Introduction
Sub-Saharan African countries continue to face challenges in regard to general population health improvement, health systems strengthening and the education of health professionals1-4. Scanning the literature, it is clear that increasing attention is being paid to the need to transform medical education through the development of relevant skills and competencies that are able to address patient and community needs relevant to their contexts and to strengthen health systems1,2,5-7. There are constraints in South African medical training that limit academic institutions from meeting the needs of the country8. The challenges are systemic as the absolute number of graduates that are produced per annum is not enough to respond to the country’s needs, and medical schools are centered around large tertiary hospitals in the cities. In addition, there is a skewed distribution of healthcare professionals, as most favour placement in urban based health facilities for a range of personal and professional reasons.
Like many other countries, South Africa is facing a paradigm shift with regard to identifying suitable training platforms and learning environments for medical education that would produce a more suitable graduate. Health personnel will be regarded as being ‘fit for practice1’ and socially accountable9, if they are able to address the health needs of the communities they serve. The focus for medical education is thus shifting towards strengthening primary health care and community based health services10. In particular, Kent and De Villiers10 accentuated the importance of medical education that produces health professionals ready to practice in rural and remote areas, and there has been a move towards this in the country11.
Transformative learning acknowledges the importance of context, relationship formation between students and society, and experiential learning12-14. As such, transformative learning can occur by indulging in community activities that will positively affect the health of the population15. Rudolf et al. emphasized the value of planning student activities with the communities where students are involved in service learning16.
Although there are clear gaps with regard to graduate competencies and meeting health system needs, medical schools are considered critical in transforming medical education by supporting a shift away from tertiary education towards decentralized training platforms (DTPs)17. Studies have been conducted showing how DTPs have been used as an approach to train a greater number of suitably trained health professionals who are more likely to remain in the underserved health sector18. DTPs allow for an understanding of the context and local needs in which learning occurs, which in turn assists in addressing relevant competencies19. Through decentralized platforms, understandings of context, culture and community are strengthened and social responsibility is encouraged through student involvement in community based projects and service learning activities20.
This study is part of a larger study entitled ‘Transformation of medical education in South Africa (TIME-SA)’ led by the University of Kwa-Zulu Natal. The other collaborating partner universities include Walter Sisulu, Sefako Makgatho and Witwatersrand universities. This scoping review focused on the thematic area that highlights suitable training platforms and learning environments as one way of fostering the transformative agenda in medical education. Therefore, this scoping review aimed to present a synopsis of the existing literature on DTP strategies for medical education, outlining existing models within it and its impact. The specific objectives were to identify DTP strategies in medical education, outline the existing models of DTPs, and highlight their capacity for realising academic, service and social learning agendas.
Methods
This study utilized a scoping review approach to collate literature on decentralized training platforms. It followed Arksey and O’Malley’s framework, which outlines the following five stages of conducting a scoping review: (i) identification of a research question, (ii) identification of relevant studies, (iii) study selection criteria, (iv) data charting, and (v) collating, summarizing and reporting results21.
Stage 1: Identification of a research question
This review was guided by the following research question: what are the existing models of DTPs within medical education and what capacity do they have for realizing academic, service and social learning agendas?
Stage 2: Identification of relevant studies (searching literature)
Literature was searched using different sources such as online databases, reference lists and hand searched journals (manual search of literature in journals). The online database search was conducted using Cochrane library, Wiley online library, PubMed, Ebscohost, ERIC, Science Direct and Springer Link. A search strategy was developed based on the research question outlined above. The original search comprised word strings/word phrases, outlined in Table 1.
Further literature was obtained by checking the reference section of articles retrieved from the online databases and through hand searching journals deemed appropriate by the authors, namely African Journal of Health Professions Education, African Journal of Primary Health Care and Family Medicine, Australian Journal of Rural Health, Journal of Family Health, Medical Teacher, Medical Education, Rural and Remote Health, South African Journal of Higher Education, South African Family Practice and The Journal of Rural Health.
Table 1: Word strings/word phrases used in original literature search to identify existing models of decentralized training platforms within medical education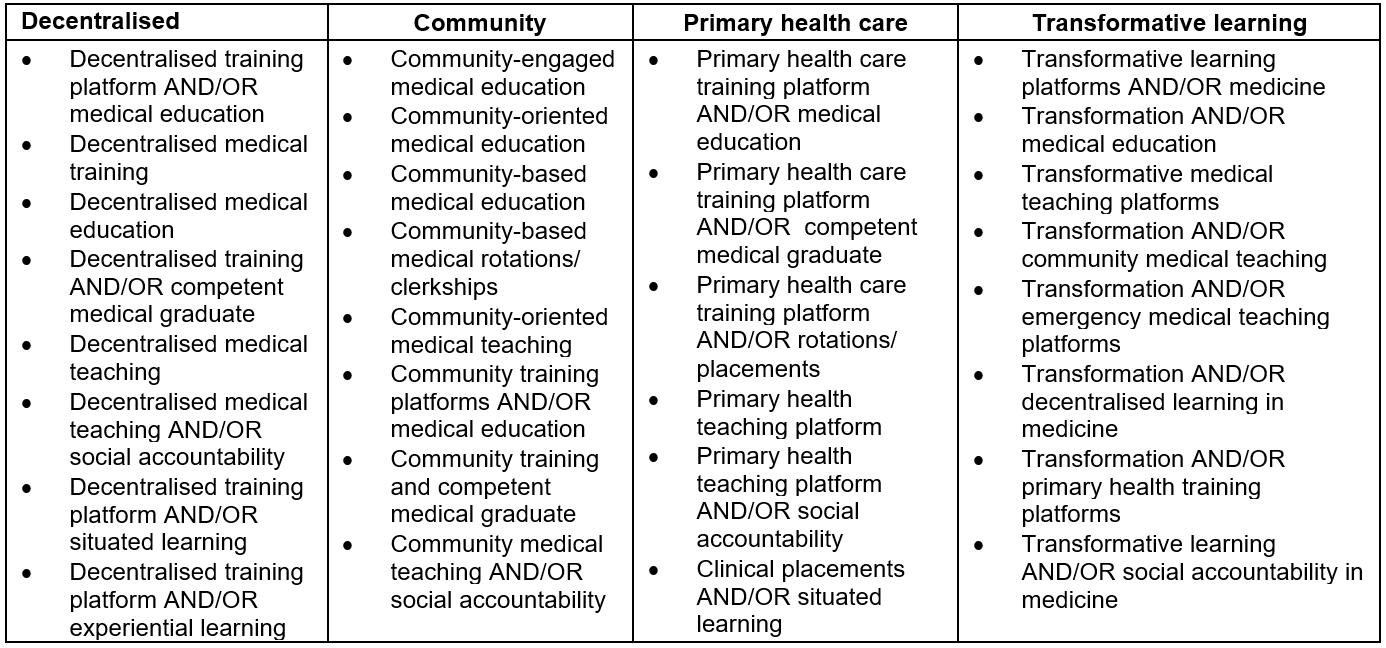
Stage 3: Study selection: inclusion and exclusion criteria
Articles were excluded if the title and abstract did not reflect the key word strings. Inclusion was based on all titles that referred to decentralization in the context of medical education, medical students, service delivery, governance, management and economics, and health services. The inclusion criteria were not limited by year and study design, to allow for a wider body of literature. All articles written in English, with a relevant title and abstract, for which full text articles could be obtained, were included in the study. Titles and abstracts were independently screened by two research assistants. Full text articles were later reviewed independently by three different reviewers (MM, AD and RD). In order to resolve any article screening and review discrepancies among reviewers, ongoing meetings took place throughout the review process22.
Stage 4: Charting of data: presentation of results
To keep track of records retrieved during the scoping review, all the extracted full text articles were managed using Endnote bibliographic software. An inductive analysis approach was used to chart and sort the data according to key themes. A data charting form was developed to capture information from various sources according to author, year, publication type, sector, aim, setting, type of study, methodology and study outcomes. Data was captured on Microsoft Excel, 2013. Descriptive analysis for study characteristics was conducted using Statistical Package for the Social Sciences v23 (SPSS; http:www.spss.com).
Stage 5: Collating, summarizing and reporting results
The scoping review findings were described narratively to provide insight regarding the content of each article.
Ethics approval
The scoping review was conducted as part of a larger study whose protocol was approved by the University of the Witwatersrand Human Research Ethics Committee (clearance certificate no: M151191)
Results
Overview of results
The initial comprehensive search process, which involved doing multiple searches using the broad search terms (word strings) listed in Table 1 within the various electronic databases described, yielded more than a million articles. The a priori decision was taken to focus on only the first 100 articles per search, sorting by relevance, as described in the review of scoping reviews by Pham et al23; using this approach yielded 12 923 articles. In cases where less than 100 articles were retrieved from a database (as part of the initial search), all articles were screened. Title screening was then carried out for these articles: 12 428 articles were excluded and 190 duplicate articles were removed. An additional 55 articles were obtained from reference lists of key reviews and hand-searched articles. Following title screening, 360 abstracts were reviewed against inclusion and exclusion criteria and 301 abstracts were found to be irrelevant. Thus 59 relevant articles were included for a full review, analysis and synthesis (Fig1).
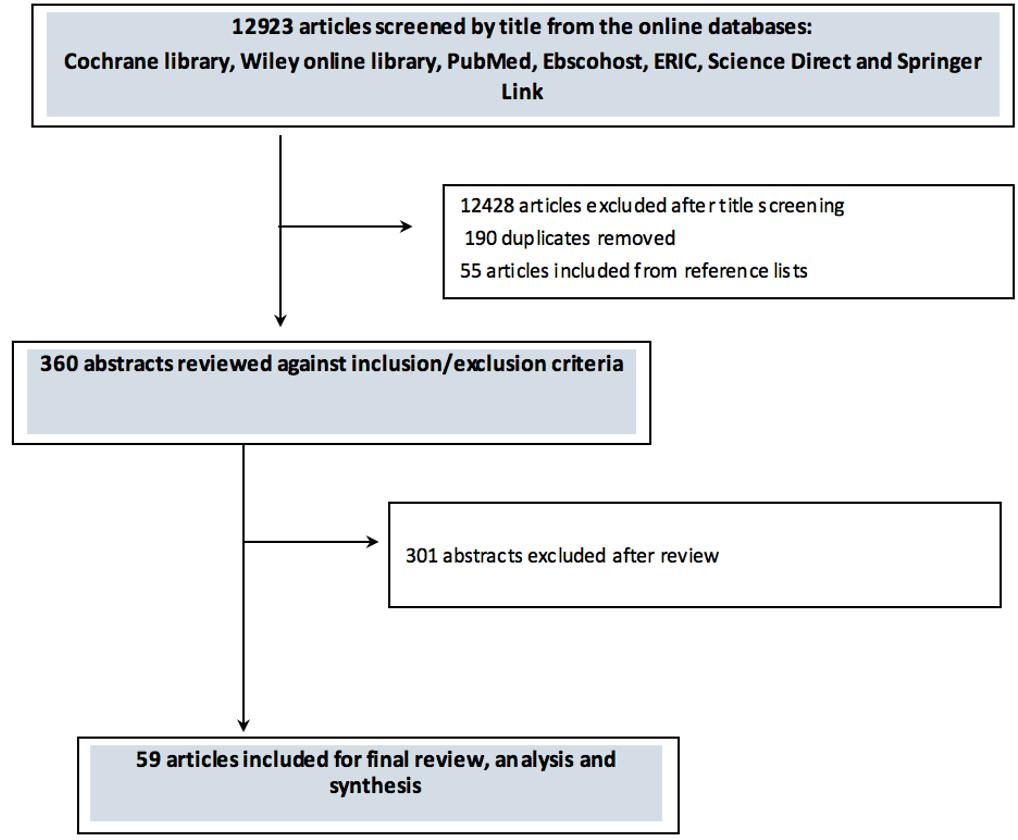 Figure 1: Article selection process for review of existing models of decentralized training platforms within medical education.
Figure 1: Article selection process for review of existing models of decentralized training platforms within medical education.
Characteristics of studies included in the scoping review
The publication dates of articles retrieved in this scoping review ranged from 1987 to 2015, with the largest group of studies falling in the period 2011–2015 (47.5%). Most of the studies were conducted in Australia (25.4%) followed by the USA (16.9%) and South Africa (16.9%). Studies mostly employed quantitative (32.2%) and qualitative methods (20.3%) only (Table 2).
The contents of the retrieved articles covered three broad themes in relation to the scoping review research question. The results for each of the 59 articles are charted according to these themes:
- DTP strategies for transforming medical education
- DTP impact on academic, service and social learning
- Models of DTP within medical education.
Table 2: Publication period, country and methodology for review of existing models of decentralized training platforms within medical education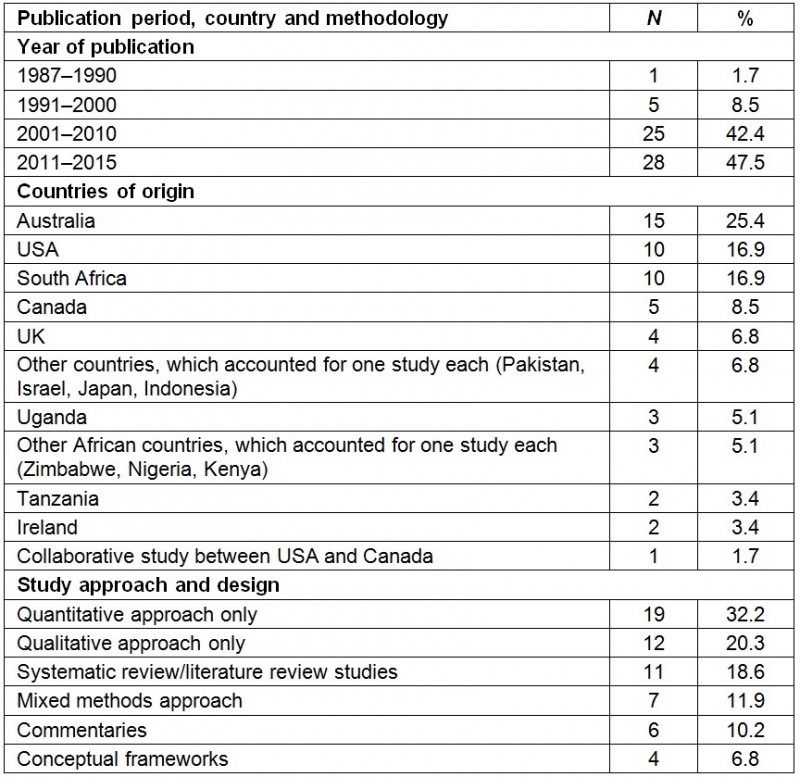
DTP strategies for transforming medical education
Thirty-one studies explored the necessary approaches for transforming medical education and they recommended the following elements as being of strategic importance in the use of decentralized training platforms.
Rural workforce training: Fourteen studies discussed the training of rural workforce as a viable strategy for addressing medical education transformation. Murray et al. recommended policy interventions that address rural medical workforce needs such as funding provision for rural scholarships purposes, creation of ‘rural clinical school campuses and regionally based medical schools’, encouraging the selection of students from rural areas, and establishment of ‘rural-health clubs’ at universities for students to create interest in rural health17. Similarly, other studies highlighted selection criteria in favour of students from underserved areas as being vital for increasing a medical workforce that is relevant to the context16,24-29.
Strategies for increasing rural origin enrolments in medical schools include having educational initiatives for both high schools and universities (through outreach programs), providing science and health programs during school vacations, funding scholarships for rural education and reviewing admission process30. Recommendations for raising rural physician numbers include increasing rural undergraduate and postgraduate training, acknowledging that the selection of location of practice depends on ‘personal and professional preferences’, financial and community factors, policy change on admission requirements and involvement of rural physicians in education provision31. Exposure to rural training equips students with enough experience to address context specific problems32-35. A review study also showed that rural medical school programs can address the health systems’ need for increasing the rural workforce34.
Context specific competencies and social accountability: Five studies highlighted the importance of developing context specific competencies as a way of promoting social accountability. Transformative learning in medical schools cannot be separated from social accountability, and a community consultative process is important for assessing the rural training of health professionals36. Having a social accountability mandate for the institution provides opportunities for community engagement that strategically contribute to the successful learning experiences of students at rural clinical schools37. Emphasis is placed on the need for capacitating educators to be change agents by encouraging peer mentoring, supporting innovations and providing educational scholarships38. Peer mentoring is necessary for augmenting learning and fostering leadership among students39. The 2010 Lancet Commission report on health professions education also highlighted a need for system based education in the 21st century that fosters adaptation of professional competencies that are specific to the rural context2. This report favoured DTPs that are located closer to rural communities, and the recruitment of rural origin students.
Community based education and community engagement: Six studies discussed community based education as an approach for strengthening and transforming medical education, suggesting that even in low resource countries it is possible for student learning to be enhanced in a context specific environment. Two studies reported that regardless of factors that affect the implementation, community based education continues to provide a viable alternative for educating health professionals in the 21st century40,41. One study provided recommendations for community oriented primary care, which emphasized community involvement, health services integration, community workers’ involvement and departmental involvement42. Teal et al proposed the engagement of community based provider organizations in early start-up and implementation to promote effectiveness and to inform policy decisions at community level43. Community engagement in planning the curriculum is also seen as a necessary requirement for transforming medical education16. Another study recommended using information and communication technologies (ICT) to foster community engaged scholarships44.
Medical education partnerships: Four studies focused on partnerships as a way of improving medical education in decentralized training platforms. Educational partnerships such as the Medical Education Partnership Initiative (MEPI), a US-funded program to support the development of medical education in Africa, have the potential to support DTPs. One MEPI-funded project facilitated the participation of medical students in rural rotations, and improvements were found in community based training45. Overall, the MEPI program was seen to contribute by producing graduates that are fit for purpose46. Collaborations and lesson sharing among medical schools increases accountability to the health system47. A symbiotic approach is encouraged for relationship building between academic institutions and health services17.
DTP impact on academic, service and social learning
Thirty-two studies highlighted students’ perceptions and experiences of training and practicing on rural decentralized training platforms.
Medical students’ experiences and perceptions of training and practicing on a rural platform: Varying views were found from several studies regarding the link between training and practicing on a rural platform. Three studies highlighted that although students had positive perceptions of rural physician expertise and the services they provide, there was no positive correlation between rural exposure, being of rural origin and having an interest in rural practice28,35,48.
On the other hand, eight studies revealed a positive correlation between rural exposure, rural origin and having interest in rural practice. For instance, some studies found that medical students had an interest in rural practice because of their rural attachment experiences32,49. Other studies found greater interest in rural practice following exposure to a rural clinical school50-53. Two studies highlighted positive experiences of rural placements among students, which included acquisition of relevant clinical skills for service provision54,55. Three studies found that students preferred longer placements in rural clinical schools because of patient-centeredness56-58.
Other studies have indicated that choosing a rural practice location is influenced by personal needs such as wanting to be near family or being in a familiar town and spouse needs59,60. Rural preceptorship was found to have an influence on specialty selection61,62.
Varying views on learning spaces were also found. Widyandana et al showed that primary health care is recommended by medical students as the best place to learn clinical skills63, whilst it was also found that district general hospitals were more preferred than tertiary hospitals64. The high preference for district general hospitals by students and the teaching staff is due to their ability to provide longer patient exposure, which leads to improvement in patient care65,66. Daly et al highlighted the learning spaces that occur within rural placements, such as learning about personal roles, experience environment and connection between students and learning spaces67.
DTP impact on community and rural practice: Five studies showed the impact of training and practicing on a rural platform. One study showed that exposure to rural or regional postgraduate training provides postgraduate students with good learning experiences30. Bicket et al found that motivators for students’ engagement were linked to their need to contribute to the community68. Students were empowered by responsibility and clearly defined roles, allowing them to have meaningful connection with others68. Training on a rural platform provided students with an understanding of health care and how it is delivered in the community69. A study on students’ experiences of innovative rural education found benefits of rural clinical schools came about because they contribute to the development of leadership qualities and that students acknowledged their role as a healer when they worked with patients36. Community based education has been found to have a great impact on communities and student engagement in community work. Short term benefits included improvement of services, decreased referrals, home visits, provision of primary healthcare services that are community oriented, communication improvement and professionalism70. Long term benefits included improved teaching and familiarity with the healthcare system and student engagement in community work70.
Three studies explored the unique learning opportunities that are provided by DTPs. Daly et al highlighted that because cultural awareness is supported, students are better prepared to practice in a particular context71. Another study concurred that learning takes place at the level of both clinical skills and ‘personal and professional development’72. Jinadu et al indicated that because the learning is more experiential, primary healthcare education seems to provide better learning to graduates compared to the ‘traditional medical schools’73.
Models of DTPs within medical education
This scoping review offers a variety of models for DTPs within medical education (Table 3). It reflects that rural clinical schools mostly use longitudinal integrated clerkships, whereby students are placed in a district hospital or general practice for extended periods, most often being of 1 years’ duration33,35,36,39,57,58,71,74. Rural clinical school training also includes offering training in a rural site, recruiting students from rural areas and having repeated rural exposure49. Some models of DTPs include distributed community engaged learning, which takes place in both community and classroom settings. This includes having multiple short term placements in communities, with classroom based reflection and learning interspersed between them37. Many community based education models range from 4- to 8-week placements, involving students spending time in community health centers and rural communities41,45,69,73.
Some studies describe a mix of three clinical practice placements such as general practice placements (2–4 sessions per week), hospital placements and remote placements (4-week placements in a remote area) during the third, fourth and fifth year of study64,66,71,75. Other placement models include urban medical schools having rural clinical placements over 6 weeks in primary healthcare settings8.
Doherty highlights varying models for rural training of health professionals33. These include comprehensive rural programs with curricula that are more focused on issues affecting rural communities, dedicated rural track programs within urban based institutions with lengthy placements in a rural environment, rural tracks that are offered as part of traditional programs, and supplementary rural tracks whereby students participate in a rural placement as an additional activity.
Table 3: DTP models with medical education identified by review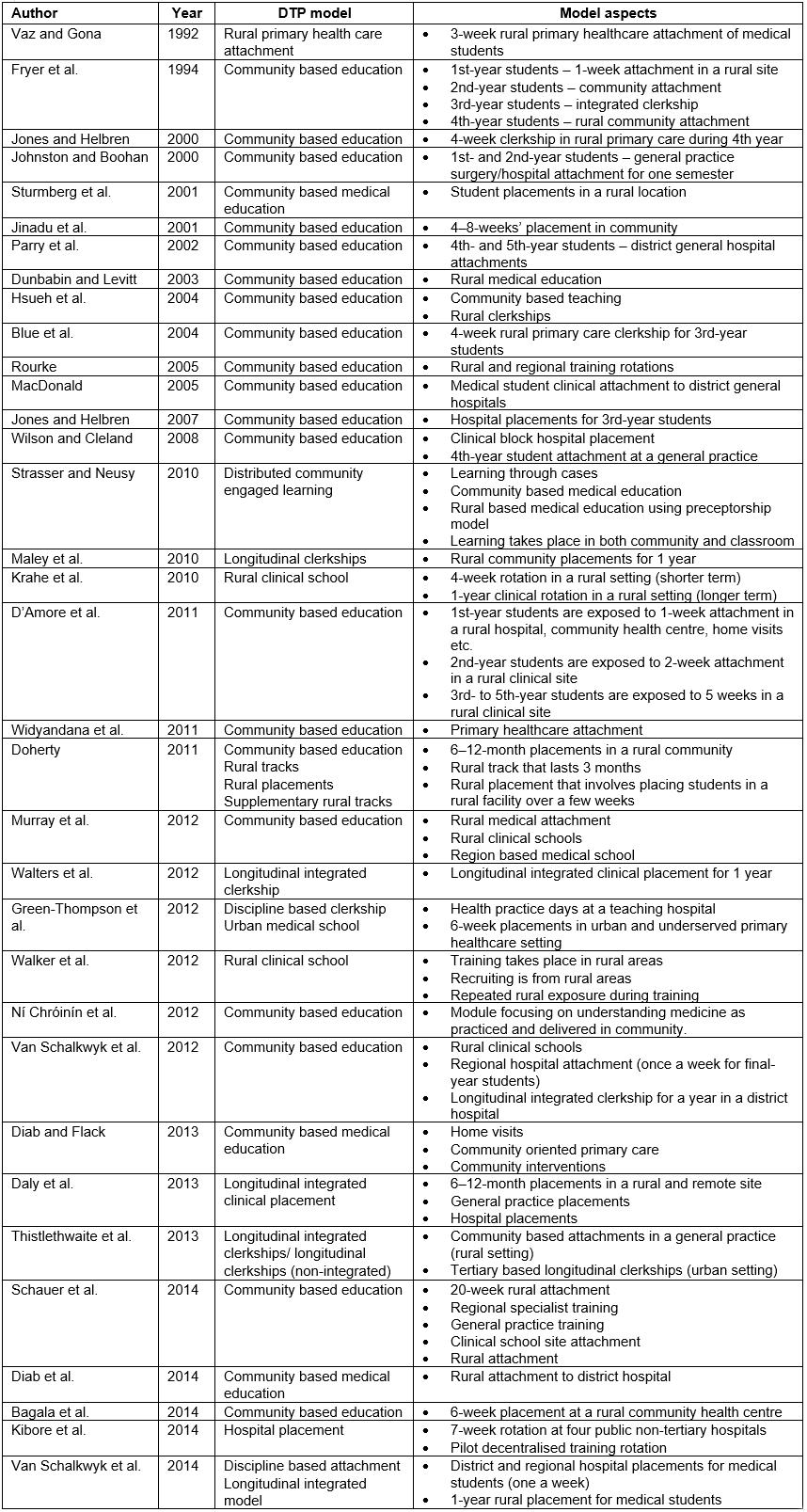
Discussion
This scoping review offers vital strategies for improving medical education. It supports the utilization of DTPs as a feasible option for providing learning that is relevant to the context, and the impact of DTPs on academic, service and social learning is noted.
The review highlights four aspects of DTP strategies that are crucial for medical education transformation. These include rural workforce training, development of context specific competencies for raising social accountability, support for community based education and community engagement, and formation of partnerships amongst key role-players. Rural workforce training is more feasible through community based education, which, being rooted in context, is focused on addressing the realities of the population to be served. The utilization of the community as a learning platform offers students an opportunity to gain personal and professional attributes such as leadership skills, an understanding of their roles as healers, better insight into health care and enhanced cultural experience69,71,74. When students are exposed to and engaged in leadership roles within a community, benefits accrue to both the parties involved68. Communities in which students undertake learning contribute to the educational environment and facilitate the interaction of students with the community. This complements Talaat and Ladhani‘s contemporary definition of community-based education, which highlights that it ‘is about the facilitation of learning in, with, for, and from the community, rendering relevant, meaningful and mutually agreed upon learning outcomes for health professionals and services to the populations in a community setting’ (p.11)76.
Decentralized placements create space for students to build self-confidence and develop competencies that assist in preparing them for practice. However, the responsibility to make the most of available opportunities requires that students have the skills to make this link. In line with Maley et al39, this review submits that a framework for a successful community of rural educational practice is one that incorporates leadership skills development for the members, embraces a ‘community of practice’ for governance, adopts internal benchmarking strategies, supports critical reflection and encourages mentoring that is both vertical and horizontal. Critical to the success of this framework is the identification of the range of stakeholders who are likely to contribute to a sustained relationship and are capable of directly influencing community based education. Ultimately, these structures should engage fully with the health system40.
The necessary adaptations needed for transformation of medical education include changing ways of selecting students16,24-29, reviewing training locations16,77, engaging communities37,44, designing interventions for rural workforce16, dealing with context specific competencies38, introducing rural scholarship programs and introducing system based education2. Many strategies have been applied to implement these adaptations. Some Canadian and US medical schools, as part of their rural scholarship programs, have introducted ’community engaged scholarships’ that assist in building participatory partnerships between communities and medical schools where communities are involved throughout the scholarship process44.
The review revealed a wide range of DTP models for medical education transformation, which are described in the results. There is a wide variety of options for DTPs, and medical schools choose amongst these in relation to context, aims and resources. It is apparent however that many of the most effective DTP models are situated in rural contexts and that rural medical educators are responsible for a significant proportion of the available literature on DTPs. This may be both because the rural context provides a unique opportunity for hands-on clinical practice and engagement with communities, and because rural academics have often taken the lead in clinical educational innovation. These DTP models show the impact that decentralized training has on students through community health service provision; the extent of the impact of this training on the communities served is less documented, and would be a valuable avenue for further research.
Although most studies in this review suggested a positive attitude towards decentralized training and rural practice amongst students, there were conflicting views about whether being of rural origin contributes to having such interest or not28,34,35,48. There is a need for further research to explore other factors that might contribute to interest in rural health training and provision of health services in a rural context. There is also a need to explore whether there is any cross-over value between training in rural or other underserved areas; in other words, does decentralized training in any context lead to greater commitment of students and graduates to service in rural and underserved communities, or is the outcome specific to context and/or sociodemographics?
Conclusions
This scoping review shows that there is considerable literature on DTPs that provides justification for implementing such adaptations as part of transforming medical education. It is clear that DTPs have demonstrated the capacity for realizing academic, service and social learning agendas, depending on the strategies adopted. Various models of DTPs provide options for developing context specific competencies that respond to the health needs of the population. Partnerships between communities and academic institutions are essential for the success of a functional DTP model in the 21st century.
Acknowledgements
The authors would like to acknowledge the following people who assisted with literature search and management of references: Ms Mamonyooe Ramahlele, Mr. Papikie Makhuba, Ms Mapula Adams, Ms Thandokazi Maseti and Ms Samantha Dube. We are grateful to have received funding for the larger study from the South African National Research Foundation and MEPI.