Context
The International Centre for Eyecare Education (ICEE)/the Aboriginal Health and Medical Research Council (AHMRC) New South Wales (NSW) Aboriginal Eye and Visioncare Program is a collaborative program aimed at improving eye and visioncare for Aboriginal communities in NSW that has established over 60 eye clinics throughout the State, and is successfully delivering local and ongoing eyecare to Aboriginal communities.
History
Vision 2020: The Right to Sight is a global initiative designed to eliminate avoidable blindness by the year 2020. The initiative was established by an alliance of the WHO, the International Agency for the Prevention of Blindness, and the Partnership Committee of the International Non-Government Development Organisations. Vision 2020 Australia aimed to organise the implementation of the Vision 2020 goals in Australia. Over 50 Australian organisations involved in vision and eyecare research, education and community came together to work in three areas: Australian community, Aboriginal and Torres Strait Islander communities, and global eyecare.
In November 1999 at an early meeting of Vision 2020 Australia, it was said that a high percentage of people in Australia with eye problems were Aboriginal Australians. It was also identified that uncorrected refractive error, which can be corrected with spectacles, was a leading cause of visual impairment in Aboriginal communities, followed by cataract, diabetic retinopathy and trachoma1.
It has been estimated that 50% of blindness and 70% of vision impairment in Australia is caused by conditions that are said to be preventable or treatable2-4. Aboriginal people suffer up to 10 times the level of blindness from preventable eye disease than non-Aboriginal people5, and they attend eyecare practitioners in proportionally far lower numbers than other members of the Australian population6. Some of the barriers to achieving progress have been a lack of availability of local and culturally appropriate services, lack of eye health awareness, lack of follow up, and economic factors5-7.
Issue
The ICEE undertook to do something about correcting this problem for the Aboriginal population in NSW. While there had been a series of efforts to improve Aboriginal eye health and vision care, both through interventions directed at specific conditions and attempts to recruit regional professionals for primary and secondary care, an effective, coordinated and sustained program that delivers quality eyecare to Aboriginal communities had not yet been achieved.
The Office of Aboriginal and Torres Strait Islander Health (OATSIH), a division of the Commonwealth Department of Health and Aged Care, and the National Aboriginal Community Controlled Health Organisations (NACCHO) agreed that one of the major barriers to Aboriginal people seeking eye examinations was the lack of optometric and ophthalmologic services within Aboriginal Community Controlled Health Services (ACCHS). It has been demonstrated that Aboriginal people are reluctant to visit mainstream hospitals, community health centres, optometrists or ophthalmologists6. As a consequence Aboriginal communities had much higher rates of vision impairment and blindness than the non-Aboriginal Australian population.
To tackle this problem, the Commonwealth Government agreed to finance equipment for 7 eye clinics to be established within rural NSW Aboriginal Community-Controlled Medical Service facilities at Wagga Wagga; Walgett; Wellington; Kempsey; Narooma (subsequently located at Bega); Bourke and Broken Hill.
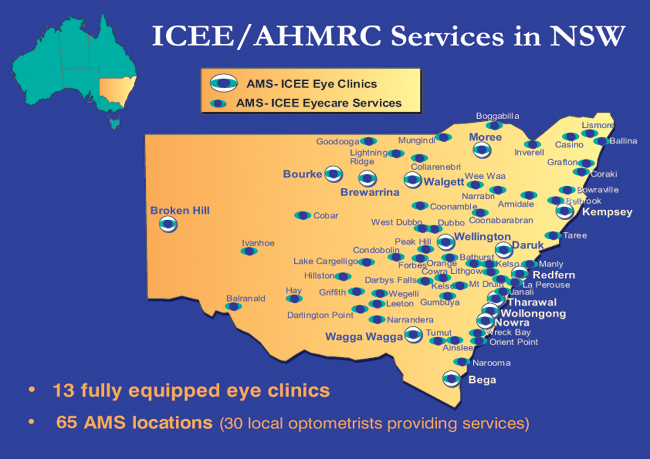
Figure 1: Map of Australia showing the locations of the eye clinics established within rural NSW Aboriginal Community-Controlled Medical Service facilities.
The ACCHS or Aboriginal Medical Services (AMS) have had major success in providing access to healthcare for Aboriginal people throughout Australia. They were established in the early 1970s to provide 'a primary health care service initiated by local Aboriginal communities to deliver holistic and culturally appropriate care to people within their communities' 8. The Commonwealth Government also agreed to provide ongoing funding for the employment of an Eye Health Coordinator (EHC) at each of these locations.
However OATSIH (NSW) encountered two major problems in attempting to implement these programs:
- Their approaches to ophthalmologists requesting the provision of staff to attend and provide regular and ongoing services in these locations were unsuccessful.
- The cost of equipment, as estimated by ophthalmologists, was excessive. A list of equipment and costing was sought from ophthalmologists, and one list was in excess of A$220 000.
The ICEE program
ICEE proposed that the clinics be established with optometric services to provide initial care and referrals to ophthalmological services where appropriate. It was proposed that the NSW Eye Clinics would provide primary eyecare and vision correction within Aboriginal community controlled health services, with local optometric participation, and triaging to regional hospitals.
In trying to set up any program in NSW, ICEE was told that the support of the peak Aboriginal Health body in NSW, the Aboriginal Health and Medical Research Council (AHMRC), was essential. OATSIH (NSW) therefore arranged for ICEE to meet with AHMRC. The outcomes of that meeting were:
- OATSIH (NSW) funded equipment for the establishment of an initial eye clinic at the AMS Redfern.
- ICEE and AHMRC signed a Memorandum of Understanding (MOU) resulting in ICEE providing optometric services for the 7 locations and such other locations as requested and agreed.
- All consultations were to be 'bulk billed' (ie charged at the Medicare rebate rate) and all patients offered optical appliances through the NSW Government spectacle program.
- The AHMRC Board worked with its member AMS Boards and ICEE in promoting the program, providing space, staff, transport and other assistance.
- Wherever possible ICEE utilized the services of a relatively local optometrist in providing eyecare services.
ICEE also approached the Royal Flying Doctor Service (RFDS) CEO at Broken Hill, NSW, and arranged for flights to be available for ICEE Optometrists and other staff to fly to selected AMS. The first ICEE team flight was made to Walgett in December 1999.
The Program established clinics at a range of locations throughout NSW to ensure that eyecare services are available to all areas, including metropolitan, rural and remote locations. ICEE now has a presence at 66 locations (educational and administrative flights are made to other locations as needed). These include:
- Fully equipped clinics at which EHC are stationed, in major metropolitan and rural areas. The cost of equipment purchased for each of these eye clinics was between $20 000 and $25 000.
- Rural and remote clinics equipped by ICEE and staffed by local optometrists.
- Regional clinics in rural and remote areas that are regularly visited by ICEE optometrists.
Program strategies
There are three levels of service within the program:
- Aboriginal Eye Health Coordinators, who have also been trained by ICEE, have a screening kit which enables testing of 7 aspects of eye and visioncare. No judgement is necessary; each test is a simple pass or fail. All EHCs have a manual and all but the present EHC at Broken Hill have attended an educational program at ICEE to receive theoretical and practical instruction in the use of the kit. EHCs are encouraged to visit schools, preschools, isolated and remote communities to screen and to educate others in screening techniques. All failures are referred to the optometrist at the nearest AMS.
- The optometrist examines those referred from screenings, self referrals, referrals from AMS and other GPs, schools, gaols and Land Councils. Those requiring referral to the GP or other healthcare practitioner are referred/directed with the aid of the EHC.
- Arrangements are made for those requiring ophthalmic surgery or other treatment to be seen by an ophthalmologist at a regional hospital. In NSW the Royal Australia and New Zealand College of Ophthalmologists cooperates fully in providing ophthalmological services to pre-screened patients referred by the AMS-based optometrists.
Approximately 85% of the Aboriginal patients seen by the optometrist in the Program are not in need of ophthalmologic treatment. Many are referred to the AMS or another GP for a range of health or eye related reasons.
Spectacles and other visual aids are made available by means of 'community friendly' forms through the VisionCare NSW program. The program is promoted by the display of relevant health promotion posters in strategic locations.
Optometrists employed in the program have an MOU with ICEE. Some are employed on a paid dollar daily or half day rate; some opt to retain the bulk-billed fees.
A particular focus of the program has been the provision of ongoing care for members of Aboriginal communities with diabetes. Diabetes and associated eye disease is prevalent among the Aboriginal population. In many communities, 10 to 30% of people have diabetes9, which is the fourth highest prevalence in the world. People with diabetes are at risk of blindness due to diabetic retinopathy, but regular eye checks and treatment can prevent vision loss. The recall system established through the Eye Clinics ensures that these regular checks take place. Fifteen per cent of Aboriginal patients attending the Eye Clinics have been diagnosed with diabetes and have been introduced into a regular eye review program as part of a Diabetes Prevention of Blindness program. Diabetic retinopathy may be present in 8-35% of Aboriginal people with diabetes10 and in the Program, 16% of those with diagnosed diabetes were found to have some level of diabetic retinopathy. It can be expected that as a result of these regular examinations very many of these people will avoid blindness or seriously impaired vision which would otherwise have been a complication of their diabetes.
The most important strategy of the Program has been collaboration. This involved working through, and with, Aboriginal community-controlled health services and the local communities themselves, which ensured that programs were developed in accordance with community needs and sensitivities. It also ensured that services are provided in a culturally sensitive environment. Collaboration also involved harnessing the contributions of a number of State, Federal, community and professional organisations and individuals. This was essential to the development of sufficient resources and has also provided efficiencies in service and resource provision, which are essential to the ongoing success and sustainability of the Program.
The cooperative nature of this program is exemplified by various contributions to the Redfern Clinic: the Commonwealth supplied the equipment; the NSW Department of Community Services supplied half the optometric expenses; ICEE supplied the other half; the AMS supplied the facility and administration; Medicare pays for the eye examination; and VisionCare NSW (the manager of the NSW Spectacle scheme) supplies the spectacles.
Program achievements, monitoring and evaluation
ICEE now has a presence in over 60 locations in NSW, with effective collaboration established among ICEE, AHMRC, AMS and local optometrists. There have been approximately 8000 consultations, and in many cases the patients attending the clinics have never been seen by an eyecare practitioner before. Patient data is collected by ICEE through regular reports from the optometrists involved in the Program.
Unfortunately, reliable and comprehensive data on both Aboriginal population statistics and healthcare needs for assessment purposes are difficult to obtain. Census data may not accurately reflect indigenous populations, and health data are commonly drawn from small and/or regional studies. However, some analysis is possible of the impact of the ICEE/AHMRC Program, particularly in the area of the main cause of vision impairment in Aboriginal communities, which is refractive error1.
It has been estimated that refractive error occurs at a rate of 20%5, and that there is significant unmet need in the Aboriginal community for refractive services7. The Aboriginal population in NSW was estimated to be 109 900 from a total State population of 6 204 700 11. Thus it can be estimated that over 22 000 Aboriginal people in NSW require refractive correction, for example with spectacles.
The effectiveness of the ICEE/AHMRC Program is well evidenced by the increased use of the NSW Government Spectacle scheme by Aboriginal people. Approximately 80 000 spectacles are distributed each year to low income earners in NSW through the scheme, which is conducted by VisionCare NSW. Until the establishment of the ICEE clinics, it was estimated that less than 20 of these each year were Aboriginal people. Now over 5000 Aboriginal people in need have received free spectacles through the scheme. In the year ending 30 June 2002, 2642 Aboriginal people were provided with spectacles through the scheme, representing an increase of 58% on the previous year. ICEE maintains linkages with VisionCare NSW to monitor and obtain data on Aboriginal use of the scheme. The 8000 Aboriginal people seen in the clinics represent 7.3% of the NSW Aboriginal population.
ICEE monitors the Program both through the collection of patient data from optometrists and VisionCare NSW, as discussed, and through continual interaction with the Aboriginal communities. The success of the program is indicated by the positive response of these communities and the Aboriginal organisations involved. The Board of the AHMRC has consistently reported to ICEE staff that the ICEE/AHMRC Program is one of the most successful of any of the Aboriginal health programs in their services. Individual AMSs have welcomed the addition of eye services, and work enthusiastically with ICEE staff to schedule services. Feedback from patients has been excellent, and services are well attended by patients, indicating acceptance among the Aboriginal communities.
The ultimate measure of the success of the development and implementation of an eye health and vision care system is the prevalence in Aboriginal people of the diseases, eye disorders and general health-induced conditions that affect vision, and Aboriginal consumer satisfaction, and improved quality of life. Initial measures are encouraging, and ICEE will continue to monitor these to ensure the most effective deployment of resources and organisation.
Program analysis
The achievements have been made possible by a number of organisational features of the program:
- The program reaches people in need. By offering services within Aboriginal community-controlled health services, and by offering bulk-billing and spectacles through the NSW Government scheme, many of the barriers to Aboriginal people receiving eye and vision care are removed.
- The program is cost effective and a good use of resources. It makes good sense to use the less costly optometrist to provide primary care and to find the 15% of the community who need ophthalmological care, rather than have all examined by the more costly ophthalmologist.
- An appropriate recall system ensures that ongoing care is provided.
- Patients with diabetes are subject to regular eye review in accordance with NHMRC and National Diabetes Strategy guidelines. This is a degree of control and ongoing service not previously available to Aboriginal communities, who are particularly in need of diabetic care.
- Local optometrists are utilised and this provides a high degree of continuity of practitioner, which ensures good quality of service, appropriate follow up and a good practitioner/patient relationship.
- A combination of regional optometrists and regular service visits is used so eyecare services can be provided in relatively small Aboriginal communities on a regular basis.
Current issues
- As the program becomes larger staffing management issues (eg annual and maternity leave, or changing practice arrangements that encroach on existing arrangements) are being encountered.
- Some communities are so isolated and or so small that the present ICEE program will not reach them.
- Not all optometrists practice in conformity with the terms of their MOU (eg statistics are not always forwarded; all Visioncare frames are not always shown), and not all EHCs screen in accordance with the program.
- Only 2 of the 7 EHCs appointed in 2000 remain. For a range of reasons they move on, requiring training for new staff and the re-establishment of community links.
- The Aboriginal community is an extremely mobile community, making continuity of service difficult. For example, patients examined in Nowra may eventually collect their spectacles in Brewarrina.
- There is a relatively high turnover of spectacles as a result of loss and breakage.
Nevertheless it is clear that the placement of eyecare services within ACCHSs is an effective strategy. Aboriginal people respond to Aboriginal people; they are more likely to return for a review if they are reminded by the AMS staff than if reminded by non-indigenous people, and Aboriginal Health workers are able to locate and transport people who don't keep appointments. Eye Health Coordinators also help to develop and maintain relationships with the communities, and to conduct screening to groups in need.
The future
The ICEE Program is continually being developed and refined in order to make it more efficient and hence more productive. The Program has also steadily expanded over its life, and will continue to expand as needs are identified, for example.
- There are many rural areas with ACCH facilities and relatively large Aboriginal populations at which a regular and ongoing optometric service is yet to be developed; examples include Newcastle, Tamworth, Gunnedah, Coffs Harbour, Lismore, Lake Macquarie, Batemans Bay.
- There are many smaller Aboriginal communities, located in the main in the remote north west, south west and north eastern areas, which the present ICEE program will be unlikely to cover. These can be best served by a mobile eye team. One team working in these three areas initially for 1 week each month may well satisfy the needs of these smaller populations. Examples of such places include Menindee, Wilcania, Ivanhoe, Hatfield, Bowraville, Moulamein, Balranald, Carinda, and Coolabah.
Lessons
The ICEE/AHMRC Aboriginal Program set out to test whether a service could be developed that would be utilized by Aboriginal communities throughout the State, and that was viable and sustainable.
The Program has shown that such a service should be:
- Conducted under the auspices and control of the local Aboriginal community.
- Organized and delivered through ACCHS.
- Coordinated by Regional EHC.
- Well supplied with patients by cooperative activities and population screening by EHC and ACCHS staff.
- Serviced by locally-based primary eyecare professionals (optometrists).
- Providing on-site dispensing of low-cost spectacles and rapid delivery of more complex prescriptions.
- Referring to secondary care personnel (ophthalmologists) at regional hospitals.
- Organising visits of appropriate team members to smaller and more remote community centres.
- Conducted with the cooperation of GPs and other key health personnel.
Importantly, the Program to date has demonstrated that such a scheme can be self-sustainable. Providing that the Medicare benefits for optometric consultations remain available and there are no major adverse changes in the NSW Government spectacles program, the ICEE/AHMRC Eyecare program in NSW should ultimately operate at a small profit.
The effectiveness of this program may have relevance to other rural regions, both in Australia and internationally where eyecare for indigenous populations is also in need. To conduct a similar program in other regions would require cooperation from the local body equivalent to AHMRC, an available optometric workforce and a program which would enable spectacles to be made available at little or no cost. It would also, at least initially, require a coordinating body to undertake the role taken by ICEE in NSW.
Acknowledgements
The establishment of the Eye Clinics is a collaborative effort involving ICEE; Aboriginal Health & Medical Research Council of NSW; University of New South Wales; Cooperative Research Centre for Eye Research and Technology; VisionCare NSW; Commonwealth Department of Health and Aged Care - Office for Aboriginal and Torres Strait Islander Health, NSW Branch; Department of Community Services; NSW Health, Aboriginal Health Branch; Royal Australian and new Zealand College of Ophthalmologists (NSW).
References
1. Royal Australian College of Ophthalmologists. The National Trachoma and Eye Health Program. Sydney, NSW, Australia: Royal Australian College of Ophthalmologists, 1980.
2. Taylor HR, Livingston PM, Stanislavsky YL, McCarty CA. Visual impairment in Australia: distance visual acuity, near vision, and visual field findings of the Melbourne Visual Impairment Study. American Journal of Ophthalmology 1997; 123: 328-337.
3. Van Newkirk MR, Weih L, McCarty CA, Taylor HR. Cause-specific prevalence of bilateral visual impairment in Victoria, Australia: the Visual Impairment Project. Ophthalmology 2001; 108: 960-967.
4. Wang JJ, Foran S, Mitchell P: Age-specific prevalence and causes of bilateral and unilateral visual impairment in older Australians: the Blue Mountains Eye Study. Clinical and Experimental Ophthalmology 2000; 28: 268-273.
5. Taylor H. Eye health in Aboriginal and Torres Strait Islander communities. Report for the Commonwealth minister of Health and Family Services. Canberra, ACT, Australia: AGPS, 1997.
6. Hecker R. A Review of Eye Health Services for Aboriginal Communities in NSW. Office of Aboriginal and Torres Strait Islander Health, Commonwealth Department of Health and Family Services. Canberra, ACT, Australia: AGPS, 1998.
7. Wildsoet C, Wood J. Primary eyecare needs and services to Aboriginal and Torres Strait Islander populations across Queensland; a user's perspective. Clinical and Experimental Ophthalmology 1996; 79: 188-201.
8. National Aboriginal Community Controlled Health Organisation. NACCHO Website, available from: http://www.naccho.org.au/ (Accessed 21 January 2004).
9. De Courten M, Hodge A, Dowse G, King I, Vickery J, Zimmett P: Systematic review of the epidemiology, aetiology, pathogenesis and preventability of diabetes in Australian and Torres Strait Islander population. Canberra, ACT, Australia: OATSIH, 1998.
10. Thomson N, Paterson B. Eye health of Aboriginal and Torres Strait Islander people. Edith Cowan University, Report No 1. Perth, WA, Australia: National Aboriginal and Torres Strait Islander Health Clearinghouse, 1998.
11. Australian Bureau of Statistics: Aboriginal and Torres Strait Islander Australians: A statistical profile from the 1996 Census. Year Book Australia. Sydney, NSW, Australia: ABS, 1999.



