Introduction
In Peru, the social health service (SHS) is performed by health professionals such as doctors, nurses, midwifes and dentists, with the objective of fulfilling the need for health care in the farthest rural areas of the country1,2. It lasts an entire year, and is considered a prerequisite to work in any public health institution in Peru, apply for a specialization program in Peru, or receive government scholarships1,3.
Depression is an important issue in health professionals, since it might affect their quality of life and even trigger suicidal thoughts4,5. Moreover, depression has been associated with higher rates of absenteeism, decreased work productivity and impoverished patient care6,7. Previous studies have found that labor migration can be an important risk factor for depression8-12.
Thus, health professionals performing SHS in Peru may be at risk of developing major depression, because they are beginning to work in rural areas, which are usually far from home, family and friends13, and therefore suffer an acculturation process that leads to conflictive relationships with co-workers and patients3,4. Moreover, it is possible that depression prevalence is higher among those health professionals who come from remote settings, or from settings with marked differences with respect to the place where they are performing SHS.
Despite the importance of the subject, the authors could not find studies that have evaluated depression rates in health professionals performing SHS, nor its association with their place of origin. This implies a limitation when trying to identify risk groups for depression among health professionals, on which preventive and therapeutic measures should be focused. Therefore, this study aims to evaluate the association between the place of origin and the presence of depressive symptoms in health professionals performing their SHS in Ancash, Peru.
Methods
Study design
A cross-sectional study was conducted among health professionals who were performing their SHS in Ancash, a Peruvian region.
Health professionals in Peru perform SHS for 12 months in primary healthcare facilities; nearly 90% of such facilities belong to the Peruvian Ministry of Health. Every year, two election processes take place, in which health professionals are assigned to the health facilities where they will perform the SHS: the first one in May and the second one in October1,3.
Ancash is a Peruvian region located north of Lima (Fig1). Its geography is characterized by a mountainous setting: the Andes Mountains cross the region. Some of the highest landmarks in Peru are located in Ancash, many of them being over 4000 m above sea level. In many rural communities of Ancash the most spoken language is Quechua, especially among the elderly.
Many of the health professionals that perform their SHS in Ancash and other Peruvian regions come from Lima city, where the number of graduate health professionals is higher.
Health professionals that perform SHS in Ancash are actually working for the local Regional Health Direction (abbreviated in Spanish as DIRESA Ancash), which is geographically divided into six health networks (Redes de Salud). Each health network has an SHS coordinator, who is in charge of the supervision of all health workers performing SHS in the health network.
 Figure 1: Map of Peru, Ancash, and Lima city.
Figure 1: Map of Peru, Ancash, and Lima city.
Participants
Health professionals performing their SHS in any Ministry of Health facility in the Ancash region during April 2015 were invited to participate. Ministry of Health facilities workers represent nearly 90% of all health professionals in SHS in Ancash.
Procedures
All six SHS coordinators, after the corresponding training, distributed the questionnaires to their respective health networks for self-application, during trips to facilities and personal meetings. Health professionals performing SHS who gave their voluntary participation were included in the study. The SHS coordinators collected the completed questionnaires in anonymous envelopes, and sent them to the investigators. Then, authors entered the data in a Microsoft Excel 2010 database using a double entry system to avoid errors during the process. Surveys with complete exposure and outcome of interest were included in the analysis, while subjects who completed their undergraduate professional studies out of Peru were excluded.
Outcome: depressive symptoms
The authors evaluated the presence of depressive symptoms using the Patient Health Questionnaire-2 (PHQ-2). This tool is composed of two questions, with four alternatives scoring 0 to 3 points each, for a total of 0 to 6 points14. It is used as a screening tool for depression, but does not diagnose depression14. The PHQ-2 questionnaire available at the Patient Health Questionnaire Screeners for Peru was used, taking into consideration the modifications suggested by Calderon et al. for Peruvian populations15.
PHQ-2 score ≥2 had a sensitivity and specificity for the diagnosis of major depressive disorder of 86% and 78% in adult patients attending primary care in New Zealand16, of 66.7% and 90.3% in patients with migraine17, and of 92.9% and 69.5% in patients with Parkinson’s disease18. Thus, the presence of depressive symptoms was define as having a PHQ-2 score ≥2.
Main exposure: place of origin
Place of origin was defined as the place where health professionals completed their undergraduate professional studies. It was evaluated through a direct question, and subsequently categorized as follows: (1) Ancash, (2) Lima city and (3) other cities. Lima city was considered as a separate option because the vast majority of universities with health professions are located in this city.
Other variables of interest
Other variables of interest evaluated in this study were age (in tertiles), sex, undergraduate university funding (public or private) and profession (physician or others). Variables related to the SHS were health facility category (I-1, or I-2/I-3), being in charge of the health facility for at least 3 months, referring work overload in the last 30 days, and having suffered any type of workplace violence during the previous 30 days (physical violence, verbal violence, threats or sexual harassment). Primary healthcare facilities where health professionals perform SHS in Peru are categorized according to their equipment and workforce as I-1 (with little equipment and workforce), I-2 or I-3 (with regular equipment and workforce).
Data analysis
All data processing and analysis was completed using STATA v14.0 (http://www.stata.com). For the descriptive analysis, measures of central tendency, dispersion, absolute frequencies and relative frequencies were used.
To evaluate the association between covariables and the presence of depressive symptoms, crude and adjusted prevalence ratios (PR and aPR) and their respective 95% confidence interval (95%CI) were calculated using Poisson regression with robust variance. The adjusted model included place of origin, sex, age, university funding, being a physician, health facility category, being in charge of the health facility for at least 3 months, work overload in the previous 30 days, and having suffered violence in the last 30 days. A value of p<0.05 was considered as statistically significant.
Ethics approval
This investigation was approved by the ethics committee of the Hospital Nacional Docente Madre-Niño San Bartolome in Lima, Peru (RCEI-40). The participation in this study was voluntary, anonymous and confidential. All data was handled only by the investigators.
Results
Population characteristics
From a total population of 573 health professionals performing SHS in Peruvian Ministry of Health facilities during the study, 364 were successfully found by the SHS coordinators, while the remaining 209 could not be located or contacted. All 364 health professionals gave their consent to participate in the study. After the application of the questionnaire, 32 participants were excluded due to missing information: four did not specify their place of origin, 11 had completed their undergraduate professional studies in another country, and 17 had no information regarding the outcome of interest. Therefore, 332 participants (57.9%) were finally included in the study.
Of the 332 included participants, 263 (79.2%) were female, the average age was 27.0±4.1 years, 78 (23.5%) were physicians, 263 (80.7%) worked in health facilities of category I-1 and 109 (33.1%) had been in charge of the health facility for at least 3 months (Table 1).
Concerning place of origin, 237 professionals had finished their undergraduate professional studies in Ancash (178 in Chimbote city and 59 in Huaraz city), 64 (19.3%) did it in Lima, and 31 (9.3%) did it in other Peruvian cities (10 in Trujillo, 10 in Piura and 11 elsewhere).
Table 1: Characteristics of health professionals performing social health service in Ancash, Peru, 2015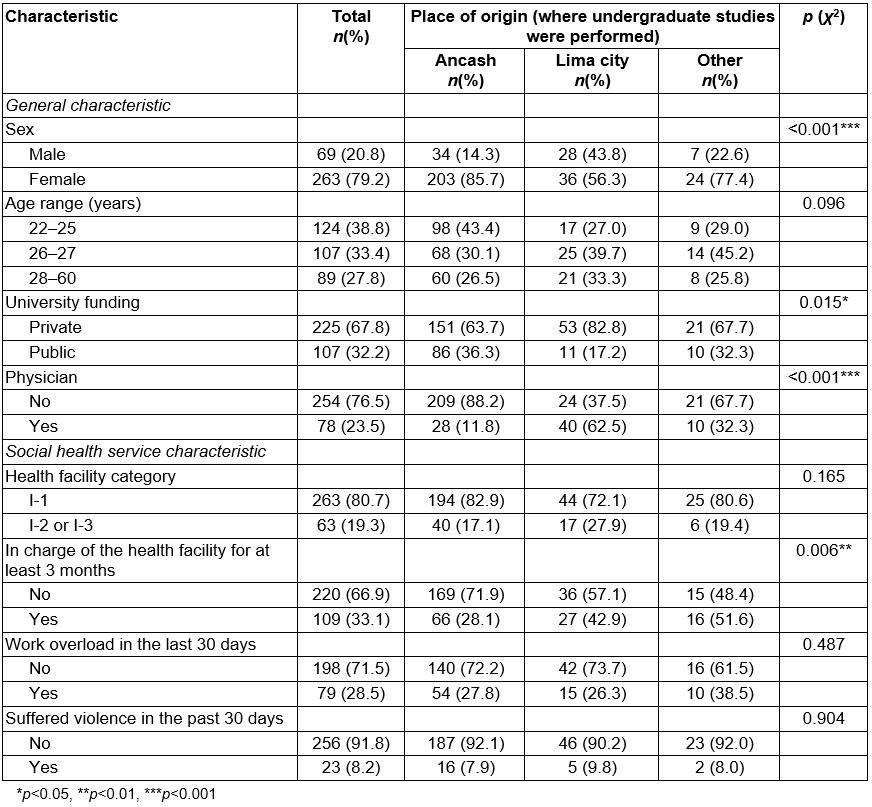
Depressive symptoms
Of the 332 included participants, 49 (14.8%) had depressive symptoms, defined as a score ≥2 in the PHQ-2 questionnaire. The proportion of having depressive symptoms was 25.0% in health professionals who completed their undergraduate professional studies in Lima, 13.1% in those who did in Ancash, and 6.5% in those who did in other Peruvian regions.
In the adjusted model, those who finished their undergraduate studies in Lima city had a higher prevalence of depressive symptoms, compared to those who did in Ancash (aPR=2.40, 95%CI=1.20–4.83). In addition, those who referred work overload during the last 30 days had a higher prevalence of depressive symptoms than those who did not (aPR=3.14, 95%CI=1.57–6.31) (Table 2).
Table 2: Factors associated with obtaining a PHQ-2 score ≥2 in health professionals performing social health service in Ancash, Peru, 2015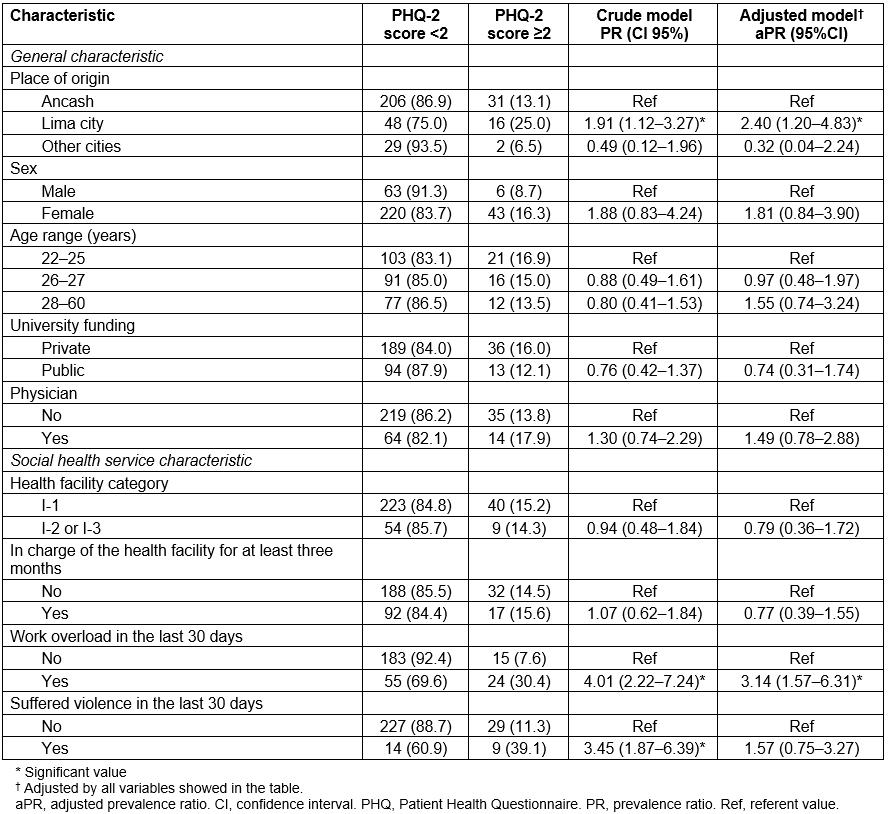
Discussion
In this population of health professionals performing SHS in Ancash, the overall frequency of having depressive symptoms was 14.8%. This frequency was up to 25.0% in those who performed their studies in Lima and 13.1% in those who did it in Ancash. In the adjusted model, those who performed their studies in Lima had a 140% greater chance of having depressive symptoms compared with those who completed their studies in Ancash.
Screening of major depressive disorder
In this study, 14.8% of professionals had a PHQ-2 score ≥2, implying a risk for major depressive disorder19,20. This prevalence is much greater than the 2.7% overall risk of major depressive disorder found in the general population in Peru by the Composite International Diagnostic Interview19 and the 5% estimated for the whole world by the World Health Organization20. However, these studies have not used the PHQ-2, so comparing the results is not adequate.
Some studies have explored the prevalence of depressive symptoms in primary health professionals, using different instruments that sought to approach a risk for major depressive disorder. In Sao Paolo, Brazil, 16% of the participants scored ≥5 using the PHQ-9 questionnaire21. A study in Mexico found a prevalence of 12.0% using the Center for Epidemiologic Studies Depression Scale22. A study in primary healthcare physicians in China found a depressive risk of 31.7% using the Zung Scale23. The high heterogeneity of depression screening instruments used in these studies represents a challenge when trying to make feasible comparisons.
The authors have identified only one study that uses the PHQ-2 to evaluate the prevalence of depressive symptoms in health professionals. It was performed in German primary care physicians and found that 23% of them had a PHQ-2 score ≥324. Conversely, only 6.0% of the population in the present study had a PHQ-2 score ≥3. Thus, the prevalence of depressive symptoms seems lower in the present study.
Association between place of origin and depressive symptoms
All health professionals who perform SHS are labor migrants who are working in rural environments. However, those who completed their undergraduate studies in Lima had more than double the probability of presenting depressive symptoms than those who did in Ancash. Although some studies have evaluated the association between place of origin and mental health problems8-10, this is to the authors’ knowledge is the first study comparing the presence of depressive symptoms among health professionals who migrate from different locations.
The link between the place of origin and depressive symptoms probably has many pathways. However, the authors propose three suitable explanations: (1) Those coming from Lima are much further from their home that those coming from Ancash; (2) those coming from Lima are exposed to a new cultural setting and environment, which may be familiar to those coming from Ancash; (3) those coming from Lima have little knowledge of Quechua, one of the main languages used in rural Peruvian settings, than those coming from Ancash.
The first explanation states that health professionals coming from Ancash are usually a few hours away from their workplace, while those coming from Lima are usually at 24 hours or more away. Because of this, opportunities to return to their hometown and visit their friends and family are limited for those coming from Lima. By law, health professionals performing SHS are granted one day off every week, but the current regulations do not clarify if these free days could be accumulated or not. In consequence, health professionals in many health facilities have only one free day per week, usually on Sundays1, which affects disproportionally those who are at a greater distance from home, preventing them visiting their relatives or friends. This beholds a chance for change – making more flexible schedules might grant health professionals the opportunity to travel to their home towns, potentially lowering their risk of depressive symptoms.
The second explanation states that professionals who completed their studies in Lima are less familiar with the culture of rural communities than those from Ancash, and must undergo a process of cultural and social insertion (acculturation), which could lead to stress and depression9,11,13. This could be because Lima city, with more than 9.8 million habitants, has a higher degree of urbanization than the Ancash cities of Huaraz and Chimbote, with approximately 127 000 and 371 000 inhabitants respectively25, which may still maintain some rural manners and traditions. Besides, students of health professions in Ancash could be performing more pre-professional practices in rural settings than those from Lima. Taking this into consideration, it is of great importance that universities expose their students to rural settings similar to those where they will work in their SHS. An interesting approach performed by a Peruvian medical school is the implementation of a ‘rural internship’, in which its students participate in a 12-week practice in rural areas26.
The third explanation states that health professionals coming from Lima are rarely exposed to Quechua, which is the predominant language in many of the rural Peruvian settings, including those of Ancash. This becomes a big inconvenience for health professionals for whom verbal communication is essential. Moreover, it poses a big difficulty when performing health promotion activities or solving problems with the community members or authorities. Therefore, it is necessary to consider the inclusion of languages widely used in rural Peruvian communities, such as Quechua and Aymara, in the curricula of Peruvian health professions. To date, only one out of nine medical schools in Lima has a mandatory Quechua course, while other medical schools have an elective Quechua course27.
These results highlight the necessity of screening activities to evaluate depression or depressive symptoms in health professionals performing SHS in Ancash, especially among those coming from Lima. However, the remoteness of health facilities where these professionals perform their SHS demands innovative strategies, such as virtual interventions, which have proven to be effective to some extent in the treatment and prevention of major depressive disorder28,29.
On the other hand, the prevalence of having depressive symptoms in health professionals coming from Ancash was not statistically different from the prevalence in health professionals from ‘other cities’, probably due to the small number of subjects in this second group.
Other factors associated with depressive symptoms
Health professionals that reported work overload in the previous month had three times the probability of presenting with depressive symptoms. This association has been previously reported30,31, along with its negative consequences on quality of life, and economic burden31,32. Therefore, it is necessary to identify the causes of high stress levels and work overload in order to implement preventive strategies. Interventions with workshops and practical seminars could be helpful33.
Limitations
Certain limitations must be mentioned. First, the population surveyed was limited only to one region of Peru, and it is possible that health professionals performing SHS in other regions have different results in terms of the variables of interest. Second, almost a third of the health professionals could not be found nor surveyed, presumably those who were performing their SHS in the most remote settings, who could have a higher prevalence of depressive symptoms. Third, few participants were categorized as coming from ‘other cities’, which prevented a comparison of this category with others. Fourth, no direct evaluation of the PHQ-2 questionnaire has been made in Peruvian populations, so no detailed data on its sensitivity and specificity is available.
Conclusions
Approximately 15% of participants in this study had depressive symptoms. Those who completed their studies in Lima presented with a higher prevalence of depressive symptoms. Possible explanations include the difficulty of visiting family and friends, acculturation, and lack of Quechua language proficiency. Therefore, labor migrants from Lima seem to be at higher risk of having depression, which should be considered when planning screening and preventive interventions for mental health problems in health professionals performing SHS.





