Introduction
This study deals with geographical characteristics and health equity, in particular when talking about the social environment and human health. Specifically, it focuses on financial equity and healthcare equity between deceased individuals and their families in urban and rural areas. The definition of rural includes population size, density, distance factors specific to care access, and administrative classifications of specific area1. Some countries, such as the US and Australia, have formal urban and rural classifications2,3, but no internationally standardised definition4. Nevertheless, in most countries there is considerable heterogeneity between urban areas and rural and remote areas. Therefore, each country is predominantly classified as non-urban and urban, based on history, culture and population distribution.
Health status between urban and rural areas is particularly important in the context of regional equity. Populations in rural and remote areas are often at a disadvantage in terms of access to health resources and also in terms of health outcome5-7. Rural residents experienced poor doctor–patient relationships and had poor cancer survival rates8. Rural areas are home to 25% of the US population, but only 10% of primary care providers work in rural areas9. In addition, rural residents have to travel longer distances for treatment than urban residents, so there is a geographical barrier10. These factors can affect healthcare costs in the last years of a rural resident's life. Rural deaths have lower healthcare costs than urban deaths11. This study focuses on deceased individuals and their households by geographical location (rural or urban).
Understanding the cost of death is important for both individuals and countries seeking financial security at affordable healthcare costs. The use of health care associated with a deceased individual and the burden on their household depends on a number of factors, including the type of treatment, geographic location, and socioeconomic status of the individual. In the US, estimates of the percentage of Medicare costs incurred by patients in the last year of life vary from 13% to 25%, depending on methodology and assumptions12. In Taiwan, spending in the last 3 years of an individual’s life reached 24.5%13. In a Dutch study of people aged 65 years and over, higher prior healthcare costs were associated with higher costs of death, with older people using more long-term care services and younger people visiting the hospital more often14.
Catastrophic health expenditure (CHE) is an indicator of household burden due to out-of-pocket (OOP) expenditure15. This is the ratio of OOP expenditure to a household's ability to pay. CHE is on the rise as poor individuals require medical intervention for survival15,16. CHE incurred during this period is significant both in terms of the government's healthcare budget and in terms of the household economy. It is noteworthy that studies on CHE in urban and rural areas have not been active so far. Therefore, it is essential to review the equity between urban and rural areas in OOP expenditure of the household of the deceased and household CHE. If there is no difference in the prevalence of CHE between urban and rural areas, it will be an achievement of the healthcare policy that has been implementing inclusive health care to alleviate geographical inequity.
The question for this study was 'Is there an existential gap in income and CHE between urban and rural households of the deceased?', and the purpose was to identify income and health equity in urban and rural areas through the Korea Health Panel (KHP). Therefore, the author established the following hypotheses in consideration of previous studies. First, the sociodemographic characteristics of deceased individuals in rural areas will be such that they were more vulnerable than those in urban areas. Second, rural deceased are likely to have had higher disease severity and lower healthcare access and household OOP expenditure than in urban areas. Third, the annual income and household ability to pay for rural deceased would be lower. Fourth, the prevalence of CHE in rural areas would be higher than in urban areas. The author hopes to discover new knowledge about rural health, and because local phenomena are global knowledge it is hoped that effective implications for global rural health can be derived through this study.
Methods
Study design
From 2009 to 2018, this cross-sectional study aimed to identify annual household ability to pay, OOP expenditure and prevalence of CHE of households of deceased individuals in urban and rural area using the KHP long-form data for 10 years.
Data used
The KHP data used in this study was surveyed to identify health level and healthcare use from 2008 to 2018, but since the present study only used variables that were continuously surveyed, data from 2009 were analysed. KHP selected about 8000 households and about 12 000 household members belonging to those household through the proportional cluster extraction as a representative sample of individuals in the Republic of Korea (South Korea). Survey variables consist of about 500 variables such as household economy and living conditions, health level and health behaviour, and healthcare use. Survey variables were changed or new variables included as needed17.
Every year, specially trained investigators conduct face-to-face surveys through home visits. In particular, for the accuracy of healthcare use and costs, subjects record the status of healthcare use in a standardised health household account book, and the investigators review the accuracy of these records. In addition, in this process, the subjects was trained in advance on the recording method, and the investigators classified and entered it into a standard classification of diseases. In addition, the collected data for each year are corrected for errors over a period of about 3 years, merged with existing data and, after the completeness of the data was confirmed through a preliminary conference, the original data were disclosed to researchers17.
Study variables
Urban and rural areas: To understand the findings and make international comparisons, the definition of rural and remote areas is important. Urban areas are generally densely populated, and have good infrastructure and a wide range of services and facilities. Rural areas generally have less developed social infrastructure such as public transportation facilities. In particular, rural South Korea is a ‘super-aged’ society with more than 20% of the local population aged 65 years or older, and the low birth rate is more accelerated than in urban areas.
When considering classification of urban and rural as an administrative system, each deceased individual’s final address is indicated as 'Eup', 'Myeon', and 'Dong'18. If a residence is determined to be an urban area, the address is classified as 'Dong'18. In the case of 'Eup’ or ‘Myeon', there are benefits such as classification, reduction of levies, and reduction of local tax according to the Rural Special Regulations19. Therefore, in the KHP data, if the address of the household of the deceased ended in 'Dong', it was classified as an urban area, and if it was ‘Eup’ or ‘Myeon', it was classified as a rural area.
The term ‘rural’ is generally associated with agricultural areas but includes other types of non-urban areas, such as fishing villages and forestry areas. These areas have low population densities but high dependence on natural resources. They also share some common characteristics, such as the relatively underdeveloped factors of transport networks, healthcare facilities, educational institutions and big commercial facilities. Therefore, rural areas in this study include remote areas in South Korea.
In reality, the distinction between urban and rural areas is different in most countries. Rural characteristics may vary depending on environmental changes such as urbanisation or population density. The situation is the same in South Korea. In the case of 'Eup', it can take the form of an urban–rural complex. This is because there are cases in which urban areas are developed according to population migration. Therefore, the distinction between urban and rural areas in South Korea can be somewhat confusing. In South Korea, the extent to which an area is considered urban is different for each sublaw, and the application of meaning is also different for each administrative department. However, in most public institutions, 'Eup' is classified as rural rather than urban. In addition, although it has a larger population than 'Myeon', it is located close to 'Myeon', so it can be said to be closer to the characteristics of a rural area.
Sociodemographic characteristics: Among the KHP data, the variables required to know the sociodemographic characteristics of the deceased are year of death (2009–2018), age (years; age group), gender (men; women), household members (number of persons), literacy (yes; no), presence of spouse (yes; no), economic activity in the year of death (yes; no), type of healthcare insurance (National Health Insurance (NHI); Medicaid as public assistance) and registration as disabled by the Act on Welfare of Persons with Disabilities (yes; no). NHI is mandatory for all citizens and pays monthly healthcare insurance fees. Medicaid, a type of public assistance, is a system that supports with national taxes the medical expenses of individuals who cannot afford monthly medical insurance premiums. This corresponds to approximately 3% of the total population20.
Comorbidities: Number of comorbidities at the time of death of the deceased was evaluated. It can be used as a substitute variable to determine the severity of disease. Comorbidity means a combination of chronic diseases diagnosed by a doctor, such as hypertension, diabetes, hyperlipidemia, arthropathy, tuberculosis, ischemic heart disease and cerebrovascular disease17.
Healthcare service use experience: To determine medical service experience in the year of death, use of over-the-counter medications (yes; no), use of emergency rooms (yes; no), hospitalisation (yes; no) over a 3-month period and use of outpatient treatment (yes; no) were assessed. This is an assessment of whether or not the deceased used healthcare services.
Annual household income: This is the sum of the total earned income and total asset income of everyone in the household in the previous year. Earned income includes business income, and asset income includes real estate/movable property income, financial income, social insurance, private insurance, government subsidy, private subsidy and other income.
Annual household income and living costs as determined by KHP are the previous year's income and living costs. For the economic variable in the panel study, the previous year's actual amount was collected and temporally matched with other variables of the year that were affected by it. This is because it is an empirical approach that balances the accuracy of economic variables, comparability and data availability.
Household income is affected by the number of household members. So, equivalent annual household income was calculated by dividing annual household income by the square root of household size21.
equivalent annual household income = annual household income ÷ √household size
Annual household living costs (deductions for food and other necessities): These costs are living costs that are essential for survival, such as food and daily necessities. KHP investigated monthly living costs of the previous year, excluding savings, and so for the present study the author converted them into annual units.
Household living costs are affected by the number of household members. Therefore, the equivalent household annual living cost was calculated by dividing by the square root of household size21.
equivalent annual household living cost = annual household living cost ÷ √household size
Annual household ability to pay: Annual household ability to pay is generally calculated by subtracting living costs from household income22 or by subtracting food costs or subsistence expenditure from household living costs23.
In this study, the former calculation was used. Therefore, the annual household ability to pay in this study means annual household income minus annual household living costs. This is the amount a household can spend, including savings, and can be said to be the household's financial capacity.
annual household ability to pay = equivalent annual household income (including annual savings) – equivalent annual household living cost
Household out-of-pocket expenditure: This refers to the household OOP expenditure paid by the household of the deceased in the year of death. This cost is the annual OOP expenditure of all household members for emergency room, inpatient, outpatient and prescription drug purchases. OOP expenditure is the sum of all household members’ copayments or uninsured expense, after excluding the NHI's reimbursement to the healthcare provider. In South Korea, OOP expenditure is about 40% of total healthcare expenditure20.
Catastrophic health expenditure: This study measured annual household ability to pay based on income after deducting living costs. There are several thresholds for measuring CHE22. For this study, the threshold of CHE was set to be equal to or exceed 40% of the annual household ability to pay. Based on consumption, the threshold of CHE is also over 40% of household ability to pay, as in this study23, which can be said to be a considerable burden for households.
- Positive household CHE: annual household OOP expenditure ÷ annual household ability to pay ≥0.4
- Negative household CHE: annual household OOP expenditure ÷ annual household ability to pay <0.4
Statistical analysis
The author analysed data for the deceased individual, and data for the household of the deceased. For data relating to the deceased individual in the year of death, the author used the student t-test and the χ2 test to identify demographic characteristics, number of comorbidities and experience of using healthcare services by classifying into urban and rural areas.
For analysis of the household of the deceased in the year of death, annual household income and household living cost were identified after calculating equivalent household size. These variables were compared between urban and rural areas through analysis of covariance (ANCOVA), and confounding variables were input as covariates. The annual household ability to pay (equivalent annual household income – equivalent household living cost) was calculated.
Annual household OOP expenditure is the amount paid by all household members for the use of healthcare services in the year of death. This included emergency room, inpatient, outpatient and prescription drug costs. Household OOP expenditures were compared by categorising them into urban and rural areas through ANCOVA. At this time, confounding variables such as age group, number of household members, presence of spouse and economic activity were input as covariates.
In this study, the final target variable, prevalence of CHE, is the percentage of annual household OOP expenditure equalling or exceeding 40% of the annual household ability to pay. The prevalence of CHE between urban and rural areas was analysed through χ2.
All costs measured in South Korean won (KRW) were converted to US$ according to the 2009 exchange rate (1 USD=1259 KRW; 1 AUD=0.82 USD). Statistical analysis was conducted using SAS v9.4 (https://www.sas.com), and it was interpreted as statistically significant when the p-value was less than an alpha value of 0.05.
Ethics approval
For the use of KHP data, the author submitted a study plan to the Korea Institute for Health and Social Affairs (KIHASA), a data management institution, and then officially received the raw data. The data information cannot identify individuals and does not cause ethical problems when the unit of analysis is a group. The data used in this study were approved by the Institutional Review Board (KIHASA 2022-17).
Results
Sociodemographic characteristics in year of death
In the 10 years from 2009 to 2018, there were 869 deceased individuals in the data. Among them, 63.5% were urban residents and 36.5% were rural residents. There were 62.0% and 65.9% men in urban and rural areas, respectively, showing a homogeneous result indicating more deaths of men than of women (p<0.24). When dividing the data on the deceased individuals by age group, the numbers of deceased under 65 years or over 85 years were higher in urban than in rural areas (p=0.02). The mean numbers of household members of the deceased were 2.7 in urban areas and 2.4 in rural areas (p=0.03). The rate of presence of a spouse at the time of death was 63.8% in urban areas and 70.7% in rural areas, respectively (p=0.04). In the year of death, 12.7% of the individuals were engaged in economic activities in urban areas and 20.5% were engaged in economic activities in rural areas (p=0.02), respectively (Table 1).
Table 1: Sociodemographic characteristics in year of death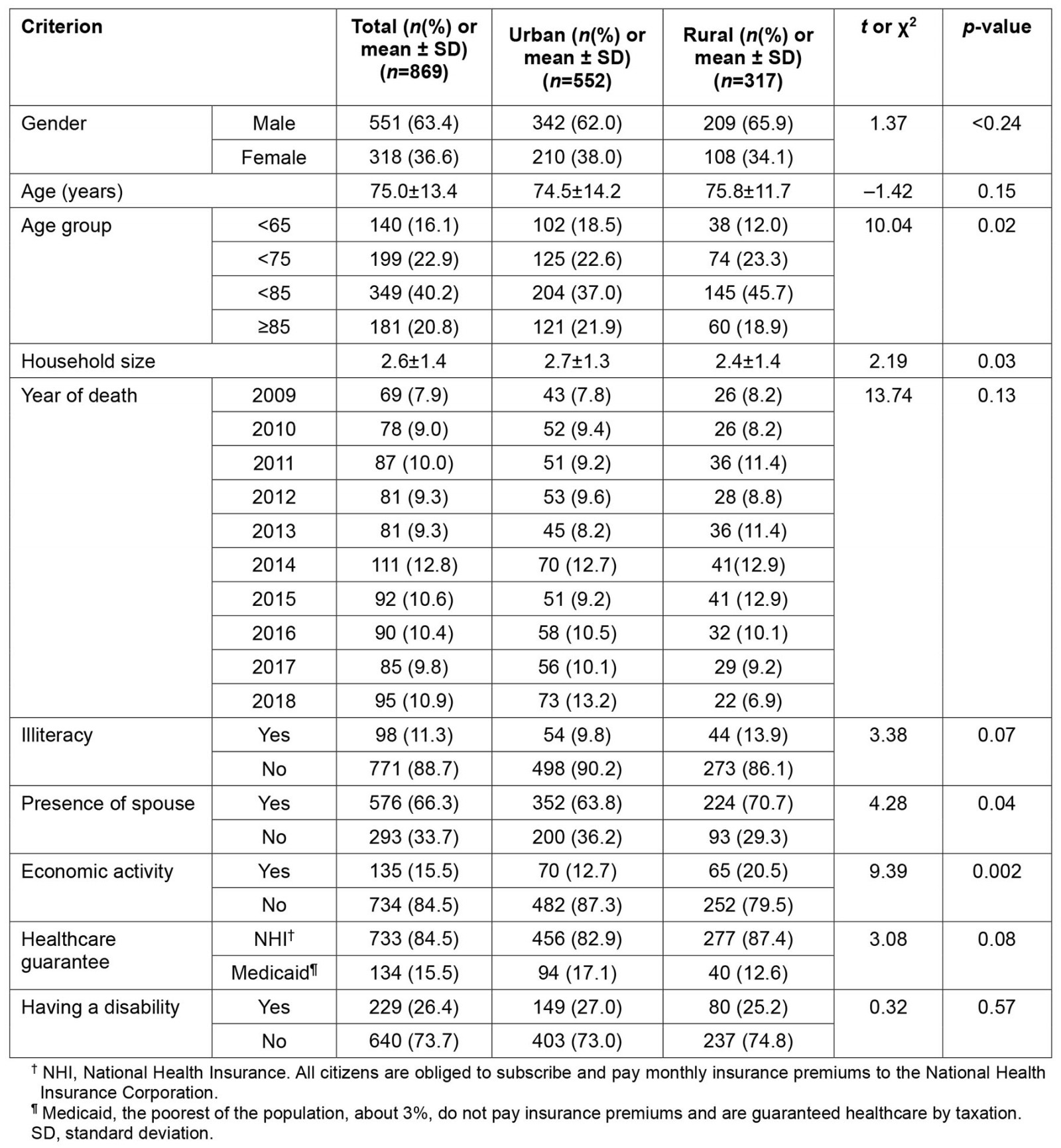
Comorbidities and experience of using healthcare services in year of death
There was no statistically significant difference in the number of comorbidities among the deceased in urban and rural areas. In addition, there was no statistically significant difference between urban and rural residents in the experience of taking over-the-counter medications for more than 3 months, the experience of using the emergency room, the experience of hospitalisation, or the experience of outpatient treatment (Table 2).
Table 2: Comorbidities and healthcare use experience rates in year of death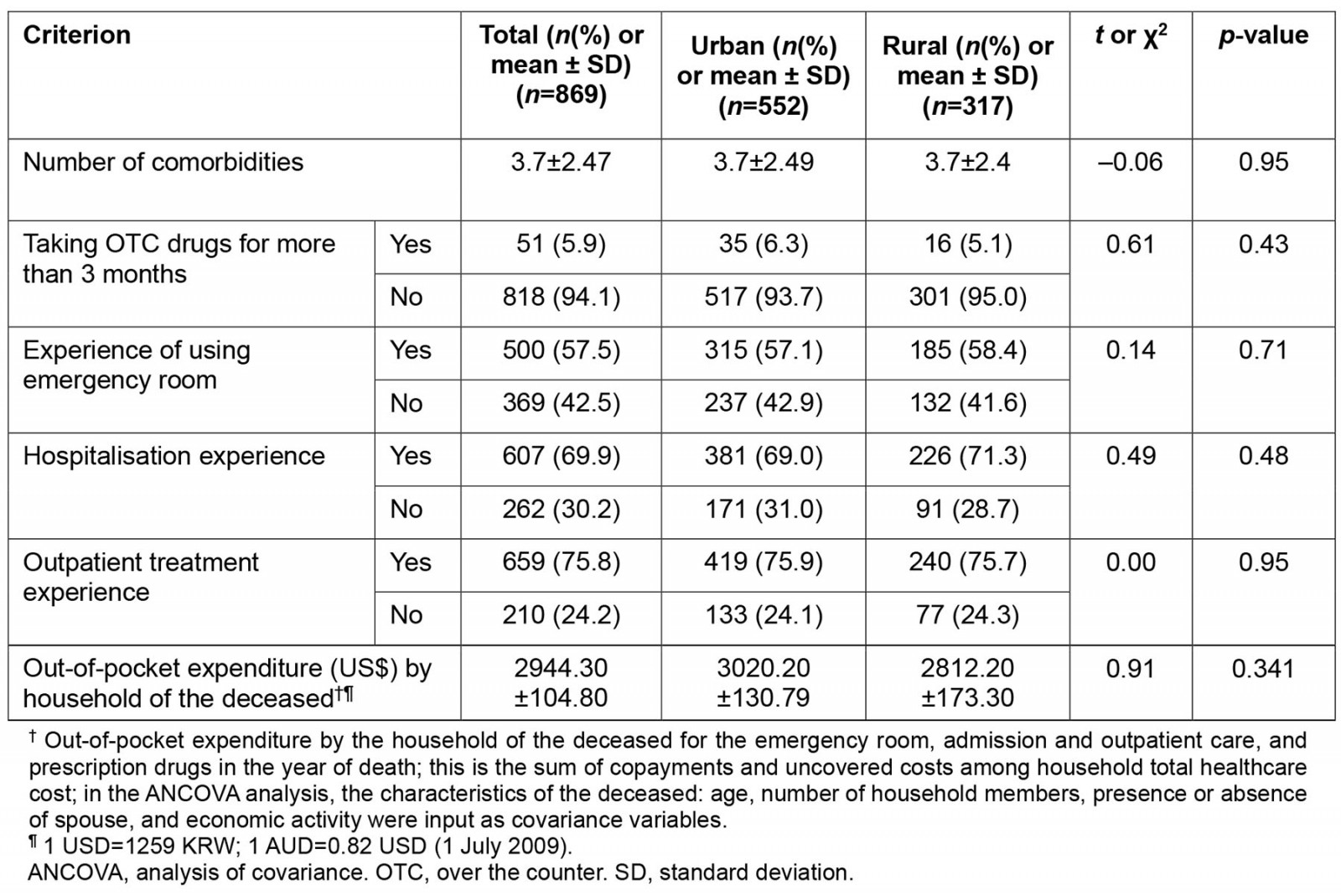
Household income, household living cost, and household ability to pay in year of death
The annual household incomes of the households of deceased individuals in urban and rural areas were US$15,673.80 and US$12,794.80, respectively (p=0.002). Living costs were US$939.70 and US$725.60, respectively (p<0.0001), and annual household abilities to pay were US$14,734.10 and US$12,069.30, respectively (p=0.03) (Table 3).
Table 3: Financial characteristics of households of deceased in year of death†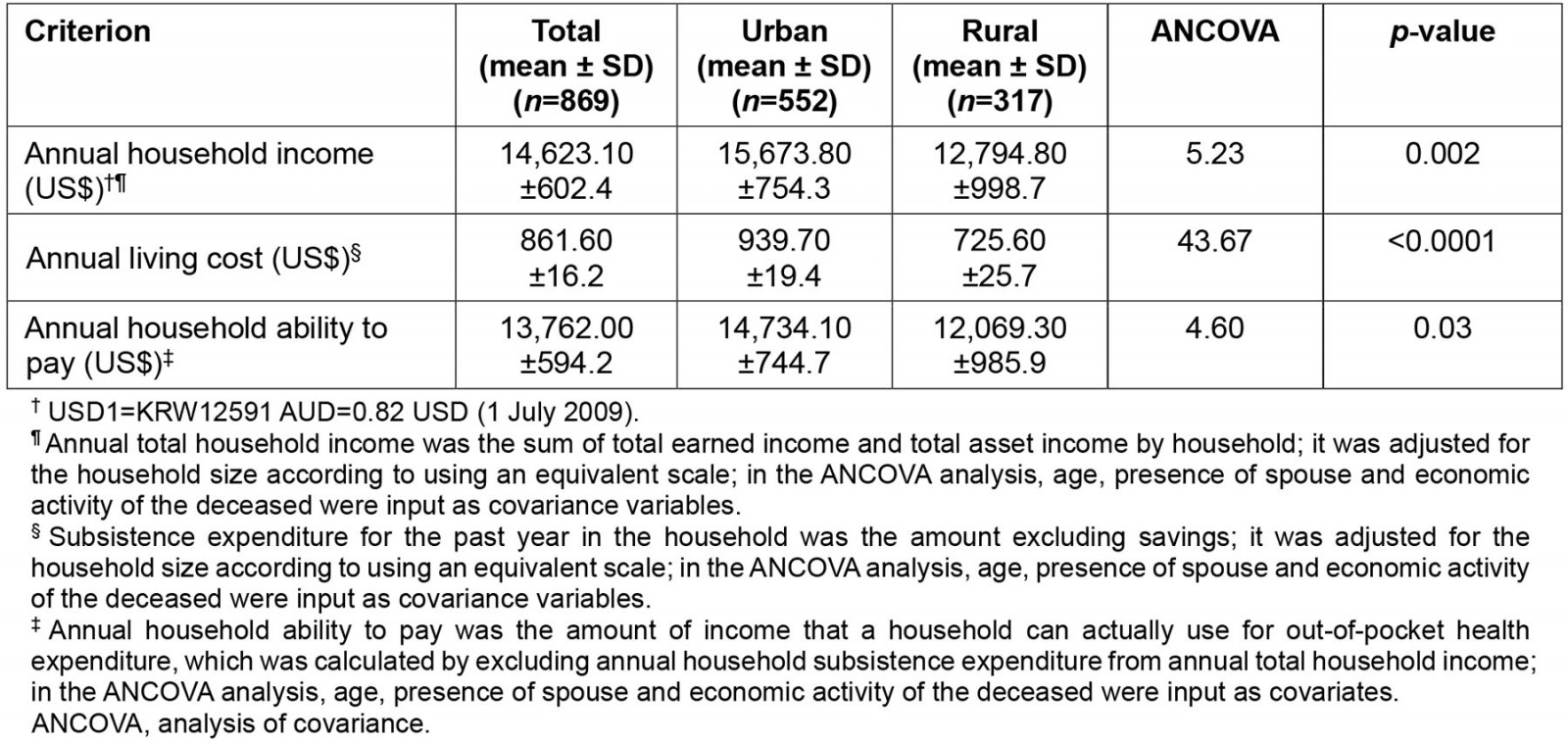
Household out-of-pocket expenditure and prevalence of household catastrophic health expenditure in year of death
In the year of death of deceased individuals, the household OOP expenditure was US$3020.20 for urban areas and US$2812.20 for rural areas, showing no statistical difference (p=0.341). The prevalence of household CHE was 68.3% in urban areas and 77.6% in rural areas, showing a significant difference (p=0.003) (Table 4).
Table 4: Out-of-pocket and catastrophic health expenditure in year of death†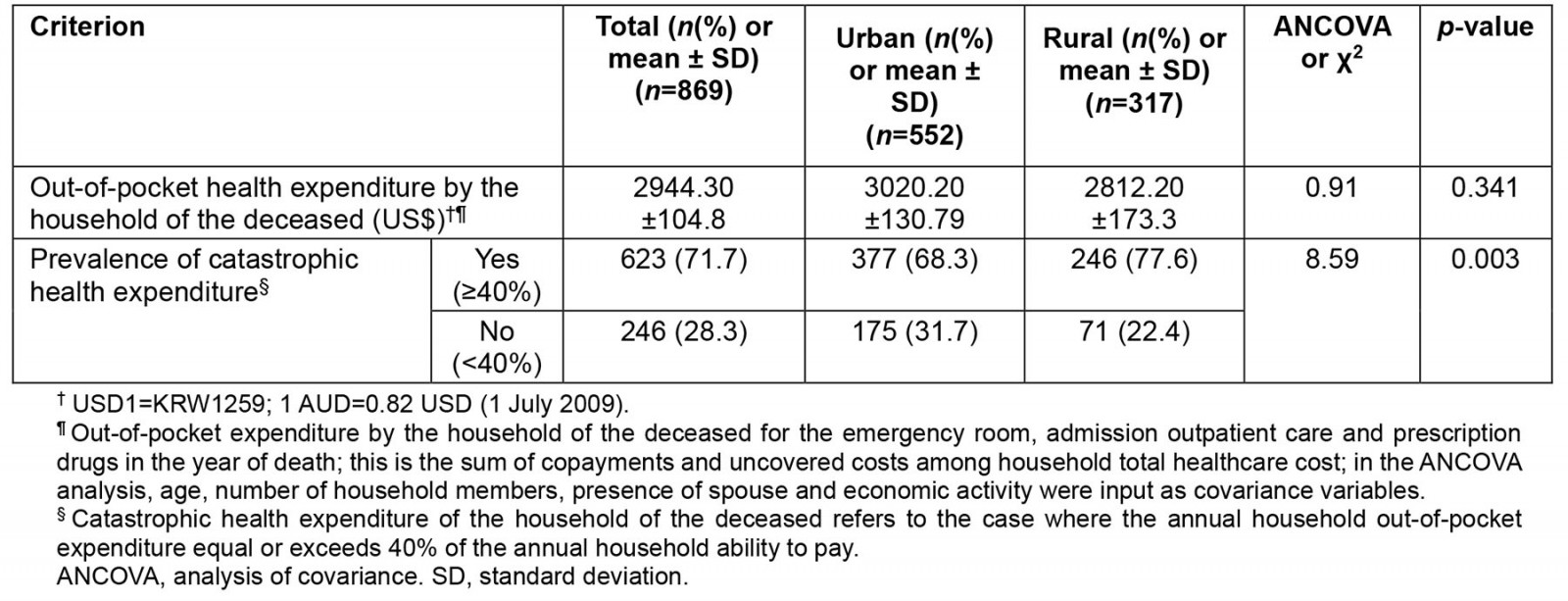
Discussion
In South Korea, since the enactment of the Medical Insurance Act in 1963, medical coverage has been provided to individuals under livelihood protection since 1977. Furthermore, in 1989, the NHI was established with the aim of ensuring universal healthcare for all citizens24. Additionally, the Act on Special Measures for Rural Health and Medical Service was introduced in 1980 to enhance equity in rural health care25 and, in 1995, the National Health Promotion Act was implemented to strengthen community-based medical care and public health functions26. Despite these efforts, the disparities between urban and rural areas persist in various aspects. Therefore, the importance of inclusive health care is emphasised. Hence, this study aimed to explore the equity of deceased individuals and their households in urban and rural areas.
It is crucial to understand the expenses associated with end-of-life care in order to comprehend healthcare costs. In high-income countries, approximately 8% to 11.2% of the annual health expenditure is allocated to individuals who pass away, constituting less than 1% of the total population27. In the Netherlands, the medical expenses for deceased individuals are 13.5 times higher than those for survivors, with a significant portion of the costs incurred in hospitals28. Similarly, in the US, healthcare costs are concentrated in the year preceding death, primarily due to chronic illnesses, which account for approximately 30% of total Medicare spending29. For cancer-related deaths, expenses tend to peak in the last month leading up to death30.
Identifying disparities in local environments and health outcomes, as well as determining relevant factors, is vital for promoting social cohesion. In a 10-year study (2009–2018) using data from the KHP, it was found that, out of 869 deaths, 63.5% occurred in urban areas and 36.5% in rural areas. This proportion of rural deaths was higher than the rural population percentage of 19% in South Korea as of 201831. One potential explanation for this disparity is that the probability-proportional stratified cluster extraction method employed by the KHP for selecting study subjects is likely to deliberately include a significant number of marginalised individuals. Another inference is that rural areas may have higher mortality rates compared to urban areas due to factors such as lower income levels, relatively weaker healthcare infrastructure, and exposure to harmful environments such as factories and pesticides.
Gender disparities in death distribution reflect the intricate interplay of biological and sociocultural factors. In this study, males constituted 62.0% and 65.9% of urban and rural deaths, respectively, displaying a higher and uniform pattern in men compared to women (p<0.24). This can be attributed to men's higher susceptibility to diseases and overall elevated mortality rates. A high rate of smoking contributes to an increased risk of atherosclerotic heart disease, liver cirrhosis, accidents and suicide32-34. These behaviors are often more encouraged or tolerated among men in society, such as engaging in adventurous activities, taking on risky occupations and consuming alcohol. Acknowledging the influence of both biological and sociocultural aspects is crucial for narrowing gender disparities. By addressing these multifaceted factors, fostering better health outcomes for all individuals, regardless of their gender, is possible.
A notable finding is that, among urban residents, there were higher numbers of deaths in individuals aged under 65 years or over 85 years compared to in rural areas (p=0.02). The high rate of deaths under the age of 65 years in urban areas can be attributed to the relatively large number of young people due to high job opportunities. Additionally, the greater number of individuals aged over 85 years in urban areas may be attributed to the higher survival rates resulting from superior income and access to quality medical care compared to in rural populations. Essentially, the concentration of older elderly individuals in urban settings can be attributed to their preference for urban living. The age composition of any country or region is important in understanding the business cycle35. Further research is warranted to explore these factors in more depth.
Urban areas have a high population density. In this study, the mean number of household members of deceased individuals was 2.7 in urban areas and 2.4 in rural areas, respectively (p=0.03). Additionally, the percentages of deceased individuals who had a spouse at the time of death were 63.8% in urban areas and 70.7% in rural areas, respectively (p=0.04). From this it can be inferred that the proportion of elderly people over the age of 85 years is higher in urban areas, so the spouse retention rate is relatively lower.
Moreover, in the year of death, 12.7% of urban residents and 20.5% of rural residents engaged in economic activities (p=0.002). One possible explanation is that rural areas lack the concept of retirement due to significant involvement in primary industries such as agriculture, forestry and fishery. Conversely, urban areas are characterised by work-oriented culture, which may have led to earlier cessation of economic activities for the deceased due to forced retirement. It is important to note that this pattern is not directly linked to income.
The first hypothesis of this study suggested that the data for deceased individuals in rural areas would exhibit relatively more vulnerable sociodemographic characteristics compared to those in urban areas. However, based on the findings of this study, it is challenging to draw a definitive conclusion regarding the sociodemographic vulnerability or superiority of data for the deceased in urban and rural areas. There were no significant differences observed between urban and rural areas in terms of other variables that could indicate vulnerability, such as average age, literacy rate and public assistance benefit rate. Notable variations in sociodemographic characteristics were observed in relation to rural areas, including smaller household sizes, and higher presence of spouse and economic activity. Therefore, these differences can be perceived as either positive or unrelated to vulnerability than urban area, so the first hypothesis is rejected. These results mean that there is no difference in terms of sociodemographic equity between urban and rural areas.
The second hypothesis of this study suggested that deceased individuals in rural areas may experience higher disease severity, limited healthcare access and lower OOP expenditure. However, the findings of the study rejected this hypothesis. The hypothesis was based on previous research indicating higher healthcare costs in rural areas11. In South Korea, major healthcare facilities are predominantly concentrated in metropolitan areas and regional urban hubs, posing challenges for rural residents in terms of accessibility, including long travel distances, transportation inconveniences, and additional expenses for lodging and transportation. Taking these factors into account, the medical-seeking behaviours and associated costs indicated by data for deceased individuals in rural areas can be inferred in several ways. Some may have chosen to seek treatment at urban hospitals, leading to higher medical expenses, while others may have opted for lower quality treatment to reduce costs. However, it is also possible that some individuals relied on local healthcare networks, resulting in similar medical costs compared to those in urban areas. The findings of this study suggest that the latter possibility cannot be disregarded.
Rural health is influenced cumulatively by health policies and practices6,36. Even in rural areas, where large hospitals do not exist, it is encouraging to see a diverse supportive healthcare system for rural residents working effectively. In this study, comorbidity was used as a surrogate indicator of disease severity, and evidence supports this approach37. In general, people with more comorbidities tend to have difficulty accessing appropriate health care38. This suggests that, in most rural areas of the country, community health systems such as public health centres, health branches and community health clinics play an important role in safeguarding the wellbeing of residents by providing affordable health care. In summary, there is no inequality in disease severity between urban and rural areas at time of death for South Koreans, implying that pre-death healthcare access and household burden experiences are similar in both urban and rural areas.
If this is the case, is there no factor of inequity in terms of health between urban and rural areas? In this study, annual household income and living costs were examined to assess the annual household ability to pay. This was done to determine a household's capability (level of income) to meet its financial obligations and expenses (expenditure). It is the amount obtained by subtracting annual living costs from annual household income. Therefore, a high annual household ability to pay is achieved when the income is high or the living cost is low, even with the same income. Generally, living costs are fixed expenses. The annual household ability to pay increases when there are better employment opportunities and potential access to financial resources. On the other hand, the annual household income and living costs in KHP refer to the income and living expenditure from the previous year. The economic variables in this study are values from the previous year, as this approach balances accuracy, comparability and other factors of economic variables.
The third hypothesis of this study stated that for the data on rural deceased individuals, annual income and household ability to pay would be lower. When comparing the annual household income of the deceased, rural households had an income of US$12,794.80, which was lower than the urban household income of US$15,673.80 (p<0.002). This difference could be attributed to urban areas having more job opportunities and higher wage levels, while rural areas rely heavily on agriculture, resulting in lower wages compared to urban industries. The annual living cost in urban areas was US$939.70, while in rural areas it was US$725.60 (p<0.0001). This disparity is primarily due to factors like higher housing prices and the overall cost of goods and services, including agricultural products, in urban areas. However, it is essential to consider that, although the living cost is generally lower in rural areas compared to urban areas, incomes are adjusted to local living costs. Additionally, the annual household abilities to pay in urban and rural areas were US$14,734.10 and US$12,069.30, respectively (p=0.03). Therefore, the findings supported the third hypothesis.
The final hypothesis of this study posited that the prevalence of CHE would be higher in rural households compared to urban households. The hypothesis was supported by the findings. CHE refers to significant and often unexpected healthcare costs that can have a severe financial impact on individuals or families. Factors contributing to CHE include limited access to essential healthcare services, a higher prevalence of chronic diseases, and lower income levels. In this study, the prevalence of household CHE was found to be 68.3% in urban areas and 77.6% in rural areas, indicating a significant difference (p=0.003). These results suggested that, while there was no disparity between urban and rural households in terms of OOP expenditure, there was a notable difference in the occurrence of CHE. The key determining factor in this outcome is annual household ability to pay, which is influenced by the relatively lower income levels in rural areas. Therefore, this study highlights the need for measures aimed at improving the income of rural households as a primary step in addressing the high prevalence of CHE in rural areas.
The findings of this study suggest that there were no significant differences in sociodemographic characteristics, disease severity and OOP expenditure of deceased individuals between urban and rural areas in South Korea. This indicates that South Korea's healthcare policy has been successful in achieving equity between urban and rural areas. However, despite these positive outcomes, the study has identified important empirical evidence that warrants consideration. The analysis of data on the household income of deceased individuals showed that rural households had lower income compared to urban households. As a result, their ability to pay for health care was also lower, even though the living cost is generally lower for rural households. Consequently, it can be reasonably inferred that the prevalence of CHE is higher in rural areas due to the close relationship between CHE and household income. These findings shed light on the current situation in South Korea and the effectiveness of efficient healthcare policies, but they do not fully address the issue of regional income equity. Therefore, it is crucial to emphasize the need for comprehensive national policies aimed at increasing income for rural households. These efforts are necessary to alleviate the burden of healthcare costs for rural residents.
The limitations and responses of this study are as follows. First, the various calculation methods employed to assess CHE pose challenges when directly comparing the findings with other studies. The unique value of this study lies in its focus on deceased individuals and their households. Second, the measurement of annual household OOP expenditure introduces ambiguity due to variations based on the timing of death. Nevertheless, this ambiguity is equally applicable to both urban and rural areas39. Third, the absence of difference in OOP expenditure between urban and rural household may indicate positive effects of health policies. However, there is a possibility that rural households may give up advanced medical services. Further investigation is necessary to understand the factors contributing to preventable deaths. Fourth, the use of financial variables spanning a 10-year period may not align with current monetary values. However, this systematic error is consistent across urban and rural areas, allowing for reasonable comparisons. Fifth, the utilisation of comorbidity as a measure of disease severity has limitations in capturing sudden causes of death, such as accidents and suicides. However, the likelihood of such events is relatively low, and their impact on the study's results is considered to be insignificant.
Conclusion
A well-balanced study of rural and remote health not only contributes to improving local health but also provides valuable insights applicable to rural and remote areas worldwide1. This study's findings reveal no significant differences between urban and rural areas in terms of sociodemographic characteristics, health status of the deceased, healthcare experience and OOP expenditure of the household of the deceased. It indicates the positive impact of various policies and practices aimed at addressing urban–rural health equity. However, a crucial disparity emerges when considering the higher prevalence of CHE observed in rural areas. It can be attributed to low household income and limited ability to pay, which directly affect the occurrence of CHE. Therefore, preventive measures for CHE in rural areas should encompass not only micro approaches such as improving medical access and controlling medical expenses but also social development plans to enhance the incomes of rural households. While these findings are primarily based on the context of rural health in South Korea, they contribute to the broader global knowledge that is vital for improvement and cross-country comparisons, especially considering countries at different stages of development1,40. The author hopes that this study further strengthens the evidence highlighting the significance of income in rural health.
Acknowledgements
Thanks to Joongbu University for encouraging this study. Also, I would like to thank the Korea Institute for Health and Social Affairs and the National Health Insurance Corporation for their efforts in producing and managing KHP data.
Funding
This article was supported by Joongbu University Research & Development Fund, in 2023.
Conflicts of interest
The author declares that there are no conflicts of interest.
References
You might also be interested in:
2004 - Investigating the health of rural communities: toward framework development

