Introduction
Mental disorders constitute the leading cause of disability burden in Australia 1. To address this situation, the Fourth National Mental Health Plan (2010–2014)2 proposed a whole-of-government approach to building continuity of care to facilitate the recovery of people living with mental illness. In this context, recovery does not imply cure or being symptom-free, but instead refers to 'rebuilding a sense of purpose, agency, and meaning in life, despite the limitation of a disorder'3 (p. 5).
Mental health recovery theory4 conceptualises mental illness as the product of biological, psychological, social, cultural and economic factors, and posits that people with or without the presence of mental health problems have the capacity to create and live a meaningful and contributing life. Qualitative studies5-8 have identified that recovery follows a developmental course of between three and five stages that can be mapped onto four descriptor labels coined by Spaniol and Koehler9: Stage 1 – Overwhelmed by the disability; Stage 2 – Struggling with the disability; Stage 3 – Living with the disability; Stage 4 – Living beyond the disability. From their review of the literature, Andresen and colleagues5 have summarised the key component processes of recovery, namely finding hope (the belief that recovery is possible), establishing self-identity (including a 'place' for illness in relation to the self), taking responsibility for recovery (self-management, goal-setting and autonomy) and finding meaning in life (identifying a sense of purpose and a way of functioning).
Models have been developed to guide recovery services, for example the Tidal Model10, which focuses on values and competencies; the Wellness Recovery Action Plan11, which utilises peer-led illness self-management; and the Collaborative Recovery Model12, in which clinicians use evidence-based recovery skills. The model prescribed for Australian Government recovery programs is the Strengths Model13-15. This model has six operational principles, which emphasise a focus on strengths rather than deficits, the importance of the therapeutic relationship, self-direction, outreach, hope and a community focus (Table 1). Supporting this strengths-based approach are the findings of a recent systematic review16 in which 'strengths principles' were identified as 'the most promising' (p. 554) basis of recovery interventions.
A program developed to support Australian mental health recovery services is the Personal Helpers and Mentors (PHaMs) service17-20. Commencing in 2008, and funded by the Australian Government Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA) for delivery by non-government organisations, this non-clinical, community-based initiative aims to provide 'increased opportunities for recovery for people whose lives are severely affected by mental illness'17 (p. 3). Accordingly, PHaMs caseworkers – who typically hold a degree in an allied health profession – support and mentor people 'at risk of falling through the gaps' between state funded clinical treatment services and federally funded social services (such as supported housing, education and employment)17 (p. 6). Utilising the power of interpersonal relationships, PHaMs assists participants to connect with these services and engage in a 'recovery journey'.
PHaMs services anticipate outcomes that reflect participants’ progress towards social and economic inclusion17,20. As shown in the service logic model17 (Fig1), these outcomes follow caseworker tasks and activities and include increased access to appropriate support services, increased personal capacity and self-reliance, and increased community participation. The links between Strengths Model principles and PHaMs services and activities are shown in Table 1. Participants’ goals are set within an Individual Recovery Plan (IRP) and may deliver improved communication, interpersonal interactions and relationships; greater capacity to apply knowledge and meet cognitive demands (eg problem-solving and decision-making); independent living (ie self-care, domestic functioning and mobility); and greater participation in recreational activities, education and employment.
PHaMs caseworkers have three key roles17: direct involvement with the participant to provide assessment, monitoring and support; involvement with other agencies to facilitate referrals and linkages; and reporting and administration. The PHaMs guidelines17 suggest that caseworkers’ support for participants should occur along 'a continuum of active care' (p. 48) with intensity linked to 'stage of recovery' (p. 47) (Table 2). While each PHaMs participant has a key caseworker, to maximise the quality of service and support for participants and staff alike, caseworkers are to work as a team, creating 'cross-team support for all' (p. 22). Lastly, as already noted, a high level of rapport between a caseworker and a participant is considered essential to achieving recovery.
While there is evidence that PHaMs is achieving its aims in metropolitan areas21, and there are emerging reports of success in rural towns22, a national report identified that PHaMs 'works less well in rural areas [because] skilled staff and supportive structures are not readily available'22(p. 45). On the basis of this statement, and uncertainty about the operations of rural PHaMs services, the aims of the study were to explore how a service had been developed and functions in a low resource rural location, and to describe the outcomes that had been achieved.
Table 1: Operational principles of the Strengths Model and corresponding PHaMs program principles and activities17 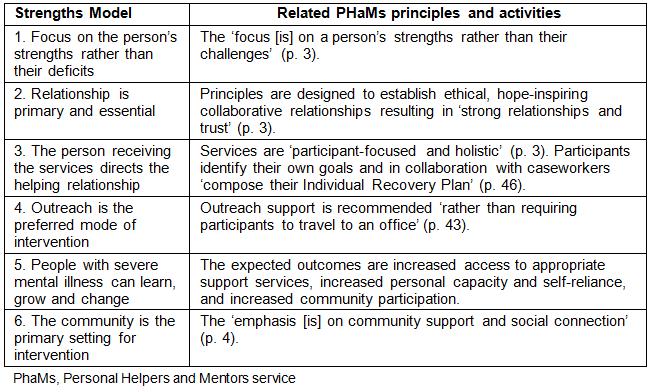
Table 2: Relationship between stages of recovery, PHaMs level of support categories, and the operational features of a rural PHaMs service 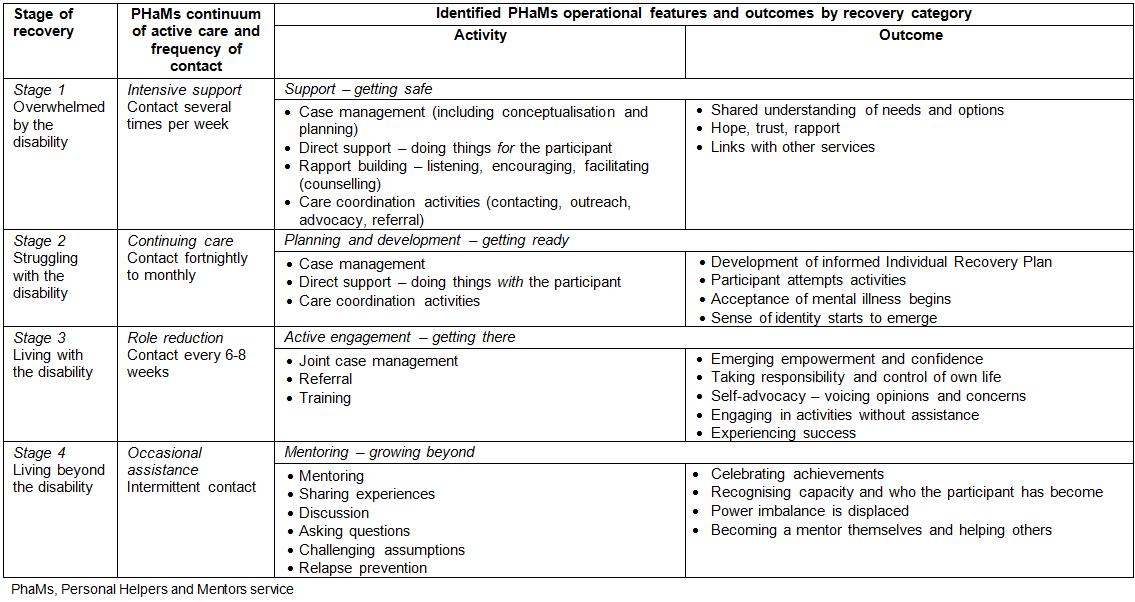
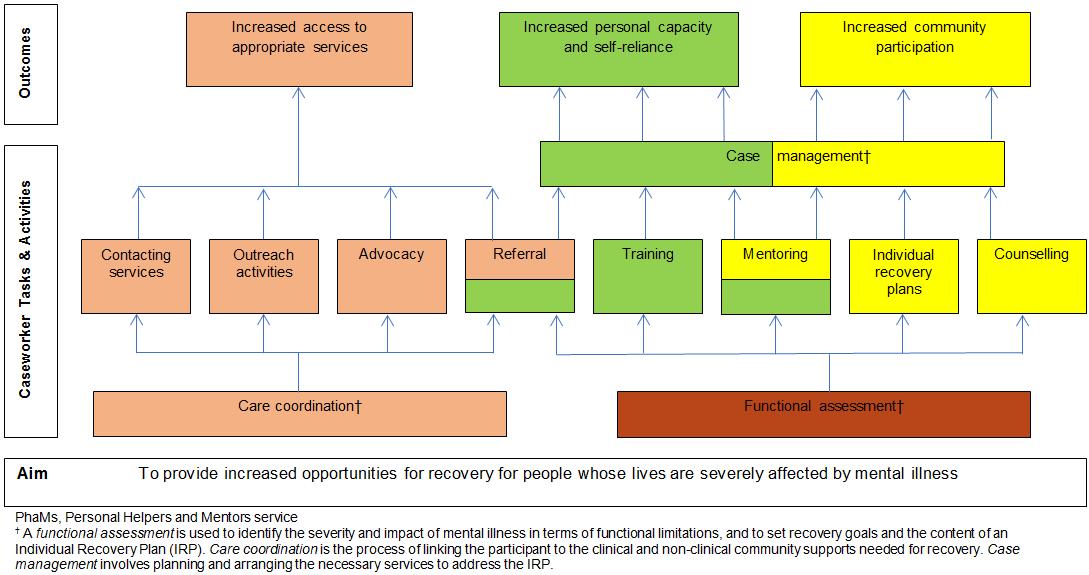 Figure 1: PHaMs logic model (adapted from the Draft PHaMs logic model (p. 78)17.
Figure 1: PHaMs logic model (adapted from the Draft PHaMs logic model (p. 78)17.
Methods
Study site
A rural town in New South Wales (NSW) in Australia was chosen as a case study site because of its sociodemographic features and the presence of a PHaMs service of almost 5 years duration (having commenced in October 2009). The 2011 Australian census23 found the chosen town to have a population of 7392 people. In 2014, the population of the wider local government area was estimated to be 14 00024. Of these, 49.4% were male and 50.6% were female. Aboriginal and Torres Strait Islander people made up 10.3% of the population. According to the local mental health services plan25, 2.5% of the total population was estimated to have a severe mental illness. On a set of measures that summarise different aspects of socioeconomic conditions in an area – the Socio-Economic Indexes for Areas – the town’s scores range from 3 to 4 out of 10 (where lower scores represent greater disadvantage)26. A community social and economic analysis of the town27, published in the same year as PHaMs commenced operations, reported that although the town had coverage for basic health needs, there were difficulties recruiting and retaining mental health service providers.
Study design
A mixed methods design was used. To address the first part of the study (how the service was developed and functions), a thematic analysis28 of local service documents coded for consistency with the Strengths Model was undertaken. For the second part (description of outcomes achieved), a quantitative analysis of uncontrolled pre-test–post-test and retrospect pre-test data29 was conducted.
Participants and procedure
Service development and function: General administrative data and nine documents30-38 produced by the service for the purpose of staff orientation or collaboration with other agencies were provided to the first author in June 2014. Analysis invoved coding of the semantic content and identifying overarching themes that captured the underlying meanings39,40.
Description of outcomes achieved: Participants were every client of the identified PHaMs service who had attended between its commencement in October 2009 and June 2014 (N=126) – the period during which the first author’s institution had a contract to monitor client outcomes via an online survey. The participants represented 31.1% of the estimated population of people experiencing severe mental illness (defined as equivalent to the US classification of 'serious and persistent mental illness') in the local government area (ie n=405)25,25. Of these, 26% were Aboriginal Australians. At initial interview, the service clients (termed ‘participants’) are routinely invited to consent to their anonymous data being used for quality assurance and research purposes. All had given this consent. By June 2014, 14(11.1%) of these had completed an IRP (mean duration 5.6 months; standard deviation (SD) 4.8 months; range 1.5–17.3 months); 15 (11.9%) had suspended participation in the service (eg due to hospitalisation or incarceration); 20(15.9%) had prematurely exited the program and 77(61.1%) were continuing as active clients. From the total sample, 51 (40.5%) had provided self-report data on two or more occasions.
A convenience subsample of 17 service participants (33% of the active client group in April 2012; n=51) gave additional written consent to take part in a semi-structured individual interview, which was developed and piloted in an earlier study0. Interviews of 30 to 60 minutes duration were conducted either by the first author or a research assistant. Interview questions elicited ratings and feedback comments on criteria based on the generic PHaMs program goals17,20 and FaHCSIA service requirements0. The interviewers documented the ratings and comments in field notes. Interviewed participants had been involved in an IRP for between 1 and 36 months.
Table 3 presents the means and frequencies of demographic features and diagnostic categories for the total group of 126 participants, the 14 IRP completers, the 51 participants who had provided self-ratings of subjective wellbeing, and the 17 participants who were interviewed.
Table 3: Mean age and frequency (percentage) of demographic features by samples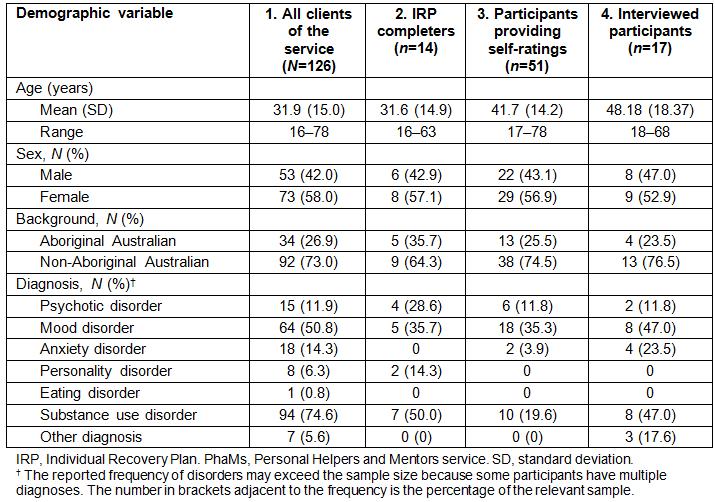
Measures for participants
Measures used for the second part of the study were chosen to assess progress in recovery through changes in wellbeing, functioning and social inclusion. These included participant self-reports and caseworker observational ratings.
Subjective wellbeing: At PHaMs review sessions, service participants provide current and retrospective ratings of global wellbeing in response to the questions 'How are you managing in general?' and 'How were you managing before you commenced with PHaMs?' Ratings are made on a 5-point scale (1=‘not managing at all’ to 5=‘managing very well’). In this study, the analysed data were the participants’ first and most recent ratings.
Individual recovery goals: A participant’s IRP goals are developed collaboratively and routinely reviewed and documented as part of the PHaMs service. Caseworkers assist participants to set IRP goals aimed at increasing access to services, personal capacity and self-reliance, and community participation. The documented gains are based on client self-reports corroborated by caseworker observations.
The next two variables were assessed via semi-structured interviews.
Gains in target outcome areas: During an individual interview, each consenting participant provides a current and retrospective rating of their functioning in the target outcome areas to be addressed by the PHaMs service (eg managing everyday tasks; Fig1). Items are rated on an 11-point scale (0='very poor' to 10='very good').
Service satisfaction and relationships: During the individual interview, each participant rates their satisfaction with the PHaMs service and their relationship with their key caseworker. Items are rated on an 11-point scale (0='very poor' to 10='very good').
Caseworker ratings of functioning
Role Functioning Scale (RFS)0: Caseworkers rate a participant’s adaptive functioning on four 7-point scales (1–7) allocated according to behavioural descriptors in the domains of work, independent living, and immediate and extended social networks. Total scores can range from 4 to 28. Scores exceeding 24 indicate optimal adult functioning, scores 20 to 24 suggest adequate functioning, scores 16 to 20 indicate moderately effective functioning, and scores less than 16 indicate varying degrees of limited functioning. Sound reliability (inter-item reliability: alpha=0.918; test–retest reliability per scale: r=0.85–0.92; inter-rater reliability per scale: r=0.64–0.82) and validity (discriminant analysis: 79% accuracy; significant correlations with self-esteem (r=0.40) and parenting ability (r=0.68) have been reported)0. The RFS has been amended for use in rural PHaMs units0. Cronbach’s alphas for the total RFS scores in this study ranged from 0.84 at commencement to 0.93 at closure.
Analyses of data collected for the second part of the study included calculation of descriptive statistics, repeated measures and between-groups comparisons, and identification of semantic themes from feedback comments, elicited to illuminate the quantitative ratings collected in the individual interviews.
Ethics approval
This study was approved by the University of New England Human Research Ethics Committee (approval no. HE11/166).
Results
Service development and function
In June 2014, the PHaMs service had seven staff members. Of these, five had a diploma and two had a Certificate IV qualification. Three overarching themes emerged from the document analysis.
1. The team had no clear guidelines on how a PHaMs service should be developed or delivered: The local program logic model38 and vignettes in the PHaMs program guidelines17,20 provided some information about how the components of a PHaMs service should be integrated, but there were no clear instructions on the processes involved, especially in a rural area. Therefore, the team focused on the service’s goal to support the 'recovery' of participants, then worked backwards and began with activity engagement.
To verify the legitimacy of their approach, the team surveyed established PHaMs sites and concluded that each had uniquely responded to its local context. For example:
The urban ones take on a background case manager role whereas rural PHaMs appear to have a more hands-on supporting role33 (p. 5).
Also unclear to the team at commencement was how activities mentioned in the guidelines were to be applied (ie 'support', 'care coordination' and, in particular, 'mentoring'). With time and experience, a developmental model of recovery was conceptualised wherein the listed PHaMs activities where integrated into a continuum of intensity of active care that varied according to each participant's needs and progression in their recovery journey (Table 2).
In sum, the official PHaMs service guidelines provided goals and a framework for operations but no details on how these should be carried out. Instead, examples of possible actions were described in brief case vignettes only. Therefore, by focusing on recovery outcomes, and using the resources that were available to them, the staff built the service on activities and processes they considered necessary and developmentally appropriate for participants.
2. Unconsciously, a strengths-based approach was applied to the development of the service: Documents also revealed that the service was established and developed by applying Strengths Model recovery principles to the staff and the service operations. Accordingly, when 'pulled together from the local community'31 (p. 1), foundational staff members saw themselves as having abilities well suited to the needs of the service and used these to guide service development and functions. In October 2009, a staff member wrote:
PHaMs [local town team] has a substantial mix of skills and expertise that neatly matches many of the issues of concern for participants and potential participants in the service area … [so we] built some structure around these skills32 (p. 21).
(Comments reflect the Strengths Model principle of a focus on strengths rather than deficits.)
Although 'the team struggled over how to define itself and its operations'30 (p. 1), there was no evidence of an assumption that a rural PHaMs service would be inferior, deficient or problematic0; instead, the documents show confidence in staff capacity to meet local needs. Specifically, those with a background in the disability sector informed actions in (what was later described as) recovery Stages 1 and 2 – getting safe and getting ready – and guided the 'support' activities involved in doing for and doing with participants who were at the beginning of their recovery journey. Staff with a background in the homelessness and the alcohol and other drugs sectors informed approaches to 'case management' and working with other services to promote Stage 3 – active engagement or getting there. A staff member with experience in business and leadership training directed approaches to Stage 4 – mentoring and growing beyond. Similarly, a member identifying as Aboriginal guided the development of a culturally safe service.
3. Teamwork undergirds successful operations in a rural setting: Application of the Strengths Model principle ‘relationship is primary and essential’ combined with 'trust and rapport' was key to establishing an effective team and successful collaborations with other agencies.
We work together as a team and team up with our peers in other agencies32 (p. 1).
Multiple strategies were (and continue to be) used to build and maintain a strong team (eg meeting each morning to address items from the fortnightly staff meeting, having lunch together regularly and debriefing when required30). Documents assert that it is the team’s corporate strength and regard for each other that permits 'heated but respectful debate'30 (p. 3) during case reviews, and that this is central to progressing participants’ recovery journeys.
Interagency cooperation and coordination were also built on relationships often forged through past links and the networks of individual team members. Yearly plans37 reveal that the service seeks to continually strengthen these relationships while identifying and building others. An initiative of the PHaMs service has been the formulation of a governance document – an Interagency Group Work Agreement35 – that sets out principles, benefits and boundaries for cooperation between local services, thereby protecting the integrity of smaller agencies that may fear a 'predatory approach'30 (p. 2) to their programs. It also makes clear that clients’ needs are the primary purpose of cooperation, and recovery is the ultimate goal.
Our model is not to get a bigger slice of the pie – instead we make the pie bigger30 (p. 2).
Interagency cooperation and coordination is recognised as the key and the solution to resolving service gaps and deficits35 (p. 1).
Participant outcomes
Outcome data was obtained from self-ratings and caseworker ratings of participants’ functioning.
Subjective wellbeing: Self-ratings of wellbeing were obtained from active service participants (n=25) who had provided data on at least two occasions. The mean length of engagement with the service was 13 months and 26 days (SD 9 months and 26 days). Participants’ retrospective ratings of wellbeing prior to commencement with PHaMs were similar on both occasions (t(50)=0.77, p=0.447, two-tailed); however, the ratings of current wellbeing showed a statistically significant increase from the first to the most recent rating time (t(50)=–4.21, p<0.001, two-tailed).
Individual recovery goals: Findings from the total sample (N=126) showed that participants had set and reported gains on a range of recovery goals, including physical health and wellbeing, education and employment, interpersonal functioning and involvement in the community.
Gains in target outcome areas: All interviewed participants (n=17) reported improved functioning in household activities and managing finances. Other gains by percentage of participants included improved relationships (59%), increased access to clinical services (41%), improved management of medications (35%) and greater satisfaction with living arrangements (53%). Although 41% were unemployed and not participating in education or training, 59% of these indicated a desire to participate in such activities. Feedback comments attested to the contribution of the PHaMs service to these outcomes:
I probably wouldn’t have gone [to the Community Mental Health Service] if they didn’t help me.
They helped me move to a unit in [local town]. Now I live in a nice environment with plenty of room.
(Comments reflect the Strengths Model principles of client self-determination, holistic services and community connection.)
Service satisfaction: Interviewed participants rated the service received as follows: overall satisfaction 7.8/10 (SD=1.8), confidence in the service to help them in the future 8.03/10 (SD=1.59) and likelihood that they would recommend the service to a friend 8.67/10 (SD=1.17). Feedback comments included:
They help me sort stuff out. They talk to me and give me confidence.
(Comments reflect the Strengths Model principles of building relationships and trust, and supporting clients in personal growth and change.)
However, some participants were not fully satisfied and felt stigmatised by some activities:
I feel embarrassed about being seen in town with [service] workers. It’s a small town and people know who they are. There is a stigma attached.
(While this comment reflects the Strengths Model principle of outreach as the preferred mode of intervention, it also highlights the need to balance this against privacy issues in small communities.)
Service relationships: Interviewed participants rated their relationship with their key caseworker at an average 8.6/10 (SD=1.3). This overall favourable rating was reflected in comments that indicated the presence of rapport and therapeutic alliance. For instance:
I feel [the caseworker] is very trustworthy.
(Comment reflects the Strengths Model principle of building relationships and trust.)
Caseworker ratings of participant functioning
Caseworkers’ observational ratings using the RFS indicated that the adaptive functioning of the IRP completers (n=14; mean length of engagement with the service 19.5 months, SD=9.6) was significantly higher at case closure (mean=21.57, SD=3.74) than at commencement (mean=15.93, SD=6.45; t(13)=–3.72, p<0.003, two-tailed, r2=51.6%). On average, participants improved by 5 to 6 points, resulting in the final RFS scores representing adequate levels of functioning. Notably, the IRP completers’ commencement scores were not significantly different to those of the continuing, suspended or exited participants (mean=13.57, SD=4.81 n=112; t(124)=1.66, p=0.099, two-tailed).
Discussion
This study investigated the PHaMs service in a rural town in NSW, Australia. The aims were to explore how a service had been developed and functions in a low resource rural location, and to describe the outcomes that had been achieved. In line with recovery research0, data included not only quantitative 'outsider' measures of the therapeutic endeavour, but also 'insider' knowledge based on the experience of the staff working in the service. Consistent with the recovery movement, the 'insider' knowledge was available in documented 'stories' of the service’s development.
The overall findings were that in the absence of clear formal guidelines on how to develop and deliver a recovery-oriented, non-clinical, mental health service, the staff had unconsciously – perhaps using procedural knowledge0 – applied a Strengths Model approach. This included a particular priority on the model’s principles with respect to relationships, which were interpreted to mean that both a strong team and interagency networks were essential for success. Thereafter, and in accordance with the PHaMs guidelines, activities to support the recovery of people living with severe mental illness were devised using a backwards planning approach0.
In contrast to the circumstances and outcomes described in a national evaluation of PHaMs services21 – that is, that rural locations can be 'impoverished service environments … [that create] … an insurmountable barrier to quality service' (p. 56) – this study found that limited professional and community resources had been overcome by staff taking a strengths-based rather than a deficit approach to the resources that were available. In terms of human resources, the staff did not have academic qualifications equal to those in the majority PHaMs services (ie a degree in allied health)21, but by focusing on the knowledge and experience that they did have, and taking a creative team approach, they developed programs and ways of working that eliminated this perceived shortcoming.
In a submission to the National Mental Health Commission (2014) by the National Rural Health Alliance0, and when referring to the design of effective mental health services in rural and remote Australia, the Alliance asserts, 'Local people will know who is available in their area and the resources that can be drawn together for [a] program'(p. 23). This is what the PHaMs team in this study did. As locals to their town, they focused on their abilities and recognised that in a rural area they may need to fill service gaps. They did not see themselves or the community as deficient compared to the 'urban norm' (Bourke, et al., 2010, cited in ref 46). Instead, they believed that by 'displaying [their] internal teamwork and influencing others to adopt this approach [they would become] influential within the local service sector'30 (p. 2).
The document analysis revealed that the team modelled mental health recovery behaviours. That is, by respectfully dispensing with hierarchical structures, believing in and empowering themselves and making collaborative agreements to capitalise on limited community resources0, the PHaMs team addressed potential competitive or defensive responses that can silo and make invisible scarce community resources. Further, through open communication and the creation of trust, they drew out and used the resources that were present at the individual, team and community agency levels to achieve a 'necessary and sufficient'0 level of service.
This study found that not only can a non-clinical, community-based recovery service for people whose lives are severely affected by mental illness be developed in a rural area, it can also significantly penetrate its target population. Overall, the study’s results suggest that rural PHaMs participants who complete an IRP make gains in overall functioning, including the performance of everyday tasks, accessing clinical services, medication management, community involvement and employment. As called for by a NSW consumer advisory group0, these outcomes suggest a focus on self-management and empowerment, and a balance between a recovery orientation and the medical model. The outcomes parallel those reported in a national qualitative review of PHaMs21 and a study of another rural service0.
The rural location of the PHaMs service was not a barrier to participants’ use of most Strengths Model principles, including client self-determination, holistic services, community connection, trusting relationships and outreach13. However, some participants reported the ongoing challenge of stigmatisation when involved in community engagement activities. Other research has found that stigma reduction begins with interventions that empower affected individuals and include community level education, contact and advocacy0. Such programs, concurrently being offered by other services in the region0, may eventually lead to a reduction in this experience.
Finally, despite a reported national failure by PHaMs services to attract Indigenous participants21 (p. 24), in this study the Aboriginal community had accessed the identified PHaMs at a frequency 2.6 times that of its presence in the local government area (ie 27% compared to 10.3%). Additionally, these participants constituted more than one-third of those who had competed a recovery plan. The cultural safety created through the employment of Indigenous staff and the sensitive practice of others0 is likely to have supported this outcome.
The limitations of this study include the use of uncontrolled data and potentially biased small samples that restrict inferences about causality and the generalisability of findings. Specifically, although the sample included all service participants, only a small percentage had completed an IRP and exited the service; almost two-thirds were ongoing consumers of the service.
Conclusions
The findings of this study suggest that a strengths-based approach to service development – one that prizes interpersonal relationships and teamwork to maximise the potential of all local human and other resources – is perhaps 'one solution to resolving service gaps and deficits'35 in rural and regional areas. Once established, PHaMs services assist some rural Australians with severe mental illness to achieve recovery in a relatively short timeframe. However, for many, ongoing support for a longer recovery journey is required.
Acknowledgements
This study was funded through an agreement between Centacare New England North West and the first author’s institution. We thank Owen Atkins, Darren Baxter, Cassie Bigarelli, Karen Larsen, Nikki Thorn, Amber Varcoe and Cigdem Watson from the Personal Helpers and Mentors service, Centacare New England North West Narrabri, for providing relevant documents and participating in a clarifying discussion session.
