Introduction
During the COVID-19 pandemic, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) did not require medical treatment in most cases1. The remaining 14% (severe) and 5% (critical) of cases involved severe pneumonia and respiratory illness, requiring hospitalization and more likely to have long-term effects2.
Skjørten et al reported a high prevalence of dyspnea (16–89%) within 1.5–6 months after COVID-19, regardless of hospitalization1. Sanchez-Ramirez et al and Daher et al determined the presence of subjective symptoms such as cough, dyspnea, and fatigue, and also decreased functional capacity, even 8 weeks after discharge3,4. Zhu et al, MacIntyre et al, and Elbehairy et al showed that impaired lung diffusion led to a decrease in exercise capacity and strength of limb muscles5-7.
It is crucial to cope with the long-term complications of COVID-19 and to explore better approaches to help improve residual symptoms in this critical process.
Clinical guidelines recommend pulmonary rehabilitation for the management of the long-term effects of critical illness associated with COVID-19. It has been reported that a supervised pulmonary rehabilitation program improved lung function, exercise capacity, and exertional dyspnea in patients with severe (requiring hospital treatment) or critical (requiring admission to an intensive care unit and even ventilation) COVID-198-10.
Rehabilitation programs can be hospital-based, home-based, outpatient, or remotely supervised11. Due to the difficulty of accessing rehabilitation services and tackling an unprecedented epidemic, telerehabilitation has great potential to cope with the impact of the COVID-19 crisis in the absence of time and place constraints12. However, despite patients’ ongoing needs, they often have problems receiving support when they return home after discharge13. In particular, those who remain in rural areas are even less likely to receive adequate support during this period.
In hospitalized COVID-19 patients, pulmonary rehabilitation may be considered after outpatient hospitalization, given the possibility of long-term disability from the disease14. Home-based rehabilitation and inpatient rehabilitation were shown to have similar effects in decreasing physical sequelae in post-COVID-19 patients in a recent randomized study15. Home-based rehabilitation is a viable long-term alternative to prevent oxygen desaturation and/or a very lengthy waiting list for patients. At the same time, it can be vital for rural residents who have limited access to specialist clinics. Moreover, Huang et al demonstrated the superiority of different types of telerehabilitation programs over usual treatment and no treatment in COVID-19 survivors16. Previously, it has been stated that synchronous or asynchronous telerehabilitation is similar to conventional treatment for respiratory diseases17. Synchronous telerehabilitation models require real-time interactions and have some limitations18; asynchronous telerehabilitation, which does not require synchronous access, may be an alternative19,20. Supporting rural and remote communities where access to healthcare services is often inadequate is crucial through various telehealth modes that facilitate remote communication. This is because not only is accessing specialized services challenging for these patients, but long-term general care can also be difficult for many residents in these regions.
The diversity and quality of modern telehealth methods not only facilitate access but also have the potential to enhance general healthcare providers' ability to connect with patients in rural and remote areas. These applications for geographically separated people include patient-centered individual goals and aim to provide the most beneficial, high-quality service through strong communication21.
The effect of telerehabilitation on hemodynamic and subjective parameters associated with exertion and physical functions in COVID-19 survivors is not well established. Additionally, there is no study in the literature comparing the long-term effects of videoconferencing-guided synchronous telerehabilitation (VCG-ST) and mobile application-guided asynchronous telerehabilitation (MAG-AT) on these parameters in discharged COVID-19 patients. We also thought that the results obtained could be useful in program design for disadvantaged groups in terms of accessibility to health services and in monitoring the recovery processes of these cases.
The current study aimed to compare the long-term results of different types of telerehabilitation programs on hemodynamic and clinical parameters associated with exertion and physical functions using the following hypotheses:
- A videoconferencing telerehabilitation program is useful for hemodynamic and clinical parameters associated with exertion, functionality, and activity dimensions in COVID-19 survivors.
- A mobile application telerehabilitation program is useful for hemodynamic and clinical parameters associated with exertion, functionality, and activity dimensions in COVID-19 survivors.
- Following COVID-19, there is a correlation between a patient’s clinical and hemodynamic responses to exercise.
Methods
Study population
Study participants comprised patients who completed the COVID-19 medical treatment; were discharged from the Kartal Dr. Lütfi Kirdar City Hospital in Istanbul, Türkiye between August 2021 and January 2022; were aged 18–75 years; had access to a secure internet connection; had sufficient speaking, computer, and internet literacy skills for telerehabilitation; and who volunteered to take part2.
Health problems other than COVID-19 may lead to respiratory, functional, and effort-related dysfunction. To ensure a homogeneous distribution of groups, patients who had serious neuromuscular problems, infections, communication disorders, severe asthma, surgery of the lower extremities, or orthopedic problems were excluded.
Sample size was calculated using G*Power v3.1.9.7 (Heinrich-Heine-Universität Düsseldorf; https://resources.nu.edu/statsresources/downloadinggpower). The sample size in this study was estimated with reference to a study that showed a significant increase in squat time in the intervention group of discharged COVID-19 patients receiving telerehabilitation compared to the control group22. In a-priori analysis, recruitment of 28 participants using G*Power23 and assuming a one-tailed alternative hypothesis with 1 – β error probe = 0.80, moderate effect size d = 0.25, alpha error rate = 0.05, assuming a dropout rate of 10%, 32 participants were needed. A posthoc power analysis according to resting oxygen saturation at the end of the study found that the study power was 86%.
Study design
The study was planned as a parallel randomized controlled trial.
Procedure
Patients who met the inclusion criteria were assigned to either the VCG-ST or MAG-AT group using a computerized table of random numbers. All volunteers received individual training via Zoom by the same physiotherapist about the applications to be used in the study. The physiotherapist and the patient conducted mobile application training simultaneously in front of the screen. Each participant received synchronous online instructions on how to operate the application and progress to the exercise steps. We also provided the participants with written information forms. Outcomes were measured at baseline assessment, post-treatment, and follow-up (8 months after baseline assessment) by the same physiotherapist. The physiotherapist evaluated each patient online once a week via Zoom and updated the exercises according to the patient's progress.
Interventions
The same exercises were applied to both groups within the scope of the telerehabilitation program, and no additional devices were needed. The exercise program for both groups was planned at three different levels and positions (sitting, standing with support, and standing without support) according to the clinical condition of the patient. The program content also consisted of the same exercises. The exercise program included aerobics, muscle-strengthening exercises, and a balance training program for the extremities in addition to the respiratory training program (respiratory control, respiratory exercises, triflow exercises, coughing, and secretion removal training). Program progression was provided based on each participant's clinical condition and response to the exercises. As one-on-one weekly interviews were held with each patient, a series of exercises were applied, from sitting balance to standing and counting.
In the exercise programs, the type, frequency, and intensity of the exercise were adjusted by taking into account the perceived severity of dyspnea and fatigue by the patient24. During the exercises, a modified Borg Rating of Perceived Exertion Scale was used for dyspnea and fatigue, as well as oxygen saturation and heart rate monitoring with pulse oximetry. In undesirable situations – such as shortness of breath and fatigue, or when patients felt uncomfortable, the exercises were interrupted.
The patients in the VCG-ST group did all their exercise sessions via Zoom videoconference under the supervision of a physiotherapist. Patients in the MAG-AT group followed the exercises from the FizyoTr mobile application. Timurtas et al reported that it is a reliable application for health problems and has demonstrated excellent usability (System Usability Scale score >80.8) for clinicians25, and did the same exercises at home during the sessions. Both interventions were adjusted to average 30–40 minutes per session and were applied 3 days a week for 8 weeks.
The adherence ratios to both training programs were recorded in the study. In the MAG-AT group, patient participation in the sessions was automatically recorded by the application. For the VCG-ST group, the physiotherapist took note of each patient's participation in the sessions.
Outcome measures
The participants' assessments were conducted online via live videoconferencing as a result of the pandemic circumstances. Thus, assessments were chosen from exams that were appropriate for online evaluation26. The evaluation was conducted in the patient's surroundings, using the technology of their choice (computer, smartphone, or tablet), and data. Prior to every assessment, all patients were given instructions.
The 30-second sit-to-stand test (30 s STS) was used as a measure of lower extremity strength and functional status. The International Physical Activity Questionnaire short form (IPAQ) was used for the physical activity score; a finger pulse oximeter was used for oxygen saturation and heart rate determination; a modified Borg scale was used for dyspnea and fatigue assessments.
The 30 s STS is a safe and feasible test. It is performed on a supported chair with hands crossed over the chest, back straight, feet shoulder-width apart, and one foot slightly forward. It is requested that the patient sit and stand as much as possible within 30 seconds at self-paced speed. The patient takes a trial before the test, and the number of sit-to-stands in 30 s is noted27.
The IPAQ determines the level of physical activity in adults. The scale involves questions about vigorous and moderate physical activity, walking time of at least 10 minutes, and daily sitting time in the last 7 days. A Turkish version of the scale with validity and reliability was used28.
Finger oximeter measurements were used to determine heart rate and oxygen saturation values for monitoring to oxygen desaturation occurring with rest and exertion. Measurements were recorded at rest before each exercise session, during exercise, and at the end of the session. An oxygen desaturation level of 4% or above was deemed to be clinically significant.
Perception of fatigue and dyspnea at rest and after exertion were assessed with a modified Borg scale from 0 (no shortness of breath at all) to 10 (maximum shortness of breath)29,30. These outcomes were recorded at the beginning and end of each 30 s STS (exertion).
Statistical analyses
The Statistical Package for the Social Sciences v11.5 (IBM; https://www.ibm.com/products/spss-statistics) was used in the analyses. The compliance of the data with normality was measured with the Shapiro–Wilk test. The study data generally failed to meet parametric assumptions due to the low number of subjects, leading to the application of non-parametric tests.
The Wilcoxon test was used for within-group analysis and the Mann–Whitney U-test for between-group analysis. Repeat measures analysis was used to compare results between the two groups at baseline, post-treatment, and at long-term follow-up. Any variable with a significant difference in the baselines between the two groups would be used as covariance in the comparison.
The Spearman coefficient of correlation (rs) confirmed the relationship between the quantity of repetitions and other parameters. Fisher’s exact test was used to compare the proportions (receiving oxygen support, time from symptom onset to treatment, length of hospital stay). The significance level was set at p<0.050.
The authors concluded that the minimal clinically important difference (MCID) for 30 s STS in chronic obstructive pulmonary disease was calculated as two or more repetitions31; it has not yet been determined for COVID.
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and the Consolidated Standards of Reporting Trials (CONSORT) statement for randomized trials. Ethics approval was obtained from the Marmara University Faculty of Medicine Ethics Committee (No. 09.2021.1065). Confidentiality of patient information was ensured. The study's purpose and procedures were clearly explained to all patients. Participants signed written informed consent for the study. The researcher provided the patients with his contact number so they will ask questions about the study.
Results
Out of 33 discharged COVID-19 patients, three did not meet inclusion criteria, one refused consent, and 29 patients were randomized. After starting the programs, a patient in the VCG-ST group and a patient in the MAG-AT group were lost to follow-up. Fourteen patients in the VCG-ST group and 13 patients in the MAG-AT group completed the study (Fig1).
There were no significant differences between the two groups in any of the demographics or concerning receipt of oxygen support, regular exercise, length of hospital stay, or time from symptom onset to treatment (p>0.05) (Table 1).
Except for the oxygen saturation parameter, the baseline values of dyspnea, fatigue, heart rate, physical activity, and 30 s STS parameters were found to be similar at rest and exertion in the two groups (Table 2). The baseline mean oxygen saturation of VCG-ST was less than the MAG-AT group at rest (p=0.019) and after exertion (p=0.008) (Table 2). There was no significant difference between the two groups in these values in long-term follow-up (at rest: p=0.202, after exertion: p=0.350). Saturation at rest and after exertion in both groups increased significantly with telerehabilitation programs in long-term follow-up (p<0.05) (Table 3). According to the initial results, significant improvement was seen in all parameters in long-term results with telerehabilitation programs (p<0.05). However, when the groups were compared, neither the baseline nor the long-term follow-up data showed a statistically significant difference between the two groups for any measure other than oxygen saturation (p>0.05) (Table 3).
Interaction effects between group and time occasions were found in the IPAQ (p=0.013). Physical activity level had increased at the end of the program. The VCG-ST group had a slightly higher mean score in IPAQ post-intervention (VCG-ST group: +1024, MAG-AT group: +884), but less than the MAG-AT group in follow-up (VCG-ST group, +1108, MAG-AT group: +1379). In the follow-up period, both groups maintained the increase in physical activity levels attained at the end of the program. This increase was similar in both groups.
The VCG-ST group showed greater improvement in the resting and post-exertion oxygen saturation at the post-intervention (resting oxygen saturation: VCG-ST group: +4.28, MAG-AT group: +2.23; post-exertion oxygen saturation: VCG-ST group: +5.07, MAG-AT group: +2.61) and follow-up (resting oxygen saturation: VCG-ST group: +4.64, MAG-AT group: +2.38; post-exertion oxygen saturation: VCG-ST group: +6.92, MAG-AT group: +3.30). A significant improvement was seen in oxygen saturation, when analyzing the between-group effect at rest (p=0.031) and post-exertion (p=0.004). According to this analysis, the oxygen saturation level of the VCG-ST group improved more than the MAG-AT group at the end of the program.
Hemodynamic parameters showed a high or excellent positive correlation with each other, between rest and after exertion (p<0.0001 for all). According to assessments after exertion, dyspnea showed a moderate positive correlation with fatigue (r=0.582, p=0.001) as well as with heart rate (r=0.412, p=0.033), while it exhibited a moderate negative correlation with 30 s STS (r=–0.424, p=0.027) as well as IPAQ (r=–0.401, p=0.038). There was a moderately negative correlation between resting oxygen saturation, dyspnea (r=–0.552, p=0.003), and fatigue (r=–0.401, p=0.038) parameters. Also shown was a strong relationship between 30 s STS and IPAQ scores (r=0.610, p=0.001). The detailed results are given in Table 4. According to these results, oxygen saturation at rest provides information about dyspnea and fatigue at rest. Moreover, post-exercise dyspnea not only provides information on post-exercise fatigue and heart rate, but also may provide insight into clinical parameters such as physical activity and lower extremity muscle strength. Patients with higher resting oxygen saturation showed lower levels of dyspnea and fatigue. In subjects with worse pre-exercise dyspnea, fatigue, and heart rate values, these parameters were negatively affected after exertion.
Table 1: Characteristics of COVID-19 patients discharged from the Kartal Dr. Lütfi Kirdar City Hospital in Istanbul, Türkiye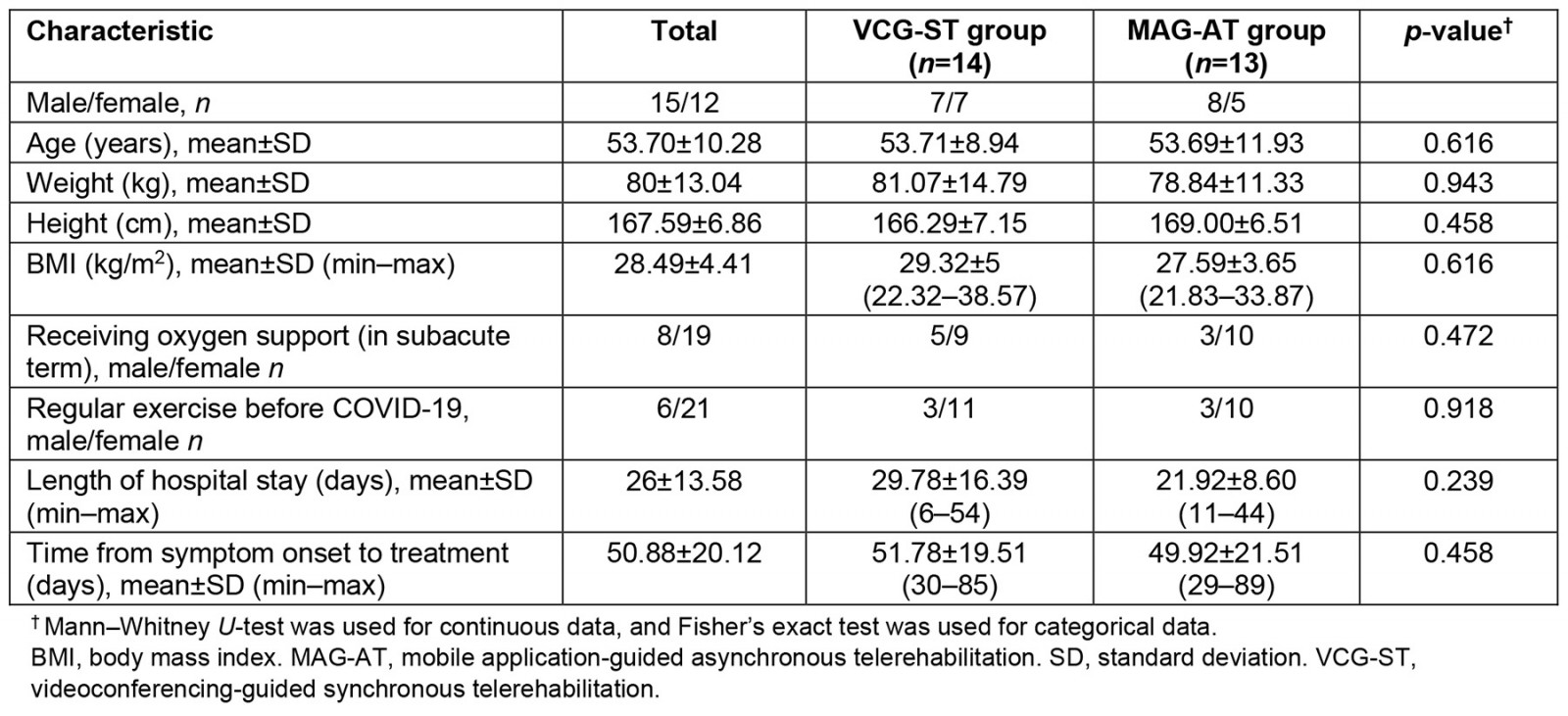
Table 2: Baseline evaluation results of participant groups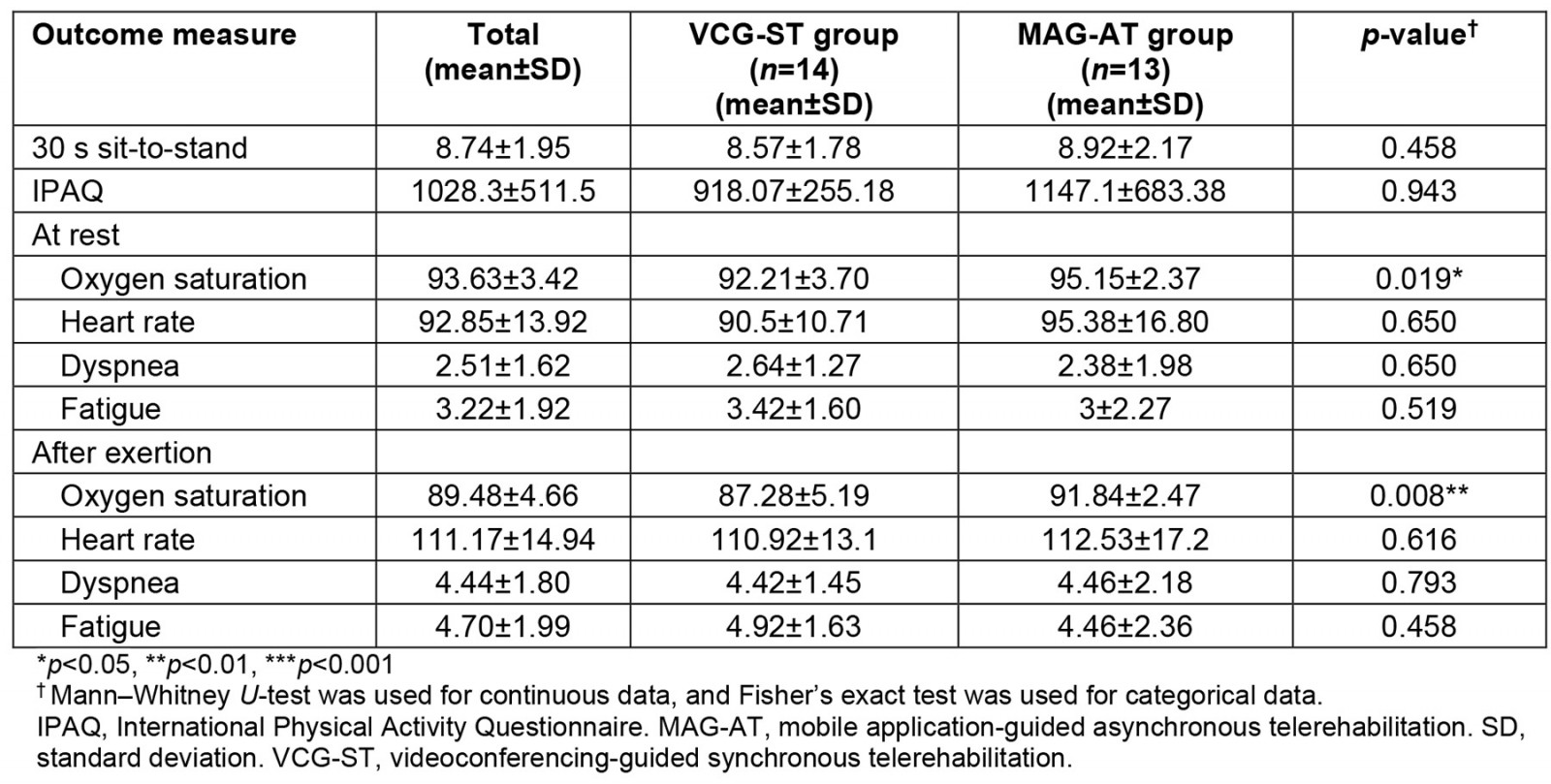
Table 3: Comparison of outcome measures between and within participant groups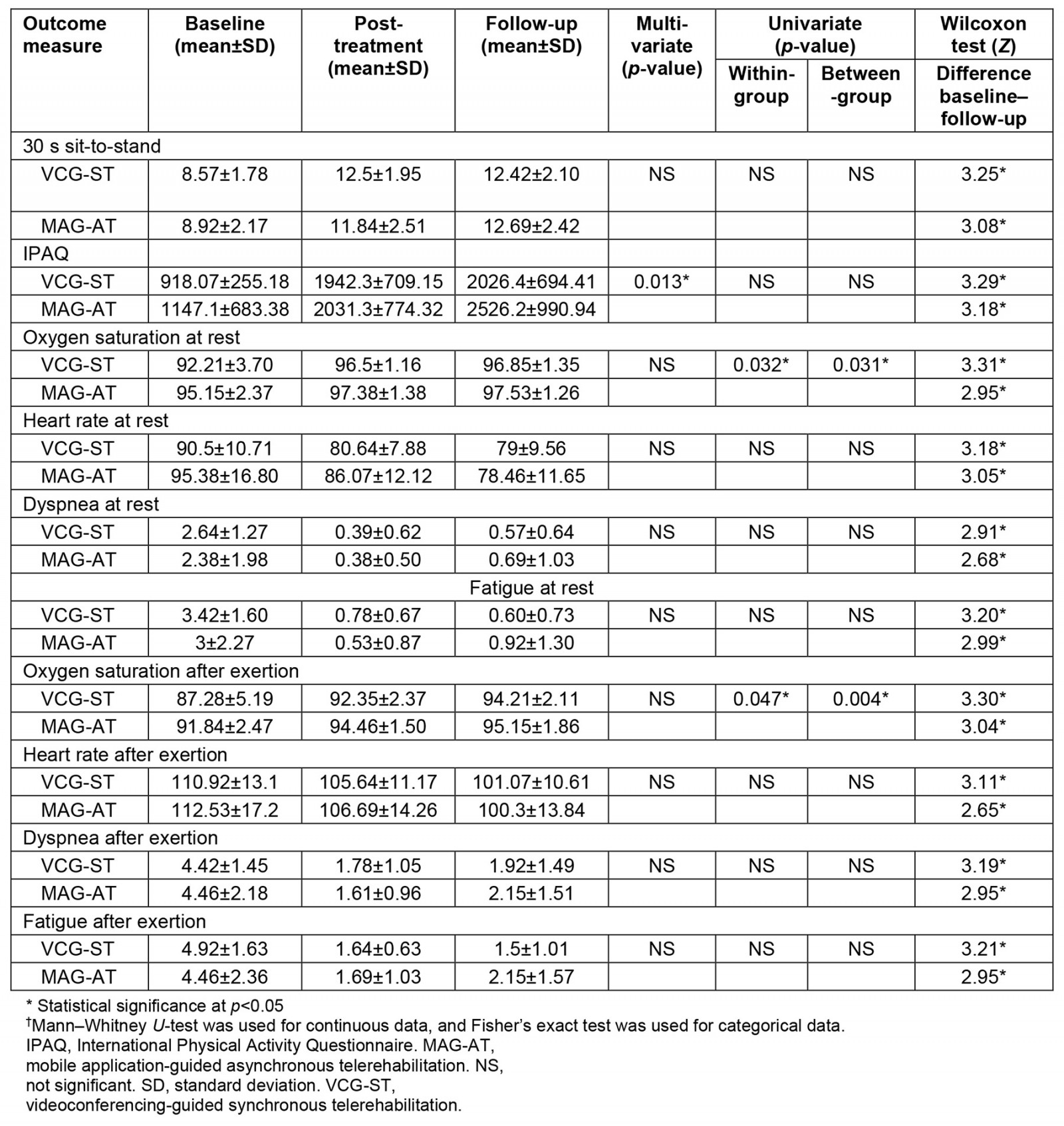
Table 4: Correlation parameters (Spearman’s rank correlation coefficient, rs) of all patients at baseline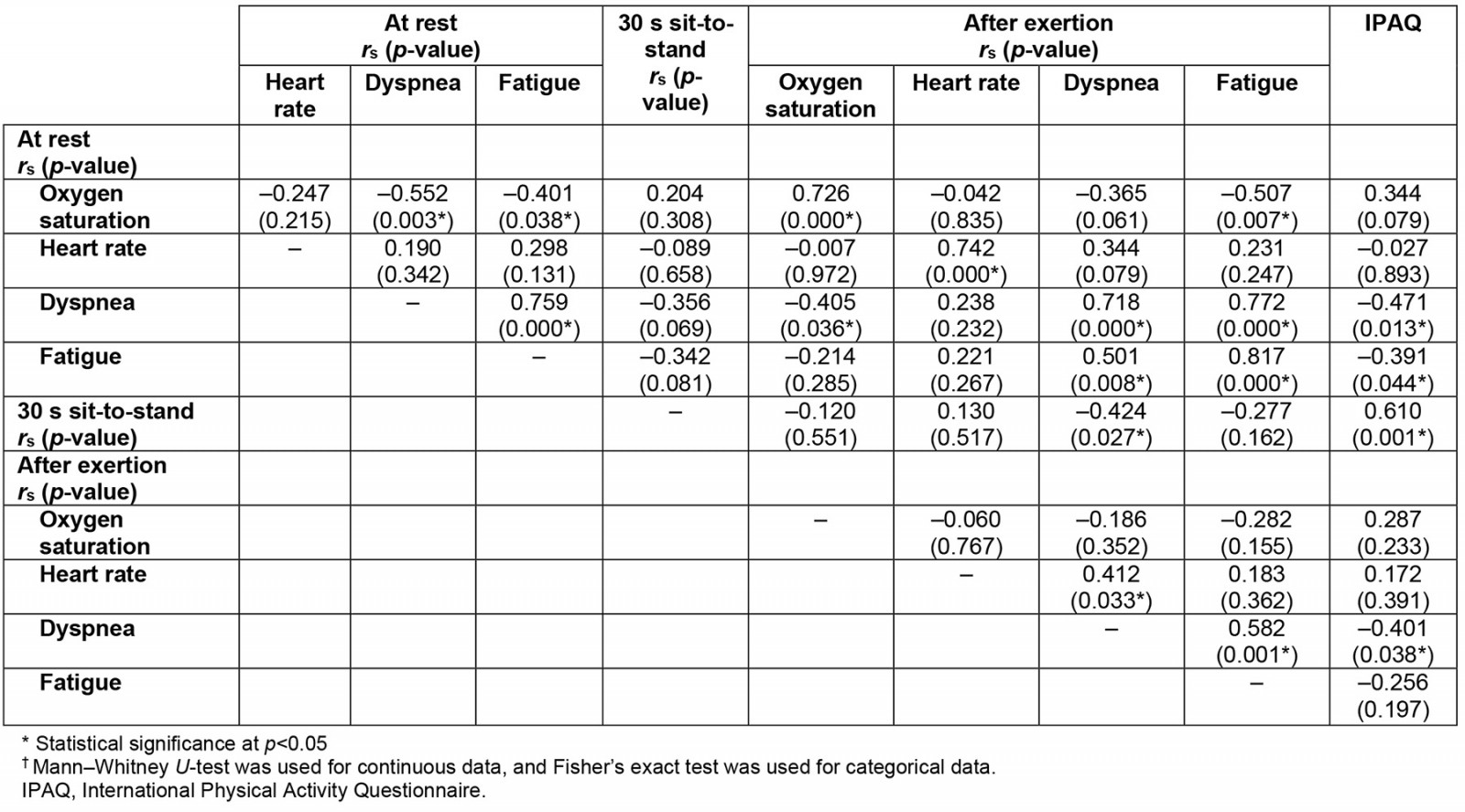
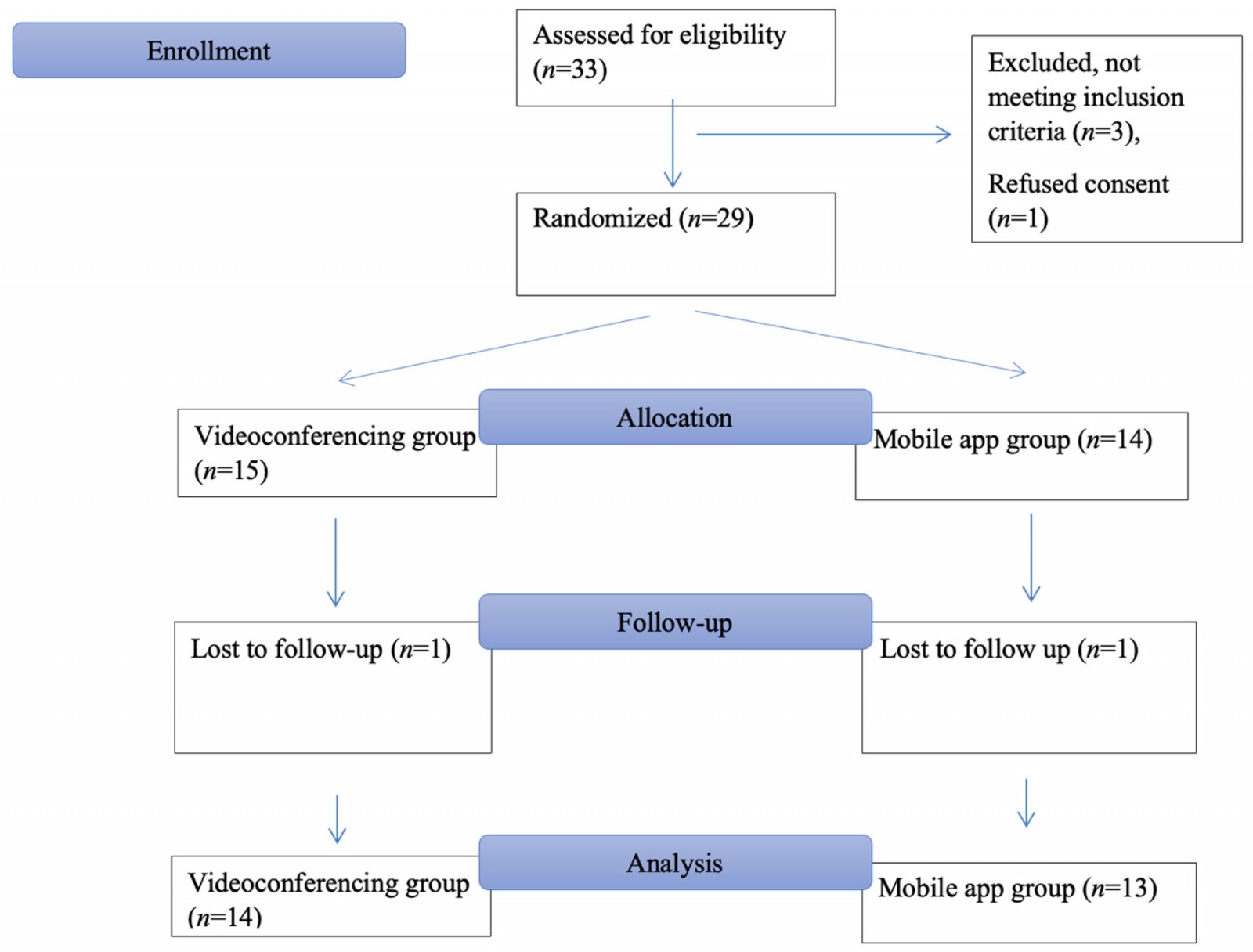 Figure 1: Consort flow diagram of the study.
Figure 1: Consort flow diagram of the study.
Clinically important difference in 30 s STS
Based on the determined 30 s STS MCID values, the patients who showed MCID were sorted as follows: between baseline and post-treatment (VCG-ST 92.86% (n=13) v MAG-AT 76.92% (n=10)); between post-treatment and follow-up (VCG-ST 7.14% (n=1) v MAG-AT 23.08% (n= 3)); and between baseline and follow-up (VCG-ST 92.86% (n=13) v MAG-AT 69.23% (n=9)) (Fig2).
Adherence to the program was determined to be 84% for VCG-ST versus 92% for MAG-AT.
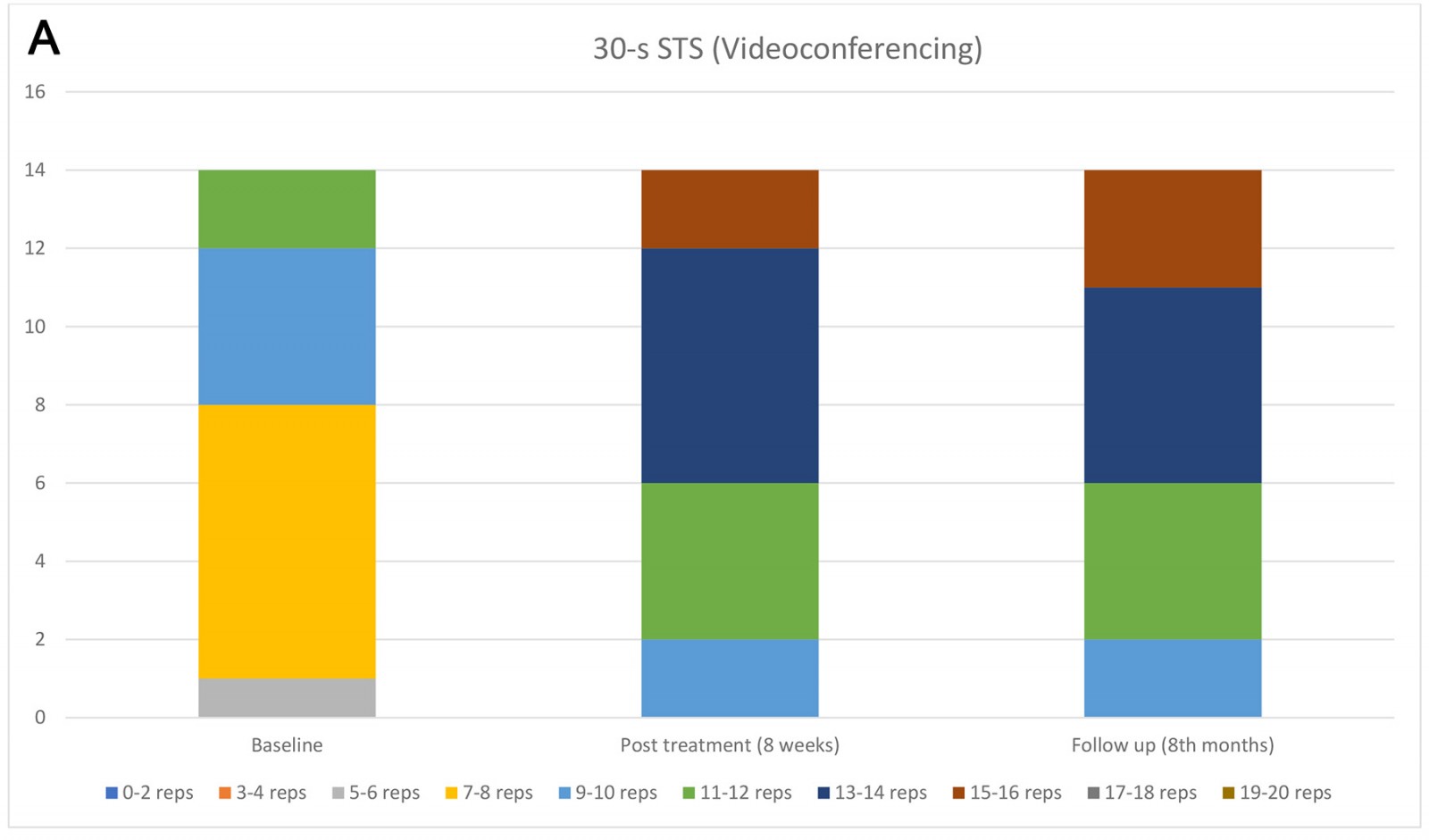
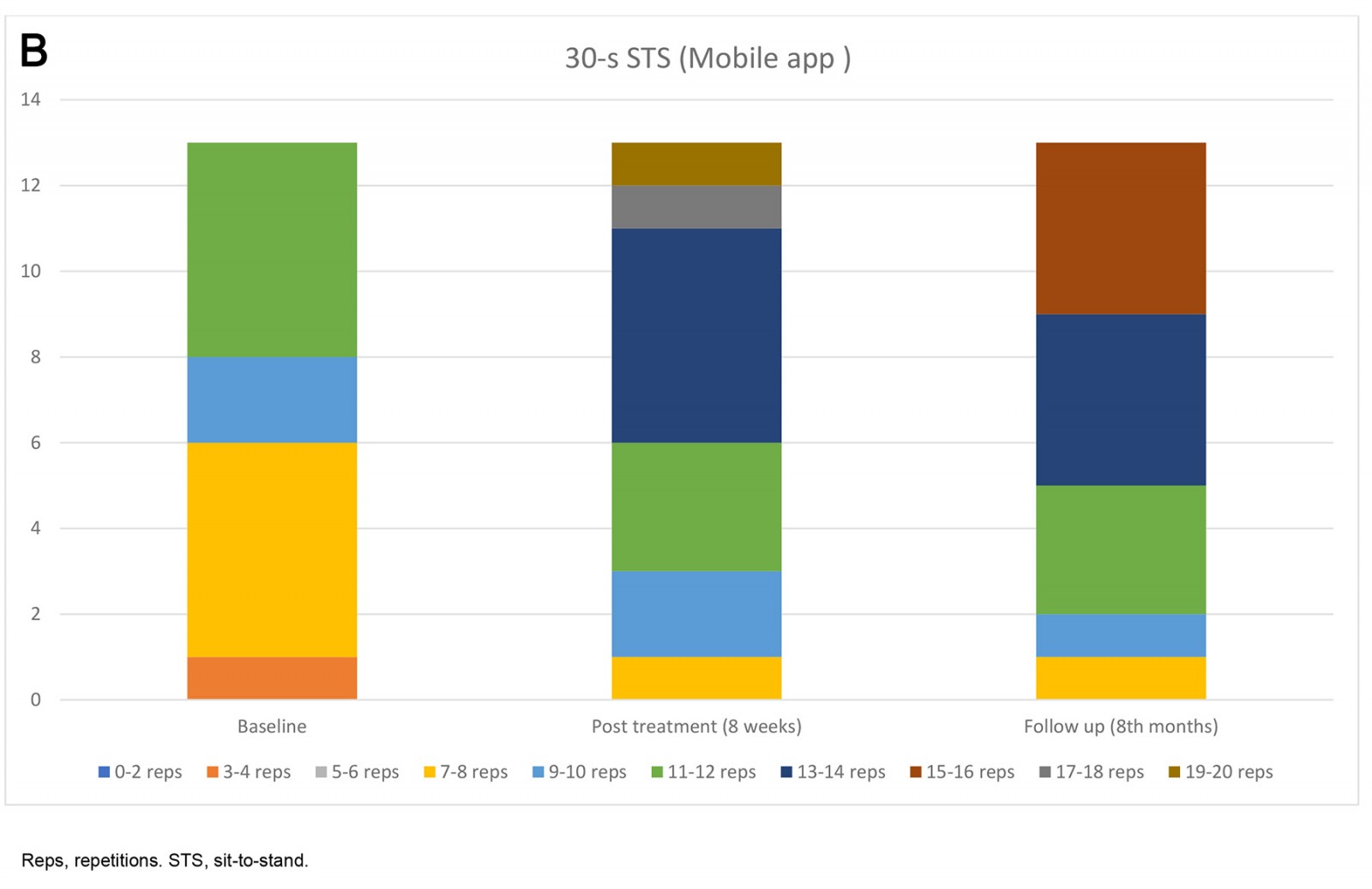 Figure 2: Number of participants with minimal clinically important difference in 30-second sit-to-stand test for (A) videoconferencing and (B) the mobile app.
Figure 2: Number of participants with minimal clinically important difference in 30-second sit-to-stand test for (A) videoconferencing and (B) the mobile app.
Discussion
Pulmonary rehabilitation is an effective treatment for lung diseases to improve functional capacity, muscle strength, muscle size, and systematic oxidative stress32. Due to the high contagiousness of the virus during the pandemic period, the American Thoracic Society and the European Respiratory Society suggest focusing on alternative approaches such as telerehabilitation in this process33 for lung diseases. Telerehabilitation has been previously studied in COPD and other chronic infections such as HIV patients34, and has demonstrated clinical benefits similar to programs in hospital-based rehabilitation35. Telerehabilitation is also recommended in patients with COVID-1936, and this study was performed with discharged COVID-19 patients in the subacute period with different telerehabilitation methods. The main findings of this study are that, first, the VCG-ST and MAG-AT showed significant improvement in all evaluated parameters; second, VCG-ST showed slightly better improvement than MAG-AT; and third, dyspnea after exertion had a moderate correlation with fatigue, number of repetitions (30 s STS), heart rate after exertion, fatigue after exertion, and physical activity level.
Exercise capacity is closely related to the function of the cardiopulmonary system; improving the respiratory system will increase exercise tolerance, and increasing the muscle strength of the lower extremities will reduce the burden of the cardiopulmonary system in ambulation32. In the current study, since the exercises were given to strengthen both respiratory muscles and lower extremity muscles, it reduced dyspnea after exertion, and 30 s STS counts increased in both groups. Additionally, in this study there was a weak negative correlation between dyspnea (after exertion) and 30 s STS and IPAQ at the baseline measure. This situation is consistent with the gains achieved. However, there was no apparent superiority of the groups over each other in these parameters. The fact that there was no significant superiority between the groups over each other in general indicates that both teletraining methods can improve cardiopulmonary function. In addition, our results proved that the hemodynamic parameters used in this study can guide the clinician in remote monitoring and treatment.
Impaired lung diffusion leads to a decrease in exercise capacity and strength of limb muscles5. The data in the present study showed that oxygen saturation at rest can provide information about other parameters at rest, and dyspnea after exertion can provide information about ambulation and exercise capacity together with other parameters after exertion. While oxygen saturation values alone have only a limited discriminative power, more meaningful inferences can be made when evaluated together with clinical conditions37,38. These two parameters, which can be measured in a short time during remote monitoring at discharge, can be questioned frequently. These results may benefit clinicians in the design and implementation of remote programs for cardiopulmonary rehabilitation candidates living in rural areas outside urban areas.
Pulmonary dysfunction39 fatigue or muscle weakness40 are the main symptoms of COVID-19-discharged patients. Prolonged inactivity causes muscle atrophy41. In the 2-year long-term follow-up of COVID-19, it was found that the patients had worse exercise capacity than non-COVID-19 patients42. Although rehabilitation has more beneficial effects on muscle strength in critically ill patients43, it is worth noting that, during the COVID-19 pandemic, physical exercise had a bilateral effect, possibly increasing the risk of heart damage and cardiac death during exercise, and even prolonging the recovery period. This means that more care must be taken when formulating the exercise prescription32,44. The change in exercise-related parameters and the correlation of these parameters with each other in the current study support these results. Although the VCG-ST program showed slightly better recovery than MAG-AT, the inexpensive and easy method of MAG-AT also proved to be beneficial. At this point, we can assume that both applications can benefit individuals who cannot attend face-to-face checks frequently, including candidates residing in remote or rural areas. Although the telerehabilitation method is often chosen based on the technology skills of the candidates, the videoconferencing method may be preferred for its group application options, which allow for instant follow-up, particularly in the program management of risky and vulnerable groups.
Telerehabilitation, which proceeds according to patient tolerance and includes mixed protocols with pulmonary rehabilitation, may be an effective and safe method to eliminate the long-term effects of COVID-1924,45. In this study, telerehabilitation programs included breathing, aerobic, and strengthening exercises of varying intensity. An exercise program was prescribed according to each patient’s response to exercises; all patients were followed up with tight weekly controls: the exercises given to the patients in both groups were first performed under the control of the physiotherapist, and the program was modified weekly. In addition, both groups received regular motivational interviews. No adverse events were experienced during either telerehabilitation program. According to the present study results, it can be said that both the VCG-ST program and the MAG-AT program are safe in COVID-19 cases discharged from the hospital.
A meta-analysis by Huang et al aimed to investigate the effectiveness of telerehabilitation for COVID-19 patients and survivors. Moderate to very low quality evidence suggests that exercise programs with telerehabilitation may be an effective and safe solution for patients recovering from COVID-19 in reducing dyspnea, improving lower extremity muscle strength, and increasing ambulation capacity16. Turcinovic et al reported an improvement in mobility in their study, which used a hybrid telerehabilitation protocol with hospitalized patients face-to-face and via a telehealth platform46. Stavrou et al reported that 8 weeks of unsupervised exercise rehabilitation significantly changed oxygen saturation and heart rate during the 6-minute walk test (6MWT), dyspnea post-6MWT, and 30 s STS in discharged COVID-19 patients47. In the current study, besides physical activities, the lower extremity muscle strength of the patients was evaluated. At the same time, 30 s STS was determined as exertion, and the oxygen saturation, heart rate, dyspnea, and fatigue of the patients were measured at rest and after exertion. Significant improvements were observed in the long-term follow-up with both groups in terms of the 30 s STS, physical activity, and also resting and post-exertion oxygen saturation, heart rate, dyspnea, and fatigue parameters (p<0.01). As a striking finding, approximately 93% of participants in the VCG-ST group achieved MCID with early 30 s STS results. This finding shows that VCG-ST provides a faster gain in the early period. Similar positive gains were maintained in long-term outcomes, and no adverse events occurred. Patients with accessibility issues can benefit from safe approaches such as synchronous and asynchronous training programs after discharge, given the fatigue and deterioration in effort levels in patients experiencing the disease.
In a randomized controlled trial, Li et al investigated the effect of telerehabilitation on discharged patients. Compared to a control group that received short educational instructions, an unsupervised 6-week home exercise program via a smartphone, which offers breathing control, thoracic expansion, aerobic exercise, and strength exercise, provided significant improvements in 6 MWT, quality of life, and dyspnea22. In the acute phase, as a result of the 7-day breathing exercises given through a video conference telerehabilitation versus the control group, it was determined that there were significant changes in multidimensional dyspnea, 30 s STS, and Borg score23. It has also been reported that videoconference telerehabilitation provides significant improvement in 30 s STS and shortness of breath in the subacute phase26. In the current study, interaction effects between group and time occasions were significant in physical activity level, but not significant in oxygen saturation at rest, and post-exertion oxygen saturation in favor of VCG-ST. A difference was determined in the between-group effect in oxygen saturation at rest and oxygen saturation after exertion, but the difference in physical activity level was similar. Although the MAG-AT group’s patients showed more adherence to the study, videoconferencing telerehabilitation was slightly superior. The reason for the improvement in oxygen saturation values at rest and after exertion in the patients in the VCG-ST group may be the more effective learning of breathing exercises. Similarly, more physical activity may be due to regular meetings and more motivation. Other factors include better observation of non-verbal cues and better clinical evaluations (eg evaluation of breathing effort) in patients in the VCG-ST group48.
These studies, in the literature, and present study findings have proven the benefits of telerehabilitation in the acute, subacute, and chronic periods. As the availability of affordable devices and software increases, the contribution of telerehabilitation to therapeutic processes may be greater49. Those who have transportation and financial obstacles to receiving health services, especially in rural areas, should benefit from the service of telehealth50. This study demonstrated that both telerehabilitation methods yield positive gains in both subjective and objective parameters related to exercise. Fatigue and dyspnea, which are subjective parameters, can give the clinician an idea about an individual's adaptability to daily life. The improvement in the oxygen saturation and heart rate parameters after rest and exercise is good evidence for the positive effects of the training program on the cardiopulmonary system. Furthermore, 30 s STS provides objective information about lower extremity muscle strength and performance, and both groups showed very good improvement.
In the current study, both groups achieved a high MCID rate at the end of the program, and it can be recommended that the cost-effective method be preferred. Unfortunately, the lack of cost analysis was a limitation of the study. Nevertheless, we think that the MAG-AT method may be cheaper than the VCG-ST. Even though oxygen saturation measurements show that VCG-ST is better, both methods improved the parameters that were looked at. In a videoconference telerehabilitation application, a specialist must accompany the patient synchronously, and the patient must be ready in front of the screen at the specified time. We cannot claim that this method has a positive effect on the working hours of healthcare professionals, but it eliminates the difficulty of the patient reaching the treatment center. It may also be beneficial for elderly people with cognitive problems who are less compliant with methods that require technological knowledge, such as mobile applications. MAG-AT, on the other hand, allows a participant to join the specified program at the desired time. For the low cost required for the application subscription on the patient side, it can save time in the clinic for healthcare professionals and allow them to reach more patients. This point may be the subject of further research.
The lack of a blinded evaluator was another limitation of this study. This deficiency was attempted to be remedied by having the statistical analysis performed by a researcher blinded to the study. Additionally, the limited number of participants was outside our target. Our aim was to include as many patients as possible in the project, but the number of cases that met the inclusion criteria and volunteered within the specified time period was below our expectations. When we performed a posthoc power analysis according to resting oxygen saturation at the end of the study, we found that the study power was 86%.
Our study is important in terms of showing the effects of two new program types on exercise and functionality for individuals with limited access to hospitals and clinics. We believe that conducting research on the design of new studies, which can further enhance the positive outcomes identified in this study, can contribute to an increase in the participation of individuals of all ages, particularly those residing outside the city center and those who live alone, in active living. In order for health professionals to access more participants with less time, future studies could concentrate on evaluating the effectiveness of the VCG-ST program, which could serve as group education. In addition, the effectiveness of these methods can be investigated in cases with comorbidities of varying severity.
Conclusion
This study was proved the positive effects of two different telerehabilitation methods on activity, functionality, resting, and post-exertion hemodynamic parameters at long-term follow up. The VCG-ST results were slightly better; conversely, adherence to MG-AT programs was higher. Potentially life-threatening multisystemic diseases, like COVID-19, restrict individuals’ participation in active life, leading to an increase in their inactivity rates. Telerehabilitation programs are safe, useful, and relatively inexpensive ways to improve symptoms like effort-related dyspnea and fatigue, as well as cardiac hemodynamic parameters and lower limb functionality during the recovery process for people who live outside of the city center, have trouble getting to a clinic, or are at high risk of infection. Future studies may examine the effectiveness of different telerehabilitation methods and their superiority over each other.
Acknowledgements
The authors express their gratitude to all participants in this study.
Funding
This study was funded by Marmara University.
Conflicts of interest
The authors declare no conflicts of interest.


