Introduction
More than 270 000 pregnant women have been infected with COVID-19 in the Americas, and the virus has killed more than 2600 pregnant women1. In Mexico and Colombia, COVID-19 was the leading cause of maternal deaths in 20211. A similar fate could soon befall Guatemala, as COVID-19 cases are rising, causing concern because only 10% of the population is currently vaccinated1. Warning that COVID-19 represents a serious risk for pregnant women in Latin America and the Caribbean, Pan American Health Organization Director Carissa F. Etienne urged countries in the Americas to prioritize vaccines for expectant and lactating mothers1.
Meanwhile, the Pan American Health Organization stated that 40% of countries in the region have reported disruptions in maternal and newborn services amid the pandemic1. In Guatemala, rural and Indigenous Mayan populations, which are considered marginalized because they disproportionately suffer poor health outcomes, among other disadvantages2-5, are at greater risk from COVID-193. The Peten, in particular, is among the most remote regions of Guatemala. No roads were built until 1990 in the area, which is the seat of the Mayan Empire. The department, similar to a state, is the largest department in the country. Nearly 62% of Peten residents live in poverty, 13% live in extreme poverty, and 60–70% lack access to basic health care6.
Guatemalan lay midwives are well-respected community leaders in a country that lacks the institutional capacity to keep pace with healthcare needs related to birth, newborns, and COVID-193,7-9. Thus, Guatemalan lay midwives, who attend the majority of births in their country and who attend most births at home10-14, are in an optimal position to offer frontline support to pregnant women and newborns regarding COVID-19, particularly in the remote Peten.
In 2018, a total of 23 320 lay midwives were registered with the Ministry of Health (MOH)15. Lay midwives are mostly low-literacy Indigenous Mayans who are apprentice trained10-13. Licensing for lay midwives was introduced in 19357, and government training programs have been offered for lay midwives since 19559, but the training programs have not resulted in improved infant and mortality rates, partially because they are taught in Spanish with written material14,15. Practicing midwifery is illegal without attending the government training programs7. In exchange for attending the training programs, lay midwives are supposed to get a stamp to sign birth certificates, a backpack with birth supplies, and a birth log, but some lay midwives reported they have not received the stamps, backpack or birth log. In addition, the MOH is supposed to offer monthly educational sessions; however, these do not occur consistently occur throughout the country16 and were not offered during the pandemic.
As in many parts of the world, misconceptions about COVID-19 and the vaccine are rampant in Guatemala. Registered nurses (RNs) stated anecdotally that pregnant women fear going to hospital because they think they will contract the virus there. In addition, pregnant women think the vaccine will cause a miscarriage or fetal anomalies. Pregnant women with COVID-19 also believe the virus passes through breast milk, so they are not breastfeeding their newborns, which is particularly dangerous as unclean water, which potentially is used for formula, is the leading cause of death worldwide17.
Further, one study related to COVID-19 in Guatemala showed 94% of pregnant women were not vaccinated compared to 6% who were vaccinated. In addition, 30% of pregnant women feared adverse effects from the vaccine, 26% were not sure the vaccine was safe, and 13% were not sure the vaccine was effective18.
Given these misconceptions, RNs from the MOH asked the primary investigator (PI), who is an associate professor at the University of Utah College of Nursing, to offer culturally relevant educational sessions about COVID-19, which are the intervention for this program of study, to low-literacy lay midwives in the Peten. The PI speaks Spanish and has maintained a program of study with Guatemala lay midwives, the MOH, and the non-profit organization Refuge International since 2009. The educational sessions were culturally relevant because they were translated into the language of participants, and were offered orally with role plays, teach backs, repetition, and stories for the low-literacy audience, as opposed to the government training programs, which are didactic, rely on written material, and are taught in Spanish.
Methods
RNs from the MOH informed lay midwives about the educational sessions, and arranged the dates, times, and 11 locations for the educational sessions. Ten of the educational sessions were held in healthcare clinics, schools, and community centers throughout the Peten, and one was held at a Refuge International healthcare clinic in Sarstun, in the department of Izabal, which shares a border with the Peten and Belize.
The PI, who is a doctor of nursing practice, certified nurse midwife, and women’s health nurse practitioner, did her original program of study in Sarstun with lay midwives, who are Kek Chi. The PI has maintained a relationship with these lay midwives as Sarstun faces some of the worst health outcomes in Guatemala.
All of the COVID educational sessions were held in locations that were accessible for the lay midwives, who traveled on foot, in the back of pickup trucks, and by tuk tuk, bus, horse, boat, and canoe. All locations had covered buildings that were open to the air and had seats where the lay midwives could rest.
When lay midwives arrived at the educational sessions, the purpose of the program of study was explained, and all questions were asked. Information was provided in Spanish and translated into Indigenous dialects. Lay midwives were advised that the COVID education would not be withheld if they chose not to participate in the study; that willingness to complete the demographic data sheet, pretest and post-test served as consent for study participation; and that they were free to leave at any time. Any participant who identified as a midwife and spoke Spanish or Indigenous dialects was invited to participate. The PI also gave her business card to all participants in case they had follow-up questions after the educational sessions.
After the introduction, lay midwives filled out demographic data sheets and a pretest regarding COVID-19 (see Box 1 and Appendix I). Data were collected face to face on paper forms. The study team, which included MOH RNs and bilingual volunteer nurses from Madre y Niño, helped low-literacy lay midwives fill out the forms. Madre y Niño is a non-profit organization the PI and other nurses founded to support lay midwives and improve health outcomes in the Peten.
The pretest (and post-test) included 12 questions with a total of 24 correct answers. Three questions had four correct answers and one question had two correct answers. Seven questions were fill-in-the-blank and had only one correct answer per question. Three questions had yes or no answers that could be circled.
The PI developed the demographic data sheet, pretest, and post-test based on a literature review about Guatemalan lay midwives and COVID-19. A judge panel of three experts established face validity of the tools and a Fog Index of 0.35. The Fog Index measures the readability of the writing sample. The resulting score is an approximation of the number of years of formal education required to understand the tool on first reading. In other words, participants with less than a year of formal education should understand the questions on the demographic profile and the questionnaires.
After filling out the initial paperwork, all lay midwives agreed to participate in focus groups to share the lived experience of responding to COVID-19 in their country, which will be reported elsewhere. Madeline Leininger’s theory of culture care diversity and universality promotes the importance of taking in information from inside the culture, or emic knowledge, before imparting information from outside the culture, or etic knowledge19. The PI employed an action research format where she designed her program of study based on information lay midwives shared20.
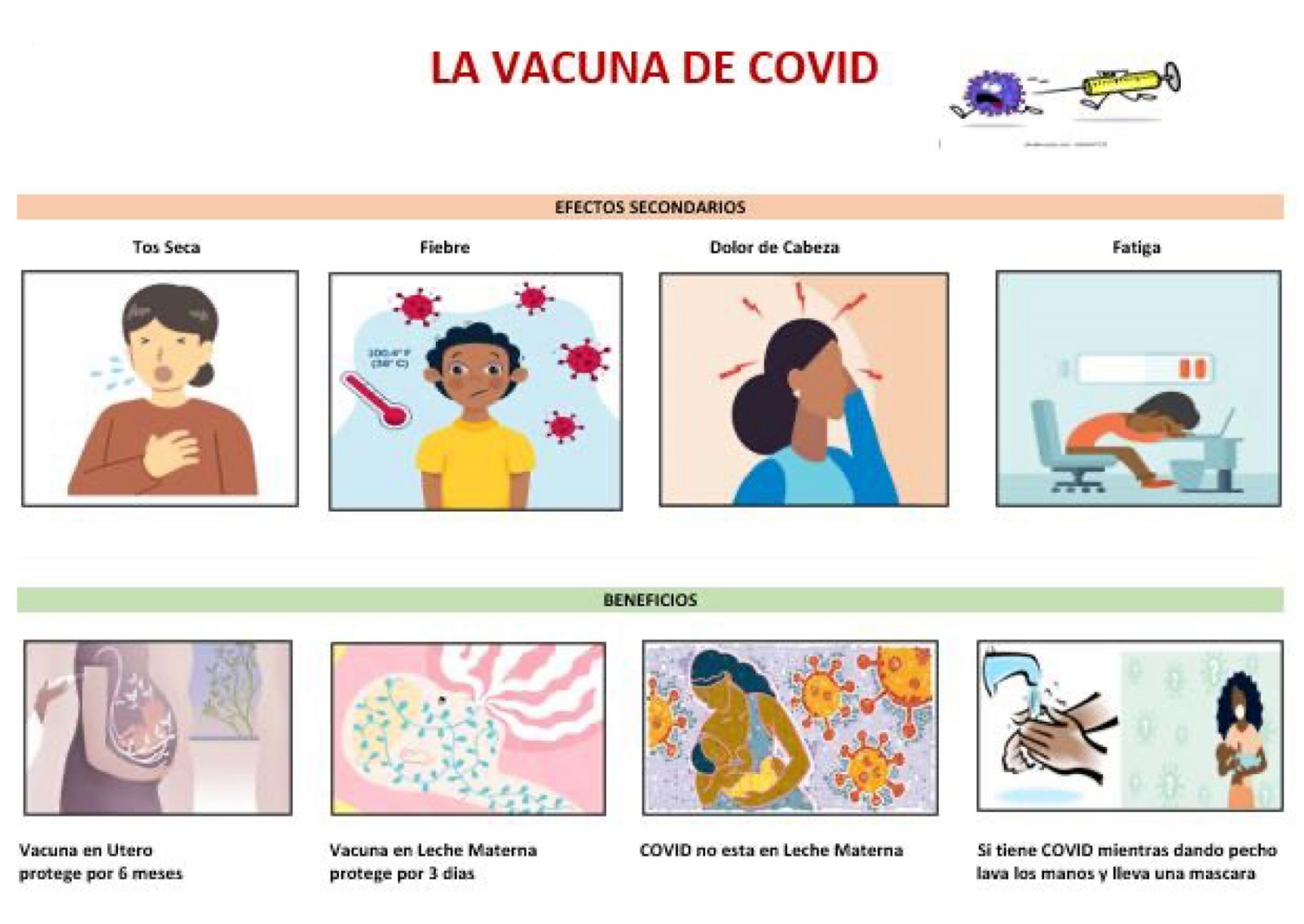
After the focus group, evidence-based educational activities about COVID-19 were offered orally in the native language of participants. Information was provided about the risks of the virus to the mother, fetus, and newborn, appropriate responses, which patients are most vulnerable to the virus, benefits and side-effects of the vaccine, timing of the vaccine, and how the virus interacts with breastfeeding. Activities included repetition, role plays, and storytelling. Lay midwives also were given laminated COVID reminder cards (Appendix II) with culturally relevant drawings of the information that was shared to encourage knowledge retention.
Past literature has reported that low-literacy audiences learn best from activities, such as storytelling, repetition, and role plays21. In addition, lay midwives understand simple color pictures from inside their culture better than complex black and white drawings from outside their culture22. Thus, the COVID reminder cards were culturally relevant and designed to increase the visual literacy of low-literacy participants.
After the educational activities, lay midwives took the post-test, again with assistance if necessary. All questionnaires, including the demographic data sheet, the pretest and post-test, were completed; thus, no forms were discarded. To thank them for their participation, lay midwives were given a meal, travel stipend, and birthing kit that included a fetoscope, towels, soap, iodine, scissors, razor blades, umbilical cord tape and clamps, plastic exam gloves, and disposable bed sheeting to put under patients.
Box 1: Educational activity about COVID-1923.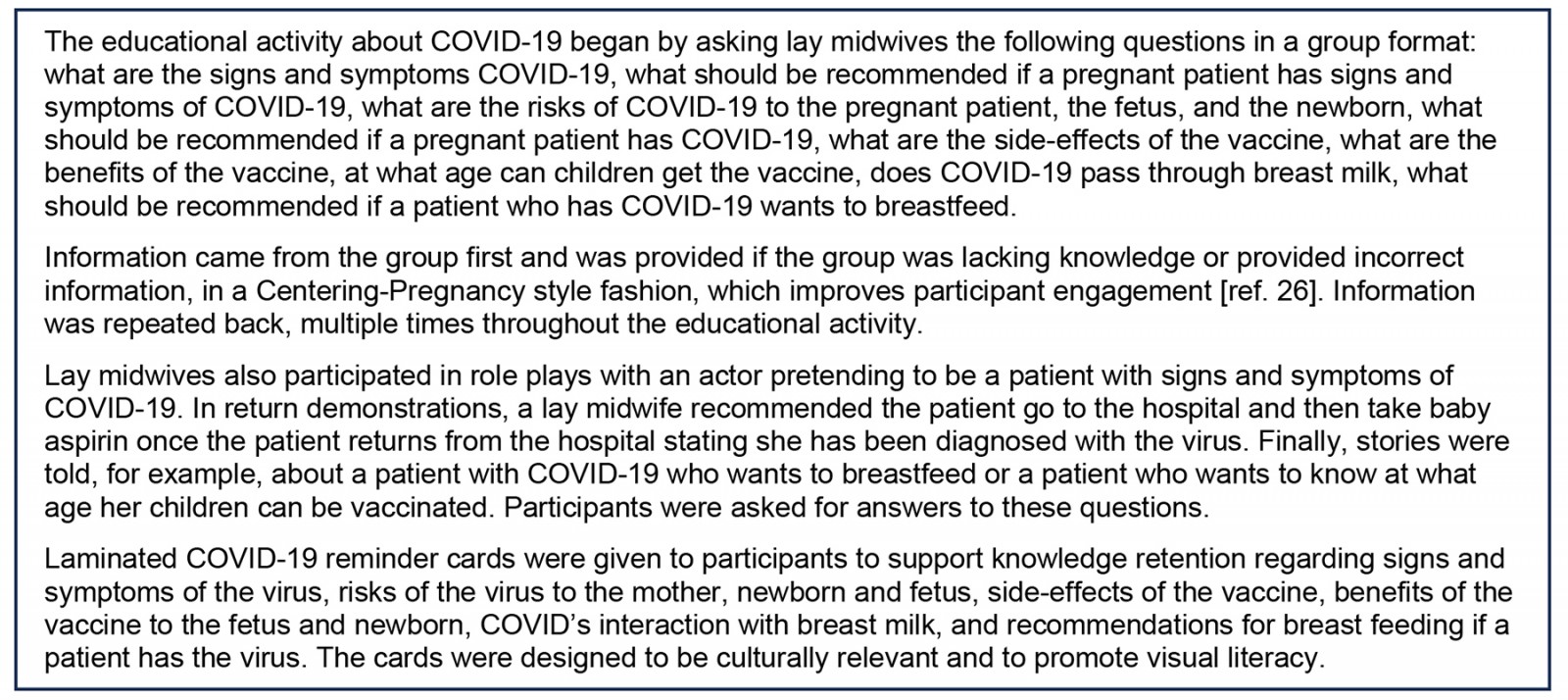
Data analysis
The evaluation relied on frequencies and measures of central tendency to analyze demographic data. Scores on the pretest and post-tests were based on the total number of correct answers from a questionnaire about COVID-19.
Ethics approval
An internal review board from the University of Utah (IRB 00154808) approved the program of study, which also met all nine of the global health competencies and skills from the American College of Nurse Midwives.
Results
Table 1 displays demographic information. Most (98%) participants were female (206) and 2% (4) were male. The age range of participants was 21–85 years with an average of 61 years. The primary language of 74% (155) of participants was Spanish, and 26% (55) spoke Indigenous dialects, such as Mam, Quiche, Kaqchikel, and Kek Chi. All Sarstun participants spoke Kek Chi.
Experience as a lay midwife ranged from 1 to 65 years with an average of 27 years. Formal education ranged from none to 7 years with an average of 1.75 years. Nearly 46% (97) of participants had no schooling. Further, 52% (109) of participants were literate, 32% (67) were illiterate, and 16% (34) could count but not read or write.
Nearly 77% (162) of participants reported they had not had COVID-19 and 33% (48) stated they had contracted the virus. Of the 48 participants who contracted COVID-19, 6% (3) went to the hospital, 75% (36) were sick at home, and 19% (9) weren’t sick. Meanwhile, 79% (165) of participants had been vaccinated and 21% (45) had not received the vaccine. Questions were not asked about how many vaccines participants received and whether participants who contracted COVID had symptoms of long COVID.
Lay midwives reported the following estimates regarding their patients’ vaccine status: 25% (52) stated a majority of their patients had received the vaccine, 27% (57) said more than 90% of their patients had received the vaccine, 18% (38) said less than 10% of their patients had received the vaccine, 21% (45) said a minority of their patients had received the vaccine, and 9% (18) stated they were unaware if their patients had received the vaccine.
Besides providing information about the vaccine, participants showed a significant increase in knowledge scores (possible 0–24) from prescores: 7.09 (standard deviation (SD)=3.06) to 15.20 (SD=4.61) (Student’s t-test p<0.001). The question that performed the best was related to what a lay midwife should do if a patient has symptoms of COVID-19. Nearly 93% of participants answered correctly on the pretest and 94% on the post-test that a patient with symptoms of COVID-19 should be sent to the hospital.
Also performing well was a question about symptoms of COVID-19. On the pretest, 15% of participants could not identify any symptoms of COVID-19. The remaining 85% knew at least one of the four symptoms, including dry cough, fever, difficulty breathing, and chills, including 4% of participants who identified all four symptoms of COVID-19. By comparison, on the post-test 1.4% of participants could not identify any symptoms of COVID-19 and 98.6% could identify at least one of the four symptoms, including 30% who identified all four symptoms of COVID-19.
Questions that performed the worst were related to breastfeeding and low-dose aspirin. A significantly higher proportion of participants mistakenly thought COVID-19 passed through breast milk on the pretest (70.1%) compared to the post-test (8.4%) (McNemar test, p<0.001). Regarding breastfeeding, 12.6% of participants knew on the pretest that women with COVID-19 who breastfeed should wear a mask and wash their hands compared to 74.3% of participants who knew these recommendations on the post-test (Wilcoxon signed-rank test, p<0.001). Finally, 2% of participants knew on the pretest that pregnant women with COVID-19 should take a low-dose aspirin compared to 67% of participants on the post-test (χ² (1)=194.7, p<001) (Table 2)
Table 1: Demographic data, n=210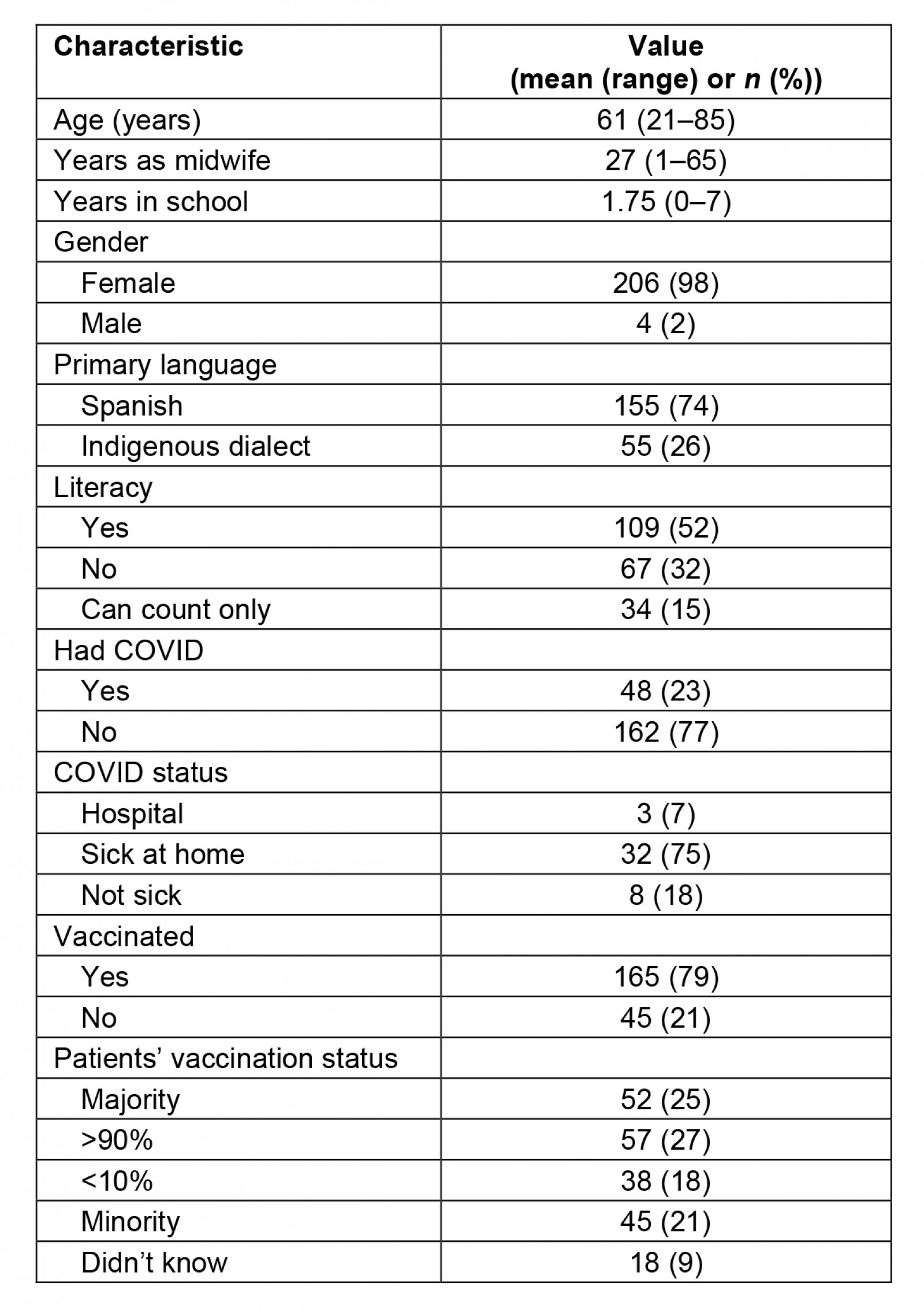
Table 2: Participant knowledge scores pretest and post-test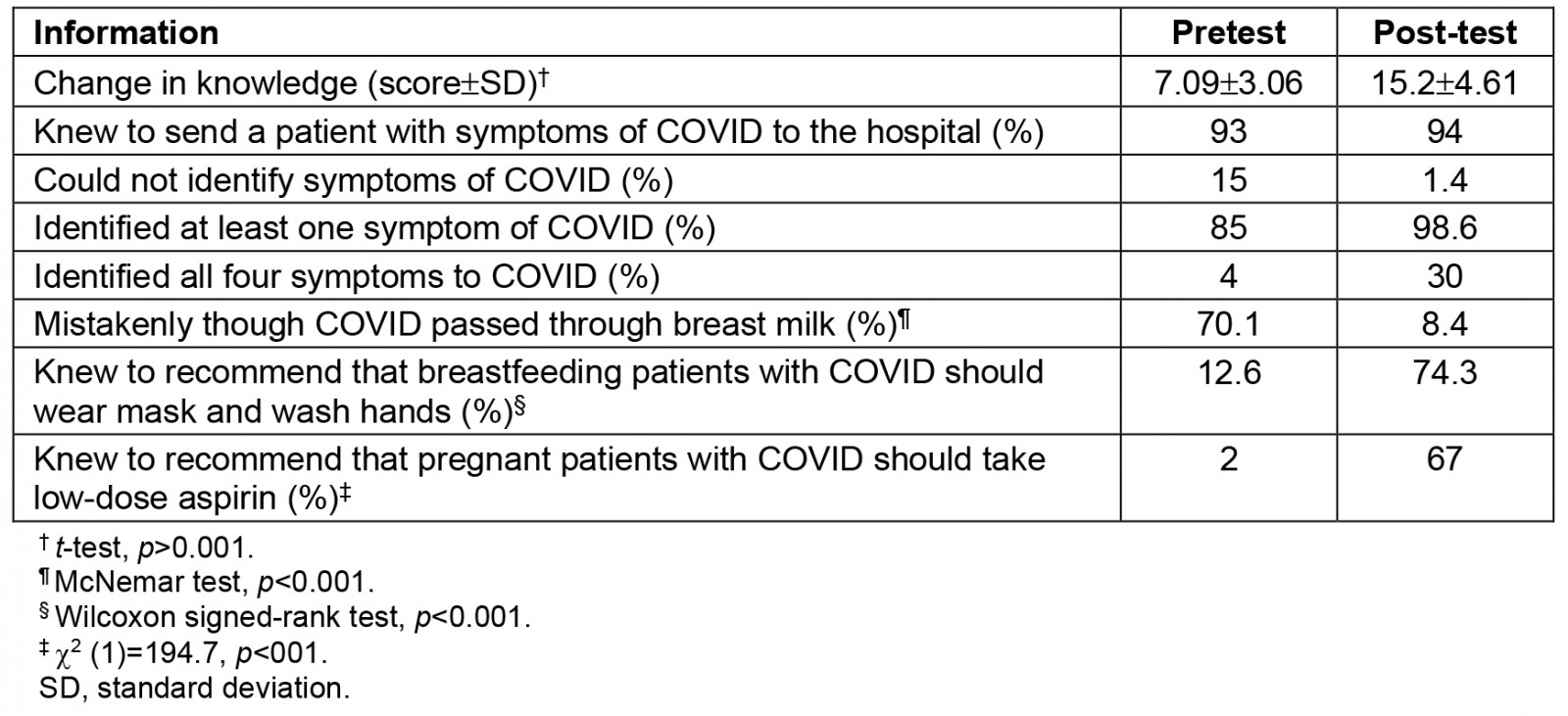
Discussion
Lay midwives who are well-respected community leaders had many misconceptions about COVID-19 and the vaccine. The biggest misconception before the educational sessions was that the virus passes through breast milk. Lay midwives were advising patients with COVID-19 not to breastfeed, which could be particularly harmful in a developing nation where unclean water may be used in bottles for formula feeding. In addition, lay midwives were not aware before the educational sessions that they should recommend patients wear a mask and wash their hands when breastfeeding.
Lay midwives also were not aware that they should recommend that patients with COVID-19 take a low-dose aspirin because of its anti-inflammatory properties. The Guatemalan government forbids lay midwives from giving patients medications, but patients can buy low-dose aspirin over the counter, particularly if their trusted lay midwife suggests this course of action.
Data participants shared about their experience with COVID-19 suggested more Guatemalan women are vaccinated than previously reported in the literature. Naquvi et al reported 94% of pregnant women in Guatemala were not vaccinated18. Lay midwives in this program of study reported 73% of pregnant women were vaccinated and the majority of their patients were vaccinated, which may be a result of social desirability bias.
A power dynamic is evident among lay midwives, who are more likely to be low-literacy, uneducated, and Indigenous, and MOH RNs who are more likely to be literate, educated, and Ladino. Further, lay midwives must answer to MOH RNs if questions arise about a lay midwife’s practice.
Conclusion
There is a paucity of data in the literature regarding the effect of COVID-19, particularly in developing nations, such as Guatemala. The pandemic is still fresh in terms of the turnaround time for publishing results after conducting a program of study. More information is needed about misconceptions patients might still harbor about the virus and the vaccine, even as COVID-19 wanes.
Culturally relevant information about COVID-19 and the vaccine presented orally in the native language of lay midwives dispelled myths and changed knowledge among these essential providers in the developing world. Similar educational sessions should be provided in other parts of the developing world to protect vulnerable populations, such as mothers and newborns, from global pandemics.
Our hope is lay midwives will pass on the new knowledge they gained about COVID-19 to their patients. Our plan is to retest lay midwives about COVID-19 a year after the initial teaching to evaluate knowledge retention. Future studies should also follow up with participants to inquire if the new knowledge resulted in practice changes.
Funding
This program of study was funded by an intramural grant from the University of Utah College of Nursing and the American College of Nurse Midwives Foundation.
Conflicts of interest
The authors declare no conflicts of interest.
References
appendix I:
Appendix I: COVID pretest%u2013post-test questions and answers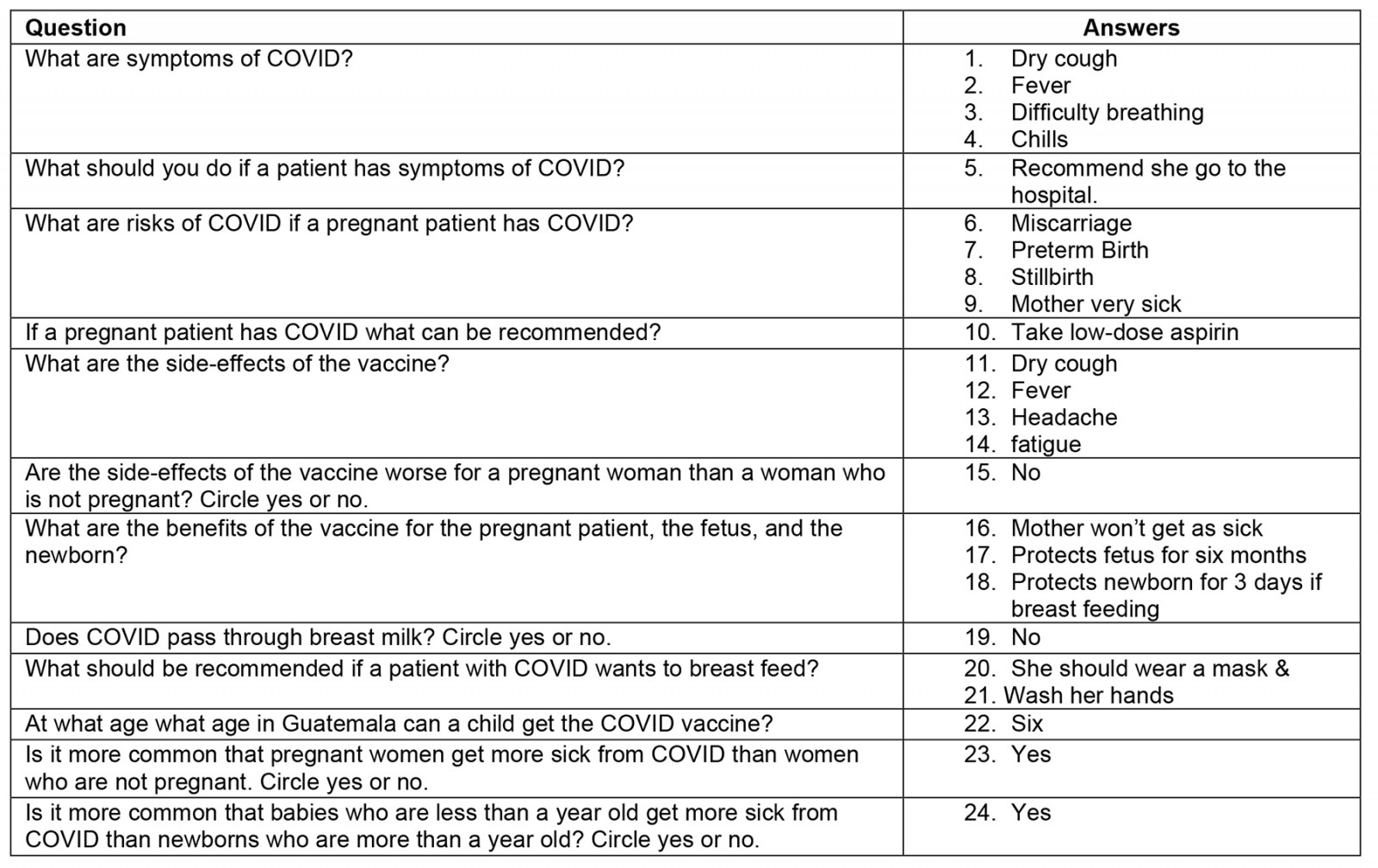
Appendix II: COVID reminder card
You might also be interested in:
2021 - Tuberculosis in the Torres Strait: the lady doth test too much
2012 - Social exclusion and myiasis of the upper lip in a Brazilian rural resident






