Introduction
Diabetes mellitus (DM) is a growing health concern worldwide, and a disproportionate increase in prevalence is expected to occur in India within the next two decades, from 62 million currently − a fifth of the world’s diabetic population − to 80 million by 2030.1-3 People with DM have high risk of developing diabetic retinopathy (DR), and the risk is increased when DM is associated with hypertension.4-6 Preventive care through regular eye examinations and proper management of DM and hypertension can reduce the risk of vision loss from DR, though knowledge of these conditions is low in the Indian population.4,5,7,8 Previous studies have reported that only about 50% of a rural South Indian population had knowledge of DM and one-third had knowledge of DR.8 The Andhra Pradesh Eye Disease Study reported that only one-quarter of the urban population of Hyderabad was aware of DR.5,9
Previous knowledge, attitude, and practices (KAP) studies have been conducted in either rural or urban populations and were focused on DM and/or DR.6-8,10-12 There is paucity of KAP information on hypertension, which is a comorbidity risk factor for DR.9 Additionally, there are no comparative KAP studies of DM and DR across levels of a pyramidal model of eye care delivery from a village to a metropolis. The L V Prasad Eye Institute (LVPEI) works on a comprehensive integrated pyramidal model of community-based Primary and Secondary eye care in underserved rural areas linked to urban Tertiary-level care in four states of India. Diabetes and hypertension screening are integrated into the LVPEI eye care model as part of comprehensive care for patients with DM and hypertension, and their related eye complications.13
This study aimed to examine and compare the KAP on DM, hypertension and DR across Tertiary (T), Secondary (S) and Primary (P) levels of the LVPEI eye health pyramid. Additionally, the study surveyed motivating factors for DM and DR screening and sources of knowledge about these conditions and eye care services. Identifying facilitators of good KAP at each level of an eye health pyramid could help design programs to increase utilization of eye care facilities and of DM and hypertension screening services.
Methods
Study design
The study locations were two fixed and one mobile (community) location in India. The fixed locations were a Tertiary facility in Hyderabad and a Secondary facility in Karamchedu, Prakasam District, Andhra Pradesh (300 km from Hyderabad). The mobile (Primary) location was selected in Prakasam District, where community DR screening programs were held. In the LVPEI model, the Primary level serves a cluster of villages with a target population of 50 000, and it is part of a network connected to a Secondary facility that serves 500 000. Patients diagnosed with eye problems at the Primary level were referred to the Secondary facility for follow-up, where services include diagnosis of all conditions, surgeries and rehabilitation. These are linked to urban Tertiary facilities that provide a comprehensive range of services, care for complex conditions and training. All participants from the study locations of age 40 years or above who consented to participate were included in the study. Eligible participants were selected randomly on each day of the study until adequate participants, 202 in total, and approximately equal numbers of diabetics and non-diabetics, were surveyed in each location. People who had difficulty in understanding the questionnaire or declined to participate were excluded. All participants were administered a validated pilot-tested questionnaire (Appendix 1) by a trained field team in the regional language. Most questions were adapted from previous KAP studies.6-8,10
Data analysis
Chi-square tests were conducted to compare demographic and systemic factors between the three locations. Knowledge and attitude were scored based on percentage of correct answers out of 16 questions (Appendix I: questions 18–23, 25–29, 31–35) weighted equally, with correct answers scored as 1 and incorrect answers as 0. Unpaired heteroscedastic t-tests were performed to compare mean knowledge and attitude scores and practice patterns between groups divided by location and diabetic status, and t-test and one-way ANOVA were used to compare scores with practice patterns. Multivariate linear regression was performed on the mean scores to identify possible predictors among the demographic and systemic factors in each location. Significance was assumed at p<0.05 for all tests.
Ethics approval
The study was conducted after approval from the Ethics Committee of LVPEI (Ethics Ref No. LEC -07-14-067).
Results
Characteristics of study population
Demographic factors and systemic conditions of the survey participants are shown in Table 1 with respect to facility level and in Table 2 with respect to diabetic status. In total, 202 participants were surveyed, with gender participation similar at all study locations. Participants at the Tertiary facility tended to be younger, highly educated, of higher socioeconomic status, had a higher prevalence and longer duration of hypertension, and had longer duration of DM compared with participants at the Secondary and Primary levels. Participants with DM tended to be more highly educated and have a longer duration of hypertension.
Table 1: Demographic and systemic factors of participants at Primary, Secondary and Tertiary eye care facilities in Hyderabad, India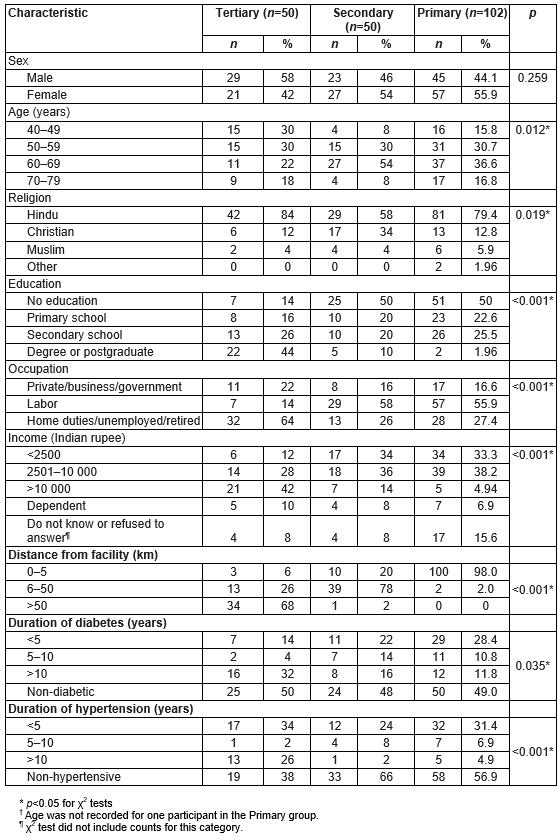
Table 2: Demographic and systemic factors of diabetic and non-diabetic participants recruited from eye care facilities in Hyderabad, India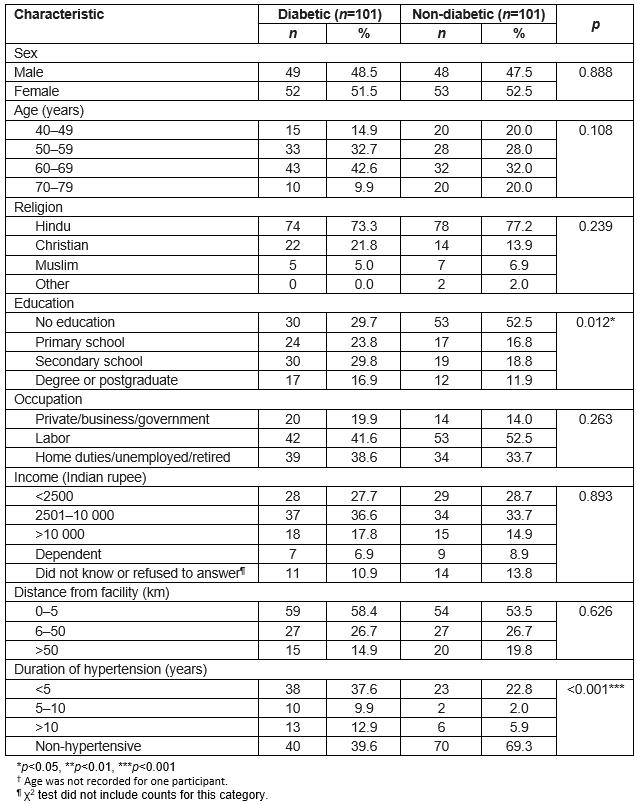
Knowledge and attitude of DM, hypertension and related eye complications
The mean percentage of 16 knowledge and attitude questions related to DM and DR that were answered correctly is shown in Figure 1 for diabetic and non-diabetic participants at each facility and in Figure 2 for hypertensive and non-hypertensive participants at each facility. People with DM had a higher mean knowledge score (67.3% Tertiary, 59.4% Secondary, 47.0% Primary) than non-diabetic participants (41.8% Tertiary, 29.0% Secondary, 23.5% Primary; p<0.001 for all locations). Among people with DM, mean score was higher at the Tertiary and Secondary-level facilities than the Primary level (p<0.001, p=0.035), and among non-diabetics, mean score was higher at the Tertiary-level facility than the Primary level (p=0.003). Mean score was significantly higher for hypertensive than non-hypertensive participants at the Tertiary facility only (p=0.038). Among participants with hypertension, mean score was higher at the Tertiary-level facility than the Primary level (p<0.001).
Although the majority of participants in each location were aware of hypertension (84.0% Tertiary, 65.3% Secondary, 52.9% Primary), less than a third knew that hypertension could affect the eyes (30.0% Tertiary, 12.2% Secondary, 13.7% Primary) or be associated with diabetic complications (30.0% Tertiary, 32.7% Secondary, 21.8% Primary). Awareness of DR was higher among people with DM (65.3%) compared with 22.0% among non-diabetics at all locations. Among the non-diabetics not aware of DR, one-third had never been tested for DM, and half of them knew nothing about DM.
Multivariate linear regression analysis of influencing factors on KAP across all three facilities showed that education through secondary school in all locations was associated with significantly higher scores (Tertiary p=0.035, Secondary p=0.034, Primary p=0.011), as with post-secondary education at the Tertiary location (p=0.003). Diabetic status was associated with higher scores at the Secondary-level facility (p=0.006) and Primary level (p=0.010).
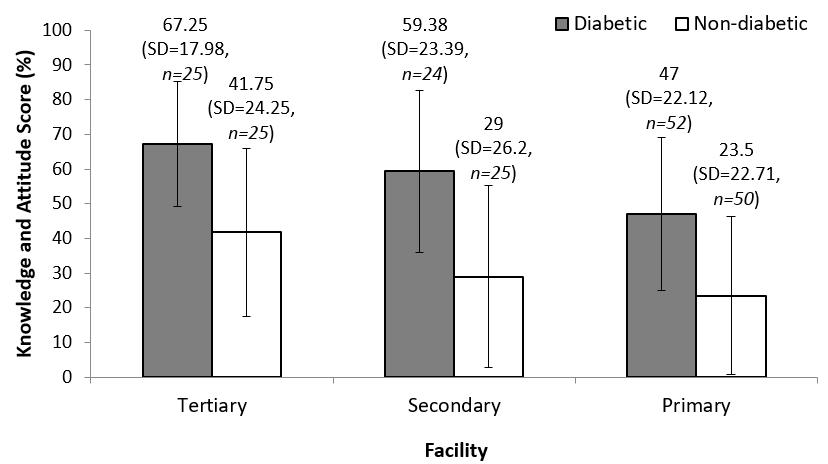 Figure 1: Mean knowledge and attitude score of diabetic and non-diabetic participants at each eye care facility in Hyderabad, India. Mean score, standard deviation and number of participants are noted above corresponding bars.
Figure 1: Mean knowledge and attitude score of diabetic and non-diabetic participants at each eye care facility in Hyderabad, India. Mean score, standard deviation and number of participants are noted above corresponding bars.
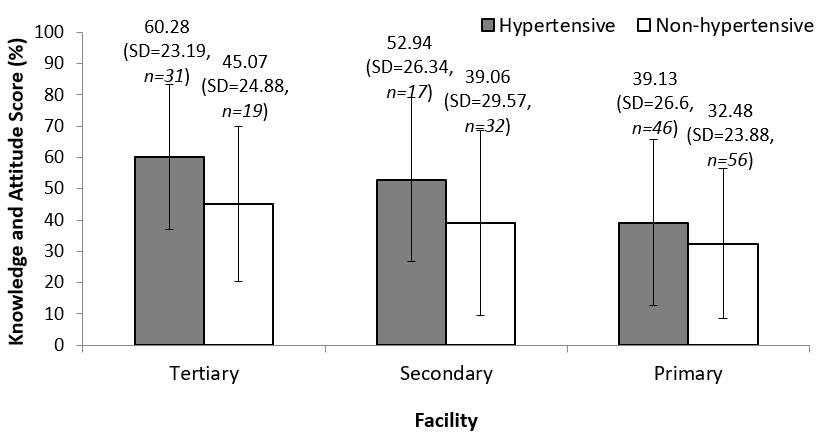 Figure 2: Mean knowledge and attitude score of hypertensive and non-hypertensive participants at each eye care facility in Hyderabad, India. Mean score, standard deviation and number of participants are noted above corresponding bars.
Figure 2: Mean knowledge and attitude score of hypertensive and non-hypertensive participants at each eye care facility in Hyderabad, India. Mean score, standard deviation and number of participants are noted above corresponding bars.
Practice behaviors
The fraction of participants who had ever been tested for diabetes was highest at the Tertiary-level facility (94.0%), followed by the Secondary-level facility (89.8%) and Primary-level facility (77.5%), (p=0.015). The most common method of diabetes control was the combination of medicine, diet and exercise, practiced by 60.0% of participants at the Tertiary-level facility, 45.8% at the Secondary-level facility, and 28.8% in the Primary-level facility. Many diabetic participants in the Primary-level facility reported that they exercised daily through their labor-intensive occupations.
Responses for duration since the last general physician checkup, eye checkup and dilated eye examination for participants in each location are presented in Figure 3. Difference between locations for duration since last visit to a general physician was not significant. Duration since last eye checkup and last dilated eye exam were significantly different between locations, tending to be shortest at the Tertiary-level facility and longest at Primary-level facility. Within each location, differences were examined between diabetic and non-diabetic participants, and significant differences were noted only at the Primary-level facility for duration since last visit to a general doctor (p=0.003) and to an eye doctor (p=0.042), Participants who never had a dilated eye examination previously were 2% at the Tertiary-level facility, 40% at the Secondary-level facility and 50% at Primary-level facility.
Association of knowledge and attitude score with practices is detailed in Table 3. Non-diabetic participants who had previously been tested for diabetes had a significantly higher mean score. Mean score tended to be higher and was significantly different between practice responses for participants who had more recently visited an eye doctor (diabetics p=0.0084, non-diabetics p=0.0173) or had a dilated eye exam (p<0.001 for diabetics and non-diabetics).
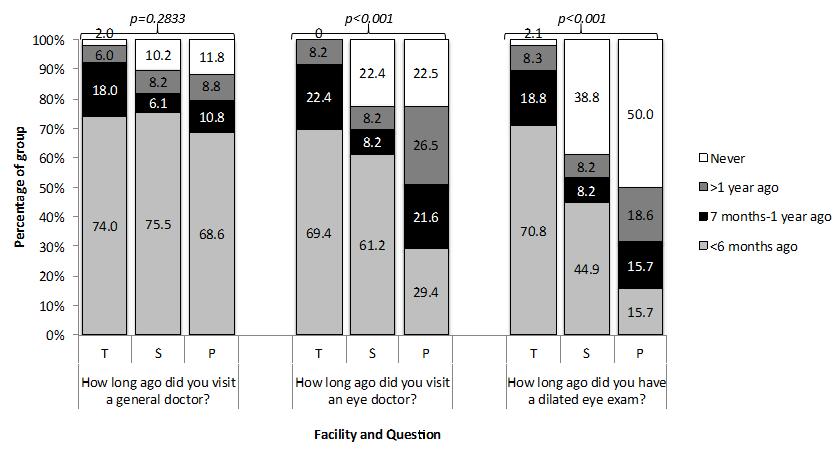 Figure 3: Practice patterns based on eye care location (T=Tertiary, S=Secondary, P=Primary) in Hyderabad, India. Significant p-values (p<0.05) for χ2 tests are marked with an asterisk.
Figure 3: Practice patterns based on eye care location (T=Tertiary, S=Secondary, P=Primary) in Hyderabad, India. Significant p-values (p<0.05) for χ2 tests are marked with an asterisk.
Table 3: Association of knowledge and attitude score and practices for diabetes mellitus, hypertension and diabetic retinopathy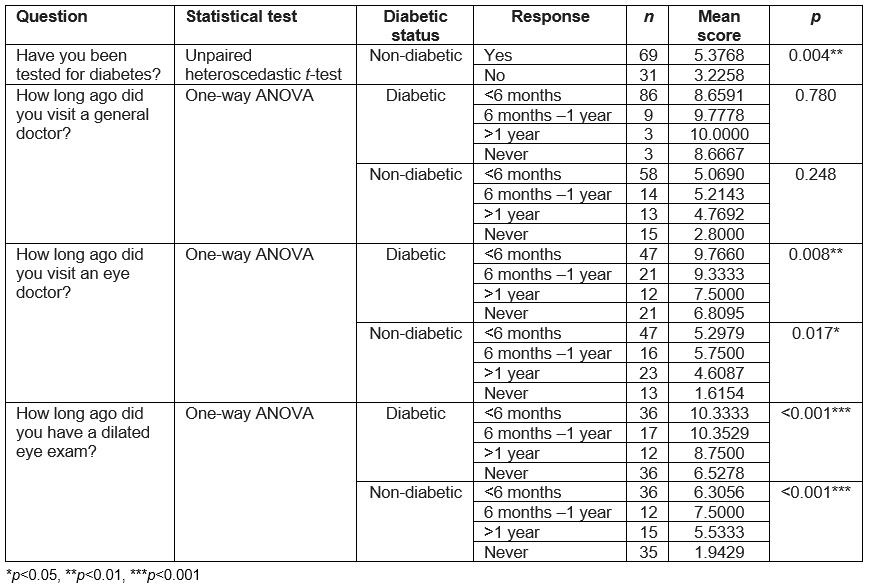
Motivating factors and sources of knowledge
Table 4 summarizes motivating factors for eye and diabetes screening and sources of knowledge about eye care facilities, DR and dilated eye examinations among participants at each level of the LVPEI eye care pyramid. Participants at Primary screening were motivated to visit the facility for a routine checkup (70.6%), poor vision (22.6%), or a glucose or blood pressure test (17.7%), while the main motivators at the other facilities were follow-up or poor vision (28% and 42% Tertiary, 50% and 30% Secondary level). A free eye checkup was the motivating factor for some who mentioned routine checkup at the Primary level. A new eye problem was the main motivator for most recent past visit in all locations (40.8% Tertiary, 46.9% Secondary, 48.5% Primary), but 22.4% of participants in the Secondary-level facility and 22.8% at Primary-level facility had never visited an ophthalmologist previously. The main reason for getting tested for diabetes was a routine preventive health check at the Tertiary-level facility (38.8%), general physician suggestion at the Secondary-level facility (40.8%) and experiencing symptoms of vision reduction at Primary-level facility (50.0%).
Most participants at the Tertiary-level urban facility had learned of the facility through a general physician or ophthalmologists (34%) or family/friends (32%); family/friends were the most common knowledge source at the Secondary-level rural facility (60%), and an announcement of the village screening program was the main knowledge source at the Primary level (72.5%). While ophthalmologists and family/friends were the most common sources of knowledge about DR and dilated eye examinations, the media and general physicians were not common.
Table 4: Motivating factors and sources of knowledge based on location (Primary, Secondary and Tertiary eye care facilities in Hyderabad, India)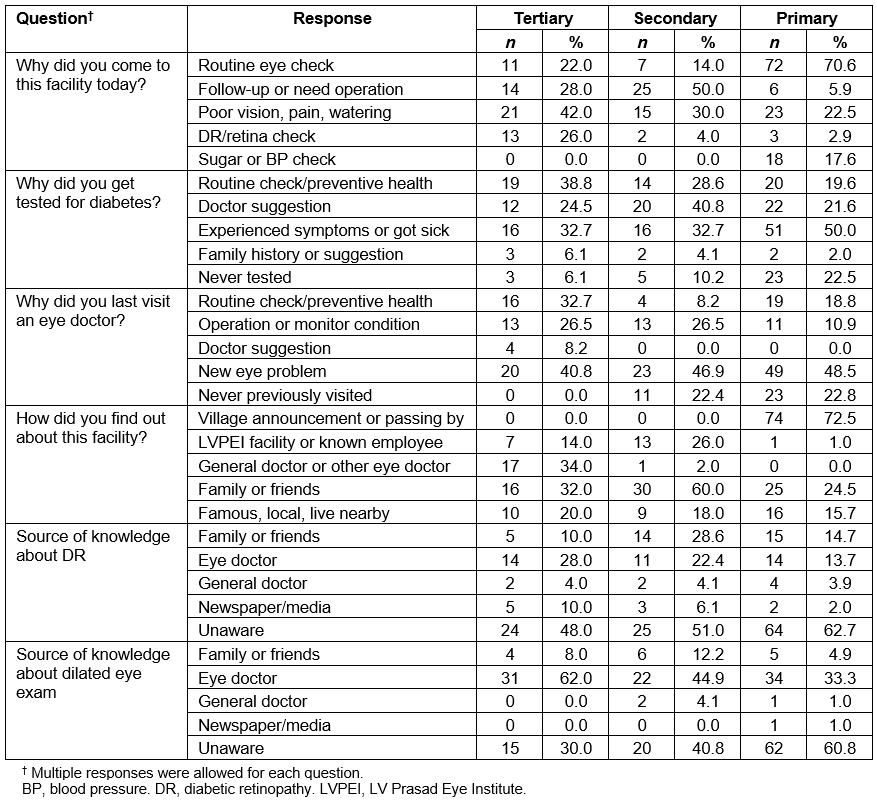
Discussion
The unique features of the present study include a comparison of KAP at different levels of eye care delivery, examining the socioeconomic factors, health conditions and motivational factors in the same cohort, and collecting the KAP of DR along with both DM and hypertension. A KAP study in different levels of care – Tertiary, Secondary and Primary – is key information for modifying healthcare delivery and resource management as appropriate for each location.
Education was the only demographic factor with significant influence on knowledge and attitude. This was noted in all non-diabetics in an earlier study in a neighboring rural district (Guntur, Andhra Pradesh), and age and use of spectacles were additional significant factors among diabetics.6 In the present study, diabetic status was tested as an associated factor and found to significantly influence positive knowledge and attitude. Gender, religion and income were the significant factors in the neighboring Tamil Nadu state rural population study, but they were not significant in two Andhra Pradesh studies (the present and earlier published study).6,8 In a study by Dole et al, female participants had accessed eye care services and free cataract surgery more at a Primary eye care facility than Secondary or Tertiary eye care facilities. However, in the present study, gender did not play a significant role in utilization/KAP scores at any level.14 Education has been found to be a common indicator of knowledge in studies in other countries too, such as Gambia and Mongolia.6,8,11,12 It is important to promote basic education at least through secondary school as part of health promotion efforts, as shown in the present and previous studies.
In comparing demographic characteristics based on diabetic status, the finding that education level was higher among diabetic participants raises the concern that there may be many more participants in the ‘non-diabetic’ group who have undiagnosed DM, because those who were more highly educated may have been more likely to know to get tested for DM. It makes sense that diabetic participants had a longer duration of hypertension since it is a common comorbidity. The distributions of duration of DM and hypertension at each facility directly depend on the frequency of health screening. This cannot accurately reflect on the health condition of patients using each facility because patients visiting the Tertiary urban facility may have been screened earlier or more frequently than patients in the other facilities.
The difference in knowledge and attitude was more pronounced between diabetics and non-diabetics at each location than between locations. This was expected since many questions specific to DM, hypertension or DR may not be relevant for people without DM. Ideally, diabetics should know the correct answers to all except two questions (Appendix I: question 26 related to hypertension and question 31 related to DR treatment) and the mean ideal score should be 87.5%. Unfortunately, the mean knowledge score of diabetics was 55.0% across locations, which was less than ideal. Similarly, the non-diabetics should know the correct answers to six questions (Appendix I: questions 18, 19, 21, 23 related to DM, hypertension and DR, questions 29 and 35 related to dilated eye examination), and the ideal score should be 37.5%, but the mean knowledge score of non-diabetics was 29.4% across locations, which was also less than ideal. This calls for the need to improve education among the entire population in Secondary and Primary-level facilities and at least the non-diabetic population at the Tertiary-level facility. The low score even for participants with hypertension at the Primary level (mean 39.13%), presses the need to educate the community of hypertensive patients, especially in rural areas, about their risks of DM and DR.
In the present study, 31% of non-diabetics and 74% of diabetics knew that DM could affect vision. This was better than the situation in Mongolia (36.9% of all participants) and Gambia (67.0% of diabetics), but less than the Australian population (78.5% of non-diabetics and 96.2% of diabetics).10-12 Lack of awareness about DR and risks of hypertension was prevalent in both urban and rural locations. Awareness of DR in the present study was comparable to an awareness level of 27% of the general Hyderabad population and greater than in the neighboring rural district, where a third of diabetics and a tenth of non-diabetics had heard of it.6,9 Education programs for populations of interest at the Tertiary urban and Secondary rural facilities should be practice-oriented, since association of knowledge and attitude to practices was not significant. Knowledge and attitude influenced practices in the Primary-level facility; hence, both general eye and health information and good practices are important to include in education programs at this level.
The present study showed that a large segment of the rural population has never had a dilated eye examination: 50% in the Primary level and 40% in Secondary-level rural facilities. Moreover, most participants at Primary-level screening who had had a dilated eye exam had their latest one more than 6 months prior, longer on average than at the other locations. Increased use of fundus cameras will greatly facilitate eye examination. The proportions of diabetics in our Secondary and Primary-level locations having received a dilated eye examination at least once in their lifetime and once in the past year in this study were greater than in the neighboring rural district in an earlier study (62.5% and 54.1% rural and 50% and 34.7% community versus 41.8% and 28.4% in the earlier study respectively).6 The proportion of diabetics in our Tertiary-level facility having received a dilated eye examination at least once in their lifetime was similar to the pattern among Australians and greater than among African Americans (96% versus 100% of Australian diabetics and 76% of African American diabetics).6,10
Better advocacy has to match with the motivating factors, the travelling distance and the facilities. Although the majority of participants at community screening had come for a routine checkup on the day surveyed, that fraction is much lower for previous visits and about a quarter had never previously visited an eye doctor, yet it seems they would have if they had better access earlier, since they were motivated to come for a routine checkup on the day they were surveyed. Glucose and blood pressure screening was a main motivator for 17.7% of Primary-level facility screening attendees, indicating the value of combining these tests with eye screening. General physicians are a source of health knowledge promotion in all locations that can be better utilized as previously recommended in the case of diabetes education in India.2,3
Limitations
The authors’ observations are only from participants who visited the eye care facilities. It is unknown how much of the population in the areas of interest did not visit eye care facilities and whether they were aware of the necessity of an eye examination. Their KAP might be worse than those participants with knowledge or motivation enough to seek eye care. The present study participants may not be representative of the entire population at each level. Thus, these KAP results cannot be generalized. Another limitation is that information about systemic health conditions and practices were self-reported. Participants were advised to report uncertainty if they were unsure of any answer, but some participants might have guessed correct answers. Despite these limitations, the strength of the study was in identifying motivating factors and knowledge sources of people who visit eye care facilities, in the hope that they could be used to promote utilization of services to a wider population.
Conclusion
In a country with fast growing epidemics of DM, hypertension and DR, and with great disparities and inadequacies of healthcare resources, it is critical to reduce risk of these conditions through increased awareness and screening and to investigate the best way to do so for diverse populations through studies such as this. The present study revealed distinctions between Primary, Secondary and Tertiary eye care centers in: socioeconomic and health characteristics; eye care and general health knowledge, attitudes and practices; motivators for health screening; and sources of knowledge about eye care and conditions. The findings call for tailored education programs, methods of advocacy and advertising of eye and healthcare facilities for the relevant populations at each level of a pyramidal model of eye health care.
Appendix I: Knowledge, attitude and practice questionnaire administered to study participants