Introduction
The use of implantable cardioverter defibrillators (ICDs) for primary or secondary prevention of life threatening ventricular arrhythmias is recognised as having substantial mortality benefits1. With the ageing of the population in New Zealand and Australia2 their use will increase, a trend already noted in both Australia3 and New Zealand4.
While the clinical benefits of this treatment are clear, insertion of an ICD can be associated with adverse physical, psychological and social consequences5-7. Decreased energy levels and sleep disturbances are two of the physical sequalae8. Psychologically, clinical levels of depression and anxiety have been described, due to fear of receiving a shock from the device, fear the device will not work and fear of death9,10. Recipients describe the experience of living with an ICD as one of ‘constantly redefining oneself’11. Recent research has highlighted that certain aspects of care may be unmet with the change of clinical management and care shifting from face-to-face clinic visits to remote monitoring12.
Other challenges for those with an ICD are also present in the literature. A recent prospective, international, multicentre patient survey conducted in seven European countries highlighted that, of the 1644 patients surveyed, 20% did not want to address end-of-life issues, such as deactivation of the device13. The literature relating to the role of support groups after insertion of an ICD is also mixed, with some favouring learning from others with similar experiences and others rejecting this format due to their lack of anonymity and the inconvenience of attending11. Furthermore, knowledge of ICDs within primary care, the first port of call for most patients, is limited. This can lead to important gaps in the planned care of ICD recipients, especially around end-of-life care decisions. Primary healthcare practitioners unaware of the importance of deactivation of the device as a recipient’s end of life approaches are unlikely to learn about this issue from the recipient, as previously highlighted13.
A considerable amount of research examining the lives of ICD recipients has viewed their life situations homogeneously, with the focus of the research frequently taking a unidimensional emphasis on psychological responses to implantation. There have been few attempts to explore the different contexts of recipients’ lives, for example the experiences of rural dwelling recipients in comparison to their urban counterparts. In a recent international review of perceptions and experiences of patients living with an ICD, the term ‘rural’ was not mentioned11.
New Zealand, like Australia, has a significant rural population, with approximately 600 000 residents living rurally, making rural New Zealand the second largest ‘town’ in the country14. Unlike Australia, New Zealand does not have an agreed rural–urban classification for health, making it challenging when undertaking research exploring the influence of rurality15,16. Older adults are more likely to live outside of the major urban centres in New Zealand, with this group more likely to be recipients of ICDs3. Therefore, it is timely that an understanding of the experiences of rural ICD recipients is developed. This study aimed to answer the following questions: ‘Does living rurally impact the ICD recipient experience and that of their partners?’ and ‘Can understanding their experiences inform best practice care for those living rurally with an ICD?’
Methods
Participants (ICD recipients and their partners) for this qualitative study were recruited from rural Southland, the southernmost region of New Zealand, where almost 50% of the population live outside of the region’s largest town, of 52 00017. Participants were identified from a cardiac technician database, with 86 current ICD recipients found in the Southland region of the Southern District Health Board. Of these, 33 were determined as living in a rural area or independent urban area based on Statistics New Zealand’s definitions18. Independent urban areas are settlements that are not significantly dependent on main urban centres. Participants were sampled purposively with the aim of ensuring maximum variation sampling (male/female, a range of ages and ethnicities, provincial town/rural/remote, time since ICD implanted). Semi-structured interviews were used to collect the data. Two topic guides, one for recipients and one for partners/carers, were developed based on the literature review and discussions within the research team. These were employed flexibly in the interviews. A debriefing meeting was planned following the analysis phase, enabling feedback to participants to ensure interpretations of the interview data reflected participants’ experiences correctly. Inability to understand and to converse in English were the only exclusion criteria.
All interviews were digitally recorded and transcribed verbatim. The text data were investigated using inductive thematic analysis19. An interim analysis of the first 10 interviews was undertaken by the second author (GNo), who developed descriptive codes and organised these into higher order thematic categories. Half of these transcripts were provided to FD-N, who coded them separately for comparison of thematic categories. TS independently assessed the plausibility and explanatory value of the developed categories against a selection of the transcripts. Four more interviews were then conducted. These participants lived in satellite urban communities. These are towns or settlements with strong links to a main urban centre. This definition is derived from the employment location of residents18. Following the coding of the transcripts, all participants were invited to the post-research debriefing meeting, facilitated by FD-N and GNo.
Ethics approval
Ethics approval for the study was granted by the University of Otago’s Human Ethics Committee (H17/006) and locality assessment approval was obtained from the Southern District Health Board.
Results
Of the initially contacted 33 recipients, 11 agreed to participate, with 10 interviews completed. A second mailout to a further 11 recipients, identified as living outside of the main urban centre, yielded an additional four participants. In total, 14 ICD recipients and nine partners/carers/whānau (family) were interviewed. Of the 14 participants, one was female and one was Māori. Ten had received their ICD for primary prevention purposes and the range of time since insertion was 1–12 years. At the project’s conclusion, five participants, their spouses and other whānau/carers attended the post-research debriefing meeting. One recipient died during the study period.
Analysis of the interview data revealed common themes between ICD recipients and their spouses and other whānau/carers. Themes unique to one or other group are presented in Figure 1, with this diagrammatic form employed to demonstrate a sense of the interconnected relationship of the themes.
An important theme common to both recipients and their spouses, and other whānau/carers, was that of the recipient–spouse or recipient–carer dyad. Essentially, this theme encompasses the concept of the dyad as an interdependent team, navigating the recipient’s post-implantation life. Within this dyad, however, the health and wellbeing of one member was prioritised over the other, resulting in potential unmet healthcare needs of spouses and other whānau/carers:
I’ve often wondered whether I should have the odd check-up too, to see how I am doing as a caregiver, … so it did cross my mind that spouses should perhaps have a check-up occasionally. (spouse of participant 9)
The prioritisation of recipients’ health and wellbeing needs is clearly expressed in the following quote, where it is clear the spouse is also stressed.
You’ve got to settle the patient – he’s a worrier, and then inwardly you are too, but you’ve got to remain strong and convincing that, yes things are okay. (spouse of participant 4)
The conversations with the mainly male recipients further emphasised this point by the almost total absence of any reference to the health and wellbeing needs of their spouses or other whānau/carers, most of whom were older themselves. However, the seeming lack of direct reference to spouses by recipients may in part have its origins in how the implant process is experienced by some couples:
[Facilitator] As a spouse, during this process around the implanting of it, are you engaged with directly by the doctors and so on there?
[Interviewee] No. Only [recipient].
[Facilitator] So no-one comes and talks to you as well?
[Interviewee] No.
[Facilitator] What do you think about that?
[Interviewee] I don’t think it’s right. I think when you are a partner you should be included, but then [recipient} has to have his say, too. So that’s not the way he wants it, so that’s not what happens, but he does bring me the information and tells me after he’s been to his appointments.
Strongly linked to the adult patient–care partner dyad theme was the theme of responsibility. Spouses and other whānau/carers felt a significant sense of responsibility for those who had received an ICD:
I tend to be a bit over the top with pills making sure he has his pills. So I suppose he’s got a bit reliant on me preparing the pills and he wouldn’t know which pill was which probably if I didn’t have them in the pill container. (spouse of participant 12)
For both recipients and their spouses and other whānau/carers in this study, there were common challenges post-ICD implantation. These challenges included advance care planning and a conversation about deactivation of the ICD, the absence of a support group, healthcare experiences and technology.
Participants and their spouses and other whānau/carers were uncomfortable discussing advance care planning and their views on deactivation of the device. Consequently, these topics were largely unexplored during the interviews. When comments were made, they were brief:
If a person becomes very elderly, … do they ever remove them [the ICD], or do they ever give the person a chance to actually pass away? (spouse of participant 2)
That’s interesting, because it [advance care planning] has never been approached between the two of us or any medical person either. (spouse of participant 2)
At the debriefing meeting held to determine if the research team had understood what participants had told them, a sensitively facilitated conversation addressed the area of advance care planning and deactivation of the device. This discussion was facilitated by FD-N, who has a nursing background, with many years of experience in the area of cardiac rehabilitation and of working with recipients of ICDs and their spouse/carers from the UK. The group discussion clarified that the collective reluctance to discuss the topic was driven by a misconception around deactivation and time to death, as well as a lack of awareness of what happens if the device remains active during death. The outcome of these misunderstandings was a reluctance to complete an advance care plan. Participants agreed that the timing of the conversation was challenging for all involved.
The lack of a support group in the region was another joint area of concern. Some participants, recipients and partners had experienced a support group in the past but at the time of the study being undertaken it was in recess. Reflecting on this invoked notions of fellowship and the benefits of information sharing:
It’s like everything, if you watch something once it’s good to look at it a second time. So there was the nutrition and there was keeping your exercise and general wellbeing. I can’t remember what it all covered but it was very good. It was very well run. They were very friendly … (spouse of participant 9)
Yeah, I liked meeting the other people – the advice and they explained how they cope, and things like that; that’s what I liked about it. We used to get a letter in the mail to say when the next meeting is. They used to have them probably about every three months or so. Used to be quite a few people there. (participant 14)
The lack of a support group was keenly felt by participants. As a result, at the conclusion of the debriefing meeting referred to earlier they spontaneously shared contact information and developed a phone tree.
For both recipients and spouses and other whānau/carers, experiences within healthcare services were mixed:
I found the X medical people up there with the heart department were absolutely brilliant – no complaints whatsoever at all … (participant 2)
He gives us the script for antibiotics to take overseas with us, which not every doctor does. So he’s very good like that, but maybe we shouldn’t have to say – how do I put it; is it time we had a blood test? I think the doctor should be the one to think. (spouse participant 12)
Two aspects of advances with monitoring technology were raised. For this generally older group of participants, setting up their remote monitoring unit when they returned home could be a challenge. In part, this challenge was exacerbated by a lack of information:
Yeah, they explain what it was all about – what this thing would do, … but what they didn’t do really as to explain just how to set the thing up. (participant 9)
For all participants, technological advances in remote monitoring were associated with fewer interactions with the health professionals, which was not always viewed favourably. Generally, however, they felt confident that, should they need to see their main point of contact in the region, the cardiac technician, access would not be an issue:
[Facilitator] Is that something you’ve noticed at all, or have you thought, oh gee I’d like to be able to talk about this a bit more?
[Interviewee] No. Well, she [a health professional] has said, you don’t have to leave it six months – if there is a time that you feel that you want us to have a look at something, or you’re a bit anxious about something, just come in. (participant 13)
For ICD recipients there was a specific theme encompassed by the phrase ‘life with an ICD’. This theme comprised three subthemes: emotions, unmet information needs and restrictions. The subthemes, their associated descriptor and an illustrative quote are presented in Table 1.
Notwithstanding the challenges of life with an ICD for these rural participants, this study highlighted an overwhelming agreement by both recipients and their partners that an ICD should be viewed as an enabling device:
I think the other thing is that this thing is supposed to enable your life, it’s not supposed to disable your life. If you’re enabling somebody’s life that will allow them to carry on doing the things that they’re doing in the way that they’ve been doing them for as long as that is possible – you don’t want it to be an impediment … If you can live with it and forget about it, that’s the perfect world because ideally you’re not going to need it but it’s there if you do. (spouse of participant 3)
Table 1: Subthemes, associated descriptors and related quotes from the recipient-specific theme ‘life with an ICD’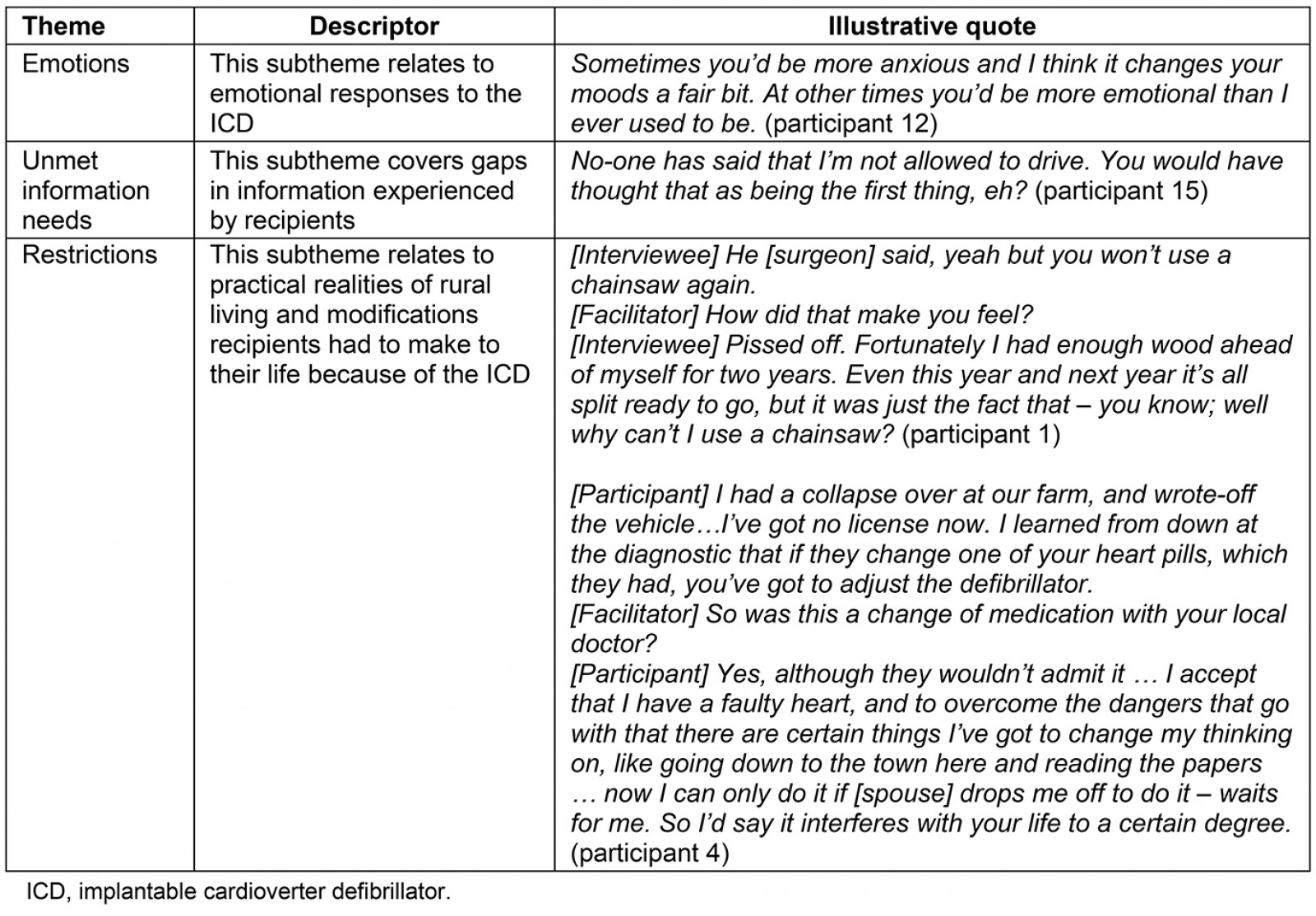
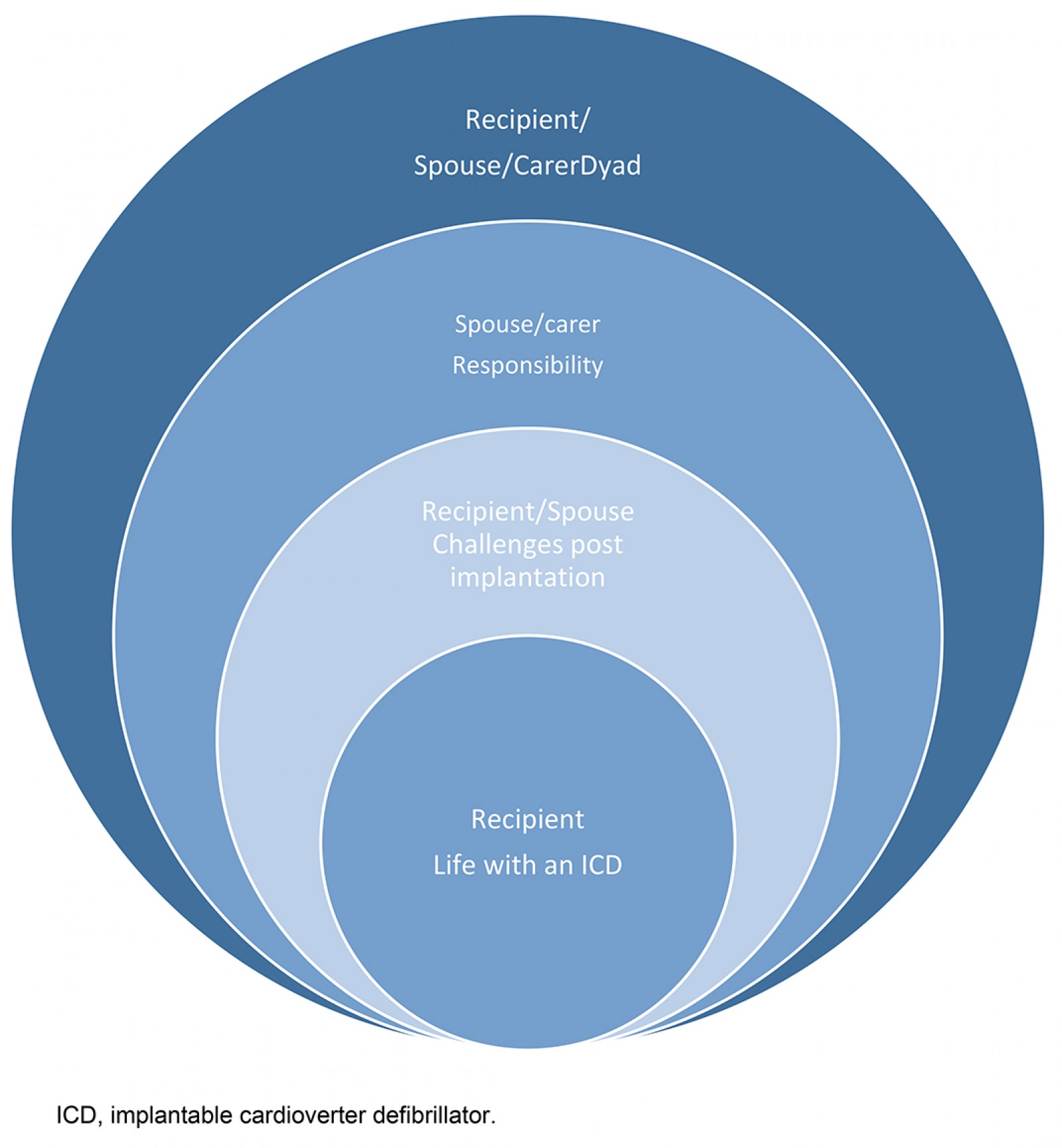 Figure 1: Themes developed from the text data.
Figure 1: Themes developed from the text data.
Discussion
This has been the first New Zealand study to consider the lives of those who live in rural areas following the insertion of an ICD. Place of residence did not seem to significantly affect the post-insertion experience of the recipients or their partner/carers. The principal theme from this study related to the role of the adult patient–care partner dyad in an ICD recipient’s recovery and the influence of a recipient’s illness on the healthcare needs of their partner/carer. Strongly intertwined with the role of the dyad was the pervasive sense of responsibility partners/carers felt. This sense of concern was tangible, irrespective of their own level of healthcare need; however, this level of concern was not overtly reciprocated by ICD recipients. Challenges were identified in the post-ICD insertion period but the rural locale of participants did not feature as a challenge in terms of access to health care; rather, the restrictions placed on individuals with the ICD had repercussions due to the practicalities of rural life.
These study findings require cautious interpretation in light of study limitations. Along with its small size, the composition of the sample had a number of demographic differences compared with other ICD studies including the few undertaken in New Zealand, with only one female recipient and one Māori recipient interviewed20-24. In addition, any interpretation needs to consider that the partner sample was entirely female and this may be why the dyadic relationship developed as such a strong theme. A further limitation is that the study did not include an urban sample of ICD recipients and their carers for comparison.
The strength of this study lies in the constant comparison of the data analysis between FD-N and GNo, the independent assessment of the plausibility and explanatory value of the developed categories by TS, and the process of member checking at the debriefing meeting. These processes support the validity of the analysis, as does the complementarity of findings between this study, other older studies and more recent ICD studies, irrespective of locale5-7,9,10,13.
The influence of the care recipient and caregiver dyadic relationship on the recovery journey of these ICD recipients was an important association. The significance of the care recipient and care giver dyad on health, illness appraisal and symptom management has only been recognised in more recent years25, especially within heart failure literature26,27. The importance of the dyad is, however, gaining more traction as a concept within chronic illness management overall28. Therefore, health professionals caring for ICD recipients need to be mindful of the role informal carers play on recipients’ recovery and the potential for the health of caregivers to be compromised.
Studies have found the unmet needs of informal caregivers differ between urban and rural residents. Informal rural caregivers seem to have greater unmet needs in relation to activities such as grocery shopping and preparing meals, and are more likely to experience financial barriers; however, they are less likely to perceive and report caregiving challenges than their urban counterparts29. Other research suggests this may be due to the self-reliance commonly characterising those living rurally30, as well as limited rural service options motivating rural carers to more readily identify informal and social supports than their urban-based counterparts31. Older caregivers, such as those in this study, are recognised as a group with the potential for experiencing significant unmet needs, as identified in a recent systematic review32. Khan and colleagues found evidence of gaps in a number of domains of the health and social care needs of older caregivers, including psychosocial, service and informational needs; constancy of care; future care planning; physical health issues; reluctance to utilise services; and financial needs32.
Dyadic illness management theory focuses on the dyad as an interdependent team25. This interdependency within the dyads in this study was out of balance with the partners/carers experiencing a significant sense of responsibility, which often appeared to not be reciprocated to the same degree by the recipients. A number of factors may account for this imbalance, including the illness experience of the recipient and the gender or age of the partner/carer25. All partners/carers in this study were female, and female gender has been recognised as a significant determinant of improved patient self-care maintenance in heart failure33.
A possible alternative interpretation of the relationship between recipients and their partners witnessed in this study could potentially be associated with regional personality differences and their influence on illness behaviour. Anecdotally, in New Zealand the ‘Southern Man’ is stereotypically viewed as a strong silent type whose actions speak louder than his words. Two recent New Zealand studies, however, found that regional similarities in personality far outweighed regional personality differences, which were fairly trivial34,35. Consequently, the stereotypical view of the ‘Southern Man’ is unlikely to influence the interactions between couples and how they manage the post-implementation experience.
For this study, the debriefing meeting answered queries of participants about deactivation and clarified for the research team why engaging the participants in discussing advance care planning in the interviews had been difficult. The timing of the conversations involving advance care planning, which for this patient group included considerations around the timing of deactivation of the device, was a key challenge. Participants acknowledged that approaching the conversation was problematic for all concerned. A recent study by MacIver and colleagues clarifies times that ICD recipients consider appropriate for the deactivation conversation to take place, namely prior to implantation, when any significant deterioration in clinical status occurred but while they remained competent to communicate their preferences, as well as at end of life36. Knowing these times and that multiple heart organisations worldwide endorse deactivation conversations, and that deactivation is both legally and morally acceptable when it is consistent with patient goals36, may encourage more clinicians in both primary and secondary care to have the deactivation conversation with ICD recipients and their partners.
Those with ICDs and their partners are recognised as having a strong identified need to be informed37. Learning from others with similar demographics and experience of living with an ICD is acknowledged as being important to some after insertion of a device11. Support groups assist participants to improve their self-efficacy in a number of ways such as by the provision of vicarious experiences and hearing from others regarded as expert sources38. Meeting support group needs for those who live in varying rural locations is seen as challenging. Funders and planners of health services that cover rural areas may want to consider the evidence that groups delivered by video-conference for a range of health issues are viable, with outcomes comparable to face-to-face groups39. There is a need to engage with telecommunication providers, such as the New Zealand Telehealth and Resource Forum, to drive the provision of high-speed broadband to all rural areas, enabling those who live rurally to enjoy the same support as those living in urban environments.
Those working in the health system also failed at times to provide the necessary advice, and on occasions advice was contradictory. A recent systematic review and meta-synthesis exploring the perceptions and experiences of those living with ICDs found that general lack of support from the healthcare team was a recurring theme37. Moreover, lack of continuity and time constraints were identified as barriers to satisfying information needs. In today’s world of multimorbidity, ICD recipients are admitted into a variety of medical departments; however, a recent study by Westerdahl and Frykman found a significant difference in ICD knowledge between physicians who worked in cardiology, internal medicine and geriatrics, with those in geriatrics scoring the lowest40. In addition, primary care physicians are less aware of ICD clinical guideline content than cardiologists41, yet recipients are likely to have more contact with their primary care physician after implantation than their cardiologist.
Although the researchers considered that rurality might impact negatively on the experience of ICD recipients and their partners, it appeared that rural living had a limited negative impact. Remote monitoring reduced the travel burden for rural recipients, thereby reducing out-of-pocket expenses, as well as enabling cardiac events to be detected earlier and inappropriate shocks reduced42. Remote monitoring was associated with some challenges for older participants in this group in relation to setting up equipment when they arrived home, with a number leaving the task for a couple of days. Other studies have drawn attention to this double-edged sword of remote monitoring for ICD patients42. While it could be argued that this challenge also faces the urban ICD recipient, access to other supports to resolve the issue is usually easier in terms of geographical access, at least for urban patients.
Participants acknowledged a variety of practical challenges related to rurality. When discussing the initial impact of ICD implantation, many reported that they had been advised to cease operating chainsaws and other power tools, common devices in a rural environment. Nonetheless, many admitted that they continued to use these tools, particularly chainsaws. For several participants who were still actively working on farms, electric fences were likewise identified as posing problems, especially when controlling stock movements. A reduced ability to undertake hard physical labour that had been a defining feature of participants’ lives was viewed with regret. Additionally, several participants described periods in their post-implantation lives when they had lost their driver’s licences for 6 months due to receiving electrical therapy from their ICDs. This is a significant problem for those living rurally due to the lack of public transport in these rural and remote areas. People either have to rely on family or friends to take them to appointments or to shop for groceries.
Conclusion
This is one of the few studies that has considered the influence of rural location on the post-ICD insertion experience of patients and their partners/carers. Rural living post-ICD insertion did not appear to substantially negatively impact the lives or experiences of these recipients and their partners/carers. For some, however, the practicalities of rural living were restricted and this proved a major irritant. The challenges associated with life post-ICD insertion were similar to those in other studies. The findings, however, suggest that female partners of rural ICD recipients undertake a significant role in terms of shouldering varying responsibilities including medication management, emotional support and transport. As the age of ICD recipients increases, so does the age of their partners; therefore, they are also likely to have one or more long-term conditions. Health professionals need to be aware of this additional burden as research suggests rural informal caregivers are less likely to report associated issues compared to their urban counterparts.
Acknowledgements
The research team would like to extend their utmost thanks to the participants of this study for giving their time and sharing their experiences with us. Without them, this study would not have been possible. The research team are indebted to the Southland Medical Foundation, who funded this study for the benefit of the people of Southland.
References
You might also be interested in:
2020 - Evaluating a centralised cancer support centre in the remote region of Northern Norway
2019 - Strategic analysis of interventions to reduce physician shortages in rural regions