Introduction
The biopsychosocial patient-centred approach to care has emerged as a cornerstone in the field of health sciences and is recognized as a standard of quality clinical practice by several disciplines1,2. This holistic approach considers not only the biological aspects of an individual’s condition but also their psychological and social dimensions3. Within this paradigm, the concept of therapeutic relationships has gained prominence as an essential component of therapeutic success4. While the importance of the therapeutic relationship has traditionally been highlighted in psychology and mental health research spanning over three decades, recent and growing evidence highlights its pivotal role in enhancing rehabilitation outcomes as well5-8. The therapeutic relationship is ‘a trusting connection and rapport established between therapist and patient through collaboration, communication, therapist empathy and mutual understanding and respect’4. It is not merely what healthcare providers do but how they engage with their patients that may serve as a mediating factor in determining the success of rehabilitation efforts9.
Relationality stands as a foundational principle of Indigenous cultures globally, underscoring the significance of relationships as the core of Indigenous Peoples’ spiritual and cultural identity10-12. Within the healthcare context, a few psychology and mental health studies showed that the therapeutic relationship is a critical contributor to positive health outcomes among Indigenous populations13-15. However, there are many contextual factors rooted in colonial traumas shaping Indigenous Peoples’ experiences with health care and how they engage with their healthcare providers, including language barriers, lack of cultural safety, abuse and discrimination experienced in the healthcare system16-18.
Telehealth has the potential to enhance access to care barriers experienced by many Indigenous Peoples19,20, but building trusting therapeutic relationships in the virtual scenario poses a potential challenge21,22. This difficulty may arise for varied reasons, including limited ability to interpret non-verbal communication, physical distance, technical issues making the conversation less personable, discomfort using unfamiliar technology, and lack of therapeutic touch23-25. The latter has been recognized as a tenet of the therapeutic relationship in physiotherapy26. Evidence suggests how touch and hands-on care can strengthen the therapeutic relationship by, for example, promoting biobehavioral synchrony (ie when different individuals harmonize their biological and behavioural processes during social interaction through the stimulation of mechanical receptors)27.
In the virtual landscape, prioritizing relationality is imperative, acknowledging the impact of remote service provision on the dynamics of healthcare engagement. Understanding the perspectives of First Nations Peoples (one of the three main Indigenous groups in Canada) on telehealth physiotherapy is vital to ensure culturally safe and effective telehealth care delivery that aligns with their values and preferences and allows for virtual therapeutic relationship building. However, there has been limited research exploring First Nations Peoples’ views on this topic. This is needed in order to develop guidance for organizations and clinicians who provide telehealth physiotherapy care. Therefore, the purpose of this study is to explore First Nations Peoples’ perspectives on telehealth physiotherapy, with an emphasis on the virtual therapeutic relationship.
Methods
Carrier Sekani Family Services (CSFS) is a First Nation-led organization that provides health and social services for 11 rural and remote First Nations in north-central British Columbia (BC), Canada. Through a community engagement process, CSFS leadership identified the need for this research in order to understand best practices for telehealth physiotherapy services for the member Nations.
Context and sampling
Between November 2022 and August 2023, we purposefully recruited 19 First Nations people, 19 years or older, from one of the 10 eligible CSFS Member Nations, in collaboration with CSFS staff and community representatives. The Carrier and Sekani People are the First Nations People of a large portion (more than 76 000 km) of North Central BC. Carrier Sekani First Nations comprises a population of over 10 000 individuals28. Carrier territories are, for the most part, sub-boreal forests dotted with numerous lakes and rivers. The climate is continental, and their traditional way of life is based on a seasonal round. Carrier People maintain a governance system commonly referred to as the bah’lats or potlatch28. Within the Carrier and Sekani traditional territories, distinct groupings maintain geographic and linguistic characteristics different from others. The names of each of the eight communities represented in our sample are Burns Lake Band, Cheslatta Carrier Nation, Nadleh Whut’en, Saik’uz First Nations, Stellat’en First Nations, Takla Nation, Wet’suwet’en First Nation, and Yekooche First Nation.
Although having experience with telehealth and/or physiotherapy was not mandatory, preference was given to those who had received it. Potential participants were informed of the study by clinicians and leadership within CSFS, and the research team contacted those interested by email or telephone call.
Researcher characteristics
One researcher (DPM) conducted all the semistructured interviews. DPM is a Latin-American White woman and a physiotherapist who moved to Canada to pursue her doctoral degree in 2021. She was trained in Western research methods and has been learning with great humility about Indigenous Peoples’ histories and ways of knowing and being over the past 3 years. Two researchers (DPM and SM) analyzed the data. SM is a physiotherapist researcher from South Africa with qualitative research expertise. Despite their efforts to approach the research with humility and openness to Indigenous ways of knowing, their unconscious bias towards Western research and their origin from different countries and cultures might have influenced data interpretation. Yet researcher subjectivity, as long as it is disclosed reflexively, is something that can enhance the depth and richness of the analysis rather than be a source of bias that needs to be controlled29. The other authors (TH, KC, KH, and PC) are all Canadians, but no researchers identified themselves as First Nations people.
Design
This qualitative study applies a narrative design to gain an in-depth understanding of First Nations Peoples’ perceptions of telehealth physiotherapy30. An experiential orientation was used, as it retains a focus on the participant’s views. The ontology adopted is critical realism, and the epistemology is contextualism, providing access to participants’ perceptions of (their) realities, which are partial, and shaped by and embedded within their cultural and historical contexts31,32.
Data collection
Semistructured interviews were utilized to elicit robust data on participants’ perceptions of telehealth physiotherapy. The interview guide (Appendix I) was produced in consultation with CSFS to ensure that open-ended questions focused on participants’ perceptions of telehealth physiotherapy and the therapeutic relationship when using telehealth. Participants who did not have experience with telehealth and/or physiotherapy were asked to articulate what they would expect of telehealth physiotherapy should it be available in their community. This allowed a rich narrative between the first author and the participants, regardless of whether they had lived experiences or not. Interviews were conducted in English (which was the first language spoken by all participants) in person or using Zoom, each lasting about 45 minutes. All interviews were recorded using a digital voice recorder. The concept of data sufficiency was used to determine the sample size when the in-depth semistructured interviews with participants yielded enough information to achieve a thorough and nuanced understanding of the research question.
Data analysis
The interviews were transcribed verbatim, and the transcripts were coded and thematically analyzed using the Braun and Clark method29, supported by NVivo v12 software (Lumivero; https://lumivero.com/products/nvivo) (Appendix II). After independently reading and re-reading the transcripts for familiarization, the researchers identified codes and emergent themes through a predominantly inductive approach to data analysis, where the focus was to unpack people’s perspectives on the topic, using both semantic and latent techniques to explore meaning. Subject IDs were used to ensure the confidentiality of participants. Pseudonyms with descriptors are used when participants are quoted.
Rigour
To ensure credibility, researchers identified codes and emerging themes using dialogue, challenging each other’s preconceptions and interpretations of meaning33. The first author documented her thoughts and also the participant’s non-verbal communication (eg facial expressions) during the interviews and analytic process to assess reflexivity and to strengthen her ability to practice cultural humility33. Transcripts were member-checked by the corresponding participants following their interview to increase dependability33. The researchers recorded all decisions made during the analytical process to provide a clear audit trail to trace every decision easily33. Descriptions of participants’ characteristics are presented along with illustrative quotes to facilitate the transferability of our results33.
Ethics approval
This study was approved by the University of British Columbia (UBC H222-02383) and CSFS Research Ethics Boards. All procedures followed CSFS research guidelines, were overseen by CSFS, and were oriented towards the goals of the organization34. One research member (TH) is the CSFS Chief Administrative Officer and was involved in the research design. In addition, we worked collaboratively with community representatives to identify and recruit potentially eligible participants, as well as to arrange and conduct the interviews in the communities. The First Nations principles of ownership, control, access, and possession (OCAP) also guided this work35. All researchers involved in the study procedures underwent cultural safety training. Informed consent for participation in the study was obtained, and permission for audio-recording was granted by each individual.
Results
A total of 19 individuals participated in the interviews. Participants’ demographic details are outlined in Table 1. We recruited individuals from eight different communities. Seventeen (89%) of participants had prior experience with physiotherapy, but only five (26%) with telehealth physiotherapy. Of the two participants who didn’t have experience with physiotherapy, one knew what physiotherapy was, and the other did not. Another two participants had experience with physiotherapy, but when asked about it they did not know that the service they received was called physiotherapy.
Most participants (74%) knew physiotherapy services were available in their communities. Nearly all were interested in this service after an explanation of what it was and agreed that there were people from their communities who would benefit from it. Over one-third of the participants expressed that they would like to see the service offered more often (when the current frequency reported was once a week). Importantly, there were comments regarding a lack of awareness about physiotherapy scope of practice and service availability:
I think that a whole lot of people could benefit from physiotherapy services, but they need to know that it’s there. I think we should have all of our elders going to promote their mobility and learn from basic exercises they can do. Like, you’re not going to ask questions about what you don’t know, so I think that there’s kind of a gap like people need to know how it can benefit them. (Mary, 51 years)
In addition, there were comments about how the lack of practitioner availability may impact First Nations Peoples’ health:
We don’t have enough healthcare staff … and a lot of it is pain management. If they had access to a physiotherapist to deal with whatever injury they were dealing with, it would make all the difference. But instead, they turn to getting opioids off the street so that they don’t have to be in pain anymore [with emotion]. (Amy, 45 years)
Participants’ attitudes towards telehealth were positive, with comments about increased accessibility and convenience of healthcare services:
You don’t have to get in your vehicle and leave too far of a distance; you’re just right here at the health center instead of driving in the wintertime all the way across town, and that’s just like, you never know what’s going to happen on the road. Without telehealth, where would we be without that? It’s convenient in a lot of ways for a lot of us. (Chloe, 48 years)
Sixteen participants (84%) had experience with telehealth. Seven participants (37%) strongly preferred in-person visits because they perceived telehealth as less personable and efficient: ‘I’m old school, I like to talk to the person in person’ (Ian, 65 years). Three participants (16%) did not have experience with telehealth, and another two (11%) were unfamiliar with this term or virtual care. When asked specifically about telehealth physiotherapy, five individuals (two who experienced telehealth physiotherapy, one who experienced telehealth and physiotherapy separately but not together, and two who did not experience telehealth or physiotherapy) expressed negative opinions: ‘I don’t think that you can have telehealth for physio’ (Amy, 45 years). Even so, most patients had positive perceptions and expressed interest in utilizing telehealth. Access to videoconference was regarded as important:
Definitely video over telephone. Faces are important, like in-person reading the whole body is the best case scenario, but at least with the video, you know you’re being heard, and you know that that person is paying attention. (Rose, 40 years)
Some situations considered suitable for telehealth physiotherapy from participants’ narratives were follow-ups, education, exercises (some people said that they would be particularly interested in group sessions), and mobile applications with reminders about treatment.
Three main themes emerged from reflexive thematic analysis (Fig1): (1) therapist’s attitude and rapport, (2) remote nature of virtual care, and (3) fostering culturally appropriate telehealth physiotherapy. Table 2 shows the themes, subthemes, processes, and examples of participants’ quotes.
Table 1: Demographic information of participants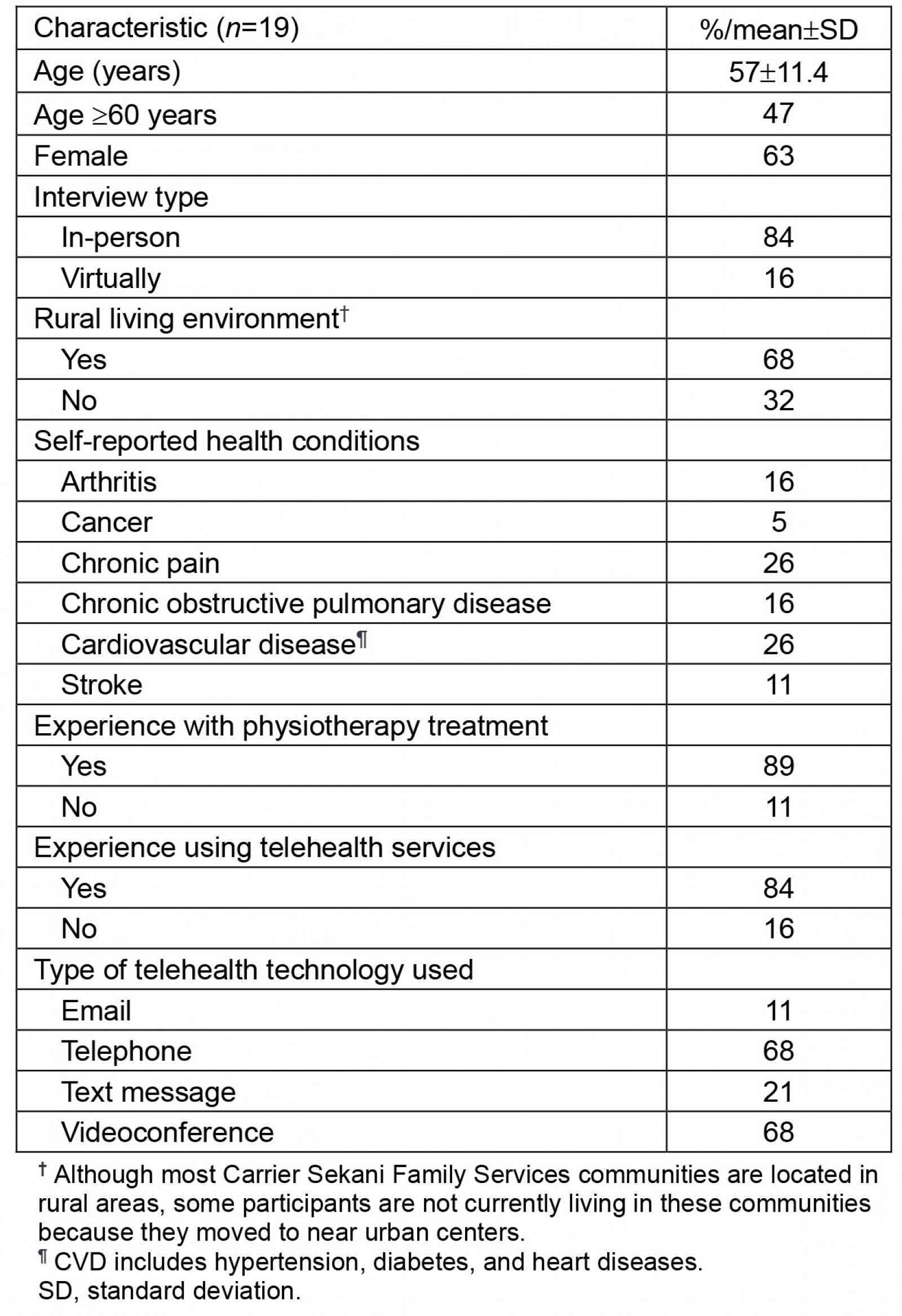
Table 2: Therapist’s attitude and rapport, remote nature of telehealth appointments, and fostering culturally appropriate telehealth physiotherapy: theme development and examples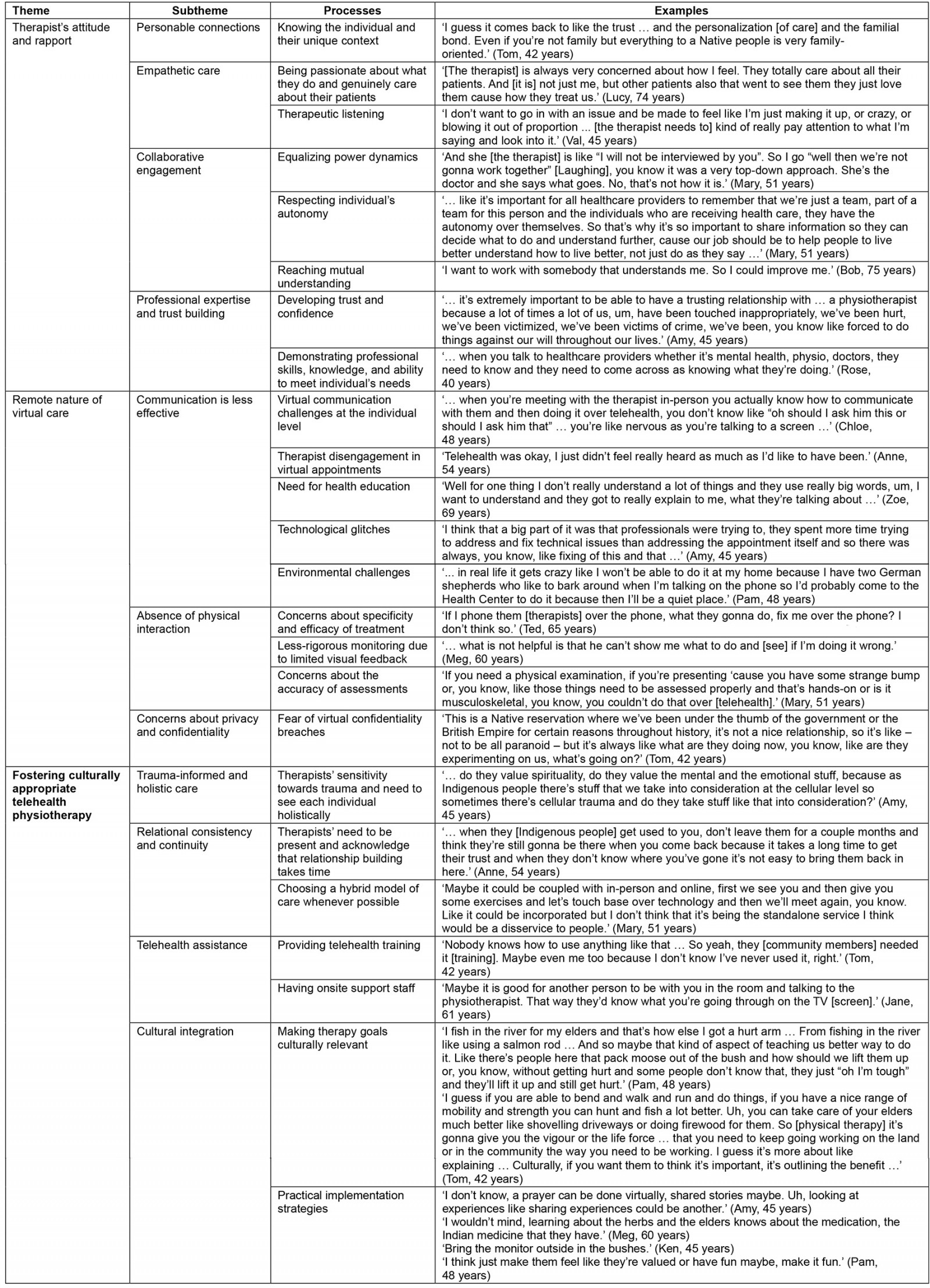
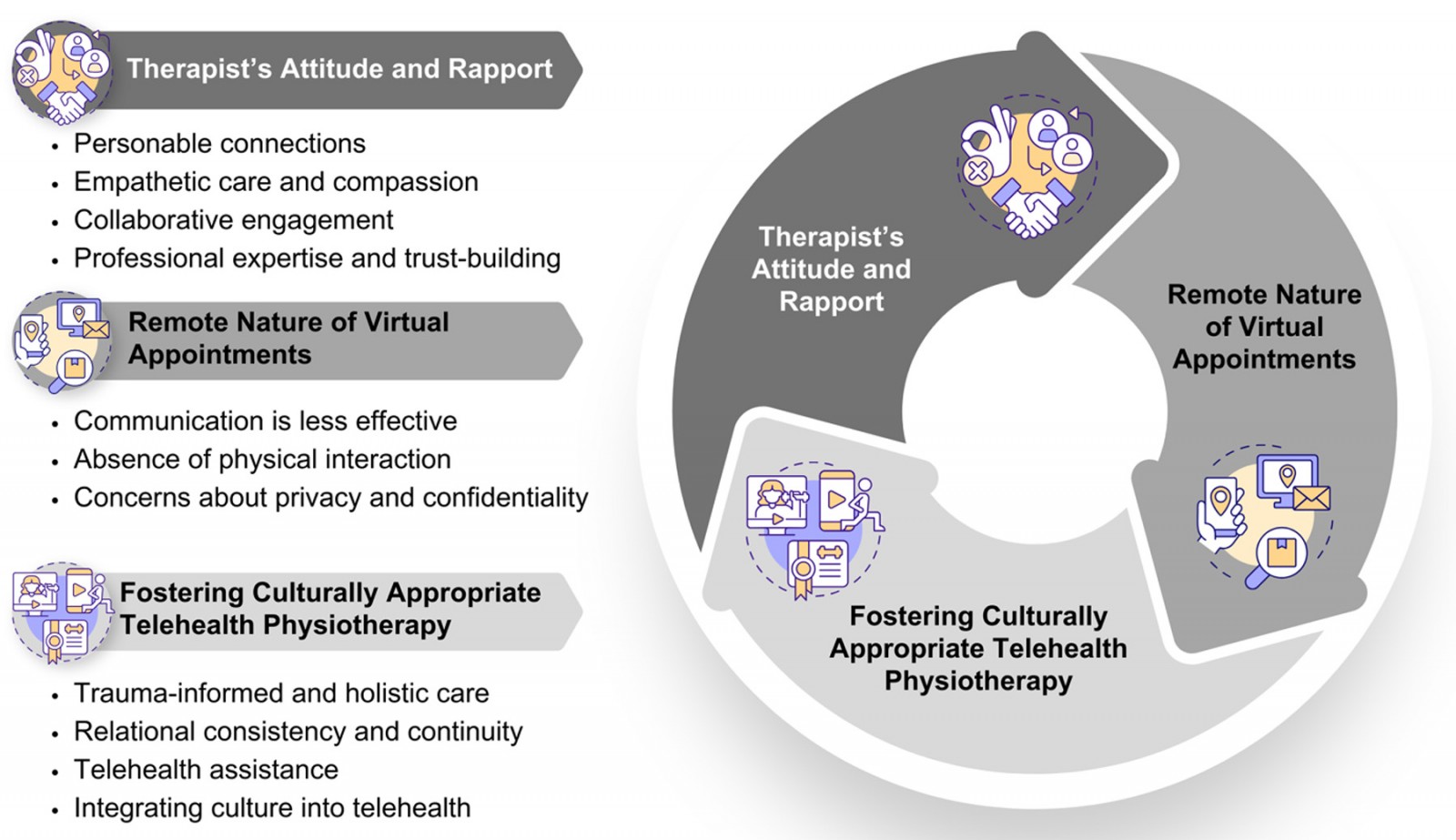 Figure 1: Graphic representation of themes and subthemes.
Figure 1: Graphic representation of themes and subthemes.
Theme 1: Therapist’s attitude and rapport
This theme captured participants’ perceptions of what matters the most in how healthcare providers, specifically physiotherapists (for those who had experience with physiotherapy, n=17), related to participants and carried out their work. The following data developed as subthemes.
Personal connections: Therapists’ efforts to get to know the individual’s unique context and connect with them on a human level appeared to be an important element of the therapeutic relationship for several participants. Participants often expressed similar views:
It’s not just about helping us, it’s about getting to know us too, I guess … Know about my Nation, what am I about, what are my people about, what do we need and how could you help … (Pam, 48 years)
While most clients valued this closer familiarity, there were a few others who held a more detached perspective:
I want them [the therapists] to be more professional and not talk about [personal interests] … I want him to tell me, you know, I could do this for you, and we’ll take it step by step for you to get better. (Bob, 75 years)
Empathetic care: Participants appreciated therapists who are passionate about what they do, as exemplified in this comment:
I just wish we had more people with big hearts … [laughing] That love to work with the patients around here. (Ted, 65 years)
These professionals were perceived as having a better ability to transmit empathy and a genuine interest in the individuals and their outcomes, which was considered fundamental to building trust and rapport. Mary (51 years) talked about an unmet expectation for an empathetic understanding of her biopsychosocial needs and the importance of feeling valued by the therapist:
I said something, and she [the therapist] didn’t even pick up on it. She didn’t basically care, and I just thought ‘You’re not getting holistic health’. So, the next time I asked her, I just want to know that if you’re providing service to me, that I’m important to you.
Another important component of empathetic care is therapeutic listening, and many participants expressed the importance of feeling heard and validated without judgment:
They [the therapist] would be sitting there, typing on the computer, looking through things, and I’d be telling them what was wrong with me and ‘Oh, what did you say?’ That’s really upsetting when somebody doesn’t listen to you. (Meg, 60 years)
Collaborative engagement: A collaborative engagement appeared to develop from a mutual understanding of both the therapist’s and the client’s values and beliefs:
To build a good relationship both the patient and the physio have to come in with an open mind to build, to be able to meet philosophies, because you’re not always gonna agree with somebody’s philosophy but if you have an open mind on either end you could still find a place to work together … (Rose, 40 years)
It also developed from respect for individual autonomy in their health-related decision-making:
I believe from the Indigenous point of view that all people have a right to their own mind, bodies, and spirits, and they are the arbiter of all of those decisions, and we don’t have a right to tell other people what they should and shouldn’t be doing. We don’t have a right to be exerting ourselves in other people’s spaces. (Amy, 45 years)
Moreover, participants expressed the desire to be considered equals in the therapeutic process. They wanted to feel that their expert knowledge and contributions are valued, as this was seen to foster dignity and empowerment.
Professional expertise and trust-building: Therapists need to demonstrate professional skills, knowledge, and ability to meet individual needs in telehealth, as these reflect on the individual’s capacity to trust the therapist and be confident in the proposed treatment. One participant said:
You have to be confident in your health provider’s knowledge base, so I think that’s important to be shared and get to question or ask things. (Mary, 51 years)
Theme 2: Remote nature of virtual care
This theme encompassed the main challenges of virtual care visits, particularly how these were perceived to impact establishing and maintaining solid therapeutic relationships.
Less efficient communication: Many participants shared difficulties in effectively communicating during virtual visits, for varied reasons like getting nervous, ‘With the telehealth you kind of get nervous and you forget things to say’ (Anne, 54 years), or just feeling that it is easier talking in person as opposed to a screen or over the phone:
You’re used to communicating with a human being and then [in telehealth] you’re talking to a machine, I don’t know … [chuckles] (Joe, 72 years)
Some participants had the impression that the therapist was less invested in virtual appointments compared to in person:
There were times when I met a physiotherapist and you could tell that their head was elsewhere and you could see that they weren’t really invested in or kind of wanting to work with you. (Amy, 45 years)
Health literacy was a challenge that seemed to be exacerbated in virtual care visits, and there were comments about the need for therapists to avoid using medical jargon and to help clients understand their health condition and treatment:
If you’re gonna help me, you would need to talk to my level and all, just tell me the message, tell me how to write, you know, don’t use the medical terms I’m not gonna understand. (Bob, 75 years)
Technological glitches were also mentioned as something that disrupted communication and could become the focus of the visit if persistent. Finally, environmental challenges were described as barriers to effective communication and good-quality telehealth visits. For example, one participant said:
There’s people running here and there at my house, and then sometimes not being able to focus on doing the exercises on hand because your kids are fighting or they’re screaming, and you’re not getting that time to just focus. (Amy, 45 years)
Absence of physical interaction: While a few participants said that the lack of physical touch would not affect their ability to connect with the physiotherapist, others expressed the opposite opinion:
Touch is a very important part of human communication and trust-building. So, I think that that does impede the dynamics of it. (Mary, 51 years)
Some participants were particularly concerned about the lack of specificity of treatment:
I feel more frustrated [using telehealth]. I don’t have as much confidence in doing it by myself because I know you have to move your body in very specific ways. Then if you don’t, it causes you damage … so they [physiotherapists] need to physically move me and show me how to do it. (Amy, 45 years)
They perceived the absence of or limited visual feedback to impede rigorous monitoring of exercises. Concerns about the accuracy of assessments were also expressed:
In physio[therapy] they’re like ‘Oh, I’m gonna put my finger behind your knee and now squeeze it or whatever’, and like testing your ligaments or whatever, they [physiotherapists] got to dig in so much and like ‘Does this hurt?’ or ‘Let me work your’ … so yeah, I think the hands-on stuff would be lacking. (Tom, 42 years)
Concerns about privacy and confidentiality: Some participants considered the telehealth environment less private. A situation that corroborates this is the presence of other people in the background of the professionals:
With professionals and specialists that are working from home, lots of times there were people in the background, they have their husbands, or wives, or children or whoever … they’re walking in the background, they’re peeking in sometimes … and I don’t think that that’s right at all. (Amy, 45 years)
On their end, First Nations Peoples may be worried about how much of their private space the camera will show on videoconferences:
Some of the community members, they don’t understand the telehealth here, and they think it’s non-confidential … because it’s over the screen and the screen shows everything … (Chloe, 48 years)
Paradoxically, there was also a comment favouring the privacy of home-based telehealth visits as opposed to having to go to the health center:
Just like if it was in your own home then other people are not hearing what’s going on here, or nobody sees you or you know. So it’d be really good with telehealth physio. Where nobody could harass or knock on the door. (Pam, 48 years)
Another point was the lack of confidence in data security management:
You just don’t know who’s hack[ing] it, like you know, if I was a computer whiz, I can hack your profile and … use the information against you or whatever … I just don’t trust it. (Ian, 65 years)
Theme 3: Fostering culturally appropriate and safe telehealth physiotherapy
This theme focuses on what is needed to advance telehealth physiotherapy in a manner that respects and reflects First Nations cultures, equipping all involved parties to provide comprehensive and sensitive services. Appendix III is a vignette on the implementation of a hybrid model for telehealth physiotherapy in First Nations communities based on the respondents’ suggestions and the researcher’s perspectives.
Trauma-informed and holistic care: Building trusting relationships with healthcare providers may be challenging to many First Nations People due to the profound impacts of colonization, racism, and social marginalization on their health outcomes and healthcare experiences. This was perceived to be potentially more challenging over telehealth visits:
… so many [First Nations] Peoples have faced so much negative in the system that it’s really hard, like there’s so many biases that people don’t even realize they have them, so like… Indigenous people are already hesitant when it comes to health care that it would make a telehealth appointment a little more tricky. (Rose, 40 years)
In light of this, therapists’ sensitivity towards trauma and a holistic approach to health that aligns with First Nations views and considers not only the physical but the emotional, mental, and spiritual aspects of an individual’s wellbeing were things that the participants wanted to have:
We should be having trauma-informed health services in every aspect of health … I think that we have to remember that we’re holistic beings so we need to come at it through a holistic view. (Mary, 51 years)
Relational consistency and continuity: Participants acknowledged that building relationships takes time and highlighted that it is particularly difficult when rotating healthcare providers do not visit the communities regularly:
Just about every time you go see a doctor it’s a different one, and you can’t establish a good relationship that way. (Ted, 65 years)
Many shared that seeing the physiotherapist in person from time to time, instead of making all visits via telehealth, would facilitate relationship building. Having an established relationship through in-person visits can help the transition to telehealth visits:
Because of the existing relationship with the physio from attending the office, because it was a good existing relationship, it was nice to be able to chat [via telehealth] and like ‘cause that relationship was already built. (Rose, 40 years)
Telehealth assistance: Most participants felt comfortable using technology, but there were a few who expressed the need to receive training to be able to engage with telehealth comfortably:
Take me out of the old school thinking, you know, maybe [with] a little bit of training … Not just throw it [telehealth] in your face and here! … train me so I could gain trust with using telehealth. (Bob, 75 years)
Furthermore, having local telehealth outreach workers serving as a liaison between the professional and the local community can be a valuable way to establish trust and support with setting up the telehealth equipment:
Having that support [onsite] would also be a good place to build a relationship to pass on to the provider on the other end. (Rose, 40 years)
Cultural integration: Participants who had previous experience with telehealth generally felt safe during their virtual visits. There was one participant who saw telehealth as a potential threat to cultural safety:
It just takes away, so like, culturally I don’t think that there’s a match. For me, culture is community, and culture is human interaction. Culture is coming together. Culture is doing things on a personal one-to-one or, you know, communal level. (Amy, 45 years)
Some participants indicated that there are aspects of their culture that they prefer to keep private, ‘A few things like in my culture I like to keep private’ (Ian, 65 years), while others simply said that they do not think that culture needs to be part of telehealth physiotherapy: ‘I don’t think culture needs to be involved at all’ (John, 63 years). Yet, the majority of participants were in favour of cultural integration and shared suggestions regarding how to do it:
I’m all for cultural integration into anything in our lifestyles. Our people, we kept fit in certain ways, and if we could integrate that into the therapy, that would be an awesome idea, really. (Emma, 45 years)
By tailoring physiotherapy interventions to align with Indigenous cultural activities, such as traditional dance, individuals are more likely to engage and commit to their rehabilitation process:
I think culture can be combined with physio in the way of like dance and stuff like that, like traditional dance and movements medicine. I think that is so important for movement. (Mary, 51 years)
Making therapy goals culturally relevant was suggested, outlining the benefits of physiotherapy in improving their health and allowing them to fully participate in their cultural activities, like fishing or taking care of the Elders. Other strategies that could be adapted to the virtual scenario, voiced by the participants, included prayers, sharing stories, creating space for traditional medicine, making appointments outdoors in nature, and using humour judiciously or making therapy fun (see Table 2 for quotes supporting these findings).
Discussion
Our findings suggest that there is a need to increase awareness of and access to physiotherapy services for First Nations Peoples, especially those living in rural and remote communities, and that people would be interested and open to using telehealth to bridge the access gap. However, participants underscored the need to address some of telehealth’s perceived limitations to ensure quality of care, which includes being able to build and maintain trusting therapeutic relationships. Not all participants were receptive towards engaging with telehealth physiotherapy services, reinforcing evidence about the need to take patients’ personal preferences into account when choosing the health service delivery medium in line with patient-centred care36.
Before exploring the differences between building relationships in person and by telehealth, theme 1 captured what matters most in the therapeutic relationship from the perspective of First Nations Peoples. Therapists wanting to know the people and their unique context was emphasized to develop personal connections, an important aspect of the therapeutic relationship for most participants. In a cross-cultural setting where power imbalances linked to colonization and healthcare relationships play a role, a visitor (eg non-Indigenous professional) should personally take on the responsibility of learning about the culture, primarily through attentive and respectful observation and gradual participation37. Cultural safety training and face-to-face interactions play a critical role in this learning process. The literature emphasizes that in-person visits allow healthcare providers to engage in direct observation and participate in the community’s daily life, fostering a deeper understanding of the cultural and social context of their patients21,22,38. These interactions help build trust, which is foundational in therapeutic relationships, especially in communities with historical experiences of marginalization and mistrust of the healthcare system39.
Addressing the disempowerment potentially experienced by First Nations Peoples in their interactions with healthcare providers can help foster a collaborative engagement and welcoming therapeutic relationships, which most participants desired40. Although physiotherapists need to demonstrate their professional expertise to enable patients’ trust and confidence, the way in which knowledge is shared with First Nations Peoples can ‘make or break the relationship’41. Throughout history, colonizers have consistently dictated to Indigenous Peoples what they need42. To enable trusting therapeutic relationships, it is critical to move away from the idea of ‘expert physiotherapists’ who will tell them what to do or attempt to ‘fix’ them to allies who value their own expert knowledge and culture, respect their autonomy, and genuinely care about them and their outcomes43,44. A practical way to demonstrate empathetic care, which aligns with the fundamental principle of cultural humility, is to speak less and listen more, creating opportunities for new knowledge45,46. Effective listening is crucial in telehealth interactions to ensure patients feel understood and valued. When patients feel listened to during telehealth consultations, they are more likely to be satisfied with the service, which can result in better engagement and adherence to treatment plans47,48.
Communication was viewed as one of the main challenges of virtual care visits, negatively impacting therapeutic relationship building. Evidence suggests that patients ask for information to be reiterated more frequently in telehealth visits49; however, individuals with low health literacy are less likely to indicate if they do not understand something50,51. There is a general agreement that telehealth practitioners need advanced communication skills to offset the lack of visual cues52. On top of that, contextual shapers like technological glitches due to poor connectivity and environmental challenges (eg overcrowded houses) have been identified in our study and in previous studies53. Physiotherapists should take these factors into consideration when choosing between telehealth or in-person visits. If telehealth is deemed appropriate, strategies to mitigate miscommunication should be adopted, like ensuring a quiet space with a reliable internet connection, avoiding the use of medical jargon, and establishing a contingency plan in case of technology failure54. Conducting virtual visits in a quiet and private space can also contribute to minimizing concerns about privacy and confidentiality. In addition, both parties are encouraged to use headphones and artificial backgrounds, keep their microphones muted when not speaking, and use the chat function whenever appropriate53,55.
While the absence of physical interactions was seen as a limitation of telehealth, its main implication was not directly related to the therapeutic relationship but the limited scope of physical examination and treatment. Most participants said that the lack of therapeutic touch did not or would not affect their ability to develop rapport with the physiotherapist, but they thought that physiotherapists could not effectively assess, treat, or supervise their exercises via telehealth. Digital physiotherapy assessments through synchronous telehealth demonstrate validity and reliability56,57, but there are other studies showing that patients deemed face-to-face assessment as more effective58. Concerns with the quality of feedback provided and insecurity about their own exercise abilities in the absence of direct in-person supervision have been reported before59. Considering that, as raised by some participants, many First Nations people may not know what physiotherapy is and how it can help due to limited access to this service, our findings suggest that it would be beneficial to have at least the initial physiotherapy visit in person. This can help establish the therapeutic relationship, facilitate physical assessment and exercise prescription, and improve patients’ self-efficacy60. In fact, combining in-person with telehealth visits (ie a hybrid model) can offer a more complete and personalized rehabilitation experience61,62, ensuring relational consistency and continuity.
The need for telehealth training in equipment operations was a key finding that has been highlighted before63. Moreover, physiotherapists are encouraged to work in collaboration with local support staff who can assist patients with equipment set-up for their virtual visits and also play a role as cultural liaisons, mediating trust building with the therapist64. This strategy can be particularly effective for Indigenous communities, given their strong communal bonds and propensity to engage openly and collaboratively with all community members41.
The need for culturally safe approaches to First Nations health is overwhelmingly supported by experts in the field, and this includes the adoption of trauma-informed and holistic care65,66. Most participants were supportive of cultural integration into telehealth physiotherapy visits, and the main suggestion was aligning therapy with cultural practices like traditional dance and ceremonial activities and making therapy goals culturally relevant (eg improving their strength and range of motion so that they can go hunting or berry picking more effectively and without pain). This could even be done outdoors in nature using portable technology, as suggested by one participant. Land-based activities have been shown to improve the health and wellbeing of Indigenous adults67, and physiotherapists working with First Nations communities recommended expanding activities and treatment to the land and culture as part of an innovative way to deliver rehabilitation services that are culturally relevant and effective64. To effectively implement these approaches, first and foremost, telehealth and cultural integration need to be an individual’s choice and not something imposed. If an individual is interested, it is crucial for physiotherapists to understand the environment in which the patient lives and tailor their care accordingly. As previously stated, this might involve in-person community visits and cultural safety training. However, it is important to acknowledge that relying solely on cultural safety training can be problematic, as such trainings often focus on cultural aspects alone and can overlook broader frameworks like social determinants of health and social justice68,69. This can inadvertently lead to stereotyped notions of culture and ‘othering’ practices68,69. Therefore, to learn about the specific histories, cultures, and knowledge systems of the people served, physiotherapists are also encouraged to engage with continuing education in partnership with knowledge keepers, Elders, and other Indigenous leaders70.
This study has some limitations. First, while compensation can aid in recruitment and is an ethical way to acknowledge participants’ time and knowledge shared, it may have influenced their responses during interviews. Second, although generalizability is typically not a primary goal of qualitative research, the specific focus of this study – telehealth physiotherapy and its impact on therapeutic relationships within First Nations communities in North Central BC, Canada – means that findings should be cautiously interpreted outside this particular context. However, by providing a transparent report of the methods and detailed descriptions of the phenomena under investigation, we enable readers to make informed decisions about the transferability of these findings to other contexts. Finally, the researchers acknowledge that their own positionality and perspectives may have influenced how the research was conducted and interpreted, which is an inherent aspect of qualitative research. Future research should explore the implementation and evaluation of hybrid models that combine in-person and telehealth visits to enhance the accessibility and effectiveness of physiotherapy services for First Nations and other Indigenous communities.
Conclusion
Our study provides in-depth insights into First Nations Peoples’ perceptions of telehealth physiotherapy to inform remote physiotherapy service delivery. While there is a need to expand access to physiotherapy services, the implementation of telehealth must navigate the nuanced landscape of building and maintaining trusting therapeutic relationships. The importance of cultural safety cannot be overstated, with a call to move beyond the traditional roles of professionals as experts to allies who respect First Nations Peoples’ autonomy and value their knowledge, experiences, and culture. Communication barriers and the absence of physical interaction pose significant challenges, although the latter was not directly related to the therapeutic relationship but the limited scope of physical examination and treatment. Our findings advocate for a hybrid model, combining in-person and telehealth visits to ensure comprehensive rehabilitation experiences and support the maintenance of the therapeutic relationship. Addressing the digital health literacy gap with telehealth training, coupled with collaboration with local support staff, emerges as a crucial aspect of successful telehealth physiotherapy implementation. Moreover, the incorporation of culture, aligning therapy with traditional practices and land-based activities, reflects a promising avenue for enhancing the effectiveness and relevance of telehealth services for First Nations Peoples.
Acknowledgements
The authors thank all participants recruited into the study. The authors acknowledge the time and effort contributed to developing the interview guide and providing feedback to the study by CSFS members.
Funding
This study was funded by the Canadian Institute of Health Research (grant number F18-04341). DPM was funded by the Four-Year Fellowship (UBC) and Canadian Respiratory Research Network (CRRN) Studentship.
Conflicts of interest
The authors declare no conflicts of interest.
References
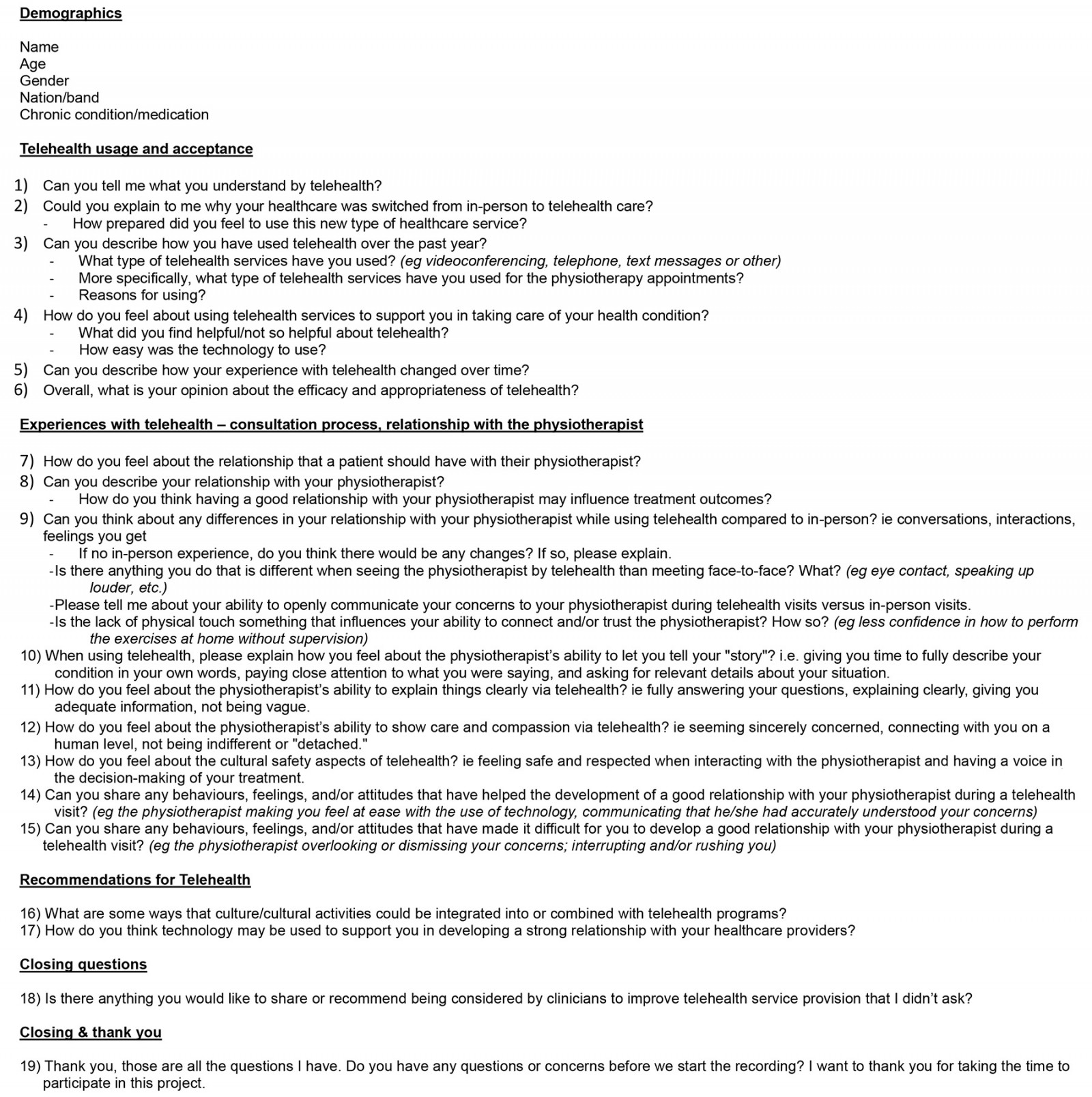
appendix I:
Appendix II: Qualitative data analysis details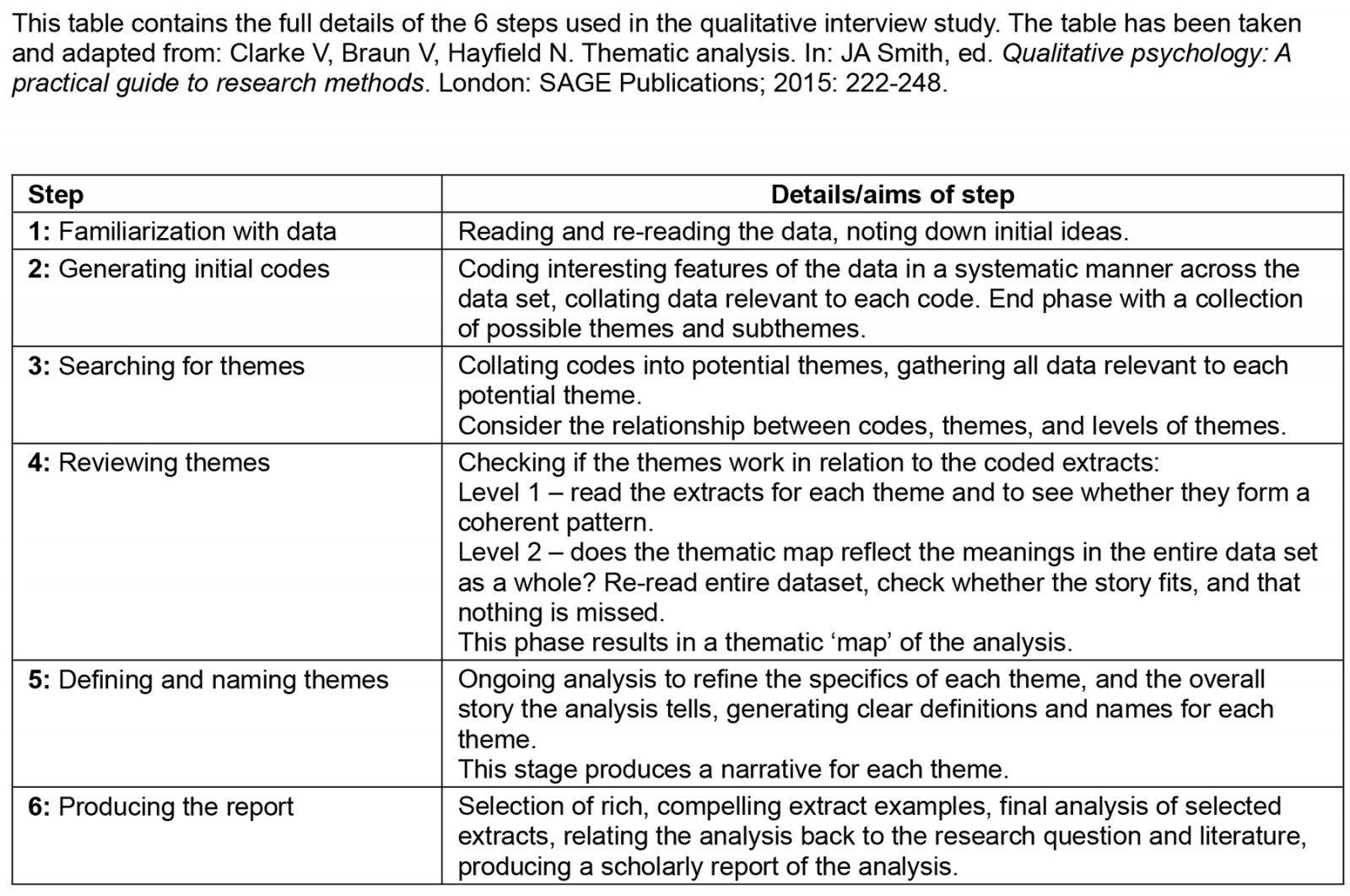
Appendix III: Implementing a hybrid model for telehealth physiotherapy in First Nations communities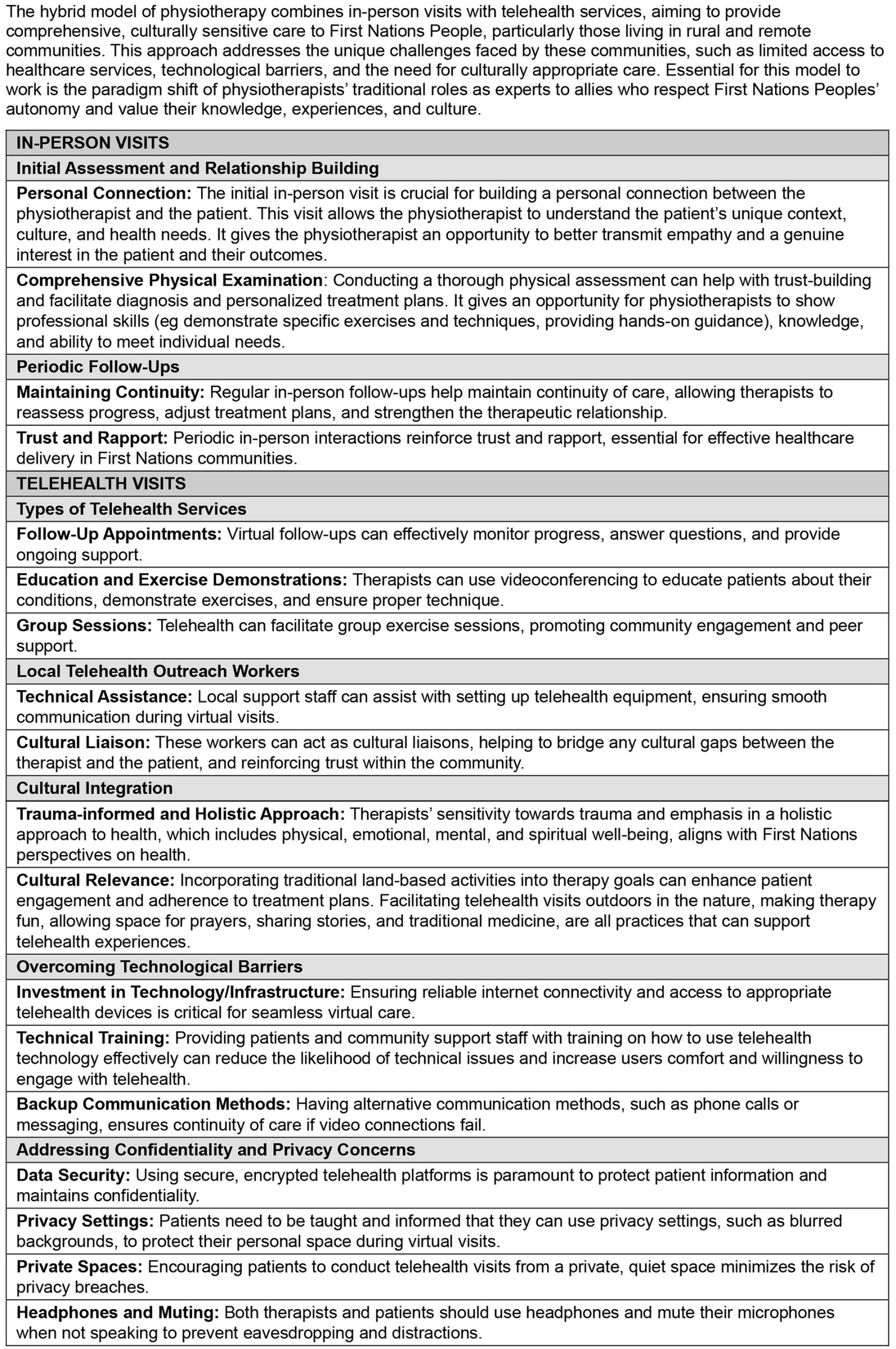
You might also be interested in:
2013 - Birthing in the Barkly: births to Barkly women in 2010