used35. A TREND checklist was also completed as the study aligns with the WHO definition of a non-randomised clinical trial36,37.
Setting
The study was conducted in the very remote Aboriginal communities of Groote Eylandt (Angurugu, Umbakumba) and Ngukurr, which are situated in the Top End of Australia and have populations of approximately 15005 and 972 respectively38, described in detail previously11 (Fig1). Both communities have a local health clinic and visiting medical services, but limited disability-friendly infrastructure39,40. Away from the main communities, travel is difficult on unsealed rough roads over uneven terrain, and living conditions can be harsh in monsoonal rain, and extreme heat and humidity41. Fishing, hunting and gathering on homelands remote from the main communities are an integral part of life. Adherence to cultural responsibilities and traditions remains very strong42,43. English is generally not the first language spoken. Anindilyakwa is the main language spoken by Aboriginal people of Groote Eylandt and Kriol is the most common language spoken in Ngukurr40,42.
Families in these communities have faced the impact of MJD for generations. Typically, most individuals are wheelchair-dependent or dependent on others within 10–15 years of symptoms emerging6. Three generations of family members have been affected by MJD simultaneously, at different functional levels and stages of disease. Many families in both Ngukurr and on Groote Eylandt consider remaining home on their lands and being close to family as a high priority, regardless of their functional level or remoteness from services12.
The research team included Aboriginal community researchers from Groote Eylandt (JL, GL, GwL) and Ngukurr (BD, OD), and a non-Aboriginal researcher who is also a physiotherapist (JC), well known to families in each community through previous research11,13. JC travelled between each community to facilitate the program, guided by JL, GwL and GL on Groote Eylandt and BD in Ngukurr. OD provided technical support with Garmin Vivofit 4 activity tracker set-up and program support when required.
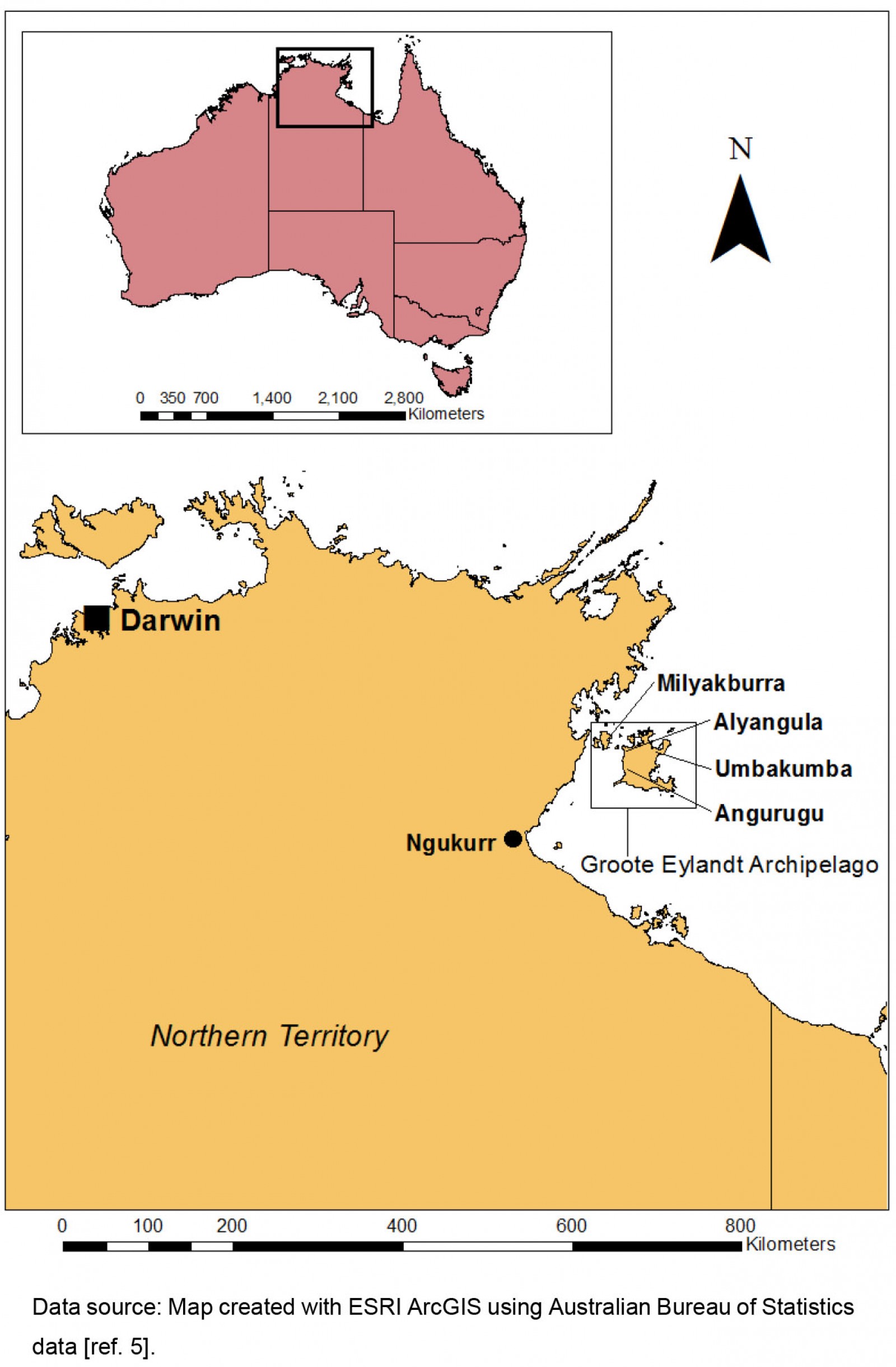 Figure 1: Location of Groote Eylandt and Ngukurr.
Figure 1: Location of Groote Eylandt and Ngukurr.
Participants
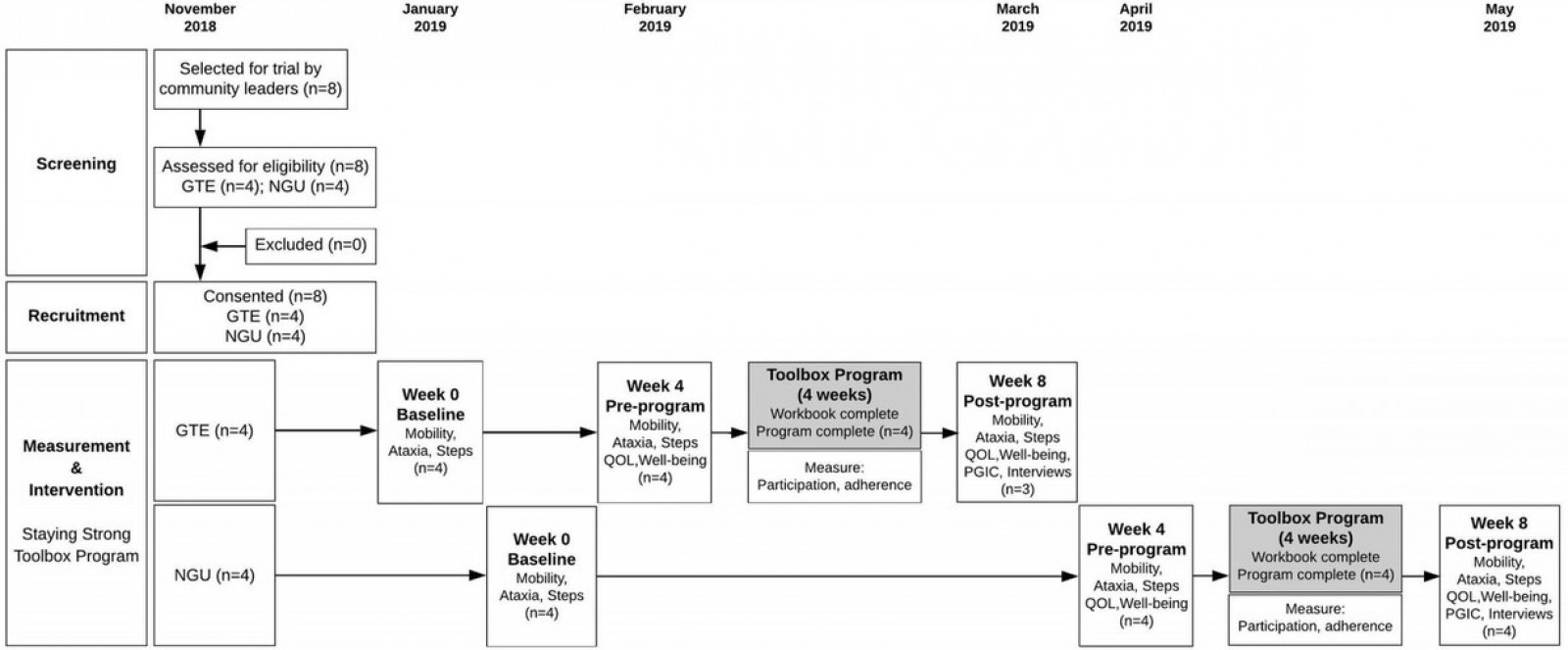
Four individuals with MJD from Groote Eylandt communities (Angurugu and Umbakumba) and four from the mainland community of Ngukurr participated in the study between November 2018 and May 2019 (Fig2, Supplementary figure 1). Participants were purposively selected and recruited in each community by local community researchers and leaders to achieve maximum variation representation of functional level, age, gender and family roles. Criteria for inclusion of participants included a clinical or genetic diagnosis of MJD, age 18 years or more, identified as belonging to either Groote Eylandt or Ngukurr communities, and able to provide informed consent. Participants were excluded if they had additional health conditions that impacted their mobility (eg a neurological condition such as spinal cord injury, a vascular condition such as amputation or a moderate to severe cognitive, intellectual or mental disability) or if deemed by their doctor to be medically unable to participate. Participants were informed of study requirements in their preferred language (eg Amamalya and Kriol) by local community researchers and provided either written or oral consent. Each participant communicated in their preferred language throughout the study.
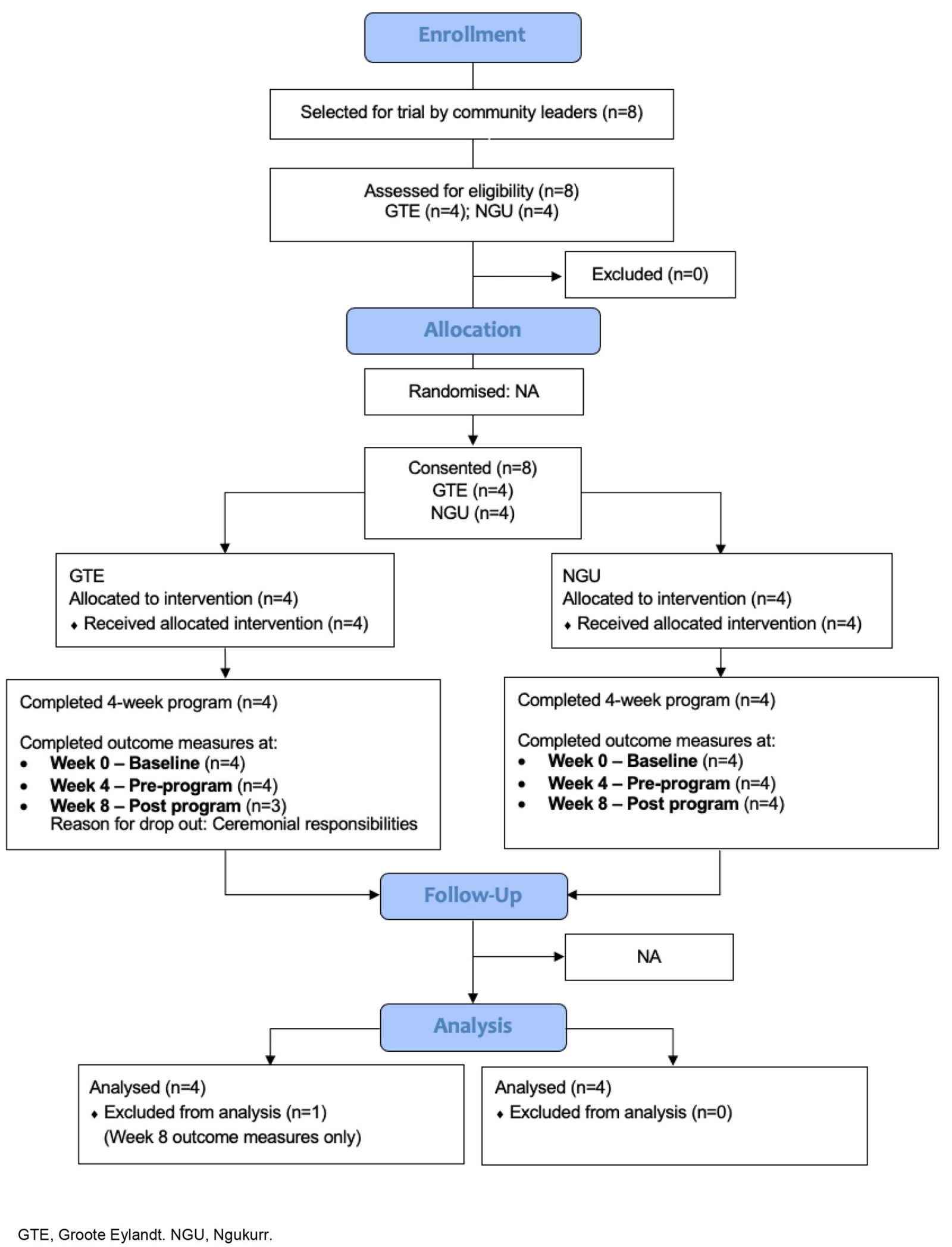 Figure 2: CONSORT flowchart.
Figure 2: CONSORT flowchart.
Staying Strong Toolbox program
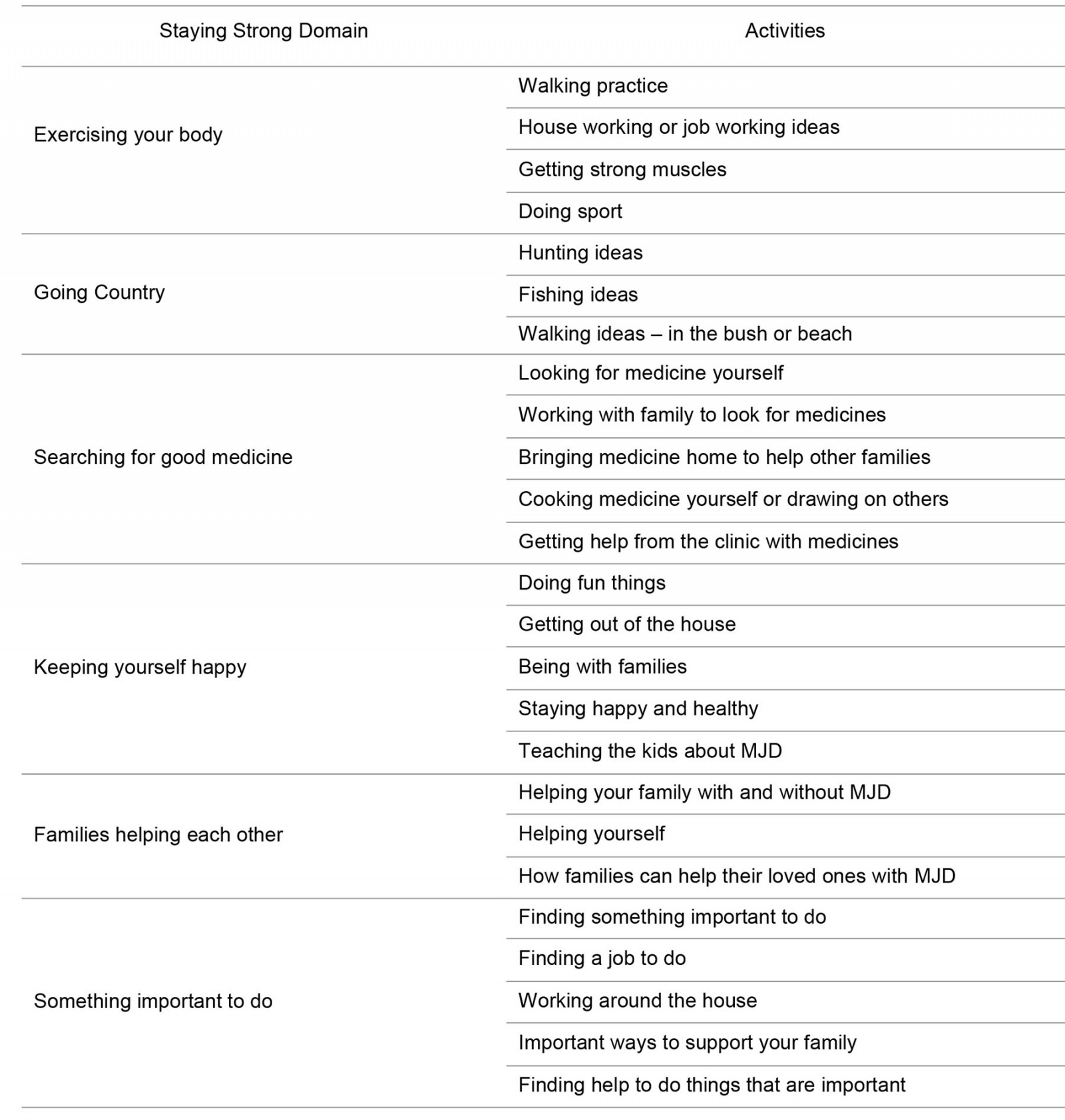
The program was tailored to each individual through use of the Toolbox workbook12. Based on the Staying Strong framework, the workbook has six domains for keeping strong on the inside and outside: ‘exercising your body’; ‘going country’; ‘searching for good medicine’; ‘keeping yourself happy’; ‘families helping each other’; ‘something important to do’11. Within each of the six domains, the workbook includes a range of activities (tools in the Toolbox). The participant selects activities of their choice from each domain to be included in their individualised program, according to their functional level: ‘strong’ (independently mobile), ‘wobbly’ (mobilising using a walking aid) or ‘wheelchair’ (wheelchair-dependent)12. Groups of activities within each domain of the workbook are included as supporting information (Supplementary table 1). The workbook prototype has been published elsewhere12.
Using the workbook (either alone, with family or with physiotherapist (JC) and community researchers) participants selected from the range of activities within each domain, by ticking activities they wished to do to keep walking and moving around. Individuals discussed activities they had selected with the physiotherapist (JC), who provided guidance where necessary on how to tailor tasks to the participant’s functional level to ensure the most physical benefit could be gained and to determine whether tasks could be performed independently or would require assistance. Lastly, participants set a specific goal to work on. Their goal and chosen activities were collated into a weekly planner by the physiotherapist (JC) alongside each participant to form a program. Participants carried out their program over a 4-week period as per Table 1.
Table 1: Program procedure13,44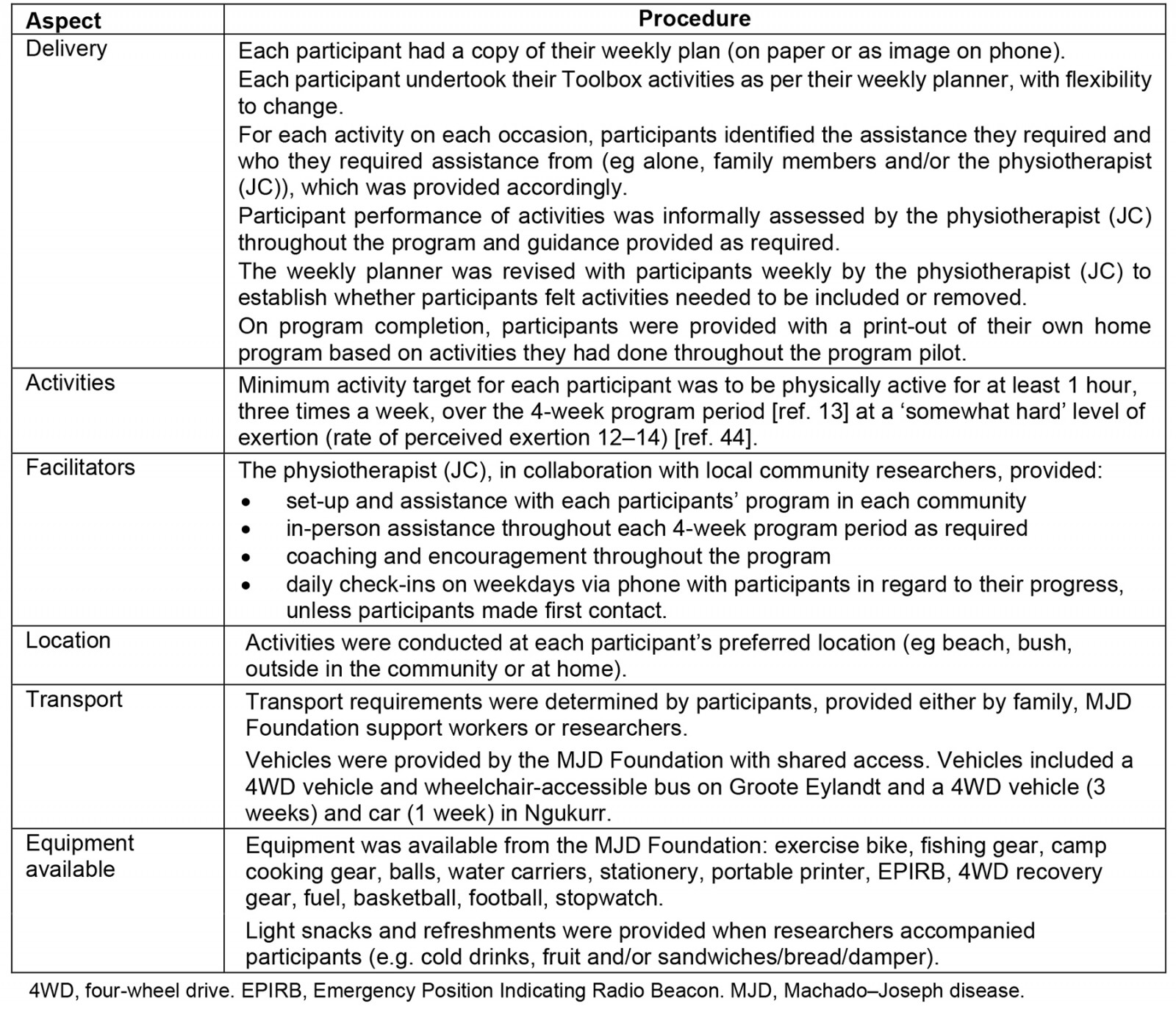
Measurement
Feasibility of the program: Participant characteristics (age, gender, location, employment status, mobility status) were collected at baseline. Feasibility was determined by (1) participation and adherence with the program (reach >80% of the minimum activity target) for each participant, (2) in the absence of serious adverse events/in the presence of coinciding events (events in the community that may or may not impact the program, such as ceremonial events, equipment issues, weather events), and (3) whether the program was acceptable from each participant's perspective (Table 2). Program activity data (types of activities, location, duration, assistance, supports, training reports) were collected from commencement of the program and recorded daily in the research diary. All study data were collated in Microsoft Excel by JC.
To determine both acceptability and impact, semi-structured, in-depth interviews were conducted with participants within 1 day after program completion. The topic guide is included in Table 3. Participants were interviewed by JL or BD and JC at their preferred location and time, in their preferred language. Costs attributed to the program were recorded.
Table 2: Measurement: program feasibility and impact32,45-55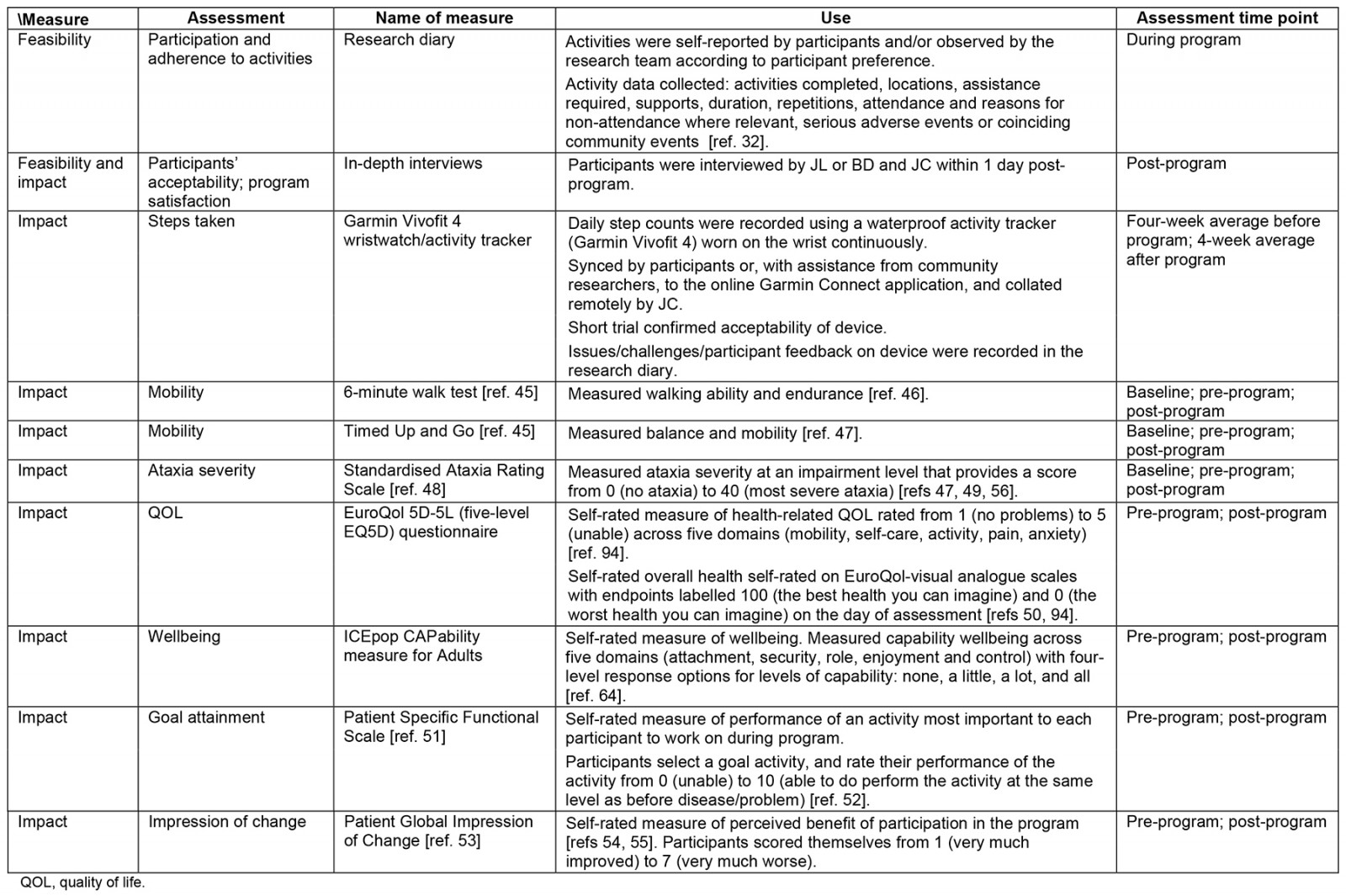
Table 3: Post-program interview topic guide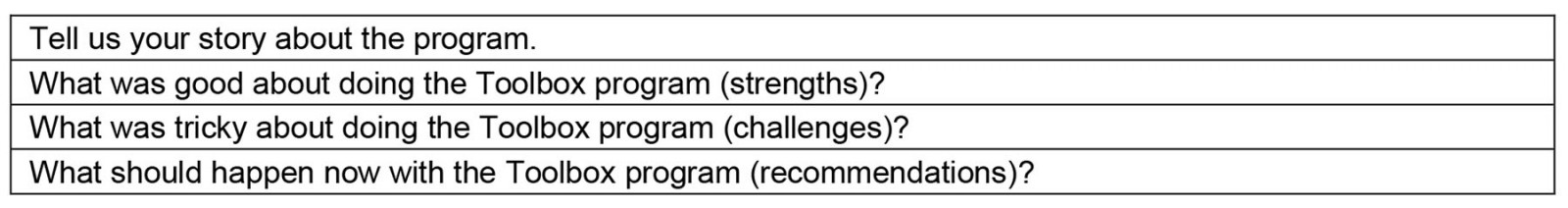
Impact on walking and moving around: Impact on physical (strong on the outside) and psychosocial (strong on the inside) wellbeing was explored using measures established as meaningful to participants13 and/or used in previous hereditary ataxia research in the absence of gold-standard measures56. Table 2 provides details of these measures and how and when they were collected.
Baseline to pre-program measures were used to confirm stability of pre-program mobility and ataxia severity57. In the absence of a control group, collection of data over the baseline period enabled participants to act as their own control. Pre-program to post-program measures were used to determine impact on mobility, ataxia, and steps taken. QOL, wellbeing and goal attainment were assessed only at pre-program and post-program to limit participant response burden58. Outcome measures were administered by the physiotherapist (JC) alongside local community researchers in each participant’s preferred language, recorded on video and scored by an independent assessor (LW). LW is a physiotherapist experienced in clinical rehabilitation, and who was provided with training on scoring guides for each outcome measure. As far as practicable, outcome measures were collected at the same location and time of day to minimise possible within-participant variability associated with the measurement environment. Participants completed all outcome measures in week 8 after completion of their program (Groote Eylandt: March 2019; Ngukurr: May 2019). No follow-up occurred after the 8-week assessment point after the program.
Data analysis
Feasibility and acceptability of the program: Participant characteristics, program participation and adherence data, and the presence of serious adverse events or coinciding community events (mean, range, percentages, descriptions summarised from research diary), were collated and described in Microsoft Excel. To determine acceptability of the program, interview data were analysed collaboratively between JC, BD and JL to describe participant perceptions of the program, positives and negatives of the program and recommendations for optimisation. NVivo v12 (Lumivero; https://lumivero.com/products/nvivo) was used to store and manage data and assist with initial coding of transcripts and notes59. Oral discussions between researchers occurred to verify codes from the data to identify and organise emergent categories60,61. A narrative was developed aligning with participants’ experiences and ideas about the program and reflecting back to the research questions. Findings were presented to participants for confirmation and to determine changes required for the Toolbox program or workbook.
Impact for each participant on walking and moving around:
- Raw scores for each outcome measure for each participant were reported at each measurement time point, except for steps taken.
- For steps taken, mean scores were calculated for the 4-week period between baseline and pre-program, and from pre-program to post-program.
- To describe change between time points, percentage change for each measure was calculated.
Impact across all participants on mobility, ataxia, steps taken:
- To determine impact on mobility and ataxia (Timed Up and Go (TUG) test, 6-minute walk test (6MWT), steps taken and Scale for the Assessment and Rating of Ataxia (SARA)), non-parametric statistical analysis was used (SPSS v26; https://www.ibm.com/products/spss-statistics) due to the small sample size and heterogeneity62.
- All pre-program measures (baseline and pre-program) for TUG, 6MWT and SARA were first compared with post-program measures with Friedman’s test (χ2, p-values). Where statistical significance on Friedman’s test was found (p<0.05), pairwise comparisons between each time point were performed to determine where greatest changes occurred (Wilcoxon signed-rank test (p<0.05)).
- Changes in steps taken before the program compared with during the program were assessed using the Wilcoxon signed-rank test.
Impact across all participants on QOL, wellbeing and goal attainment: Change was described by examining raw scores because no appropriate normative data were available to facilitate comparisons for EQ5D-5L and ICECAP-A health and wellbeing questionnaires63,64.
Ethics approval
This study was approved by the Human Research Ethics Committee (HREC) of the Northern Territory Department of Health and Menzies School of Health Research (HREC 2018-3044) and externally approved by James Cook University HREC (H7367). The approved study protocol has not been published previously (Supplementary figure 2). Permission to conduct the research was granted by responsible Indigenous agencies (Anindilyakwa Land Council and Northern Land Council) and appropriate land permits were secured prior to research commencement. The study was registered with the Australian and New Zealand Clinical Trial Registry (ACTRN12621001325897) after study completion, as community researchers’ enthusiasm and community expectations demanded that the study commenced expeditiously. Hence, belated registration was unavoidable. The authors confirm that all ongoing and related trials for this intervention are registered.
Results
Participant characteristics
All participants completed the program. Participants were aged between 42 and 51 years, and six of the eight participants were female (Table 4). Participants were walking strong (2/8), wobbly (4/8) or used a wheelchair (2/8). Three participants were casually employed. All participants (n=8) lived with others. Seven out of eight participants were assessed at all three time points. One participant was unable to complete final outcome measures due to ceremonial responsibilities relating to a family member who passed away, and hence their data was excluded from the pooled analysis, with the exception of step data (Fig2). Participants completed program activities alone (n=2), supported by a family member (n=5) and/or local community researcher and physiotherapist (JC) (n=3). The weekly planner was followed by participants on their phones (n=4) or on paper (n=4). Those employed participated in the Toolbox program before or after work hours. Others completed sessions either early in the morning before noon, or later in the afternoon, in the cooler periods of the day.
Table 4: Participant characteristics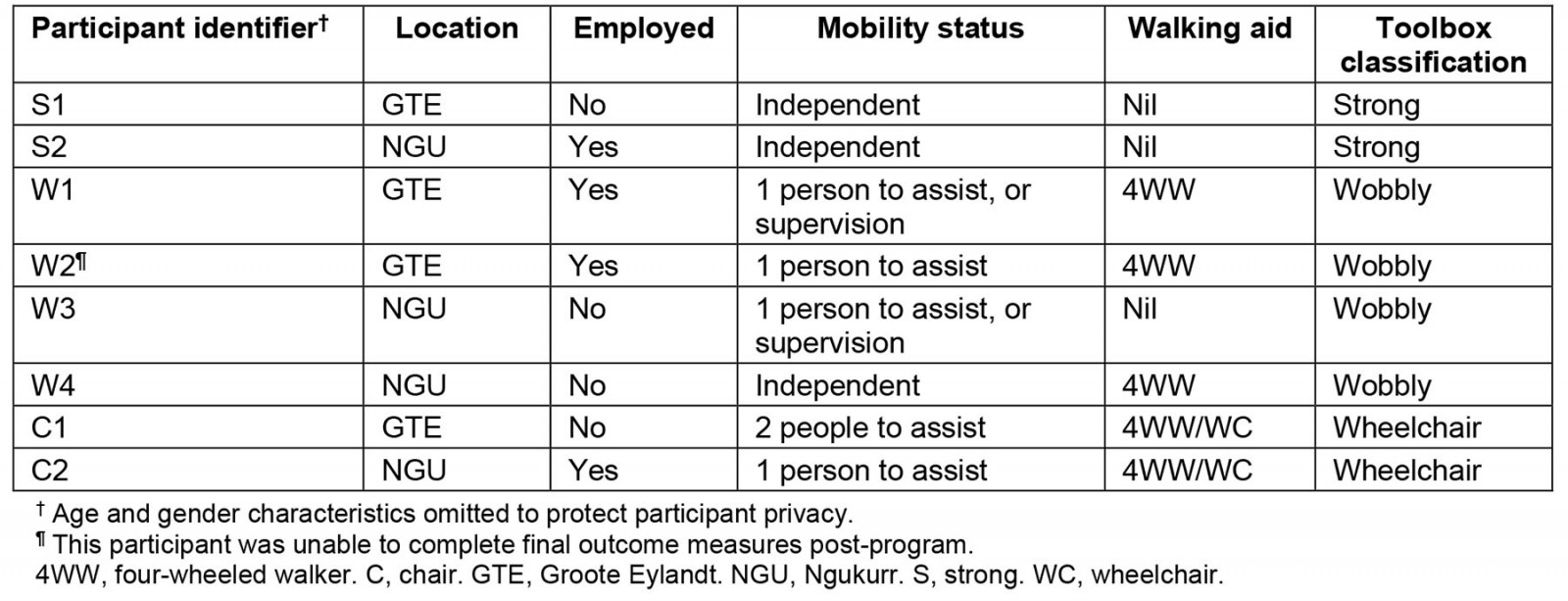
Feasibility
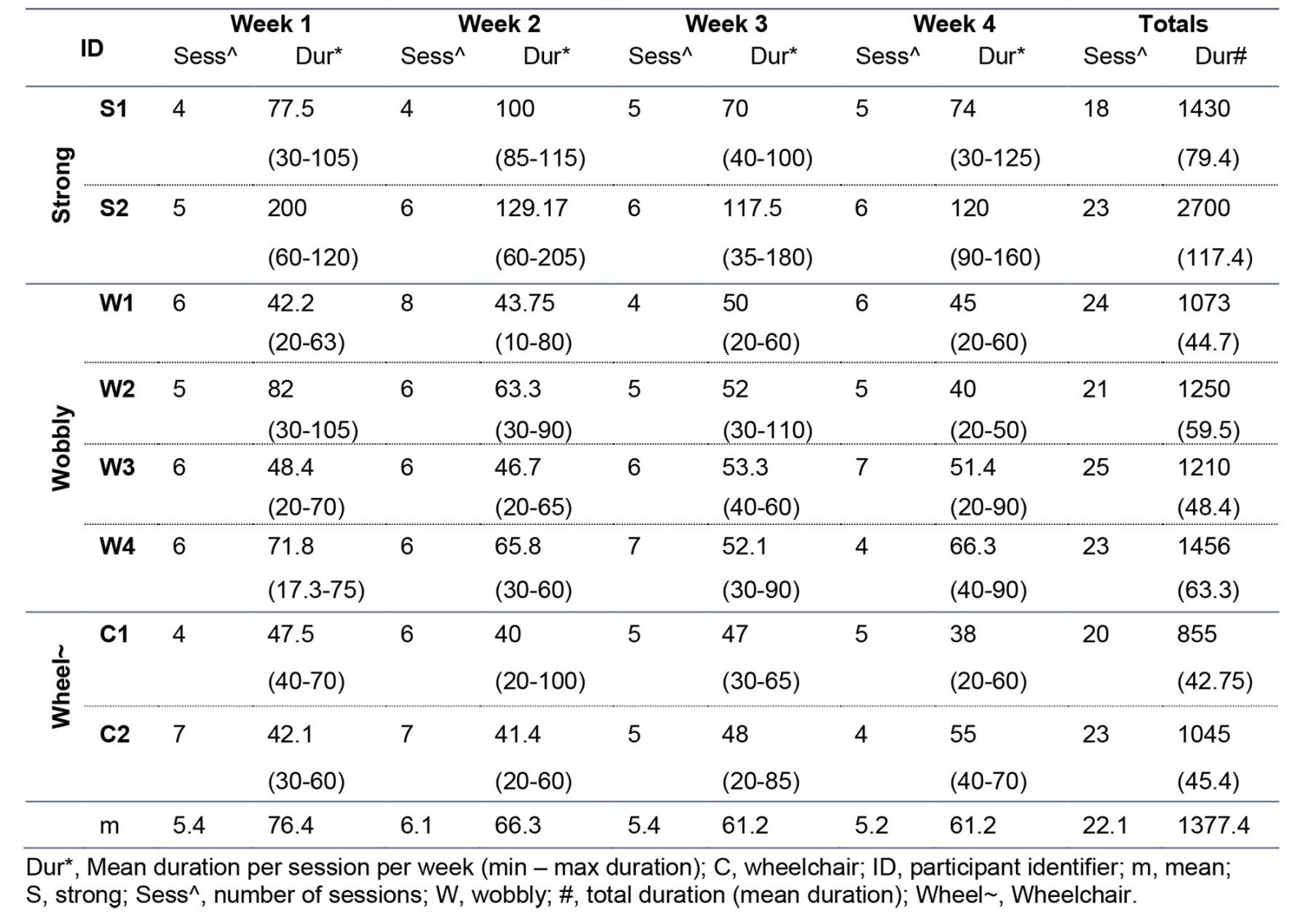
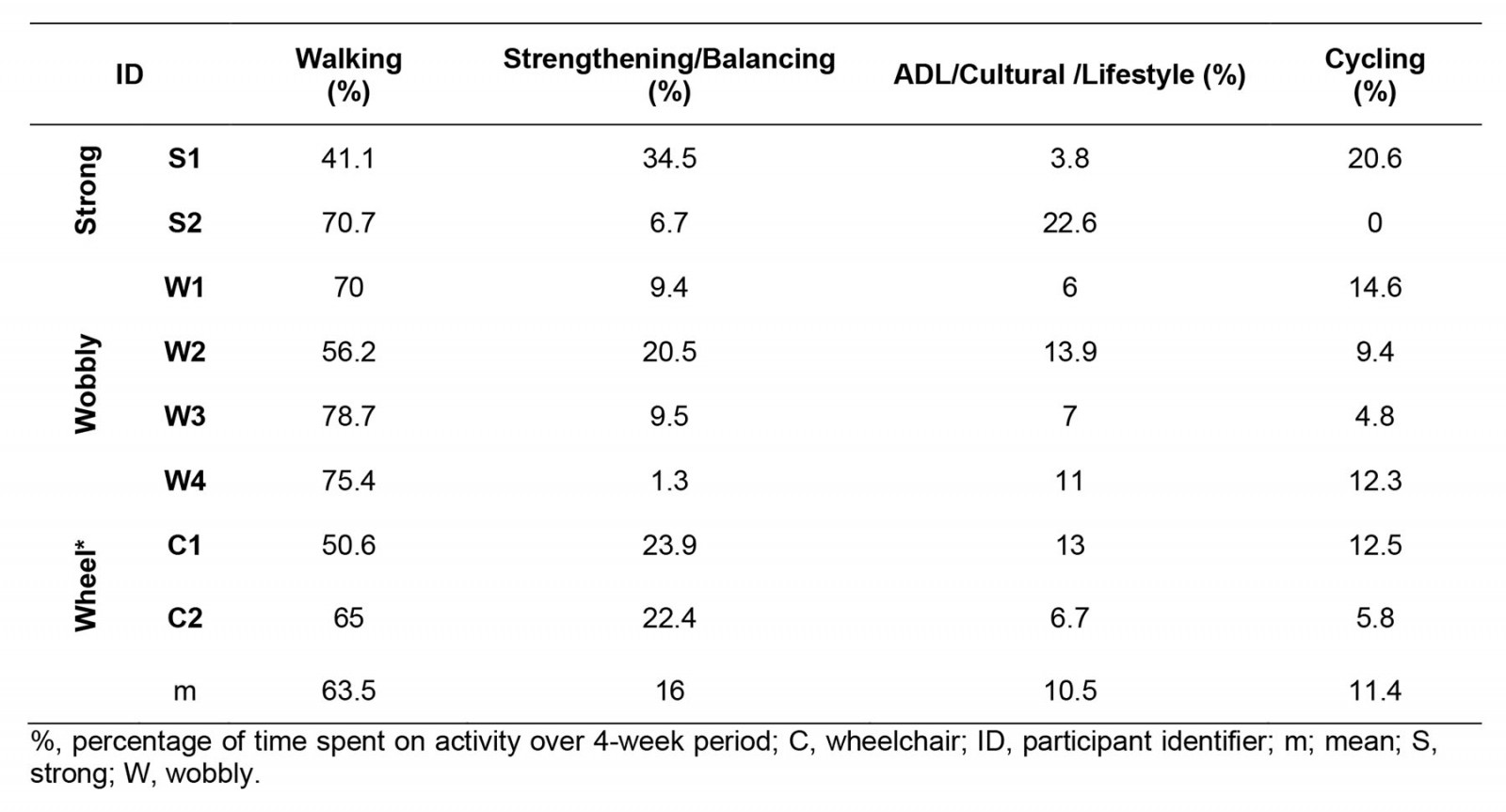
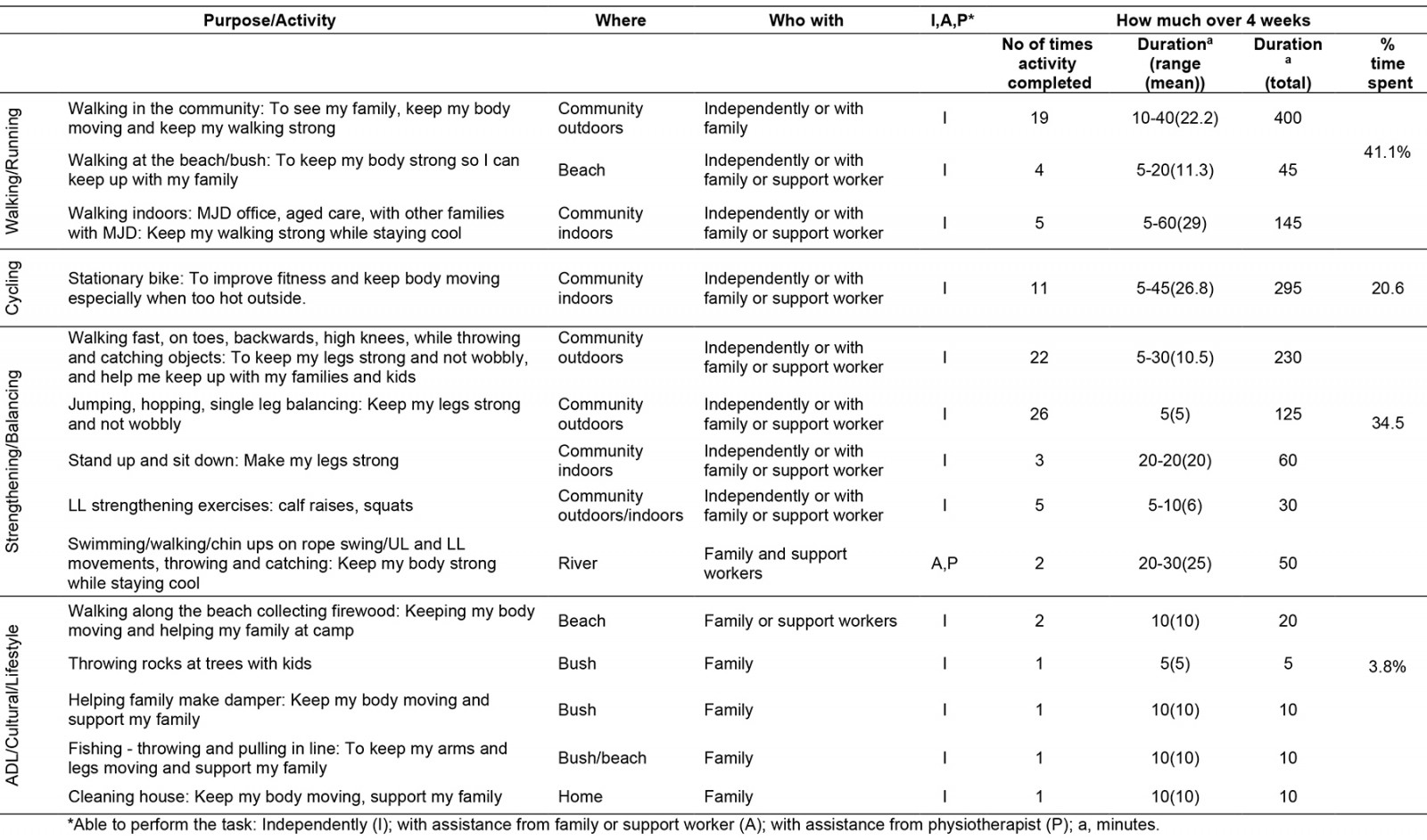
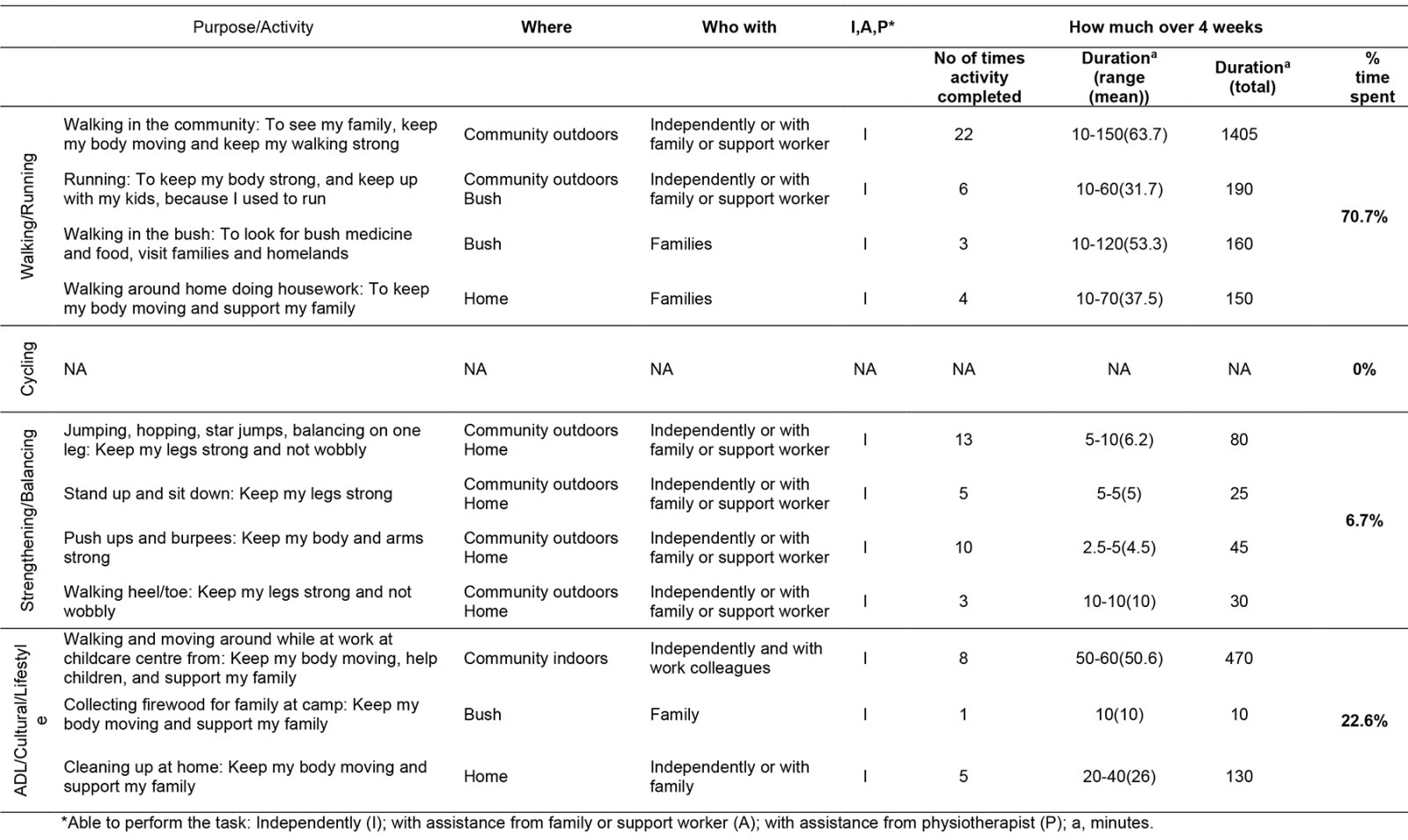
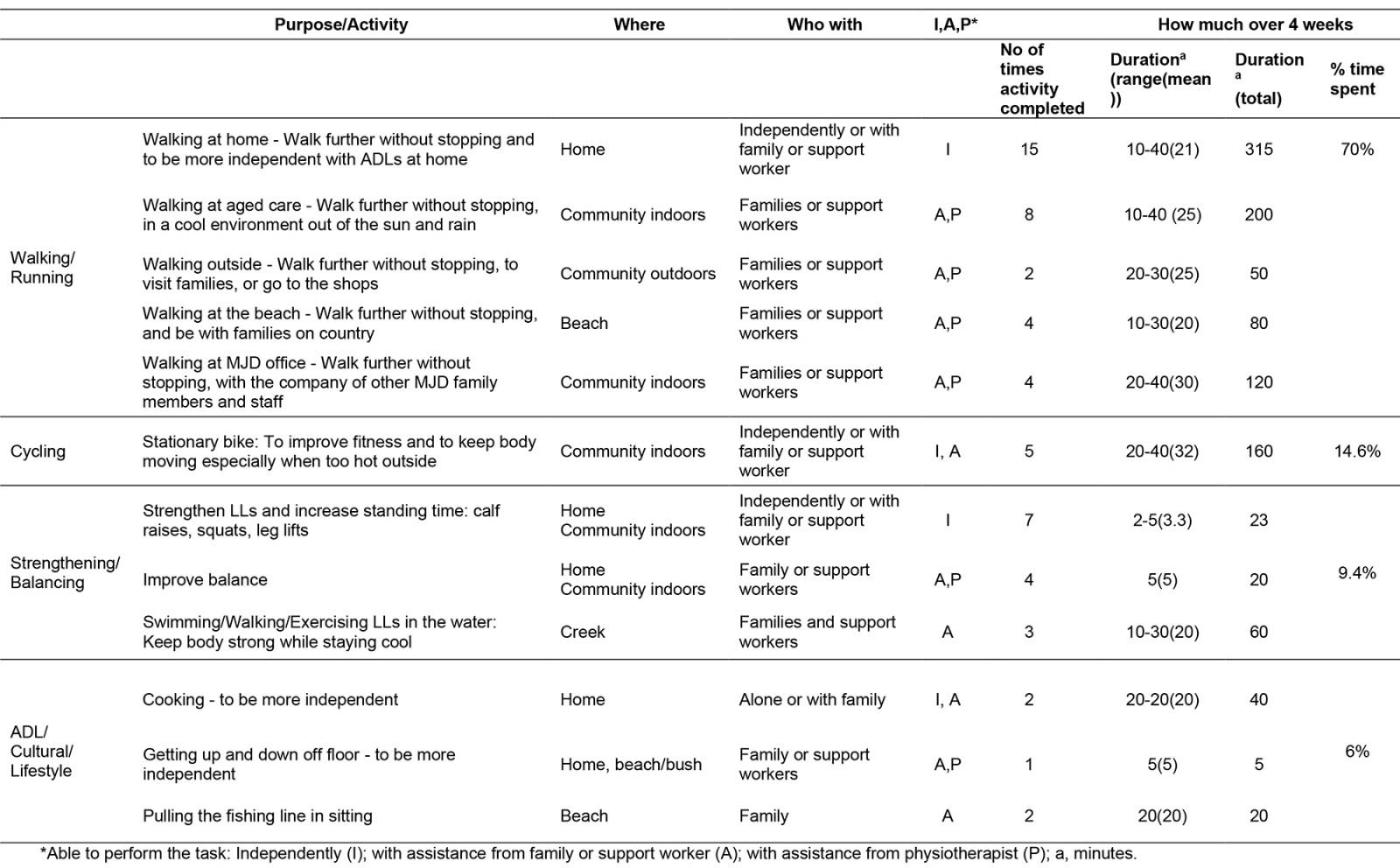
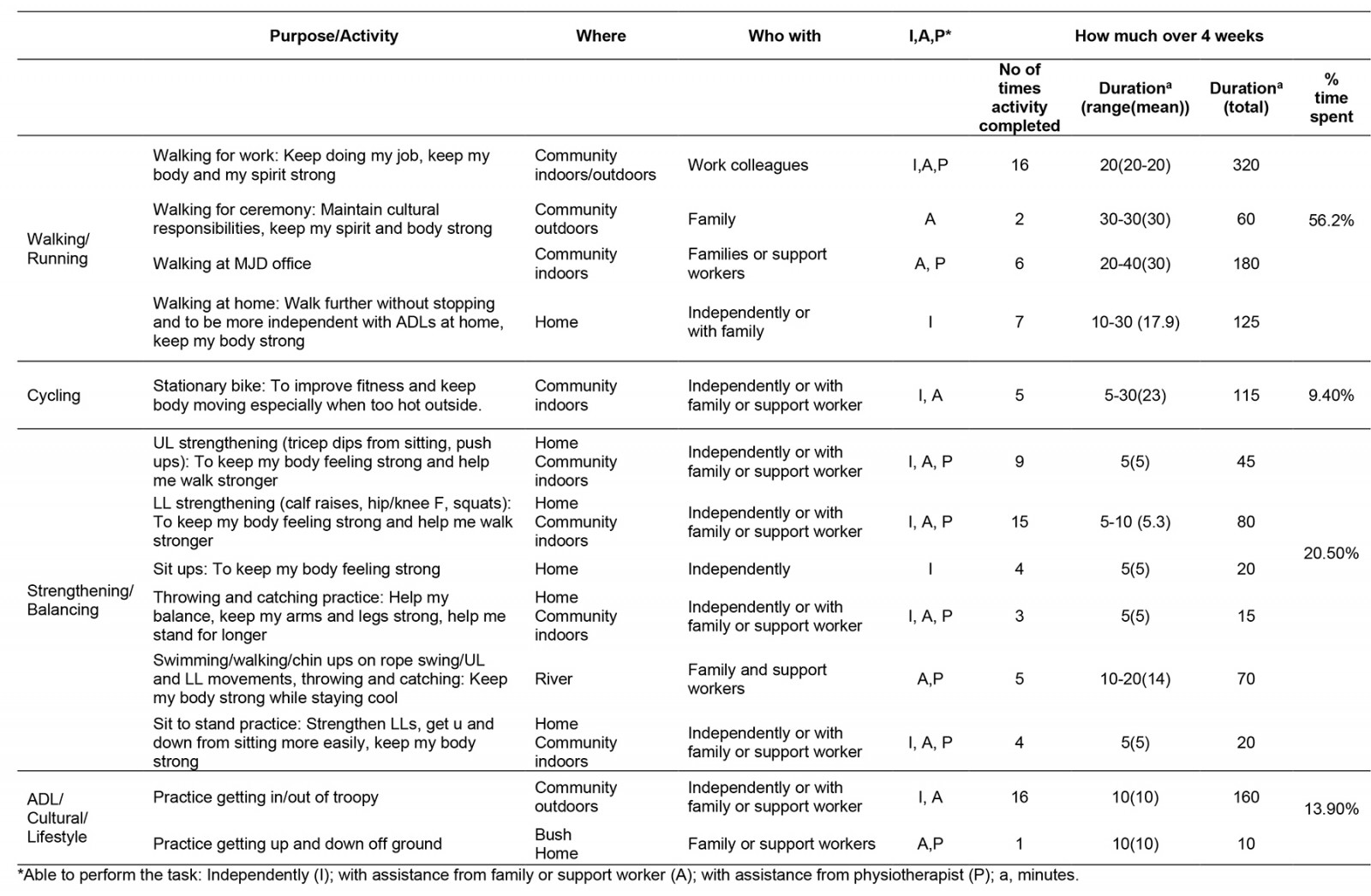
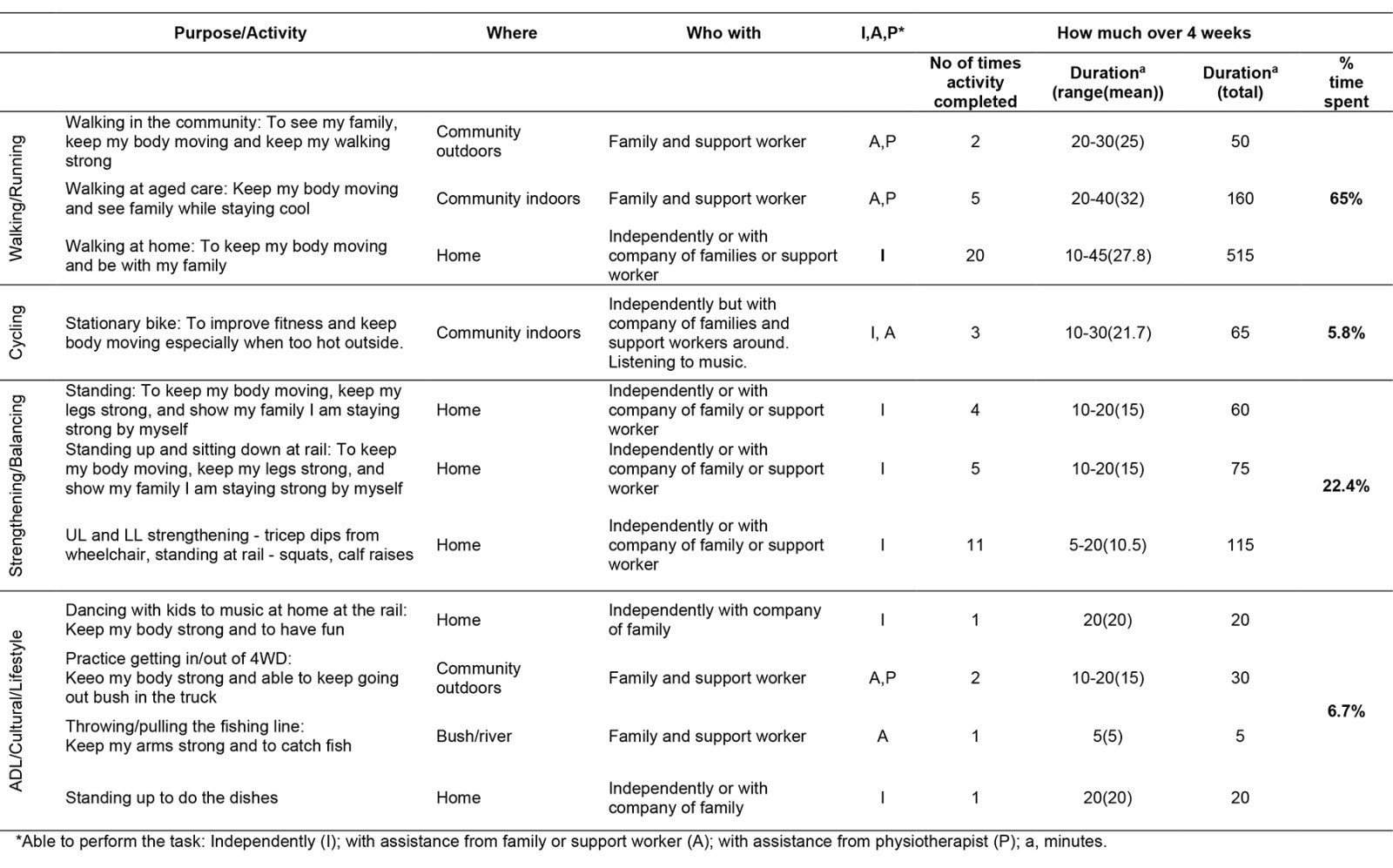
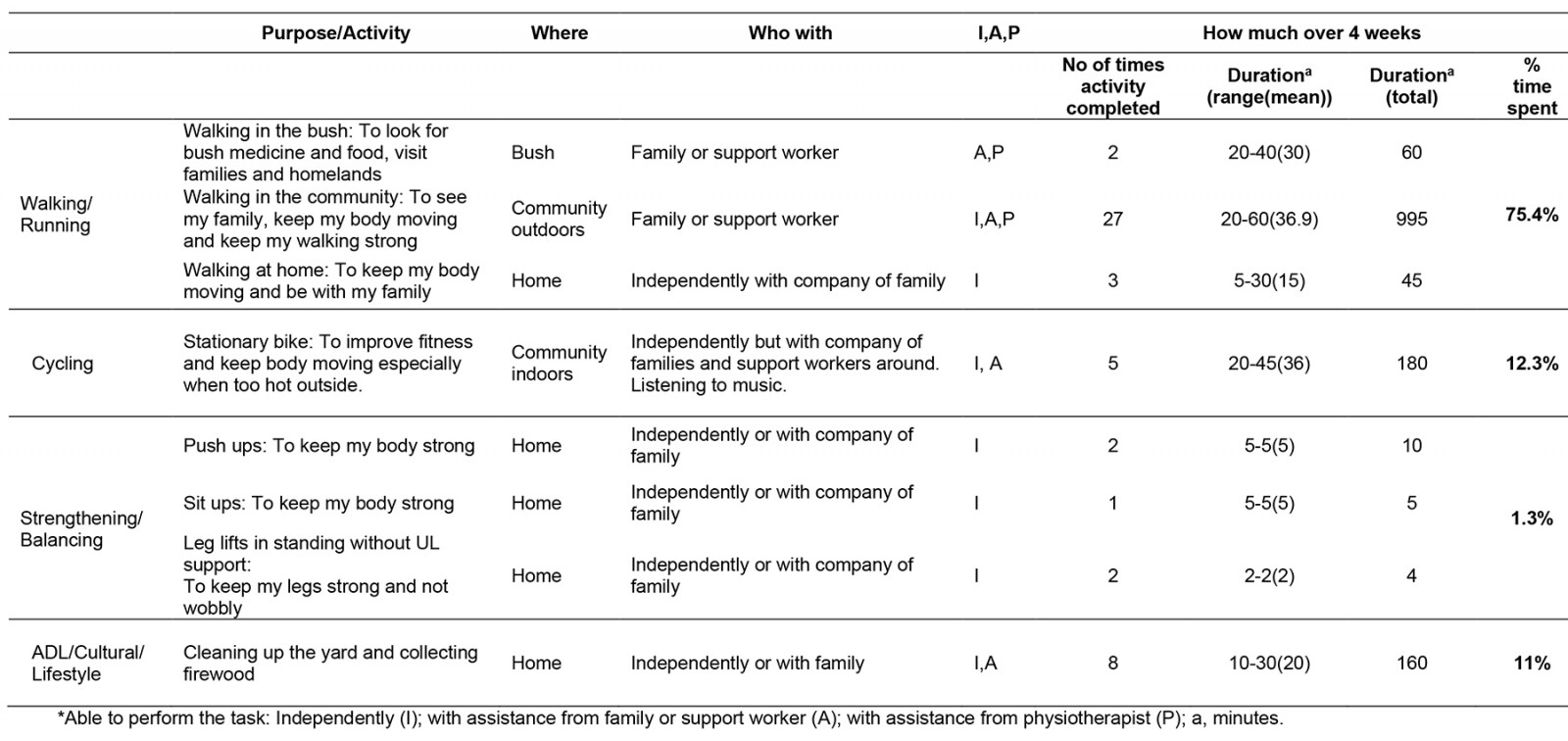
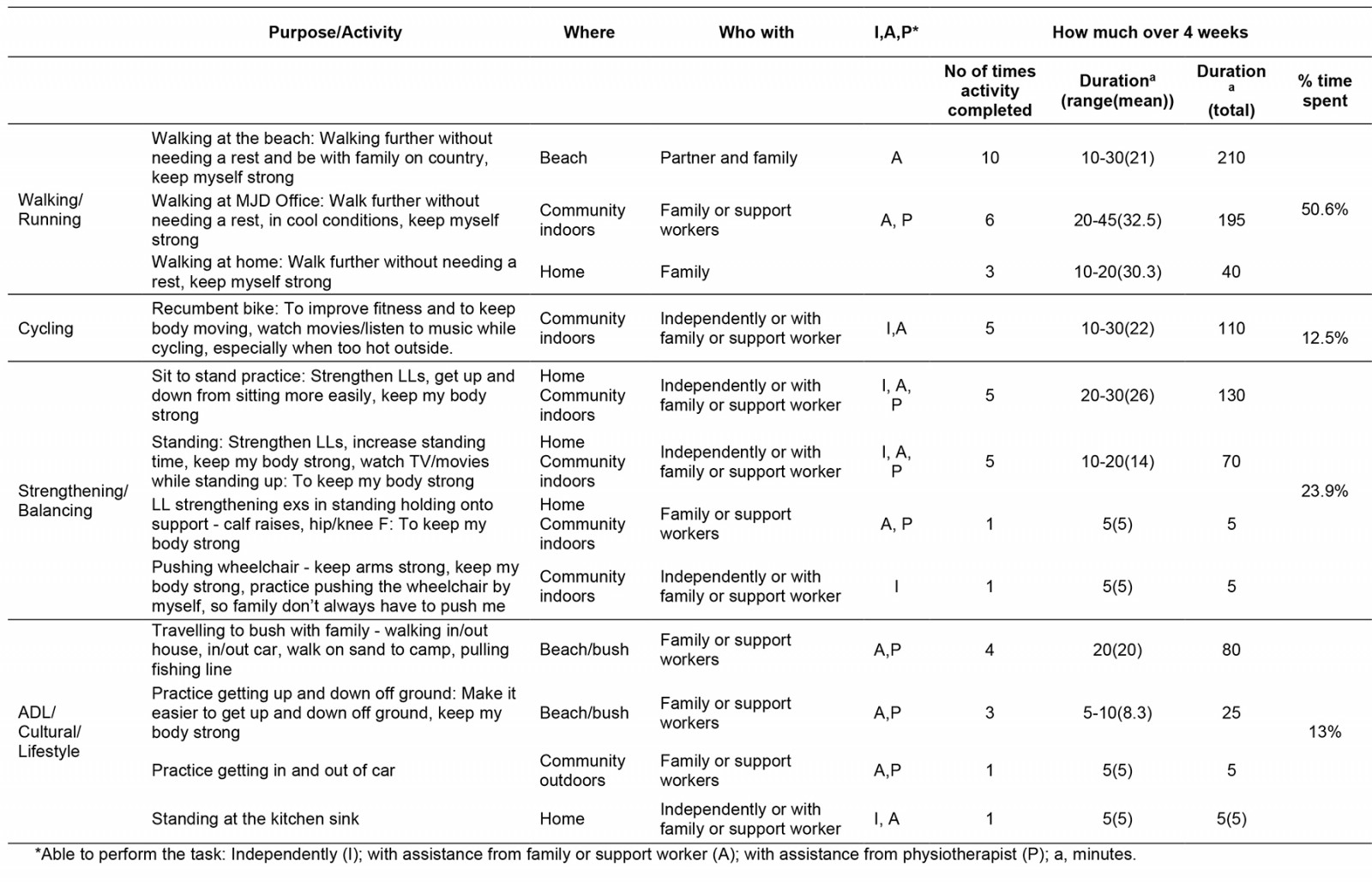
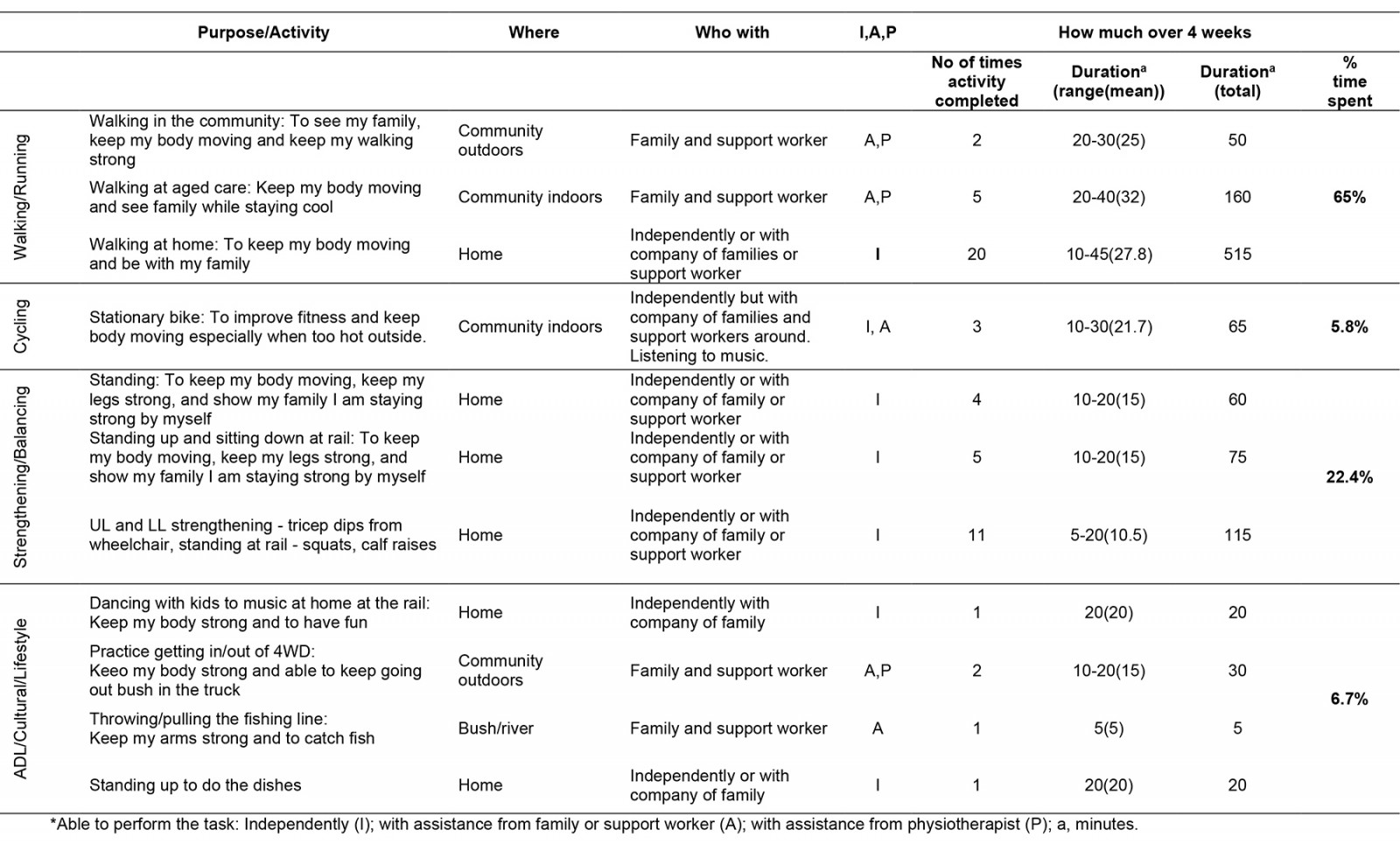
Participation and adherence: All participants met the minimum activity target (100%) (physically active three times a week, for at least 1 hour, at a ‘somewhat hard’ level of exertion, for 4 weeks). On average, participants completed five (range four to seven) sessions per week for 66 (range 35–91) minutes (Supplementary table 2). Activities were related to walking (63.5%), strengthening/balance-based activities (16%), cycling (11.4%) and activities of daily living, culture and lifestyle (10.5%) (Supplementary table 3). Specific details of activities performed by each participant are included as supporting information (Supplementary tables 4–11) and are summarised in Table 5. Activities were completed at home (33%) in the community indoors (27.2%), in the bush/at the beach (20.4%) or in the community outdoors (19.4%). Garmin Vivofit 4 activity tracker devices, well tolerated by participants, collected consistent step data and could be synced independently by all participants except one, who lost smartphone access during the program.
Table 5: Participant activity across functional levels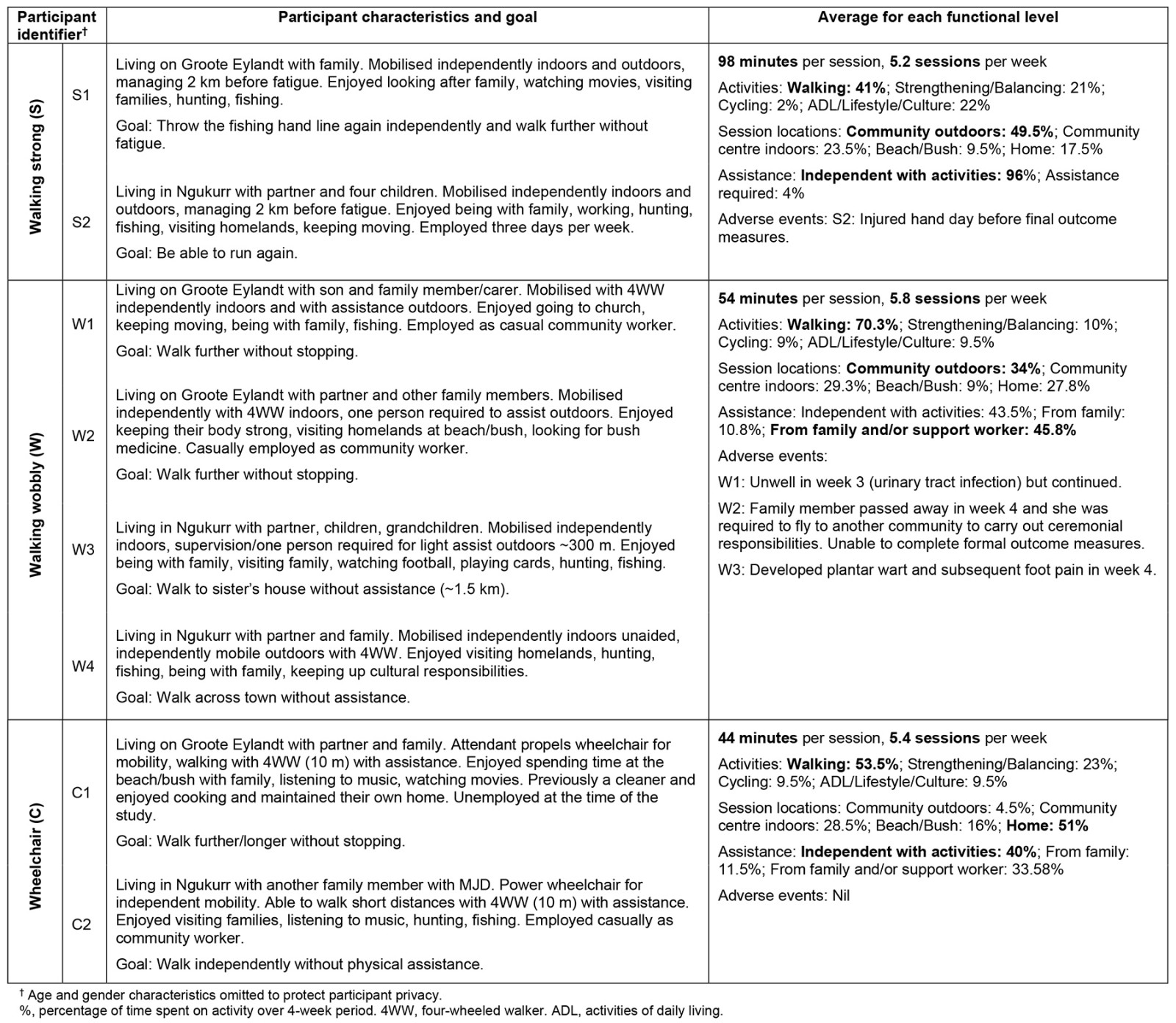
Adverse events and coinciding events: No serious adverse events occurred. One participant developed a mild infection in week 3, as did another in week 4. One participant sustained a hand injury unrelated to the program and two participants experienced stressful family events.
Coinciding events that occurred during the program included three significant ceremonial events (three funerals) with 3 days, when participants were unable to engage in program activities. A vehicle breakdown occurred, limiting travel to beach and bushland for 1 week. Heavy rainfall with flooding occurred for 3 weeks during the program on Groote Eylandt and 1.5 weeks in Ngukurr. High average temperatures and humidity prevailed (Groote Eylandt: 26–35ºC; Ngukurr: 22–34ºC), which limited outdoor training in warmer periods of the day65,66.
Program costs: Costs associated with the program included wages (community researchers only), travel, accommodation, food, refreshments and technology (Garmin Vivofit 4 activity tracker devices, digital tablets for community researchers, fuel for vehicles) (approximately $44,500). Approximate time per person contributed to the project from commencement until completion of data collection was 552 hours for researchers across project activities (community researchers combined 272.5 hours, JC 280 hours). Participants contributed 208 hours to activities throughout the project (26 hours per participant). JC resided in each community during data collection. Research team members collaborated via telephone and Zoom when unable to meet in person.
Impact
Impact for each participant on walking and moving around: Individual participant scores at all three time points are shown in Table 6.
Impact across all participants on mobility, ataxia, steps taken: Individual participant scores at all three time points are in Table 6. For all participants, results for mobility and ataxia changed significantly pre-program to post-program (6MWT, TUG, steps taken, SARA). Participants walked significantly further and faster (6MWT 58% further (range 24.5–234.5 m); TUG 36.8% faster (range –98.4 to –2.4 s)) and steps taken significantly increased, by 98% (range 2343–56 375 additional steps). Ataxia severity (SARA) reduced significantly, by 2.5 points (range 1–4 points), with a minimally clinically important reduction in ataxia reported to be 1 point in degenerative cerebellar disease67,68 (Tables 6, 7). Between baseline and pre-program, there were no significant changes in mobility and ataxia severity, suggesting functional state was stable prior to program commencement (Table 7).
Table 6: Impact – mobility, ataxia severity and steps taken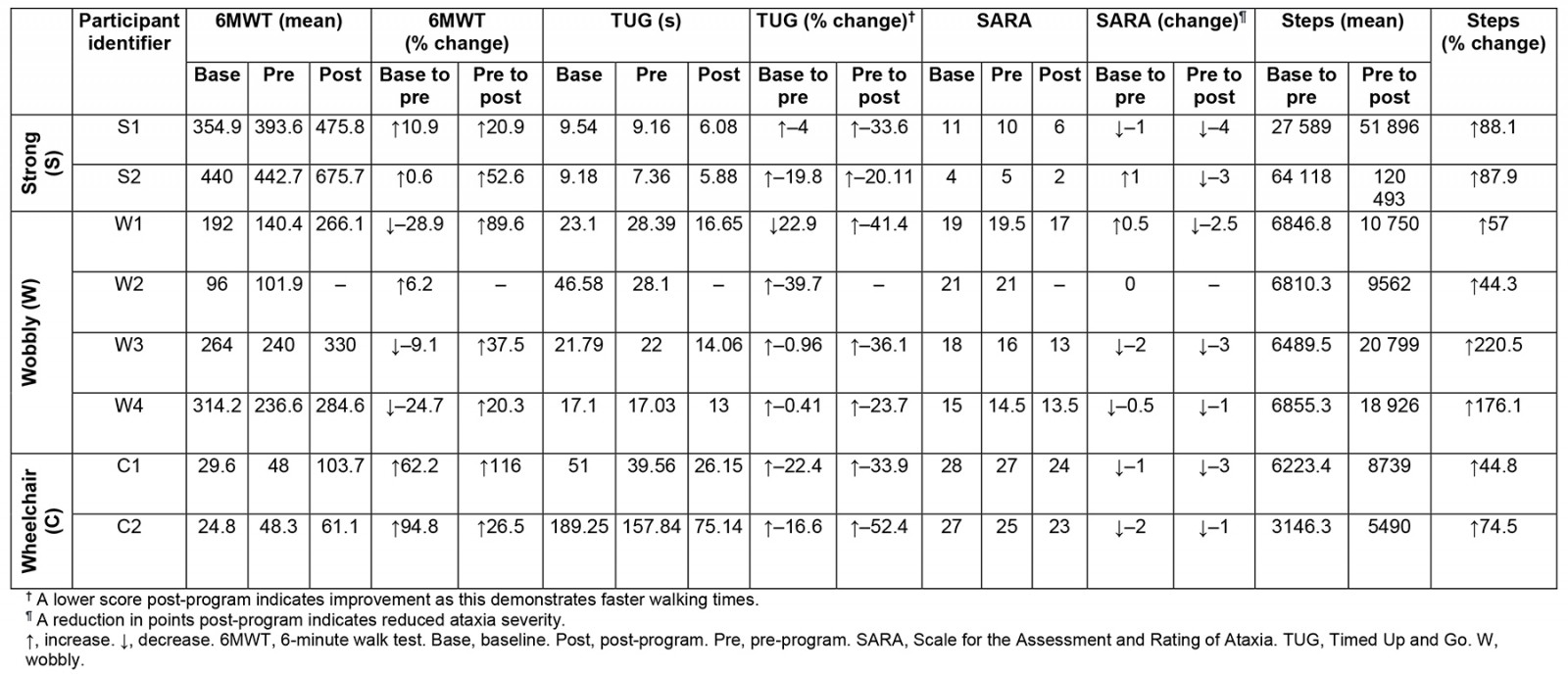
Table 7: Repeated measures analysis: mobility and ataxia severity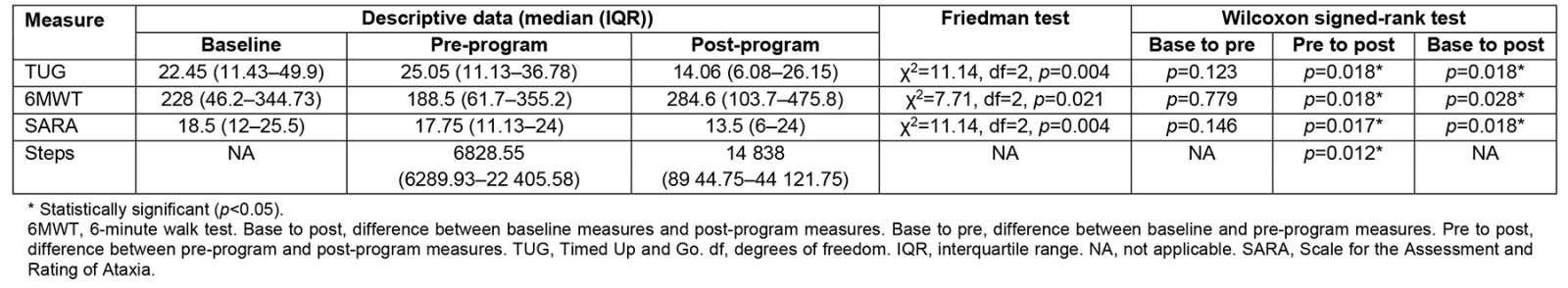
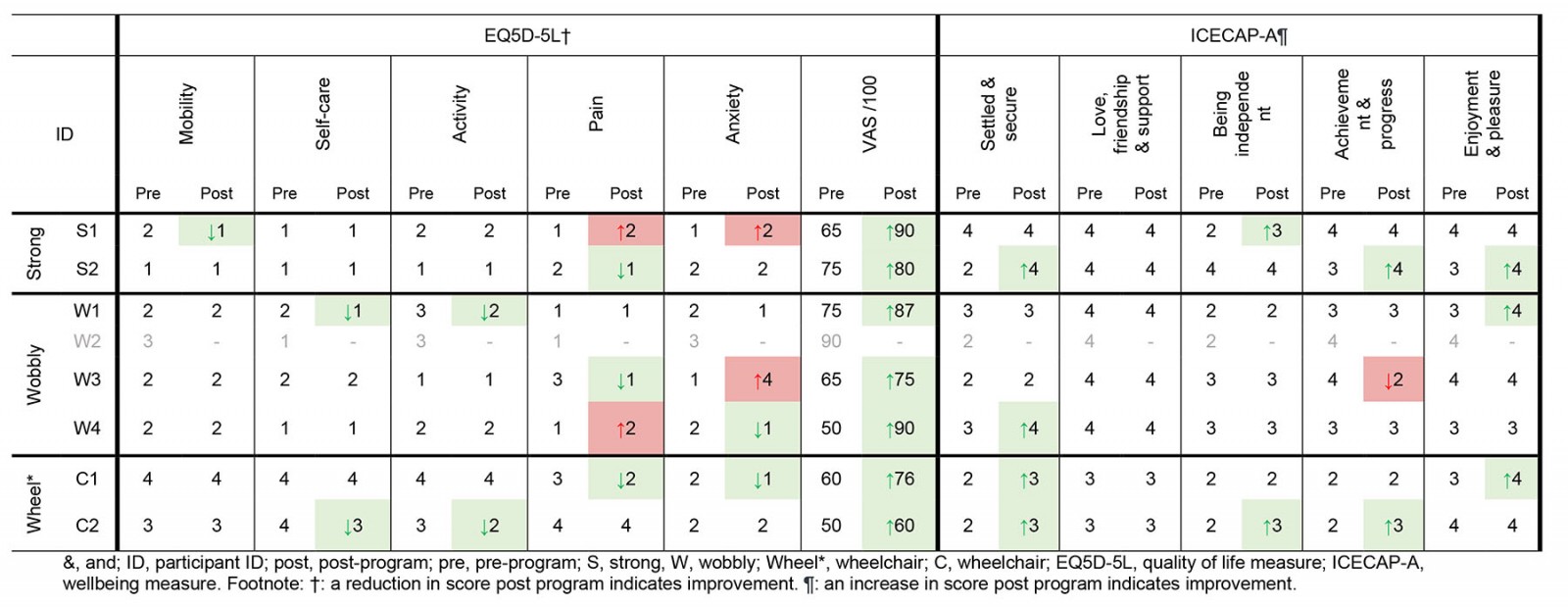
Impact across all participants on QOL, wellbeing and impression of change: There was minimal change in QOL and wellbeing. Data are included in Supplementary table 12. All participants perceived that they were ‘much improved’ (Patient Global Impression of Change score 2) after the program and all goal ratings improved 3 out of 10 points on average on the Patient Specific Functional Scale, above a minimally clinically important difference69 (Table 8).
Table 8: Goals and patient global impression of change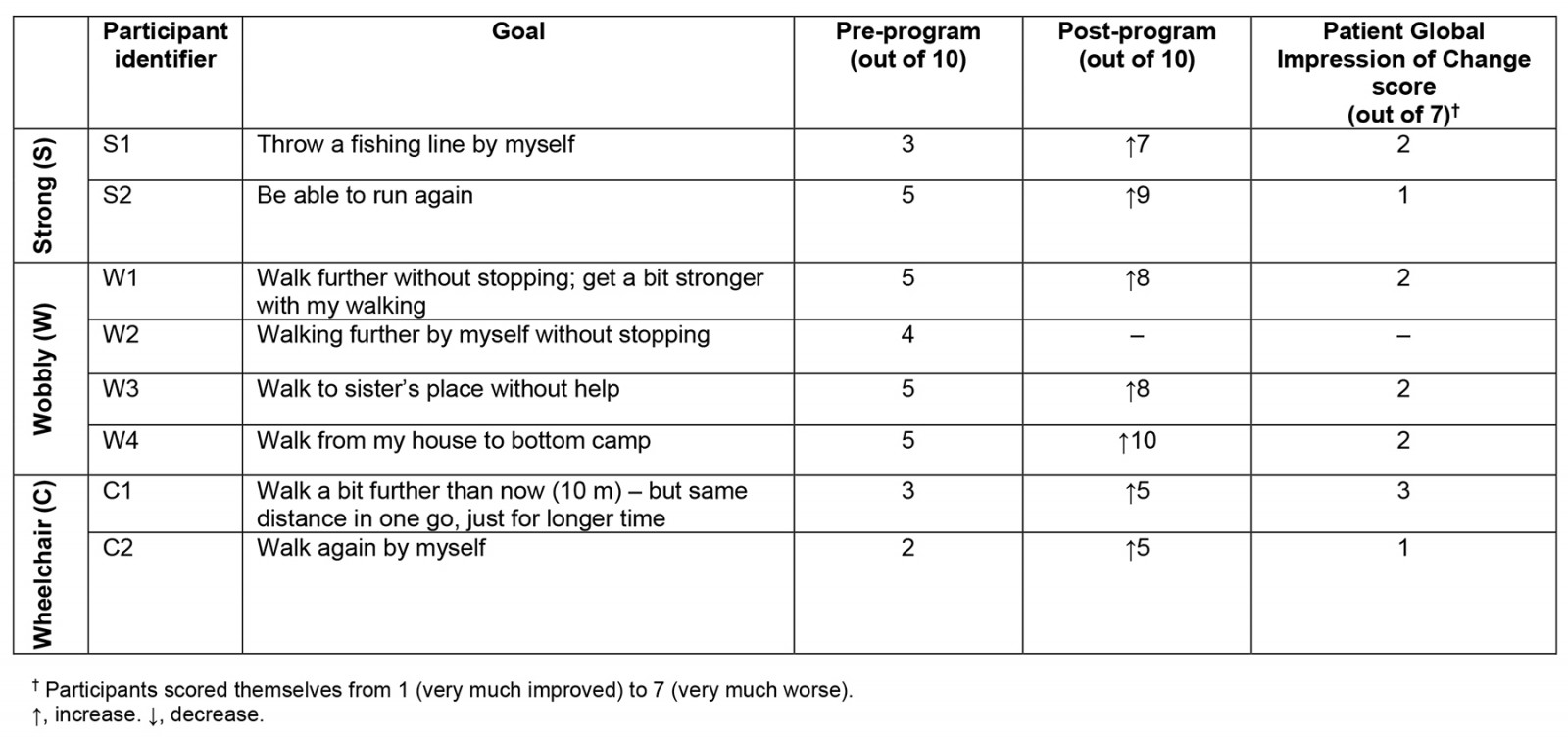
Feasibility, acceptability and impact from participants’ perspectives
All participant interviews had durations of 30 minutes to 3 hours, with one or two interviews per participant. Interview responses are summarised below, and illustrative quotes are shown in Table 9.
Table 9: Participant perspectives of Staying Strong Toolbox program: acceptability, feasibility, recommendations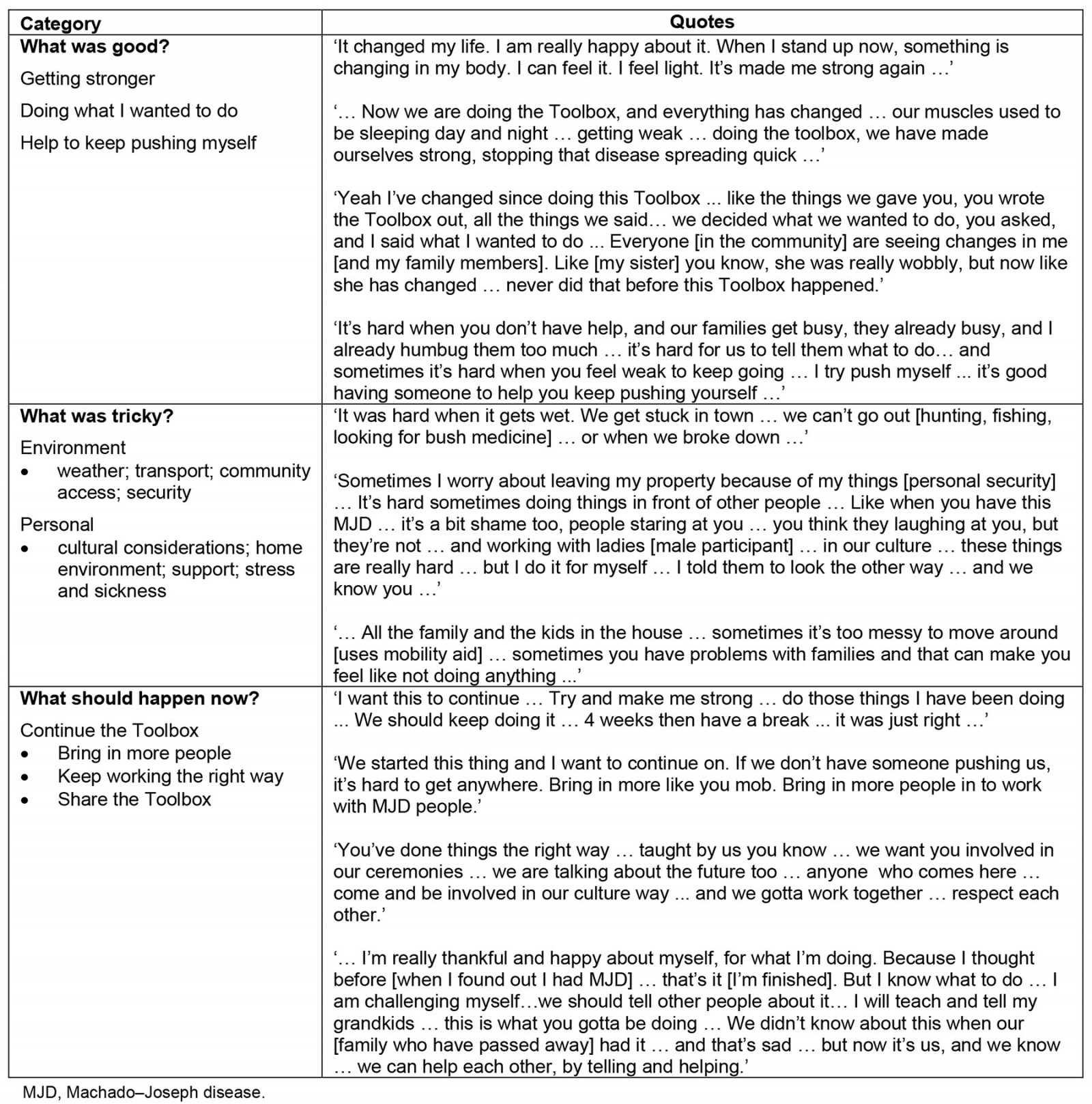
What was good?: Getting stronger inside and outside All participants wanted the Toolbox program to continue and felt they made improvements physically (improved strength, endurance, overall fitness), psychosocially and emotionally (felt happy and proud of the changes they had made) after the program. Participants enjoyed the experience, reported their bodies had changed and felt their ‘disease slowed down’. On the outside, participants felt light, strong and able to do more independently. On the inside, they expressed feeling less worried and ‘sick’, and more relaxed, happy and healthy, with some noting improvements in cramps and sleep. Participants felt 4 weeks was ‘just right’, and that a break was needed after that. Since completion of the Toolbox program, participants felt more confident doing things they thought were not possible before. Some expressed they selected activities they were initially not sure if they were capable of, but encouragement from support workers and family members offered confidence to try, and helped tasks feel achievable. Most participants remarked that family and other community members observed their improved mobility with some remarking that they ‘didn’t recognise’ them, as they were ‘looking strong’, and their body had ‘changed’.
Doing what I wanted to do Each participant felt the benefits of building a program, tailored to their needs and what they wanted to do, that offered flexibility to do what suited them and their family. They felt accountable to do the activities they selected. Many expressed the benefits of having a written plan, so they could be reminded about what they had set out do.
Having help to keep pushing myself Encouragement from family and support workers to complete the activities in the Toolbox was important, as was having the company of family members during these activities. Positive feedback and encouragement helped participants to keep going. All acknowledged difficulties of keeping going sometimes, when everyday challenges arose. While participants preferred to go to the bush or to the beach, having a place indoors to exercise provided participants more opportunities to keep pushing themselves when conditions were too hot or wet outside, when the bush or beach became inaccessible due to adverse weather, or when home was too crowded. It provided a place where participants could exercise in private but have family and/or support workers with them if they wished. Participants felt the mobility measures and watches to measure steps taken helped them to realise what was possible and gave them something to work towards.
What was challenging?: Challenges were largely those faced in everyday life for families in remote communities in the Top End. Heavy rainfall, hot and humid conditions and rough terrain limited outdoor mobility and restricted travel at times to bushland and beaches, as did car breakdowns and the need to share vehicles. Locally, participants were wary of ‘cheeky’ dogs and drivers who may not see them (the participant) walking slowly outside their home. Personal property and food security were concerns for some if they left their home unattended, while overcrowding posed a challenge for indoor mobility, impacting motivation and ability to engage in activities they wanted to do at home. Exercising in front of others in the community was a challenge managed continuously. Some worried about feeling ‘shame’, being seen moving slowly or with a walking aid around the community. Regardless, participants continued because they wanted to keep themselves strong and were confident that they would, with persistence. Having a ‘private’ place to move around, such as a community centre indoors, was helpful for many in this regard.
Receiving assistance from family members was sometimes difficult. Many family members had been long-term carers for participants with MJD across multiple generations. Having the capacity to assist with Toolbox activities, in addition to providing day-to-day care and support other family members simultaneously, was challenging. Participants and family members acknowledged the positive impact on their family of having extra help from support workers. Stress or family conflict, aches, pains and other illnesses presented continual challenges. Finally, although outcome measures for mobility were well tolerated, the SARA was least favoured as it was confronting for some because they had routinely completed the assessment over many years and observed gradual increases in their ataxia severity.
Recommendations by participants
Participants made the following recommendations:
1. Continue the Toolbox program for 4-week periods, repeated through the year, with:
- support from trained and trusted support workers
- flexible and responsive work hours.
2. Bring in more support workers, or students, and teach them the right way:
- Increase capacity for support.
- Create opportunities for one-to-one support.
- Provide ways for men to be able to work with men, and women to work with women.
3. Keep working the right way:
- Provide appropriate cultural orientation.
- Provide opportunities for support workers to learn from people in the community.
4. Share the Toolbox program:
- Share with other families with MJD and anyone interested in walking and moving around.
- Encourage others to use the Toolbox program as a framework and design their own.
- Keep testing the program to show people it is working.
Discussion
The Staying Strong Toolbox program is, to the authors’ knowledge, the first person-centred, individually tailored physical activity and lifestyle program found to be feasible, acceptable and to have a positive impact on walking and moving around for Aboriginal families with MJD. Using a mixed-methods, multiple case study design, eight participants with MJD completed the 4-week program as intended, with no serious adverse events. From a stable baseline, all participants demonstrated significant improvements in mobility and a reduction in ataxia severity. Participants’ qualitative experiences of the program were that it had a positive impact on their physical and psychosocial wellbeing.
Feasibility
The program was feasible because participants could adhere to the program, despite coinciding events, and they recommended it should continue. Factors that likely contributed to program success were that participants believed the program would help, had ownership of the program70, and had flexibility within the program that is otherwise rarely offered71,72. The short program duration likely facilitated adherence73,74. Future research to explore adherence over a longer program duration, and whether ongoing program flexibility and support could be provided sustainably, could further confirm these findings.
An indoor space for activity was beneficial and worthy of consideration in future programs. It provided a private, safe alternative when weather was poor, away from stress, with trusted support workers and family members available. The incidence of bush or beach activities was surprisingly low considering the importance of ‘going country’11, as a consequence of seasonally typical weather75 and transport difficulties. Regardless, participants exceeded activity requirements.
The program required minimal equipment, could be completed almost anywhere and did not require continuous specialist therapist input, with activities predominantly related to walking or aerobic training. The program did require specialised knowledge of local lands, families and languages, held by community workers/researchers76,77. Future programs could be facilitated by suitable local community workers, but the existing burden of care on individuals needs to be considered, as many provide daily care to family members with MJD or have MJD themselves. In such circumstances, community-accepted Aboriginal or non-Aboriginal support workers to work alongside local community workers could offer relief and support participants to keep ‘pushing’ themselves11. Supervised training has been found effective for individuals with hereditary ataxia68,78-80.
Impact
The program reduced the impact of MJD on physical function despite differences in functional level, goals and activities. A constant was that each participant tailored their program to their own needs, with support from the physiotherapist and community researchers as needed81,82. This reinforces the benefits of individually tailored, lifestyle-orientated physical activity83, relevant for families with MJD who live in remote areas, lacking services, facilities or specialised support6,11. These programs utilise the surrounding environment, foster inclusiveness in communities and require little equipment or specialist services84,85. Many individuals travel long distances to access periods of intensive rehabilitation. While impact of the program was positive, an economic evaluation to compare the Toolbox to the use of distant rehabilitation services is required in future research.
Predominantly walking or aerobic-type training brought significant increases in activity levels that exceeded WHO recommendations (150 minutes of moderate-intensity activity spread throughout each week, in bouts of at least 10 minutes)86. Ataxia severity reduced 2.5 points on average, higher than the minimally clinically important difference67,68 and well below the annual estimated average increase in ataxia severity of 1.1–1.3 points87-90. Whether changes occurred at a cellular level is beyond the scope of this study14. However, similar improvements have been reported after aerobic training for those with hereditary ataxia, having been found to be potentially more beneficial than balance training68,91. Hence, aerobic-type lifestyle activity may allow individuals to remain ‘fit enough’ to manage their deficits and delay disease progression91,92. The overall health benefits cannot be ignored, with higher chronic disease rates for those with a disability, particularly in rural and remote areas71,93. The impact of activity on wellbeing is equally important, given MJD has the highest rates of suicidal ideation across SCAs13,94.
Participants felt stronger on the inside as well as outside, which is incongruent with quantitative QOL and wellbeing measures. Measures likely lacked relevance or sensitivity to Aboriginal families in the Top End within their own culture, language and concepts of QOL and wellbeing95. A variety of QOL measures have been used in SCA research but few have drawn significant findings13. Responsiveness, validity and reliability of the EQ-5D, ICECAP-A and other questionnaires are yet to be determined96. While further work is required to develop valid QOL measures to assist with economic evaluations, participant perspectives can contribute meaningfully to describing program impact97.
Strengths and limitations
Findings cannot be generalised to families with ataxia elsewhere, but the Toolbox could be adapted for their use. The sample was small and heterogenous, and the design allowed program flexibility and inclusion of participants across all functional levels. Data collected over the baseline period, as well as after the program, enabled participants to act as their own control. Potential assessor bias was reduced with external assessment of video recorded measures98. Bias may have occurred because participants developed the Toolbox program and because interviews were conducted by the research team who facilitated the program99. Although the risk of bias cannot be eliminated in this type of study, the co-design process strengthened program feasibility and aligned with ethical guidelines for research engaging Aboriginal families100. Research team members were female but were accepted by family members to lead the research due to their knowledge and strong relationships with families101.
Garmin Vivofit 4 activity tracker devices likely had inaccuracies for slower walkers and those using mobility aids102, but were accepted by participants and survived environmental challenges, and participants kept the devices for use after completion of the study. Introduction of the devices may have raised enthusiasm among participants and increased activity before program commencement103, but no significant differences were found on measures between baseline and pre-program. While physical outcome measures detected consistently positive changes, all are yet to be validated for use among Aboriginal families with MJD71. Follow-up assessments were not possible within study constraints, although other research has demonstrated similar improvements in ataxia and fitness 3 months post-training91.
Implications for practice
The Staying Strong Toolbox program is feasible to keep Aboriginal families with MJD in the Top End walking and moving around by staying strong on the inside and outside. Research to evaluate the program in repeated blocks, with a follow-up period, would be valuable. Program implementation would increase support worker opportunities for involvement. This would enhance the capacity of those working with individuals with ataxia and provide greater opportunities for culturally appropriate support (eg men working with men, women working with women). The Toolbox workbook and program could be adapted for families with MJD in other locations within Australia and internationally.
Conclusion
We explored feasibility, acceptability and impact of a physical activity and lifestyle program, the Staying Strong Toolbox program, for Aboriginal families with MJD in northern Australia. The 4-week, person-centred program was feasible and acceptable to families involved. Additionally, the program had a positive impact on walking and moving around for individuals with MJD. Participants recommended continued implementation of the program, which could be adapted for use by families with MJD elsewhere. Research to explore the impact of physical activity and lifestyle interventions for others with MJD in a way that is culturally acceptable is required.
Acknowledgements
The authors sincerely thank Aboriginal families of Groote Eylandt and Ngukurr who generously welcomed the researchers to their country and trusted them to share their story with the rest of the world. The authors acknowledge the Traditional Owners of these lands, and Elders past, present and emerging. The authors gratefully acknowledge Mario Naritjarruwa Faggion, Bakala Wurramara and Ayangkidarrba-langwa Media for their generous support with linguistics and film production, and the MJD Foundation, for their ongoing support of this research.
Funding
The in-kind support provided by the MJD Foundation and Anindilyakwa Land Council provided funds for flights and accommodation for JC for part of the study. GL received salary from MJD Foundation. This study received funding support from the Lowitja Institute Aboriginal and Torres Strait Islander Health CRC (Lowitja Institute Cooperative Research Centre (CRC)) (Grant ID: 017-SF-005). JL received salary from the Lowitja Institute CRC. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Conflicts of interest
Community research partners JL, GL, GwL, BD are employees of the MJD Foundation. This does not alter adherence to Rural and Remote Health journal policies on sharing data and materials.
References
Supplementary material is available on the live site https://www.rrh.org.au/journal/article/8376/#supplementary
You might also be interested in:
2020 - Evaluating a centralised cancer support centre in the remote region of Northern Norway
2013 - Core clerkship in internal medicine at a rural community hospital in Israel
2006 - Leaving the land: An exploratory study of retirement for a small group of Australian men



 Supplementary figure 1: Study flow timeline
Supplementary figure 1: Study flow timeline