Introduction
Community paramedicine is a new field that embraces a paramedic's knowledge, expands their scope of practice, and implements them in a community and home health aspect. Utilizing the advanced knowledge and technical skills of paramedics in the aspect of home health care, community paramedics expand the role of home health nursing for a more affordable cost to patients and healthcare systems. Community paramedicine allows paramedics to function outside their traditional emergency response roles to improve access to primary and preventative health care1. The community paramedicine concept is becoming widely used in rural communities to assist in maintaining and improving healthcare disparities. An aging population, urbanization, and healthcare worker shortage leave rural areas more vulnerable. In rural areas, community paramedics can help fill gaps in the local healthcare delivery systems. In extending their scope of practice, paramedics use their knowledge and skills beyond emergency health response to introduce preventative and rehabilitative health2.
A review of nearly 100 studies from across the globe summarized that community paramedicine demonstrates an apparent lack of research and understanding of the scope of community paramedics as well as an inconsistency of evaluations and an impact on health programs3. Most studies focus on health services outcomes, including 30-day, 90-day, and 6-month hospital readmission rates, 911 emergency number utilization rates, number of emergency department (ED) transports and admissions, and hospital length of stay4. Formal cost outcomes are only discussed in two publications, calculative in Quality Adjusted Life Years and costs-per-visit comparisons5,6. While this initial research has a broad topic, many of these studies have yet to be reproduced or expanded across countries.
Community paramedics provide more than a physical and mental health assessment. Community paramedic visit notes give insight into a patient's home and social situation. These known social determinants of health play a role in the patient's care7. Any of these factors can affect patient care and health recovery. With paramedics being within the homes of the patients, these social factors are in the front of their minds and can help mitigate resources to aid in proper healing, with all factors affecting care taken into account.
Regarding community paramedic practice overall, within the US a study from rural South Carolina showed a reduction in emergency room visits by 58.7% and inpatient visits by 68.8% in patients following their enrollment in a community paramedic program6. A study in Texas found similar results in decreased ED and inpatient hospital admission for those in community paramedic programs8. In preliminary data from a program in Queens and Long Island, New York, 78% of community paramedic responses could be contained in the home and not require transport to EDs9.
A sample of high users of healthcare services with one or more chronic diseases, including congestive heart failure, chronic obstructive pulmonary disease, hypertension, stroke, and diabetes, showed significantly less reduction in quality-of-life scores in community paramedicine services compared to conventional treatment5. In rural-dwelling older adults, a study of emergency medical services in-home assessments showed that 69% of these patients had medication management-related needs that could benefit from community paramedics10. Analysis of these two studies shows there are applications for community paramedics in Midwestern areas known for having larger rural populations of patients with numerous comorbidities.
In current practice, community paramedics function in the out-of-hospital setting with an expanded scope of practice differentiated from traditional emergency medical services or nursing practices. Community paramedics help provide a more cost-effective way to provide follow-up to specific populations, for example postoperative care for patients who have undergone major surgery. A valid option for this kind of postoperative care and possible reduction of rehospitalization lies with patients who underwent a coronary artery bypass grafting (CABG) procedure.
CABG surgery requires a complex follow-up to prevent readmission and ensure proper healing. Patients are often placed on various medications, including blood pressure regulators and blood thinners, in addition to wound care for the surgical site. This care is generally taken by a primary care provider and a cardiologist; however, many postoperative CABG patients utilize EDs and walk-in clinics for care. Studies have shown there to be an almost 12.9% readmission rate following a CABG surgery for circumstances including sepsis, respiratory complications, new-onset cardiac arrhythmias, or new onset chronic heart failure11. Smaller studies regarding the use of nurse practitioners have been performed, and statistically significant decreases in readmission rates have been observed, from 11.5% to 3.85% with follow-up care12. Additionally, home care training for patients after CABG significantly reduced the mean anxiety score, heart rate, respiratory rate, and blood pressure in the intervention group compared to controls13. Nurse practitioners are expensive and are in high demand across the healthcare system. Community paramedics can take a similar role and provide follow-up care through home visits with ECG reading, blood pressure, oxygen saturation and weight measurements, physical exam findings (murmurs), medication plans, wound care, eating habits, and sometimes venous blood orders. Community paramedics may be performing the same function as interdisciplinary teams with decreased cost to the patient, decreased cost to the hospital systems, and better patient outcomes overall.
Randomized clinical trials of community paramedics are occurring in Canada14,15. In the US, there is still work to be done. There is a lack of rigorous, longitudinal studies with control groups, resulting in the inability to render conclusions about the value of community paramedic programs with concrete evidence4. Ideally, this can be one of the first studies to open the gate into community paramedicine research, especially in rural areas where these authors believe they would be the most helpful.
This study hypothesizes that community paramedics can efficiently reduce unplanned hospital admissions. This study hopes to show hospitals and insurance providers that funding community paramedics is a cost-effective means of providing patient care by reducing the overall cost of patients in hospitals and strengthening preventative measures. Community paramedics have the potential to offer patients far more affordable bills than those from EDs. By studying how community paramedics interact with certain chronic diseases, starting with postoperative recovery of CABG surgery, a collection of evidence-based practices of community paramedics can be employed to reduce healthcare costs for both patients and facilities.
Methods
This study is a retrospective chart review of existing data collected from electronic patient medical records documented between January 2021 and September 2022.The participant dataset was pulled from Sanford Health OneChart CI-1040 software v100.2406.3.0 (Sanford Health; https://www.sanfordhealth.org/medical-professionals/onechart). From this initial data pull, a manual chart review of the Sanford Electronic Medical Record was conducted to select the participants and controls. The de-identified data utilized for the study was consolidated on a password-protected spreadsheet and stored on a Sanford computer on the Sanford Network, only accessible by researchers on the project.
From January 2021 through September 2022, there was access to 242 total patients who were referred to community paramedicine after receiving a CABG at Sanford Health in Bismarck, North Dakota. A total of 115 participants accepted referrals after the CABG procedure, and 127 patients canceled their visit, were not seen due to schedule concerns, or were outside of the service area. Based on a previous study with a similar aim12, this study would require 160 patients (up to 80 per group). The 242 patients were randomized, and participant review ceased once 80 community paramedic participants and up to 80 controls were identified.
Patients included in the study are those who underwent a CABG between 1 January 2021 and 30 September 2022, who were older than 18 years, with a referral and visit by a community paramedic in the designated North Dakota service area. Control participants are those who underwent a CABG between 1 January 2021 and 30 September 2022, who are older than 18 years, with a referral and without a visit by a community paramedic in the same designated North Dakota service area. Patients who did not meet the inclusion criteria or who met the inclusion criteria but died during the study period were excluded.
Controls were location-matched to the participants within the same distance of 108.7 miles (174.9 km) from Bismarck, North Dakota as participants. This range was predetermined prior to this study for the community paramedic program when deciding on the feasibility of which patients to treat. Location-matching consisted of finding patients who lived in similar towns or within the same distance as study participants. Participants' chart data were analyzed from the surgery date through 180 days postoperative date, searching for the length of initial hospital stay, complications of the initial surgery, visits from community paramedics, ED visits, inpatient admissions, outpatient visits, and walk-in visits. While the study was able to review up to 80 controls, only those who were location-matched to the participants were included in the study.
Chart review consisted of examining the notes for the patient’s CABG operation written by their cardiothoracic surgeon and the discharge note typically written by a member of the cardiology team to assess their initial hospital course. The community paramedic notes were also reviewed for the participants. In looking at readmission and utilization of health care following the procedure, any notes that were designated as ED, walk-in clinic, primary care provider, or cardiology were reviewed in both groups mainly in their ‘assessment’ and ‘plan’ sections of the providers’ note. Dates of procedure, discharge, community paramedics, and any encounter in their study search period for the variety of healthcare encounters tracked in the study were also collected.
SAS Studio v3.81 (SAS Institute; https://www.sas.com) was used to analyze the data in a manner that accounts for the complex sample survey design. Analysis was performed using summary statistics and bivariate comparisons (χ2 tests, proportions tests, and regression models). All significance tests were two-sided, with a p-value less than 0.05 for significance.
Ethics approval
This study was approved by the Sanford Institutional Review Board under the (ID: STUDY00003122).
Results
A total of 80 participants were identified to meet the inclusion criteria of undergoing CABG surgery between 1 January 2021 and 30 September 2022, at Sanford Health in Bismarck, North Dakota who were older than 18 years with a referral and a visit by a community paramedic in the designated service area. A total of 38 controls meet the location-matched inclusion criteria. Table 1 shows the participants' characteristics. A total of 85% of participants were male and 87.5% of the controls were male. The mean ages of both groups were similar at 68.16 years in participants and 65.87 years in controls. The mean lengths of stay were similar in participants versus controls (7.05 v 7.24 days; p=0.7228). Given similar lengths of stay, patients in both groups had similar hospital complications and outcomes. A total of 19 (23.75%) participants and 10 (25%) controls sought out ED care in the postoperative period (p=0.1094). Totals of 46 (57.5%) participants and 21 (52.5%) controls attended visits with their primary care provider during the postoperative period (p=0.8187). A total of 3 (3.75%) participants and 7 (17.5%) controls sought walk-in care during the postoperative period (p=0.0075). On average, participants had 4.83 cardiology appointments compared to the 5.07 appointments per patient in the control group (p=0.5618). A total of 13 (16.25%) participants and 11 (27.5%) controls were admitted during the postoperative period (p=0.6688).
Table 1: Study participant characteristics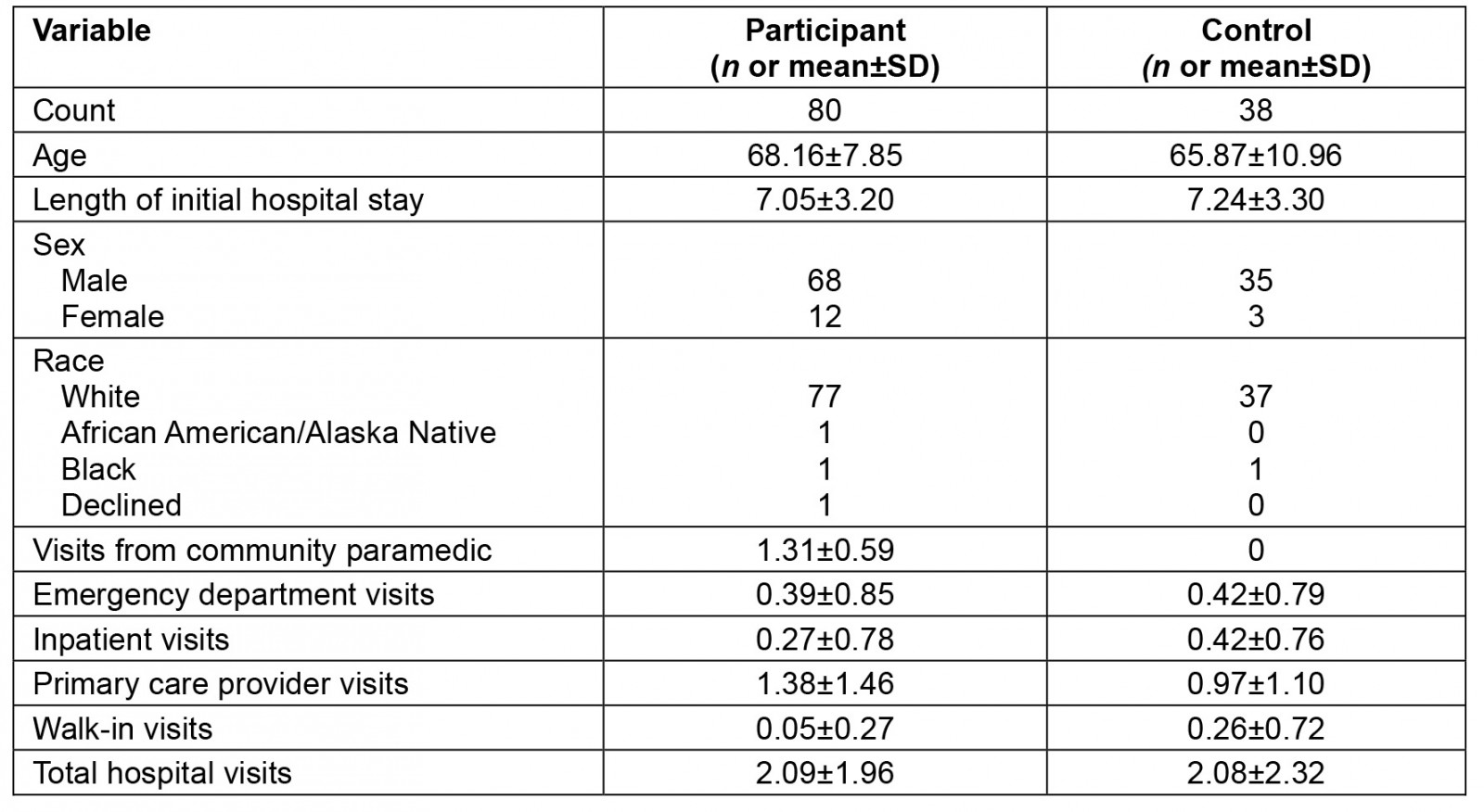
Discussion
This study emphasizes the first 30 days due to the commonality in research as well as the general rule of insurance coverage and reduction programs across the nation16. While many of the inpatient admissions in both groups in happened outside the 30-day post-admission window, participants were admitted to inpatient wards 10 times (45.45%), while controls were admitted five times (31.25%). Within the first 14 days, participants were admitted to inpatient wards six times (27.27%), while controls were admitted four times (25%). Clinically, these first 30 days are crucial for insurance coverage and performance metrics. While there was no statistical significance for this small study, there may be differences that would likely be clear with larger scale studies.
Throughout the study, one factor of significance was found: between the controls and the participants, seven sought medical attention at walk-in clinics (urgent care), while only four did so in the community paramedic group. It was also clinically significant because, in the community paramedic group, no patients sought care in the first 14 days post-discharge, which is the period of time the participants were seeing the community paramedics (average of 3.36 days of post-initial hospital discharge).
Given the limited access to primary care providers across the nation there is a higher dependence on walk-in/urgent care centers17. In patients who saw the community paramedic, the effect of having statistically significantly fewer walk-in visits highlights this effect. In the first couple of weeks post-discharge, patients have new care routines and questions that need to be assessed and answered. By providing a healthcare provider in the form of a community paramedic, these patients are having their questions answered in their home instead of going to walk-in centers.
While a statistically insignificant finding, participants sought primary care providers more than controls. This difference could indicate that, compared to the controls, participants are more likely to seek help or medical advice while also being more involved in their own care. Additionally, a major limitation of this study was a lack of randomizations. Patients were able to refuse community paramedic visits. This refusal of community paramedicine may mean they are more likely to refuse other forms of health care such as primary care provider visits. Given that the participants chose to have community paramedics added into their care, these patients may be more likely to schedule and attend visits with other healthcare providers.
A closer look into the patient notes in charts accessed for this study found that a number of patients could have been seen by a community paramedic instead of their primary care provider. While patients have a limited knowledge of the scope of practice of the new field of community paramedicine, increased awareness could decrease the workload on primary care providers and improve access to that care. While this was not a direct question of this study, the chart review of these patients raises further questions on how best to apply community paramedics to bridge specific gaps in care.
In the rural US, community paramedics could serve as an extension for primary care providers to access those outside of higher-resourced areas. Community paramedics would expand the steps made with telehealth, however, essentially bringing physical care to the patient instead of avoiding it. For this practice to be implemented, further review and development of the scope and practice of community paramedicine would need to be performed.
As it pertains to the cardiology visits, there were many instances when the community paramedic could have been utilized to help reduce the burden on cardiologists. An example of this utilization is that on multiple occasions a patient called into their cardiology clinic, and the community paramedic was contacted to perform bloodwork and a 12-lead EKG on the patient. This appropriate utilization was found to be limited to a few providers, and the underutilization of the community paramedic was still prominent among most cardiology providers. Expanding awareness of community paramedic practices can help other cardiology providers utilize them as a resource. While patient referrals were initially sent by the cardiothoracic surgeon, there needs to be proper communication with the cardiology team as they play significant roles in postoperative care.
There were instances when cardiology follow-up appointments included a 12-lead EKG that could have been performed by the community paramedic. Reallocation of this procedure to a community paramedic would not only save clinic space for the cardiology, but also minimize the travel burden on the patient. The cardiologist visits included blood draws and assessment of the incision site, once again something that could have been done with a visit from the community paramedic, especially in the more acute 14 days postoperatively. With more research on the scope of community paramedics and their effectiveness, future studies should show a significant difference in cardiology visits in postoperative care with and without community paramedics.
Many of the ED visits by participants happened at mean times of 46.87 days post-discharge and 55.94 days post-discharge in the controls. Within the first 30 days, participants sought the ED 17 times (54.83%), while controls sought it six times (37.5%). Within the first 14 days, participants sought the ER 14 times (45.16%), while controls sought it five times (31.25%). This difference may also support the theory that participants were more likely to seek out health care compared to controls. For example, one participant was seen in the ER for peripherally inserted central catheter obstruction, a complaint that may have been handled by community paramedics if the patient was aware of that option. The higher utilization for participants in the ED could be due to being more likely to seek services or it could be due to a higher number of comorbidities, a factor not taken into account in this study. An analysis of comorbidities would be a factor to consider in future research.
The most clinically relevant analysis of this data comes from the chief complaints for the readmissions between the groups. The proportion of patients with readmission rates was 0.71 (participants) versus 0.78 (controls). While no significant difference was present (p=0.3747), when separating the chief complaints from the healthcare visits into physiologic systems, some ideas come to light (Table 2). For the controls, the readmissions were six cardiac, two pulmonary, four gastrointestinal, zero musculoskeletal, and four miscellaneous readmissions. The participant readmissions comprised eight cardiac, two pulmonary, eight gastrointestinal, three musculoskeletal, and one miscellaneous readmission. A total of 8.99% of admitted participants were for cardiac complaints compared to 13.95% of the admitted controls.
Participants were admitted for conditions such as pneumonia, atrial fibrillation with rapid ventricular response, right leg pain requiring exploratory surgery, non-ST elevation myocardial infarction, internal cardiac defibrillator placement, dehydration with syncope, fluid overload causing shortness of breath, chest pain, and pulmonary embolism. Controls were admitted for conditions such as pneumonia, atrial flutter with syncope, cholecystitis, cellulitis at the vein harvest site, and pulmonary embolism. Of these admissions, there was a case of cellulitis of the leg, possibly due to venous harvest sites. Harvest site infections may be able to be taken care of by community paramedics from the patient’s home, preventing hospitalization. While one hospitalization may not have made the difference statistically significant, clinically this reduction in time and cost for the patient matters.
A thorough analysis showed that controls were seen in the ED for cardiac-related issues four times, and the participants were seen eight times (9.09% and 8.70%, respectively). These rates were very similar, and the complaints seen for each of these instances were examples of patients that would be appropriate for community paramedic utilization if that option had been clear to the patient. Given the novelty of community paramedics, patients may not be aware of their services or how to contact them. Additionally, these lesser known healthcare resources of community paramedics may be a reason the controls initially rejected their services. These control patients may not be aware of the benefits of community paramedics or that their services are covered.
Future studies will need to consider the population being served, as people may often ‘snowbird’, travelling to warmer states during the winter. This ‘migration’ is a common practice in northern climates as older populations prefer warmer environments. This habit leads to a gap in their medical records, given that Sanford facilities are typically not present in both locations. Additionally, within this study, the Care Everywhere software (Epic Systems; https://www.epic.com/careeverywhere) was not utilized, and this feature may be able to fill the gaps in care seen on the electronic medical records from healthcare facilities outside of Sanford.
In addition to covering the effects of snowbirding, expanding the geographical region would increase the sample size. This issue was immediately hindered by the range of the community paramedics' practice area, predetermined prior to this study. Increasing the time of chart review would also increase the sample size. The hope with future studies is that community paramedics could serve as an additional bridge to fix gaps in care that are intrinsic to rural populations.
While visits for anticoagulation were not tracked in the study, three patients still utilized warfarin for anticoagulation in their postoperative care and required frequent visits for laboratory testing. Community paramedics can help provide international normalized ratio (INR) checks at home for patients with a lack of mobility and access to health care. With the increased access to non-warfarin anticoagulation medication, warfarin is becoming less common; however, there are still indications for INR checks. Most often, non-adherence is due to lack of access, which is a common barrier for rural patients. With increased access to community paramedics, providers can continue to bridge gaps in care.
Overall, it seemed that community paramedics were often underutilized by patients either due to a lack of awareness of their specialty or a lack of referral by providers who may not be aware of this new option. With this thin crossover of the margin of error, it can be inferred that those few patients where the community paramedic was underutilized would lead to data showing significant effectiveness of – and, more importantly, clinical relevance and increased patient satisfaction with – proper use of the skills of community paramedics.
This study has many limitations. Care Everywhere software was not used to assess visits outside of the Bismarck Sanford Health System. Utilization of this feature could have expanded the reach of participants who are not consistently seeking care in Bismarck and may have more visits within the healthcare system than appear on their Sanford charts. Given the colder climate of North Dakota, many people in this study's participant group travel to warmer climates for the winter months. For some participants, gaps in their medical records were present, typically between October and March. These participants were still included if they met inclusion criteria; however, this may cause a skewing of the data due to missing healthcare visits over a prolonged period of the 180 chart review days.
Of all patients referred to the Bismarck Community Paramedic Program, approximately 58% accepted the referral in 2021. Those patients who did not accept the referral or canceled their appointment were put into the control group. This biased participant selection needed to be a proper stratification of participants, given that those who denied control might be more likely to deny healthcare appointments in general. Additionally, those who accepted care from the community paramedics may be more likely to seek medical guidance in general. Due to the lack of randomization, there is a considerable limitation in being able to compare our participants and controls appropriately. These factors call into the need for participant enrollment as a prospective study or a larger geographical area of rural residents to be able to include more study participants for a proper characteristic analysis of one participant group.
This article outlines the first data analysis of an ongoing study. This population of patients undergoing CABG procedures and being referred to community paramedics continue to be tracked and assessed. With a higher sample size in the coming year, more detailed statistical analysis will be conducted. The community paramedic program at Sanford is also undertaking new care programs relating to congestive heart failure and hyperemesis gravidarum in order to assess the community paramedic’s effectiveness on patient care throughout patient populations.
Table 2: Systems-based analysis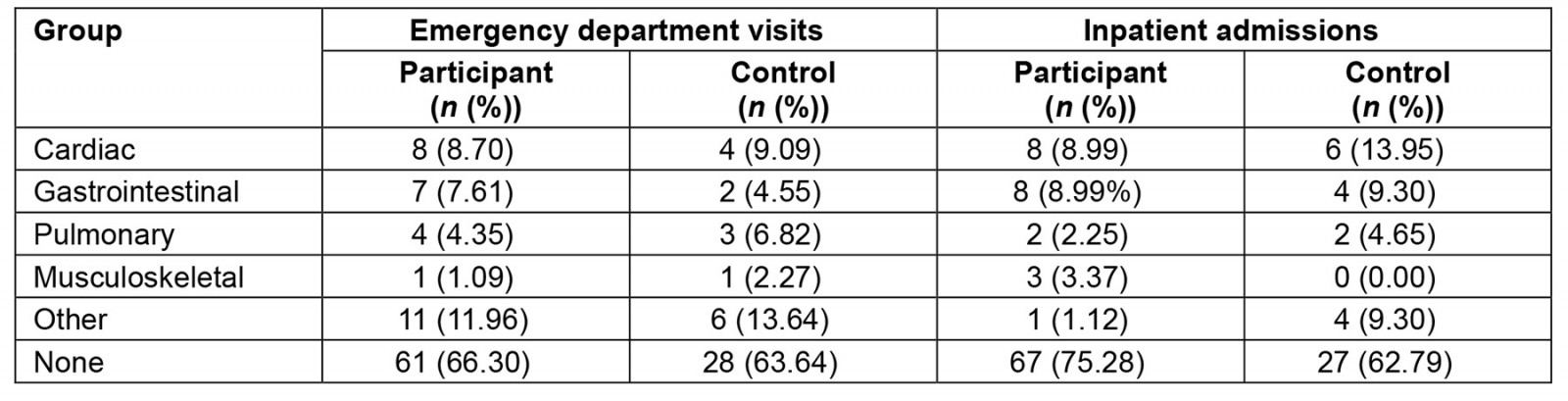
Conclusion
With this being an initial study of community paramedics in the field of postoperative care, proper randomization in future studies is necessary to draw comparisons between the two groups. However, the study does show that community paramedics can play a role in postoperative care, especially in the case of CABG recovery. Further steps must also be taken to avoid the biases encountered in this study in order to increase the statistical significance and power of patient analysis. Future studies can also provide a more in-depth assessment of the community paramedic's effectiveness in improving any population's health. Future studies should include proper randomization instead of a pseudorandomization of patients into the control group, given that they denied community paramedics’ care. Expanding to larger geographical areas that cover a large population of rural residents could put these changes into effect to clearly show the differences that community paramedics can make in patient care. The benefit of studies on community paramedicine is to show insurance companies and hospital systems that coverage and support of community paramedics can dramatically decrease the overall cost of health care to everyone involved.
References
You might also be interested in:
2020 - Decisions on cancer care by Indigenous peoples in Alberta and Saskatchewan: a narrative analysis
2011 - Understanding the rural food environment - perspectives of low-income parents


