Introduction
When a patient is critically ill or injured in a small rural community in British Columbia (BC), Canada, an emergency number is called and the ambulance dispatched will, in most cases, transport the patient to the nearest local hospital emergency department (ED). This is consistent with other rural jurisdictions internationally. Small rural hospitals are typically not resourced to manage high-acuity cases beyond initial stabilization; therefore, when these cases require specialist involvement, patients must be transported to a larger hospital for definitive care. When the need for transport is urgent and the patient requires interventions en route, a healthcare provider escort is required. This is often a nurse or even a physician from the small hospital as rural ambulance attendants often do not have the necessary skill set to manage high-acuity situations that may necessitate en route interventions. Removal of a nurse or physician from a rural community immediately compromises the limited care provider resources, thereby destabilizing local care. This challenge of transporting a high-acuity rural patient to definitive care is one faced by every health region with significant rurality and plays out against the competing priorities of excellent patient care and cost containment1-5.
A small number of studies from Canada, the USA and other international jurisdictions have examined rural high-acuity transport models, including challenges and best practices. They have found that high-acuity transport models need to be flexible while adapting rapidly to diverse emergent medical situations that may or may not require advanced life support. Key obstacles in rural contexts are difficult geography, long travel distances and weather conditions1,4-6. In Canada, these obstacles lead to clear discrepancies in emergency medical system (EMS) care between rural and urban residents7. In some jurisdictions in Australia, the length of time preceding arrival to a hospital was found to be a significant predictor of death6. Rural sites, however, typically do not have the volume of critical care cases that would necessitate specialist critical care staff and even if a critical care specialist was stationed in a low-volume setting, they may not see enough volume to keep their skills relevant.
Critical injuries are often sustained at great distances from trauma care centres, meaning that many patients must be stabilized on the way to a local outlying hospital as well as during transfer to a tertiary care centre1,5. This reality expresses two integral considerations for effective critical care: first responders who have a long distance to travel to hospital need to be capable of delivering critical care stabilization5, and interfacility patient transport mechanisms need staff and vehicles that can transport a patient in critical condition. EMSs in many jurisdictions are typically challenged with this variation in patient acuity and must strive to create staffing and dispatch models that can deploy an appropriate level of service within their geographical context. A successful model is Scandinavia’s pre-hospital EMS teams that include physicians who are specially trained to perform necessary and advanced procedures during transport trips that can take as long as 425 minutes4. Scandinavia’s EMS system is flexible, remaining paramedic-based, with the physician team available for deployment depending on case needs. Key to good outcomes in a system that contains different modes of service is collaboration between agencies and having a highly coordinated system, including effective interfacility transport1.
The High Acuity Response Team background
Like other jurisdictions in Canada and Australia, patient transport is primarily centrally organized by the province and then regionally by the health authority. In rural BC, Provincial Emergency Health Services (BCEMS) owns and operates air and ground ambulance services primarily staffed by paramedics trained in basic life support (BLS) and a transport network responsible for coordinating all interfacility transport. In 2009, the Interior Health (IH) authority of BC recognized a gap in services where rural nurses and physicians, often the only ones available to a community, were being removed to transport a patient with critical care needs to a higher-resourced hospital. The High Acuity Response Team (HART) was proposed as a much-needed missing piece from the puzzle of comprehensive emergency services.
HART’s main goal is to keep rural nurses and physicians in their communities rather than having them leave to transport a patient. The HART team is deployed to attend to acute-care patients at rural/remote sites and works to either stabilize the patient so they may remain in their community or transfer them to more a complex care facility when necessary. Interfacility transport is carried out in partnership with existing provincial emergency services who coordinate teams and dispatch vehicles to transport the HART team to a patient and then on to more definitive care. The HART team is made up of one dedicated staff role, a critical care registered nurse (CCRN) who has specialty training and equipment, and is staffed 24/7 at each of four regional referral centres dispersed across IH. In addition to specially trained CCRNs staffing the HART team, specialized registered respiratory therapists (RRTs) are on call to the program and involved in patient transport when needed. When the HART CCRN is not called to transport, they are expected to integrate into their base hospital (regional referral centre) by fulfilling a supernumerary clinical support role in the emergency department (ED) and intensive care unit (ICU) under the direction of the hospital’s operation manager or site supervisor.
This article presents the qualitative findings from a program evaluation of the efficacy of the HART model, focused primarily on key stakeholder experiences and suggestions for improving rural high-acuity patient transport. The study highlights the challenges in interfacility transport for acute conditions in rural settings.
Method
The current study is a part of a larger program evaluation designed to gain an in-depth understanding of the HART program. The current study used qualitative inquiry to understand and document the experiences of the key stakeholders in the HART program through unstructured interviews. An open-ended approach was used for the interviews to allow maximum opportunity for unanticipated influences of the HART program to be expressed.
HART has four base sites (Trail, Kamloops, Cranbrook, and Penticton) from which CCRNs and RRTs are deployed and at which CCRNs fulfill their supernumerary role of clinical support. The main administrative site for the IH authority is in Kelowna and functions to coordinate all care for the region. In addition to the base sites and administrative site, HART also interacts/functions with peripheral rural hospital sites across south eastern BC. All four base sites and the administrative site were approached to participate in the evaluation and 16 peripheral sites were selected to represent diversity in base affiliation, distance to base hospital, and community size/local resources.
The study had three objectives: to determine if the HART program has (1) contributed to a change in practice at either the base sites or the peripheral sites; (2) contributed to the sustainability of health human resources in the peripheral sites, or (3) faced any challenges integrating into existing (provincial) patient transport mechanisms.
Research participants in base sites included HART team members (CCRNs and RRTs) and administrative leads for the HART base hospitals. Research participants in the peripheral sites included local hospital administrators, local physicians who participate in ED calls, and ED nurses. Research participants in the central administrative site included those involved in supporting HART at an administrative level. Participants were identified through key contacts within the HART program and a letter of invitation was sent to each. Postcard reminders and follow-up phone calls were used to achieve a high participation rate (n=107). Two interviews with provincial key informants were completed by teleconference; otherwise, interviews were held at a location convenient to the participant (usually their clinical offices) and lasted on average one hour.
Thematic analysis guided the approach to making sense of the data, chosen for its applicability to policy work for audiences outside of academia8. Analysis was done by following the basic principles of thematic analysis8-10, starting with immersion in the transcripts (an initial reading to make note of predominant themes). As one of the two lead academic investigators was involved in all of the interviews, this step also involved matching interview field notes to transcript data. Transcripts were re-read (line-by-line) for a micro-analysis of the data and further differentiation between themes emerged within each interview topic. Similar topics were then organized into larger themes and data were organized by these themes. At this point, codebooks were created independently by the two reviewers, compared, and found to have a high degree of congruence. Further work refining and defining each theme was done in collaboration before the research coordinator completed coding of all the transcripts.
Findings were interpreted from both a clinical and an academic perspective as per the transdisciplinary composition of the research team. Consistency of findings was verified in relation to current literature on the topic. (The principal investigator has conducted a realist policy review on best practices for patient transport, and findings from this review were used to triangulate data11.) The draft findings were presented through two presentations with the full team (representing Health Authority administrators and clinicians) for feedback on verisimilitude. Verisimilitude was found to be high.
Ethics approval
Ethics approval was obtained from UBC’s Behavioral Research Ethics Board (UBC BREB H14-01663) and harmonized with the health authority ethical approval process. The interviews were audio-recorded with the participants’ permission for transcription purposes.
Results
A total of 107 interviews in 21 study sites were undertaken with HART team members, administrators and care providers in the referral and regional hospitals between September 2014 and March 2015. A demographic table listing the role of each participant is depicted in Table 1. Participants expressed overall satisfaction with the HART program in meeting the high-acuity transport needs of rural communities. Within this context, specific attributes, challenges and recommendations were described, each of which are explained below.
Table 1: Number of participants reported in each role category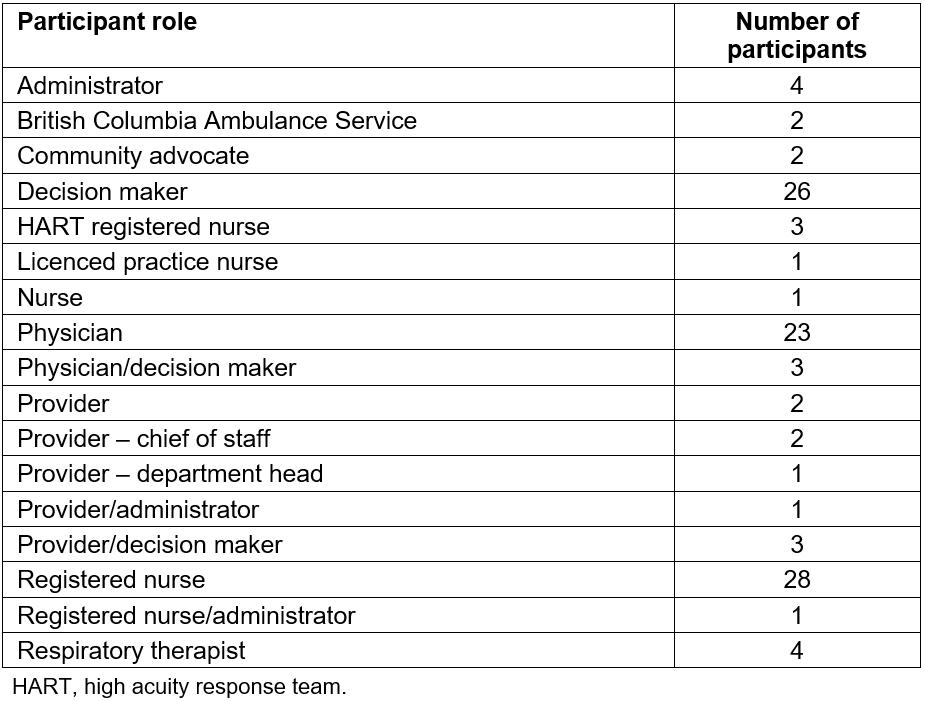
HART’s health human resource model
The HART team itself rests on the collaboration of the HART CCRNs and RRTs, which was deemed to be an effective human resource model, improving on the previous BLS paramedic model for rural services. Several participants pointed out that the former model was fraught with conflicting institutional roles whereas CCRNs and RRTs were both familiar entities in the hospital setting. Further, their respective roles were defined well enough to reduce friction. As one participant noted:
I think it is a combination of the individuals – the HART nurses are committed to the program and so are the RRTs. As far as the challenges go on either side, they haven’t been involved in the interpersonal things. We respect them – they respect us. It is a smaller site, we work closely together. It is collegial, supportive and respectful. (Respiratory therapist)
Almost all participants in the rural sites commented favorably on the role HART had in stabilizing their health human resources in times of high acuity, reflecting the achievement of a key program objective. Participants from all roles noted that the HART team brought integrated critical thinking to each facility. That is, they were seen to have the ED skills needed to stabilize patients along with the ICU skills for ongoing management.
HART’s primary role: interfacility transport
The team’s role in interfacility transport was frequently valued by the rural sites, as it reduced the number of interfacility transfer escorts required by the rural physicians and nurses. As one participant noted:
[HART] is great. For your STEMI [ST-elevation myocardial infarction], it is lovely. STEMIs are otherwise a pain, because you feel that you have to go with them, it is not fair to just put them in an ambulance with the basic ambulance crew and it is really not fair to stick a nurse in there, because their rhythms look horrible and that is scary. So you stick the physician in there, not to do anything – to deliberately not do anything. For patients like STEMIs, [HART] is great, it makes everything better. (Physician)
HART team members themselves recognized their value at the rural facility:
I think we provided an excellent service. I think one of the defining characteristics is seeing the relief on the faces of the nurses when you walk in the door with your stretcher full of gear and your capacity to take that person away. That [is] very satisfying. (HART team member)
Waiting to be deployed: supernumerary clinical support
The most significant advantage of the HART team seen by base-hospital respondents was a result of the supernumerary role of the CCRNs: they were an extra pair of hands. The pairing of CCRNs with RRTs was seen as a significant advantage that led to better care and better outcomes. Several participants noted a reduction in codes called on the floors:
[Codes are] extremely rare now because whenever there is a patient that might be crashing, our nurses know to call the HART RRT or CCRN to come and take a look. When the HART CCRN or RRT comes to the ICU … they are immediately listened to because the level of respect is there and the patient is moved to an appropriate place, before they crash. That is because of the HART nurse integration. They are getting all kinds of great work out of them in the hospital. (Physician)
The advantages were seen primarily as having the ‘critical care eye’ available to respond to deteriorating patients. For physicians, the HART team often enabled smooth running of the rest of the ED, where the physician is free to be a resource to other patients. (‘I will leave it in their hands if it is possible and see my other patients.’) One participant recognized it as ‘the domino effect’ of a patient needing acute care in a low-resource environment sometimes leading to dwindling health for pre-acute patients, who may not get time with the physician. Indeed, most sites praised HART’s role in rounding on patients recently discharged from ICU and participating in the rapid response team calls (eg in-hospital cardiac arrest). The involvement in the pre-acute phase was seen as key in reducing the number of acute cases. As one participant said:
In any hospital, you always have problems not with patients that have become critical and need to go to the ICU, but patients who are kind of circling the drain and actually haven’t started to go down it yet, if you know what I mean. (Physician)
The HART CCRNs themselves strive for balance between responding to the demands of calls out to the peripheral sites and responding to the demands of the base sites. The study heard from participants that this requires mindful attention to the dual nature of their roles: contributing to (sometimes) acute situations on site with the recognition that they must be ready to be deployed at a moment’s notice (most said they must – and can – be ready to leave within 5 minutes of a call coming in).
Challenges to the CCRN and RRT staffing model
Although many saw the CCRN–RRT dyad as an efficacious staffing model, it also gave rise to challenges due to the different way these roles are staffed within HART. Where the CCRNs are dedicated to HART, the RRTs are not; they are considered on call to HART and otherwise considered a non-supernumerary to the hospital site. Having an RRT go out on a transport call, which may last up to 9 hours, sometimes left the base site without RRT coverage. Some of the RRTs noted that coverage then relied on the good graces of other RRTs – and the transport RRT’s ability to reach them on their time off. This was part of a larger discussion at some sites regarding a supernumerary RRT, in the model of the CCRNs, to reduce the need for call-in and back-fill capacity at the base site. Due in part to this, and other conditions of practice, RRTs at a few of the sites expressed feeling undervalued in their role, with their educational leadership and skill contribution valued only in times of high acuity.
Likewise, although the HART CCRNs were recognized as ‘value added’ for the base hospital, several participants expressed the desire for a more clearly defined role for the CCRNs when they were not on a transport call to create clearer expectations for their contribution. Some participants identified a fundamental misunderstanding about HART’s role and capacity to take on assignments due to the possibility of quick deployment and noted that this led, in some instances, to the perception that they resisted contributing. In defence, one HART nurse observed the differences in the nature of their role:
The frustrating parts come down to feeling like a unit in particular is using you as workload or break-relief; not taking into account the fact that 8 hours into your shift, you may get called out to do another 12 hour transfer – long after they have gone home, we are still on the clock. (HART nurse)
Administrators, who were recognized as providing oversight on the issue, identified the challenges they faced in keeping the nurses busy (‘We certainly don’t want them sitting around, waiting for the phone to ring.’) and recognizing the unpredictability of their shifts (‘But at the same time, we can’t consume them with activities they cannot be taken away from.’).
Inter-organizational functioning
HART services are deployed in partnership with provincial ambulance services who provide and dispatch ground and air vehicles for HART calls as well as receiving and coordinating all requests in the province for patient transport.
Inter-organizational functioning within the partnership was largely viewed as a challenge, irritating to many participants at a systems level: when translated to a patient care level, however, it was devastating. There were patient stories from almost every site that vividly expressed the implications of the delays on patient safety and outcomes, and on care providers. Thematic to these vignettes was the urgency of the clinical situation (potentially life or death), the expressed vulnerability of the attending care provider(s), the unrealistic communicative expectations to arrange transport (at the cost of patient care in situations where there was limited or no back-up) and the anguish of the wait time. In these instances, an ultimate good outcome did not mitigate against the lasting trauma of the situation for most involved.
Not all delays in deployment were attributed to dispatch issues, however. Some participants pointed out that sometimes the wait time was simply due to over-demand on the HART team.
Requests for patient transport
A particular challenge related to deployment – communication with the provincial service responsible for receiving and initiating requests for patient transport – was expressed by nearly all of the participants in this study. Specifically, the experience of inefficiencies and redundancies in the communication were described:
[E]ven though it is a LLTO [life, limb or threatened organ], they take the patient’s name – get all the information and ask how are things going. Usually, they want to talk to the doctor right away. What happens in that situation, there is only one doctor – they don’t have the time to sit on the phone and talk. (Nurse)
Deployment of vehicles
The HART team’s reliance on the provincial ground ambulance service was recognized by many as a significant barrier to efficient transport, aggravated by the lack of control the team had on vehicle deployment. Several participants suggested the need for alternative transportation to the site. (‘We want the HART nurse and the RRT to come – we don’t necessarily need their ambulance – we have ambulances’) Some participants discussed ways in which individual sites attempted to address this through alternative transport, primarily through taxi transport. This was particularly relevant when the team was requested for site support as opposed to patient transport, the former considered to be out of scope for provincial ambulance services. Taxis, however, were reported by many to be unreliable:
I was asked to send the HART nurse there for site support, which I did arrange to do, she didn’t really end up there, because the taxi I sent her in broke down halfway between here and [there]. (Decision maker)
Many participants recognized the delay in transport vehicle as the result of the practice of using the on-call paramedic staff for a HART-commissioned vehicle. For the provincial ambulance service, this ensured availability of immediately available, first-call ambulances to respond efficiently to emergency calls from the public. For the HART team, usage of on-call paramedics often meant at least a 20-30 minute delay. Ground-up efforts to address deployment challenges were described, such as the HART team providing the rural sites with their personal cell phone numbers in case they hadn’t been notified about a call-out where they were needed:
Now when we launch them, we will phone their cell phones and let us know that they have or have not been dispatched. If they don’t hear within half an hour, they would call back and ask to be dispatched. (Administrator)
The delays led to some participants in the rural sites saying that if a patient was severely unstable, they would not wait for HART and would transport with an escort by local ambulance. This was articulated most clearly in sites that had experienced adverse outcomes due to transport delays. The delays were difficult as well for the HART team waiting to be deployed. As one team member noted: ‘you feel helpless – you know that there is a patient that needs help and you just cannot get there’.
Several participants related stories of air ambulance transfers being cancelled due to inclement weather but HART not being notified to take over the transfer, thus not being able to dispatch. These participants suggested that HART be dispatched (via ground ambulance) when air ambulance is dispatched. This would mitigate frequent air transport cancellations, with cancellation of the HART team en route being preferable to re-dispatch once air ambulance is cancelled. ‘Triage error’ or redundancy was accepted by most participants as a necessary by-product of good care. It was further suggested that contributing to the care of the acute patient in the rural site until air ambulance arrives frees up the local care providers to continue care in the ED.
Participant recommendations
Almost all participants in this study expressed ideas on how to improve the HART model, the suggestions themselves an indication of both investment in and thought to the practice environment they worked in. The thematic recommendations were not distinct to key stakeholder groups (administrator, HART team member or rural care provider), but instead cross-cut the participant groupings. The leading recommendation was to work at improving relationships, both between the hospital and the transport sites and between the HART program and provincial transport programs.
Beyond the need to attend to improving relationships, the overwhelming suggestion of participants in all sites was for HART to establish its own mode of transportation. Although a dedicated vehicle was the most common suggestion, several participants also suggested the need for consistent access to a rotary or a fixed-wing aircraft, particularly for distance communities. Participants felt that the capacity for rural sites to auto-launch HART would lead to more expedient transports.
Not surprisingly, participants in the smaller sites suggested that the availability of local HART CCRNs and RRTs would improve outcomes, and they suggested that availability could be achieved through site rotations of the HART team or having a rurally based reserve team to provide back-up. As one participant said:
I believe the HART team should be based out of [small community], or to have them based out of [referral community] and stay in [small community] for half a month. We have an active maternity service here – we have no RRT support. The HART nurse could be an adjunct here to labor and delivery. I see them using their skill set here, just like they could in [referral community]. (Nurse)
Many of the participants from rural sites recognized that they did not have the volume of high-acuity cases to keep critical skills up, but felt their site would benefit if the HART team were to be stationed with them on a rotating basis, even, as some suggested, for one day at a time. As one participant explained:
Their time is being totally monopolized in [the base hospital] – I don’t think that is a fair use of the resource. They should have a presence in [smaller communities] ... The population is very spread out around here. I wouldn’t make the argument that they be based [here], but I would strongly say that they need to have a real presence outside of [base site] and to realize that they can be dispatched from anywhere in the Region. (Physician)
Correspondingly, many acknowledged this might not be sustainable based on volume, costs, and the complexity it would add to the existing challenge of dispatching a vehicle effectively through provincial ambulance services. That is, the HART team member would likely need to be transported back to the ‘hub’ before travelling to the call and any delays in moving the team member could pose a risk to patients.
Discussion
Findings from the HART evaluation have been remarkably consistent among participants in demonstrating the need for an innovative solution to transport of high-acuity rural patients. There was strong thematic resonance across multiple sites on challenges faced by the program, such as delays in deployment and inter-organizational challenges. This finding is supported by literature acknowledging the organizational challenges rural hospitals face11, and the importance of a collaborative and coordinated approach for high-acuity transport in rural settings12-16.The salient issues are grounded in a somewhat artificial distinction between pre-hospital and interfacility transport for rural patients, which leads to a lack of service coordination and potentially avoidable delays. A beneficial systems change would be to move towards dedicated integration of high-acuity transport services into hospital organizational structures and community health services in rural areas.
Solutions to the larger issue of rural patient transport are system wide, demanding an integrated and networked team-based model to enhance communication and continuity for high-acuity patients as they are transported from rural community settings to small rural hospital ERs and then on to referral centres as required. The success of the CCRN supernumerary role encourages the system-changing idea that more patients can be stabilized on site at small rural hospitals, which is a finding supported by current literature11,17,18, lessening the instances of interfacility transport, but certainly not lessening the need for it. In some instances, allowing flexible deployment of personnel from the local hospital staff with transport expertise in response to the acuity of the 911 call may increase efficiency and effectiveness11. It is crucial that this flexibility is maintained while protecting the ideal functioning of the rural service11. Ultimately, this will require patient-centred emergency transport plans, which seamlessly integrate prehospital management, rural hospital care, and transport to definitive care11.
Limitations
A possible limitation to qualitative research interviewing is the self-selection of participants who have strongly held views. However, recruitment in this study was extensive as expressed through the total n=107. Additional theoretical concerns regarding integration of the HART program team management into the research team are plausible. It is the experience of the academic leads that this did not take place but instead the integrated approach enabled a more thorough understanding of the topic at hand and access to participants. Perhaps the most significant limitation of the analysis has been the absence of participants from provincial ambulance services and other system representatives. This lacuna does not impact directly on the veracity of the results from the HART program, but would provide additional insight into some of the higher-level challenges and will be undertaken as part of the next steps.
Conclusions
This in-depth qualitative research evaluation of an innovative rural patient transport program illustrates an effective and efficient model that is working on the edges of a provincial transport system to meet the particular geographic realities of rural landscapes. The management of the occasional high-acuity patient, however, is a problem endemic to all rural communities and gives rise to the need for other contextually responsive solutions. Further research on patient transport models would benefit from comprehensive cost-effectiveness analysis of such programs within a network of rural high-acuity patient care and information flow, quality management and continuing professional development/medical education. Central to all models and evaluation, patient and family experiences must clearly be understood and responded to. Maintaining the perspective of supports needed for rural sites, even when this perspective challenges the status quo, is an absolute necessity in strengthening the integrity of rural care.
Acknowledgement
The authors would like to gratefully acknowledge the key stakeholders (interview participants) who participated in this study.