Introduction
Low back pain is an international public health issue affecting over half a billion people worldwide. Globally, low back pain is the greatest contributor to years lived with disability1,2. The burden of low back pain related disability is increasing, particularly in low- and middle-income countries, where the rise is the most pronounced due to fragile health and social systems1,3. Up to 95% of those suffering from low back pain are diagnosed with non-specific low back pain because no patho-anatomical problem can be identified4. Low back pain is a complex biopsychosocial condition influenced by many factors such as cognitive (eg negative beliefs), psychosocial (eg depression) and social (eg culture) factors. These factors have been identified as important contributors to low back pain disability as well as mediators and moderators of treatment efficacy for low back pain1,3,5. However, use of opioids, surgery and injections is inappropriately high in the general population without significant improvements and in contrast with the evidence-based recommendations5. Furthermore, low back pain is partly iatrogenic and exposure to healthcare practitioners (HCPs) with biomedical orientation can be harmful, possibly increasing long-term disability. These findings have been reported in both the western population and Indigenous Peoples6,7.
It is estimated that Indigenous Peoples constitute approximately 5% of the global population. Disproportionately, they represent around a third of the world's population living in extreme poverty8. It was previously thought that Indigenous Peoples would be buffered from the disabling effects of low back pain due to their cultural beliefs9, but recent qualitative research suggests otherwise3. Low back pain is a highly disabling burden in Indigenous Peoples and is further compounded by the presence of comorbidities3,7. Furthermore, many risk factors for low back pain are present in Indigenous Peoples such as worse overall health and social outcomes compared to non-Indigenous Peoples3,10.
When Indigenous Peoples seek care for their low back pain within the western healthcare system, they face numerous and unique barriers11-14. The experience is often unhelpful, leading to a long-lasting negative impact on Indigenous patients7,11,13. Many Indigenous Peoples around the world have a traditional medicine knowledge system that has been passed down through generations15,16. These practices are deeply rooted within the culture of Indigenous communities. Traditional medicine has been historically used to treat various diseases including low back pain15,16.
In 2017, the Community Oriented Program for Control of Rheumatic Diseases protocol (COPCORD) was executed in Suriname to provide the first insights into the burden of musculoskeletal diseases17,18. Suriname is a multi-ethnic, middle-income country in South America with cultures from all continents. The COPCORD Suriname study showed that low back pain is a highly prevalent health condition in Suriname, with more negative beliefs present among inhabitants of the rural areas than in urban areas18. Furthermore, treatment seeking was more prevalent among Indigenous Peoples18. Even though this research provided a first perspective into the burden of low back pain in Suriname, research suggests quantitative questionnaires may not be valid for Indigenous Peoples as they lack cultural validity, and abstract scales are hard to interpret for Indigenous Peoples12,19,20. Qualitative methods can gain a rich insight into the experience of illness, attempting to understand the data through an Indigenous cultural lens19,21. The aim of this study was to explore the experience of low back pain and the care-seeking process within a Kalinya Indigenous community in Suriname.
Methods
Setting
The research was undertaken in Galibi, the biggest Kalinya Indigenous village (approx. 600 inhabitants) in the north-east of Suriname. The village is in a rural area at the mouth of the Marowijne River on the border with French Guiana (Fig1). Galibi is only accessible by boat, with limited access to goods and services. Electricity is present between 7 pm and 11 pm if fuel is obtainable, and no running water was available at the time of the data gathering. The main source of income for the village is fishing, selling vegetables at the market, and tourism22.
A trained nurse, employed by the regional health services and with limited equipment, is the only HCP present in the village. For a visit to the GP, inhabitants need to travel by boat for 2 hours to Albina, the capital of Marowijne. Most HCPs such as physical therapists and medical specialists are located in the capital, Paramaribo (travel time approx. 5h).
 Figure 1: Location of Galibi, Suriname.
Figure 1: Location of Galibi, Suriname.
Study approach and design
This qualitative study adopted an interpretive perspective. This approach acknowledges that the reality of low back pain is constructed by those who experience it, shaped by their daily interactions within their immediate and broader social world23. A clinical ethnographic approach was used to understand the relationship between the lived experience of an illness (the bodily experience and know-how) and the illness as domesticated and understood theoretically and ‘scientifically’ by medicine24,25. Researchers were tasked with interpreting the lived experiences of Kalinya Indigenous Peoples with low back pain within the context of current understanding of low back pain. The biopsychosocial model was used as a theoretical framework to guide this inquiry1 and the Andersen Behavioral Model of Health Services Utilization was used as a sensitizing framework for care-seeking behavior for low back pain26. During the study, respect for the culture and tradition of Kalinya Indigenous Peoples was paramount.
In 2017, the COPCORD protocol was executed in Galibi over a period of 2 weeks18. Following this, a revisit was conducted in 2019 to fulfill the commitment made in 2017, presenting the COPCORD study results to the inhabitants of Galibi as requested by traditional authority and part of our pledge to give back to community. As a result of this previous research project a relationship already existed between the researchers and this Indigenous community.
Information was gathered during a 2-week period in March 2020. This visit marked the first of several planned for 2020 as part of a new qualitative study on low back pain and the influence of migration. When the researchers arrived at Galibi, a krutu (traditional meeting with local traditional authority) was organized to discuss practical issues and daily execution of the research project within the village. After this, participants were informed by the traditional authorities and their representatives by word of mouth. Using snowball sampling, additional participants were identified through family and social networks of participants and evaluated on eligibility during the data gathering in the 2-week period27.
Eligible participants were Kalinya Indigenous Peoples (at least three of the four grandparents needed to be of Indigenous descent based on the method mentioned by Khrisnadath et al28) with current low back pain with or without leg pain.
The data were generated through in-depth, semi-structured interviews. The language used was Dutch or a mixture of Dutch and Sranan Tongo (an informal language spoken in Suriname). Participants had the option to do the interview in the Kalinya language, but all participants were fluent in Dutch and/or Sranan Tongo. The interviews were audio-recorded and lasted between 40 minutes and 1.5 hours. After each day, researchers discussed the information obtained during the interviews, and key informants were consulted if needed. Some participants were interviewed a second time if the researchers identified missing information. During the stay in the village, observations of inhabitants were systematically recorded as field notes.
Although the research project in Galibi had additional research goals, information-gathering was prematurely halted due to COVID-19. We as researchers felt confident data saturation had been reached on topics discussed in this research article as participants responses ceased to introduce novel themes or insight, indicating a comprehensive exploration of the subject matter.
Data analysis
A thematic analysis method was chosen to analyze the qualitative data, hereby building an in-depth description and interpretation of low back pain in the Galibi Indigenous community. Based on methodological literature, the structure of the qualitative data analysis relied on a complementary and pragmatic set of guiding principles29,30 and adopted an iterative process.
Interviews were transcribed and compared with field notes (and memoranda) of the first author to identify points of convergence and divergence. The field notes were used to annotate the interview transcripts, adding comments, observations and insights. These annotations contextualized the data and provided additional layers of interpretation. In-depth data analysis was done by two researchers using NVivo R1/2020 v1.7.1 (Lumivero; https://lumivero.com/products/nvivo). First, the researchers familiarized themselves with the raw data to improve effectiveness and efficiency of the in-depth analysis. Second, both researchers separately identified key topics during the process of initial coding. After discussing the key topics and reaching agreement, both researchers reduced the elaborated codes into themes by searching for common elements or patterns. Themes were evaluated and reviewed in order to categorize subthemes and higher-order themes. Last, a network of subthemes and higher-order themes was created to visualize their interrelationship. Through this collaborative approach, we mitigated individual biases via researcher triangulation. By bringing together these perspectives, including an independent researcher who did not partake in the data collection process, we ensured a more robust and impartial exploration of the data, enhancing the reliability and credibility of our findings.
Ethics approval
Approval was granted by both the Ministry of Health (ethics approval number CMWO2019_15) and the local traditional authority of Galibi prior to the start of the project. During the first engagement with a participant, a representative of the traditional authority was present to facilitate the interviews and give context to make participants feel ‘secure’ during the interview. Before every interview, written consent was obtained.
Results
Twelve people (Kalinya Indigenous Peoples) participated, aged between 23 and 69 years. Five participants were male and seven were female. An overview of the participants is in Table 1.
Table 1: Demographics of study participants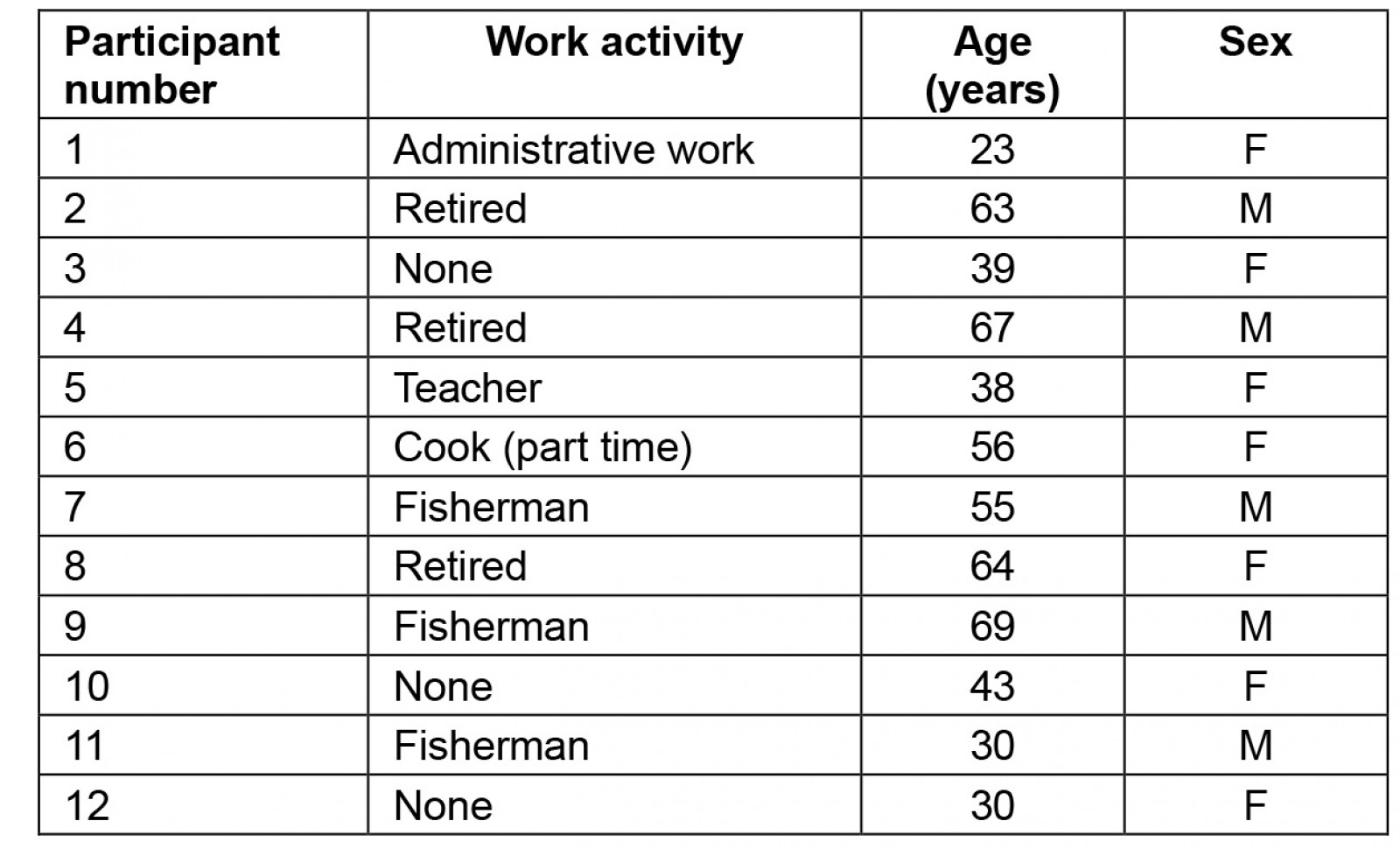
Impact of low back pain
Impact of low back pain on activities of daily living: All 12 participants reported activities of daily living (ADLs) related to the Indigenous way of living such as fishing or working and on the land as aggravators of their low back pain.
When I start to work [fishing], it is going to be painful, especially at night when I lay down. I can do it, but it is very taxing and requires a lot of effort. It is very physical work. But I must do it otherwise I can’t eat. (Participant 11)
I have to carry the water [buckets] … the pain gets double, but I can’t change that. (Participant 12)
In Galibi, the ground consists of loose beach-like sand. Carrying heavy loads such as firewood is done with a traditional basket on the back, secured with a band to the forehead. Wheelbarrows are seldom used because of the loose sand. Continuing ADLs was essential for (economic) survival as no social security is present.
We, as women work hard, and some movements or activities cause pain ... for example rasping tapioca or carrying firewood … It’s because of the traditional basket, it can store a lot of firewood and it is heavy … Men can get low back pain from clearing the jungle with a machete or collecting coconuts by climbing in the tree. (Participant 3)
If possible, I would do less (during the day) to reduce the pain … but I am alone, there is no other help … so I work the whole day and evening as well. (Participant 6)
Impact of low back pain on sleep: Half (6/12) of the participants had problems with getting to sleep or waking up at night due to low back pain.
I can sleep, but I have pain in my back. I have to try to lie down onto my belly, afterwards on my side … then the other side … than on my back until I fall asleep. Once I fall asleep ... I sleep well. (Participant 2)
If I have low back pain, I have trouble lying down on the bed. I have to lie down in a specific position, usually on my side. If that doesn’t work, I go lay down in the hammock and rest in there. (Participant 5)
If the low back pain intensity is high, I have to get up at night and walk a bit, then I go back to sleep … In one night, I wake up maybe 3–5 times. (Participant 11)
Impact of low back pain on emotional wellbeing: Low back pain was an emotional burden in two-thirds (8/12) of the participants. Participants described negative emotions including anger, grumpiness, anxiousness and worrying. The reason reported for anger and grumpiness was attributed to the pain itself, mostly when participants had an episode with high pain intensity.
Participant 1 preferred to keep pain and emotions related to low back pain to herself. When low back pain intensity was high in combination with other (stressful) factors, she would snub people due to frustration of the pain.
What I noticed in the past 8 years about myself. I try to act normal and participate in activities of daily living and avoid people noticing I am in pain … Sometimes it happens subconsciousness [sic] that I snub at people at work … I try to control myself but sometimes it is too much … (Participant 1)
Worrying was the most described emotion. Some participants (6/12) expressed fear and anxiousness related to the cause of the pain. They were unsure what caused the pain and were anxious something severe might be present.
I am worried what causes the low back pain … I was talking about it to a friend and said, I am going to do some checkups to see if everything is really ok with my back and lower abdomen. (Participant 5)
What is actually the cause of the pain? ... I still remember what the trained nurse said to me. Maybe it is clotted blood that causes the pain. (Participant 10)
Participants expressed concerns about their future, fearing their ability to do ADLs independently would diminish, forcing them to depend on others.
I think ... What if it gets worse? Am I still going to be able to work? (Participant 6)
I am worried that, later when I get older, and I need to do something … Lift something. I won’t be able do it anymore [because of low back pain] and somebody needs to help me [with household activities]. (Participant 8)
Furthermore, participants were worried about their financial situation and how to provide an income and pay for basic services and needs.
I am a little bit worried; I can’t do specific activities anymore … for example, I can’t finish building my house. Nobody can do it for me because you need money … (Participant 4)
One participant referred to the stress caused in her family by excessive alcohol abuse, which negatively influenced and contributed to her low back pain.
Low back pain is also caused by alcohol that the men drink … It results in stress for the family [dealing with a drunk husband] as well as financial consequences [due to spending all money on alcohol]. (Participant 12)
Care-seeking behavior for low back pain
Participants used a wide variety of both traditional and western care options for low back pain.
Traditional care: Some participants (5/12) in this study described the use of medicinal plants as a form of traditional medicine. Description of the preparation, method and choice of plants varied between participants. Leaves of the plants are either ‘steamed’ (a selection of leaves and flowers were cooked) and the person inhales the damp of the pottage (with a cloth over the head), or ‘dabbed’ (leaves are dabbed or rubbed on a specific part of the body). For low back pain, the focus of the traditional treatment was on pain relief.
We have medicinal plants … you need to dab them on places that hurt … somebody needs to help you because you cannot apply pressure on your back … (Participant 8)
You cook it [the leaves or plants] and then you damp over it … you will feel some relieve [sic]. (Participant 5)
Two traditional healers are present in the village. They are called Piaaiman. A Piaaiman focusses on diseases with a spiritual cause resulting in physical complaints. According to the Piaaiman themselves, they communicate with the spirits of the woods (no use of potions or plant-based recipes) to treat their patients. Only one participant visited the Piaaiman for low back pain. Based on the participants’ statements, low back pain is not a disease of the mind, thus the Piaaiman could not offer any help.
You can go to the Piaaiman when you feel annoyed … but don’t really feel any pain … you don’t really know what it is or why, but you have pain all over your body and it has a spiritual cause. (Participant 8)
I go [to] the Piaaiman but only for spiritual problem but not for low back pain because low back pain cannot be caused by a spiritual problem. (Participant 1)
I went to the Piaaiman to get treatment [for other complaints] but he didn’t treat my back because low back pain is a doctor’s disease. (Participant 11)
Western health care: Participants visited a diverse range of western healthcare options. Every participant had consulted a HCP at least once to address their low back pain. According to participants, the trained nurse only provided pain medication for low back pain.
The trained nurse only provides painkiller … they help for a while, but afterwards the low back pain returns. (Participant 8)
Access to other HCPs was influenced by logistical and financial barriers. Inhabitants of Galibi try to combine non-urgent visits to HCPs outside the village with other duties and obligations. Thus, visits to HCPs were limited. When participants visited a HCP outside the village, the experience was often negative. Lack of advice, treatment or a diagnosis left participants wondering and worried about their low back pain. According to participant 1, she underwent a surgical procedure for which a lumbar puncture for anesthesia purposes was needed. During the follow-up visit, she addressed her low back pain but received limited information from her HCP.
Because of the lumbar puncture, I suffered from low back pain … I told the specialist I suffered from low back pain after the surgery. The doctor told me there is not much they can do for me; they only could prescribe pain medications to reduce the symptoms … (Participant 1)
Participants shared their recollections of (lack of) information and diagnosis given by HCPs of many years ago, underscoring the long-lasting impact of HCPs on their patients.
I went to a specialist in the hospital in the capital when I suffered from low back pain after my husband had hit me. They took an X-ray of my back and told me everything was fine … but I was suffering, I even cried from the pain ... After that I never went back, and the low back pain stayed. (Participant 12)
I want my low back pain to improve ... I do not think it is going to happen because there is no medication …The doctor gives pills, they help against the pain but not against the cause of low back pain … I don’t know what the cause is … (Participant 7)
The general practitioner had done assessment of my back and told me my spine had moved and pushed against the nerves. So, when I play soccer, the spine pushes against the nerve which causes the low back pain … They cannot do anything about it. (Participant 11)
Massage therapy was another treatment option used by most of the participants (9/12). Among these nine participants, six individuals elaborated on this by highlighting that massage therapy offered temporary pain relief during periods of high pain intensity. These massages were administered by spouses or family members.
The pain comes when my spine gets flatter … when my wife massages my back, it gets longer again … you notice it, if somebody massages you … you hear it ‘crack’ and everything goes back in the correct place. (Participant 9)
Additionally, four participants mentioned the utilization of whole-body massage therapy as a treatment option for low back pain, provided by massage therapists in Paramaribo, the capital of Suriname. This treatment did not focus on low back pain specifically but did improve their outcome with low back pain.
When I am in the capital, I go to a lady who does massage therapy [for the whole body]. When I am here [in the village] and I have severe back pain, my husband massages me and I see my low back pain reduces. (Participant 8)
A person’s choice of care assumingly reflects their beliefs and opinions about low back pain31. When asked why they suffered from low back pain, almost all participants (10/12) referred to the workload regularly put on their bodies during their lifetime by the Indigenous way of living, eventually resulting in suffering from low back pain and other musculoskeletal diseases.
Due to working hard when I was younger, I got low back pain … I had some accidents when I was younger such as a tree falling on me … I didn’t have low back pain at the time, it only came later due to getting older. The ‘machines’ in my body don’t work that well anymore due to hard work. If I had worked less hard, it would have been better. (Participant 14)
We, as women work hard and some activities cause pain ... for example rasping tapioca or carrying firewood … Men can get low back pain from clearing the jungle with a machete or collecting coconuts by climbing in the tree. (Participant 3)
One participant described that low back pain is unavoidable for Indigenous Peoples who lead a traditional Indigenous way of life and suggested a relationship between the amount of hard work done and number of musculoskeletal complaints.
Most people will eventually develop [musculoskeletal] complaints. If not, they maybe have not worked so hard. I, myself didn’t have to work that hard when I was younger as I had the opportunity to go to school [secondary school in the capital]. But those who stayed in the village and helped their parents … (Participant 8)
Only one participant mentioned clearly a non-biomedical cause of low back pain, namely stress due to alcohol abuse of family members.
Low back pain is also caused by alcohol that the men drink … It results in stress for the family [dealing with a drunk husband] as well as financial consequences [due to spending all money on alcohol] … (Participant 11)
Discussion
Impact of low back pain
Low back pain has an impact on different aspects of life such as ADLs, sleep and emotional wellbeing. Participants in this study hold strong beliefs that the strenuous manual labor (related to the way of living of Kalinya Indigenous Peoples) is a significant contributor to low back pain. The attitude of the inhabitants was to endure low back pain to assure financial security. Similar findings have been reported in other Indigenous communities19,32,33. Indigenous Peoples state that traditional physical labor plays an important role in the development of musculoskeletal complaints (including low back pain) and, as a result, perceived it as unavoidable in their traditional way of living34. Furthermore, acceptance of musculoskeletal pain within their traditional way of living could possibly result in underestimation of the true burden of low back pain, especially using quantitative research methods that lack cultural validity12,19,32,33.
Sleep disturbances due to low back pain were reported by six participants. Research indicates sleep problems are common in patients with low back pain, with an estimated prevalence of 50–60%35. Furthermore, sleep disturbance can negatively influence low back pain intensity and is a predictor of poor recovery from low back pain36. Future research is needed to determine whether sleep improvements lead to pain reduction. Research on sleep in patients with low back pain is limited and none of the participants in these studies were Indigenous Peoples. However, good quality sleep is crucial, and its disruption can have serious consequences on overall wellbeing37.
The emotional impact of low back pain was significant as participants expressed feelings of worrying, anger and anxiousness about the future and cause of the pain. Cognitive and emotional factors such as pain-related fear, anger and psychosocial distress are known to be contributors to low back pain disability and have also been observed in other Indigenous Peoples with low back pain1,19. According to the fear avoidance model, unhelpful beliefs can induce pain-related fear, which can lead to avoidance and disability38,39. Furthermore, a theoretical link between anger, the experience of injustice and disabling pain has been suggested in the literature40. More research is needed into this association given the injustices and discrimination against Indigenous Peoples8,10. Participants in the present study expressed mostly biomedical perspectives regarding the origin of their low back pain. They attributed their discomfort to structural vulnerabilities and anatomical factors affecting their spine. Biomedical-oriented beliefs are considered negative beliefs5. Thus, the emotional burden observed in this study may, in part, be explained based on the fear avoidance model38,39. More research is needed into the link between emotions and perception of injustice in Indigenous Peoples suffering from disabling pain.
One participant displayed her anxiety about the social effects on the family due to excessive alcohol use. The local traditional authority of Galibi confirmed the excessive alcohol use and its social effects on family and the society/community. The link between alcohol abuse and pain is complex and multifactorial41. Alcohol use has several negative health effects including poorer general health, sleep disturbances and mental health problems, increasing the risk of low back pain1,41. Not only the individual struggling with alcohol is affected but also their family members due to psychosocial and financial consequences. An alcohol-abusing individual may trigger stress, anxiety and depression in other family members, which can permeate family dynamics and relationships contributing to the burden of low back pain42.
Care-seeking behavior
Apart from a certified nurse available in their village, Kalinya Indigenous Peoples must undertake a boat journey of minimum 2 hours to seek medical care from a medical doctor. For more specialist care, travelling to Paramaribo is necessary. The expenses associated with travel and accommodation can be significant and could possibly be a financial burden for Indigenous people suffering from low back pain. These geographical and logistical barriers in accessing healthcare services are not unique to Kalinya Indigenous Peoples. This has also been observed among other Indigenous communities worldwide11,43.
When participants consulted their HCPs for low back pain, the experience was often negative and unhelpful. Due to lack of information and education about their low back pain or a more biomedical-oriented diagnosis, patients were left with negative beliefs and anxiety related to low back pain. Lin et al demonstrated that in Indigenous Peoples this can contribute to long-term, disabling low back pain7.
To help Indigenous people suffering from low back pain, HCPs should adopt an engaged strategy that prioritizes psychosocial factors, education and improving function within a healthcare setting with cultural adaptations5,44. These cultural adaptations should include attention to language use and understanding of context by knowledge of history of Indigenous Peoples44,45. Therefore, easily accessible, culturally adapted information about low back pain in line with the current guidelines could be beneficial, decreasing the reliance on physical and western health care as well as strengthening positive beliefs about low back pain46.
Massage therapy by spouses overcomes some of the logistical barriers but research suggests this is not an effective treatment of low back pain, with only short-term results47. However, massage therapy as utilized by Indigenous Peoples may exhibit variations in its application, usage and cultural meaning compared to western populations.
A wide variety of traditional medicines were applied by participants in Galibi. Traditional care methods centered around pain relief, often employing techniques such as steaming or application of leaves from medicinal plants. Use of traditional medicine is deeply rooted in cultural practices in the Indigenous Peoples in Suriname16. Combined use of allopathic approaches with traditional medicine has been reported by other Indigenous Peoples around the world32,33. For example, Indigenous Peoples in India use kadhas (herbal medicines) or allopathic medicine to treat low back pain caused by ‘bad or impure’ blood33.
Despite its unique advantages such as cultural importance, accessibility and community support, traditional medicine remains a relatively underexplored area of research. There is need for further investigation to determine if traditional medicine has the potential to function as a secure and economically viable addition to health care that can help reduce the burden of low back pain48.
Strengths and limitations
A strength of this study is the use of qualitative methods to explore impact and care-seeking for low back pain. If done correctly, qualitative research allows for a more in-depth exploration of participants' perspectives19. This is particularly important when considering the potential for misrepresentation of abstract scales, often used in quantitative questionnaires, which can be challenging for Indigenous Peoples12. Some quantitative methodologies, such as COPCORD, have addressed this issue by incorporating research on cultural validity and adapting their quantitative questionnaires11,20,49,50. As both qualitative and quantitative methods possess unique strengths and limitations, incorporating cultural validity is essential for accurate data collection in research involving Indigenous Peoples.
A limitation of this study is that for logistical reasons all researchers except for one were not Indigenous. Increasing the presence of Indigenous researchers in these studies can only enrich the depth of the research and foster greater community engagement. In the present study, explicit attention was given to cultural security. Meetings with the local traditional authority and key informants prior to and during data collection were implemented. Since all researchers and participants spoke both Dutch and/or Sranan Tongo, no language barrier was present and participants could speak freely.
Conclusion
Low back pain is a burden for the Kalinya Indigenous Peoples of Galibi, impacting different aspects of their lives. These findings shed light on the unique experiences and challenges faced in managing low back pain by a Kalinya Indigenous rural community in Suriname. This study’s use of a clinical ethnographic approach emphasizes the need for cultural sensitivity in research on low back pain among Indigenous Peoples. More research is needed on impact of low back pain and care-seeking behavior in Indigenous Peoples to develop effective strategies. Without better insights into these topics, improving health outcomes and reducing the disability associated with low back pain becomes a challenging endeavor.
Funding
The authors acknowledge the financial support by the Research Foundation Flanders (FWO), Belgium, granted as a fundamental research PhD Fellowship for Yano Truyers (project number 11H2224N).
Conflicts of interest
The authors have no conflicts of interest.

