Introduction
Mexico is a socially heterogeneous country with a population that includes thousands of families living in extreme poverty in the mountains, on the brink of survival, without any food, education, housing or health services1. Simultaneously, the population includes prominent members on the Forbes World’s Billionaires list, including the richest man in the world. Between these extremes, an entire range of social nuances exists. Therefore, it is impossible to objectively discuss Mexico in terms of a single category or national average, such as the categories managed by the Food & Agriculture Organization and the United Nations (UN). From a qualitative perspective, it is possible to reach a more objective and reliable analysis that provides a demographic division between Indigenous, rural and urban areas.
Qualitative division separates divergent social worlds that cannot be combined without the risk of obscuring the reality of the rural world and, above all, that of the Indigenous world. The methodological error derived from averages that both conceal and erase extreme poverty in rural zones has been widely demonstrated2. In Mexico, the Indigenous peoples of the Sierra Tarahumara (one of the most marginalized regions) represent one example of erasure in studies that use national and state averages3 with the associated imprecisions previously discussed.
Poverty, particularly extreme poverty, is primarily concentrated in the rural regions of countries in transition4. One study conducted in 36 low-income countries clearly demonstrates that the problem is by and large exclusive to rural zones. The investigation demonstrates this finding using data on malnutrition among rural children in comparison with children from urban zones5. Similarly, some researchers have identified contrasting differences between the rural and urban populations in countries in transition in Europe6. The same phenomenon has been shown in Latin America at the regional level, where poverty is concentrated in rural zones7.
Medical services coverage shows the same pattern. According to the most recent report by the International Labor Organization, more than half of the world’s rural population lacks access to health services, particularly noting African countries8.
In a country-by-country classification, the situation is practically identical. For example, according to World Bank statistics, 51% of the population in China is rural9 and living in extreme poverty10; nevertheless, China was one of the first countries in the world to reach the UN Millennium Development Goals, reducing extreme poverty by half between 1990 and 201511. In Latin America, rural poverty has been analyzed in detail in a comparable manner in Ecuador and El Salvador12,13. Likewise, researchers have found marked differences between rural and urban areas in terms of food and nutrition security in Mozambique, a south-east African country14.
A similar phenomenon occurs in Indigenous zones across the world. Although it is true that almost all Indigenous areas are found in rural zones, not all rural zones are Indigenous. In that context, nearly 400 million Indigenous people on the planet are living in extreme poverty, characterized by the lowest levels of development in health, malnutrition, overcrowding and infections15. Without question, the Indigenous groups of the world live under ongoing marginalization16. According to the conclusions of the United Nations 5th session of the Permanent Forum on Indigenous Issues, millions of Indigenous peoples spread over 70 countries across the world continue to be among the poorest social strata17. Locations with Indigenous populations are a separate category that should not be studied in combination with high social strata in large cities within the same countries. What may or should occur, at the very least, is the differentiation of the target population into Indigenous and non-Indigenous to reach more objective results18,19.
The phenomenon of extreme poverty in the Indigenous population is replicated in Latin America. Studies estimate that more than 400 different Indigenous groups remain the most marginalized20,21. Presently, 62 ethnic groups exist in Mexico, accounting for approximately 8% of the population. Mexico, not only at the national level22 but also in federated states such as Oaxaca23 and Veracruz24, have a high percentage of marginalized Indigenous people. Many of these groups are threatened with extinction3,25.
Extreme poverty has been an ongoing conflict since the origins of humanity, and its most severe manifestations are undeniably hunger and disease26. In contrast to urban Mexico, in the sierras and mountains of rural and Indigenous Mexico, hunger and its afflictions have been a historical reality. It seems that for these communities, time has stood still and social development is excluded by definition. The living conditions of the majority of families in the poorest localities go unnoticed in official circles at the municipal, state and national levels and, thus, by their social programs and health service coverage as well. Therefore, the objective of this investigation was to study the marginalization and public health service coverage among urban, rural and Indigenous populations in Mexico.
Methods
Mexico has 32 federated states and 2456 municipalities. These municipalities have 107 458 localities that represent the greatest level of administrative territorial disaggregation in the country. For this study, we use the most recent database from the last official national population census of localities in 2010. Localities in the country were used as the experimental unit. Databases from the National Institute of Statistics, Geography and Information Technology were obtained27; data from the National Population Council (CONAPO)28, the National Commission for the Development of Indigenous Peoples (CDI) and some estimates from National Council for the Evaluation of Social Development Policy (CONEVAL) based on the Population and Housing Census in 2010 are also used29,30. The study employs the official definition of a rural population that CONAPO has used since 1930, in which rural localities are those with a population of fewer than 2500 inhabitants. Urban settlements are defined as having a population of greater than 2500 inhabitants. For work related to the Indigenous population, the study uses the CDI classification, which describes Indigenous towns as those where more than 40% of the population speaks a language or dialect belonging to any of the country’s 62 ethnic groups. Furthermore, it is noteworthy that there are an additional 29 909 localities with an Indigenous population of less than 40% that are not officially considered Indigenous. These localities have percentages that range from 1% to 39%, and are considered to fall under the rural category. The present study is a retrospective, comparative and analytical study conducted to understand the situation of marginalization and lack of health services among the rural, urban and Indigenous populations in the year 2010.
Snedecor’s F-test and Kruskal–Wallis tests were applied to compare means (α=0.05) of the marginalization index categories between Indigenous, rural and urban localities. Snedecor’s F-test is an analysis of variance that is best utilized to compare the means of big data with numerical information while the Kruskal–Wallis test is a non-parametric analysis of variance with ordinal variables. Additionally, Spearman’s correlation was performed to associate two ordinal variables: population type and degree of marginalization. The gradient of marginalization follows the index developed by the National Population Council28, which established five intervals: very high, high, medium, low and very low and was used to classify the 107 458 localities. The study takes the percentage of the population that is not eligible for health services (population without medical coverage) from the social gap index, developed by the National Council for the Evaluation of Social Development and Policy30. The numeric data were transformed into five intervals from the percentages of the population without health coverage into homogeneous subgroups: (1) 0–30%; (2) 30.01–40%; (3) 40.01–60%; (4) 60.01–80%; and (5) 80.01–100%.
Ethics approval
The Research Ethics Committee from the National Institute of Medical Sciences and Nutrition Salvador Zubirán has reviewed and approved this research under the registration number SNE-1862-16-16-1.
Results
The Indigenous population represents 7.9% of the country’s total population and is found in 21.6% of all localities. The rural population comprises 17.7%, distributed among three-quarters of the localities. The three-quarters of the population who belong to the urban area are concentrated in 2.9% of the country’s localities (Table 1).
Table 1: Number of inhabitants and localities in each category in 2010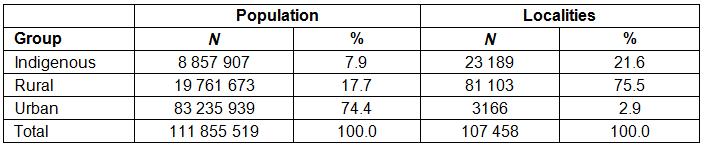
Comparison between population areas with respect to average marginalization and lack of access to health services
Significant differences were found among the mean levels of marginalization in the three areas of study (Indigenous, rural and urban). The Indigenous areas were the most marginalized and the urban areas the least (Figure 1). Similarly, each locality was analyzed according to its number of inhabitants in the three population types (Indigenous, rural and urban) and the significant differences were also found; in other words, to know the total number of inhabitants that have no health service coverage classified into Indigenous, rural and urban areas, we considered the total number of inhabitants independent of the number of localities. In the Indigenous and rural areas, marginalization is greater than in urban areas (Table 2). In relation to lack of medical coverage, the Indigenous area was the most disconnected from government health services. Nearly half of the population of Indigenous localities (45.6%) does not have access to medical coverage. The lowest percentage of persons not affiliated with health services occurred in the urban sector. These results are statistically significant. Similarly, Indigenous inhabitants were those with the highest percentage (40.9%) of non-eligible persons.
The urban area has the lowest percentage without medical services (32.6%).
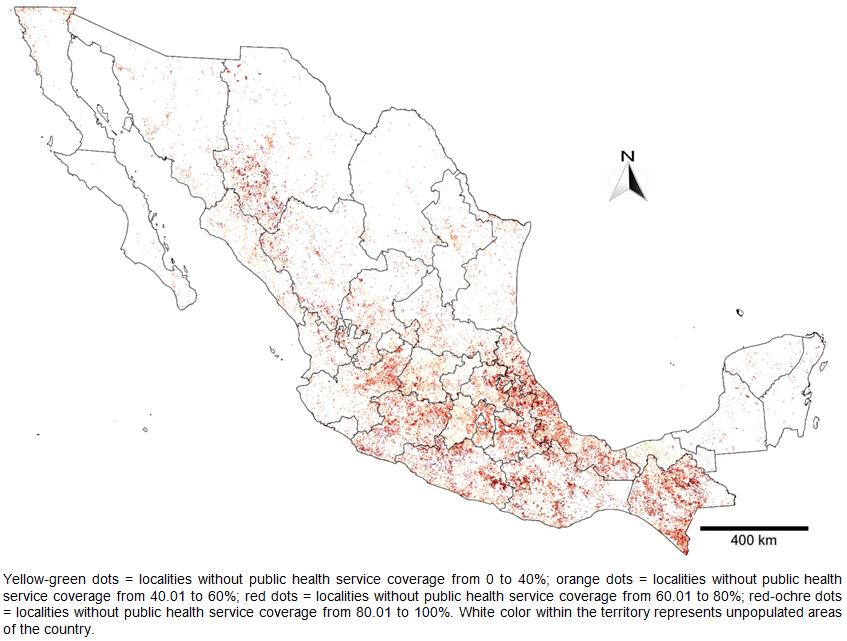 Figure 1: Distribution of the Mexican population without public health service coverage.
Figure 1: Distribution of the Mexican population without public health service coverage.
Table 2: Average marginalization score and percentage of people without health services coverage in 2010 for Indigenous, rural and urban populations 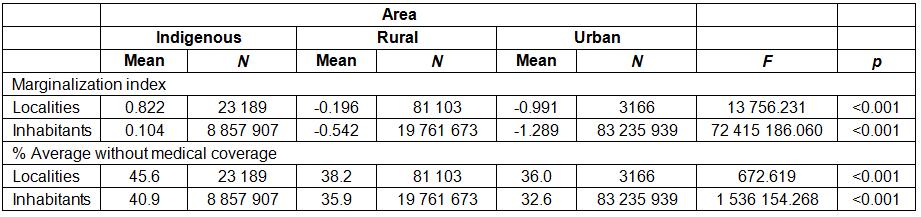
The prevalence of the degree of marginalization by population area
Comparing the degree of marginalization between the Indigenous, rural and urban populations, we found that 98% of the localities in the Indigenous areas and 75% of rural localities fell under the high and very high classification of marginalization. In the localities in urban areas, no polarization was found, and the highest percentages were distributed between low, medium and high marginalization. However, the very high marginalization was almost zero. The differences were statistically significant between the three areas (Table 3).
Table 3: Distribution of localities by study area and by 2010 degree of marginalization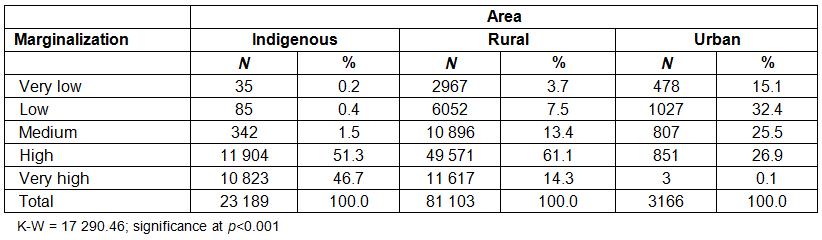
Correlation between population area and degree of marginalization
The correlation was calculated between the type of area and the degree of marginalization, taking account of the number of inhabitants in each town. Spearman’s coefficient was negative (–0.687), from which it can be inferred that the greater the marginalization, the lower the impact in the most favored social strata, which is urban. This finding confirms that a hierarchy exists between the study areas. As a result, these social strata exist on a continuum that ranges from precarious conditions in Indigenous areas to more favorable conditions in urban areas (see Table 4).
Table 4: Correlation between the population area and the degree of marginalization in 2010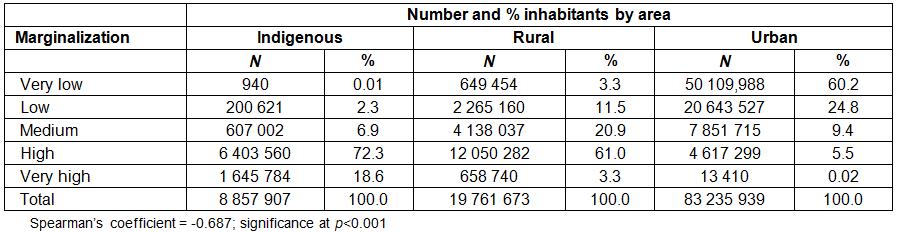
Correlation between degree of marginalization and lack of health services
The 0.288 correlation between degree of marginalization and lack of medical coverage was positive and significant (p<0.001), indicating that the higher the marginalization, the higher the percentage of lack of medical coverage. Figure 2 shows the distribution of the degrees of marginalization of the localities with the highest percentage of population without access to health services (interval 5). As marginalization increases, the percentage of those localities also increases.
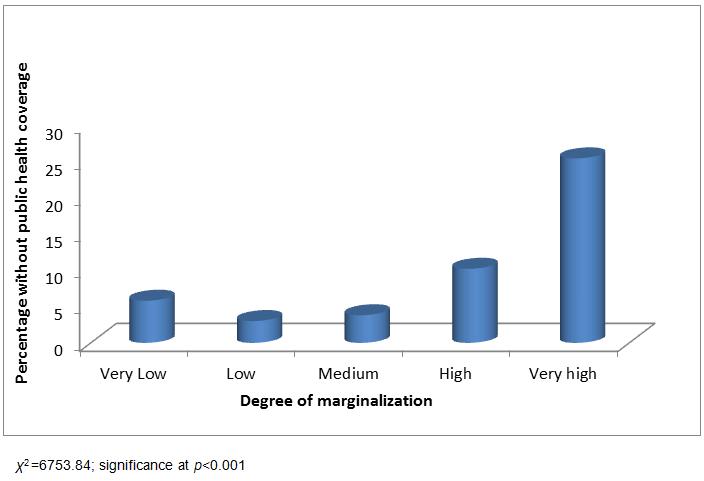 Figure 2: Distribution of population in terms of percentage without health coverage by degree of marginalization.
Figure 2: Distribution of population in terms of percentage without health coverage by degree of marginalization.
Finally, a correspondence analysis was performed to ascertain how the five intervals in each area of the study cluster. Figure 3 shows that interval 5, which involves the highest percentage without health services coverage (80.1% and above), is mainly related to the population located in the Indigenous area. Meanwhile, interval 60.1 to 80% is associated with rural areas, and the least affected interval in health services (0 to 30%) corresponds to the population in urban areas. Figure 3 clearly demonstrates how a lack of access to health services is an issue that mainly corresponds to populations living in rural and Indigenous communities.
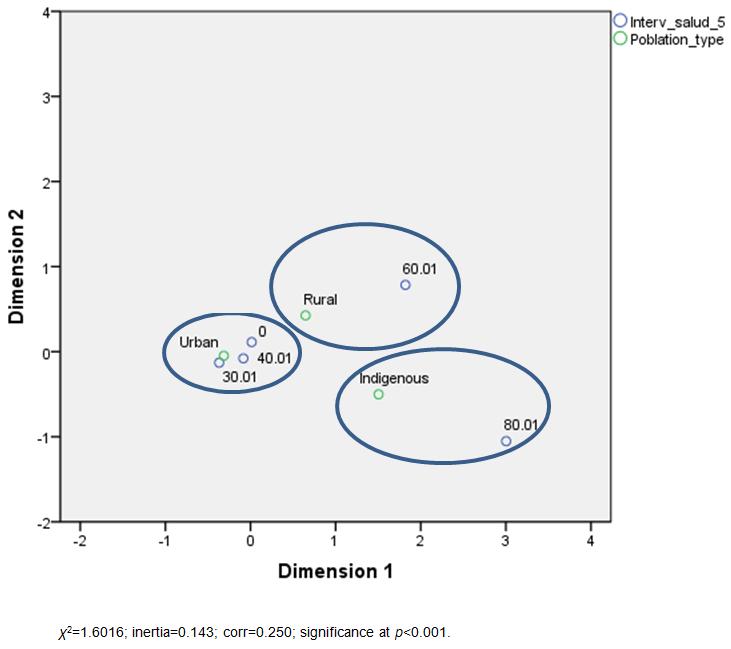 Figure 3: Distribution of five intervals without medical coverage in each type of locality: Indigenous, rural and urban.
Figure 3: Distribution of five intervals without medical coverage in each type of locality: Indigenous, rural and urban.
Discussion
A full analysis of 107 458 localities sheds light on an unknown scenario within the overall national focus in Mexico. The analysis highlights the local needs and problems that cannot be seen in general contexts or state and national averages2. Therefore, it is imperative to reexamine the rural and Indigenous scenarios, preferably by studying the Indigenous population in a separate category to obtain the best results18, as in the present study. This is line with the recommendation of a study carried out in the region of Kerala, India – an excellent work that considered the division of the population into Indigenous versus non-Indigenous and health coverage services19. Likewise, any study of social polarization in Mexico must be preceded by a division of the population into urban, rural and Indigenous. Anyone who omits this qualitative separation in the analysis, quite simply loses objectivity and has results that would not reflect the reality of Mexico.
It is recommended to study the micro-regional universe, which is only accessible through case studies on the geographical scale of localities, their individual histories, and the histories of their inhabitants, their ethnicities and their homes31. The Indigenous population is recognized as a historical constant that occupies the bottom rung of social development not only in Mexico but around the world17. This situation in Mexico at national level is also repeated at the state level, given that the states with the largest Indigenous populations also have greater marginalization and a worse lack of basic health services23,24. As socially critical regions of the country, the situation in rural areas is not an issue that is unique to Mexico; it is a global issue that is prevalent in nations with high social heterogeneity such as China10,11 and Mozambique14.
Nevertheless, the problem exists within a large contradiction, an unlikely paradox. Especially when we consider that socially critical zones are rich in food and natural resources, studies have shown successful proposals to benefit poor rural farmers in Mexico32. What is occurring, as this study has clearly shown, is the concentration of marginalization in the majority of rural localities, which, historically, are the majority and remain the same4. They are the mountainous areas where elements of progress do not reach and from where one escapes at the cost of identity, culture and way of life. Alternatively, we observe less marginalization in the majority of urban localities, which, historically, are the minority and where the benefits of social development are monopolized19. Impoverished communities have the misfortune of living on the precipice, under conditions of high social inequality. In this setting, they are subject to whichever economic, political and climate turn that can break this fragile balance. The most recent example is the famine reported in the Sierra Tarahumara at the end of 2011 in Chihuahua, Mexico, where severe drought, combined with frost, destroyed vegetation and grasslands. These events triggered hunger and diseases in this ethic group, the Raramuri.
This phenomenon can also be observed more widely in Latin America6,7, where, similarly, Indigenous groups are recognized as the most marginalized20. We find obvious examples in the cases of Ecuador12, Brazil21, and El Salvador13. The social polarization in Mexico found in this study exposes extreme marginalization between the Indigenous and urban worlds and inequality of access to health services. The lack of public health service coverage most frequently occurs in Indigenous and rural localities. In those conditions, Indigenous and rural localities are deprived of fundamental necessities for preserving health and wellbeing status. For instance, childbirths in Indigenous and rural areas are often assisted by midwifes while in urban scenarios childbirths are supported by the public health service. Such precarious conditions in Indigenous and rural areas represent a direct threat to life. This situation highlights a national social problem15 and a public health problem16.
It’s apparent that there is a serious public health problem, such that the health problems of the neediest population can hardly be addressed when there is no corresponding medical coverage. The paradox of the problem is that Mexico celebrated the bicentennial of the War of Independence (1810) and the centennial of the Mexican Revolution (1910). These were armed movements involving a marginalized rural and Indigenous social base that struggled for fundamental rights. However, as this study shows, given the knowledge that there is severe social deprivation among millions of Mexicans, without the universal right to health services after 200 years, the celebrations are pointless, at least for Indigenous and rural populations.
Conclusions
Significant differences between the three population areas – Indigenous, rural and urban – in relation to the degree of marginalization and access to health services were found. The present study confirms that the localities and inhabitants in the Indigenous area are the most marginalized and most deprived of health services and that urban areas are the least affected in this respect. Governmental policies aimed to overcome the lack of access to health service coverage should pay attention to rural populations with special emphasis on Indigenous areas.