Introduction
The aging of the baby boomers has made caregiving an increasingly relevant topic for individuals, families, care providers, and policymakers. In 2012, 43.1 million US adults, 13.7% of the population, were aged 65 years and older. By 2050, that number is expected to grow to 83.7 million, or a quarter of the US population1. At least 70% of these adults will need long-term care, but the cost of care can be prohibitive, leaving an unmet need2,3. These changing population demographics predict the growing need for caregivers.
Assistance needs of adults are often fully or partially met by family members and friends working as unpaid caregivers4. The value of caregiving is significant: in 2009, the estimated economic value of unpaid caregivers was $450 billion5. These workers serve as both care coordinators and service providers and face physical, emotional, and financial strains. The rapid increase in unpaid caregivers will only continue as the population continues to age6,7. The burden on unpaid caregivers is evident: national studies examining the prevalence of caregiving have found that caregivers are more likely to self-report poorer health, mental stress, and dissatisfaction with life compared to non-caregivers4,8. The use of supportive services among caregivers is low, with only one in four caregivers receiving these services9. Availability of support services may differ by rurality. Thus, rural caregivers may differ from their urban counterparts.
Theoretical frameworks are instructive for positing why rural caregivers may differ from their urban counterparts. The scarcity hypothesis of role theory asserts that when people do not have enough resources to support the obligations of multiple roles and commitments, there will be role strain and role conflicts10,11. These constraints subsequently contribute to a lack of choice in caregiving. The lifespan theory of control supports this idea, positing that the absence of choice leads to negative feelings due to loss of control12,13. The ability to have choices has been linked to better behavioral and psychological outcomes14,15. Lack of choice in caregiving has been found to be associated with higher levels of emotional and physical strain16. Higher levels of caregiver burden which may be due to lack of choice or scarce resources have been shown to negatively affect both the physical and mental health of the caregiver17-21. This may be especially true for rural individuals, who often live in tighter-knit communities than individuals living in urban settings. These rural communities may provide additional support, but may also foster a sense of obligation and thus a lack of choice in taking on the caregiver role22. Beyond social obligation, the lower availability of caregiving supports such as home health contributes to lack of choice.
Rural caregivers face a multitude of barriers and resource gaps that their urban counterparts may not face such as distance and lack of transportation, heavily burdened service agencies, healthcare provider shortages, and other access issues23. These time, financial, physical, and emotional constraints will only exacerbate the strain of caregiving24. Previous research on the role of residence in caregiving has yielded mixed descriptions of the characteristics and burden of rural caregivers. Of the differences found, many were modest and explained by caregiver or care recipient characteristics such as age, gender, and employment25. Dwyer and Miller (1990)26 found that rural caregivers had the highest stress levels but the lowest levels of burden, while others27 found that caregivers who live in more densely populated areas were more likely to experience a poorer quality of life and greater levels of burden. Additional studies found no evidence that residence mattered for the depressive symptoms of a caregiver28,29. Much of the research on rural–urban caregiving has been limited to very small sample sizes within a particular geographic region (limiting the interpretation of the results) or has not included an operational definition of ‘rural’25,29.
Differences in caregiver experience associated with residence have yet to be investigated using a national sample. Previous national studies have characterized the sociodemographics and health of informal caregivers with little attention to residence16. The present study aims to profile rural and urban caregivers and to examine whether rural–urban differences exist in self-reported caregiver health, and emotional, financial, and physical strain among unpaid caregivers of adults.
Methods
A cross-sectional analysis was conducted of publicly available data from 'Caregiving in the U.S. 2015', a survey fielded jointly by the National Alliance for Caregiving (NAC) and AARP. The survey was conducted to estimate the prevalence of caregiving for someone of any age within the USA, as well as to describe the characteristics of caregivers of an adult30. The survey used the GFK Knowledge Panel, a probability-based online panel, designed to represent the US population. Selected households were invited by telephone or mail to participate and given use of a computer and internet connection if needed. The online questionnaire was first used to screen for the presence of any caregiver in order to measure prevalence of caregiving. The main portion of the online interview asked questions of all unpaid caregivers of adult recipients identified by the question, 'At any time in the last 12 months, has anyone in your household provided unpaid care to a relative or friend 18 years or older to help them take care of themselves?' Interviews were conducted in the autumn of 201430.
The total sample included a base study sample size of 1248 caregivers of adults with completed full online interviews. The 1248 full online interviews comprised 698 non-Hispanic White, 206 non-Hispanic African-American, 208 Hispanic, 95 Asian-American, and 41 'other' caregiver interviewees. Additional groups were oversampled: caregivers aged 65–74 years (total n=213), caregivers aged 75 years or older (total n=269), and additional Asian-American caregivers (total n=201). This added 683 caregivers to the base sample of 1248 caregivers. Population weights were applied using a single-stage weighting procedure by age, sex, and race/ethnicity from the public-use data file of the March 2014 'Current Population Survey' to correct for the oversampling described. Weighting brought the final weighted sample for the study down to 1352 caregiver observations, with a margin of error of 2.8 percentage points at the 95% confidence level30.
Dependent variables
The principal dependent variables were physical strain, financial strain, emotional stress, and caregiver health. To determine self-reported level of physical strain, the questionnaire asked how much of a physical strain caring for recipient is/was. For financial strain, the questionnaire asked how much of a financial strain caring for recipient is/was. Self-reported levels of difficulty for physical and financial strain ranged from 1 (‘no strain at all’) to 5 (‘very much strain’). For emotional strain, the questionnaire asked how emotionally stressful caring for recipient is/was. Measures of emotional stress were self-reported between 1 (‘not stressful at all’) and 5 (‘very stressful’). Levels of strain and stress were collapsed into two categories: levels 3–5 (moderate to high strain/moderate stress to very stressful) versus caregivers who rated their emotional strain caring for a recipient as level 1 or 2 (low strain/low stress). For caregiver health, caregivers were asked, 'How would you describe your own health?'; reported levels of health were 1 (‘poor’), 2 (‘fair’), 3 (‘good’), 4 (‘very good’) and 5 (‘excellent’). Caregiver health was then collapsed into two categories: health status rated as poor to fair, and health status rated as good, very good, or excellent.
Independent variables
The principal independent variables were residence and caregiver burden. Residence was determined by asking whether the caregiver lived in a rural area. While respondent perceptions may not perfectly overlap with other measures of rurality, they do reflect evaluation of environment. The level of burden index, prepopulated and calculated by AARP and NAC, assigned points based on the number of hours providing care (0–8 hours=1 point, 9–20 hours=2 points, 21–40 hours=3 points, >40 hours=4 points) as well as the number of activities of daily living (ADLs) and instrumental activities of daily living (IADLS) performed for the recipient (0 ADLs with 1 IADL=1 point, 0 ADLS with ≥2 IADLs=2 points, 1 ADL with any number of IADLS=3 points, ≥2 ADLs with any number of IADLs=4 points). Five levels of burden were constructed from these points. These levels ranged from 1, with no ADLs and few hours of care, to 5, with at least two ADLs and more than 40 hours of care per week. Levels of burden were further divided into three categories: low (levels 1 and 2), medium (level 3), and high burden (levels 4 and 5). The categories of low, medium, and high burden was used for this analysis.
Covariates
Additional covariates included the sociodemographic characteristics of the caregivers: age, sex, race, educational attainment, employment, and income. Age was measured using three categories: 18–49, 50–64, and ≥65 years. Race was self-reported and grouped into two categories: ‘non-Hispanic White’ and ‘other’. While it would be desirable to examine the experience of specific race/ethnicity populations, the number of rural respondents was too few for accurate estimation (18 African-American respondents). Educational attainment included three categories: ‘less than or equal to high school graduate/GED [General Equivalency Diploma]’, ‘some college/technical school’, and ‘college graduate or above’. Employment was defined as whether the caregiver was employed at any time during the past year. Income was measured using three categories: ≤US$29,999, US$30,000–74,999, and ≥US$75,000.
Statistical analysis
Standard statistical analysis procedures were used to estimate frequencies and proportions for categorical variables. Bivariate analyses were carried out to detect statistical significance between variables using χ2 with α = 0.05. As sociodemographic characteristics may also affect caregiver strain and burden, multivariable regression models were used to examine the impact of caregivers’ characteristics and level of burden on overall caregiver health, physical strain, financial strain, and emotional stress, adjusting for covariates. All analyses were conducted with Statistical Analysis Software v9.3 (SAS, http://www.sas.com) using survey sampling weights that account for the sampling strategy used by the study.
Ethics approval
The data that were examined in this study are publicly available and do not contain individual identifiers; the study was approved by the University of South Carolina’s institutional review board as exempt.
Results
In the total sample, the majority of caregivers were female (59.0%), aged less than 65 years (81.5%), and resided in an urban location (84.4%; Table 1). Compared to urban caregivers, a larger proportion of rural caregivers were non-Hispanic White (p=0.002). Rural caregivers reported lower socioeconomic status than urban caregivers as measured by income, education, and employment. Rural caregivers reported lower incomes than urban caregivers, with 75% of rural caregivers reporting an annual income of less than US$75,000 compared to 61% of urban caregivers (p=0.003). Rural caregivers were less likely than their urban counterparts to have a college degree or greater (27% vs 41%, p=0.003). Finally, rural caregivers were less likely to be employed than urban caregivers (63% vs 51%, p=0.0018).
Rural–urban differences were not found in the relationship of the caregiver to the recipient, level of burden, and whether the caretaker had a choice in taking on the role of caregiving. The use of respite care also did not differ by residence (Table 1). In unadjusted analysis, rural residents did not differ from their urban peers in self-reported health or the physical, financial or emotional stress associated with caregiving (Table 2). Overall, 16.4% of respondents reported poor health. Moderate to high physical strain was reported by 46.0% of respondents, and similar financial strain by 38.7%. The emotional burden was higher, with 63.4% of respondents reporting moderate to high emotional stress.
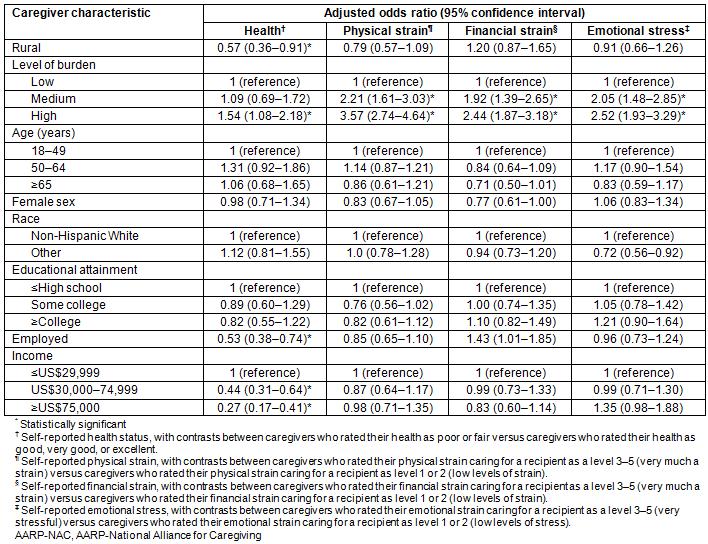
In multivariable analysis adjusting for age, race, educational attainment, and reported caregiver burden, residence was associated with self-reported health status of the caregiver but not with physical, financial or emotional distress (Table 3). The odds of rural caregivers reporting poor to fair health were significantly lower than their urban counterparts (adjusted odds ratio (OR) 0.57; 95% confidence interval (CI), 0.36–0.91). Other factors associated with fair/poor health included caregiver burden, employment status, and income. Caregivers with a high level of burden were more likely to report poor to fair health (adjusted OR 1.54; 95%CI, 1.08–2.18). Employed caregivers had lower odds of fair to poor health than caregivers who were not employed (adjusted OR 0.53; 95%CI, 0.38–0.74). Finally, the odds of self-reported fair/poor health declined with income.
The only variable consistently associated with physical, financial or emotional stress was caregiver burden (Table 3). Caregivers with high levels of caregiving burden were more likely to experience financial strain (adjusted OR 2.44; 95%CI, 1.87–3.18), emotional strain (adjusted OR 2.52; 95%CI, 1.93–3.29), and physical strain (adjusted OR 3.57; 95%CI, 2.74–4.64).
Table 1: Characteristics of caregivers, AARP-NAC survey, 2014, by residence
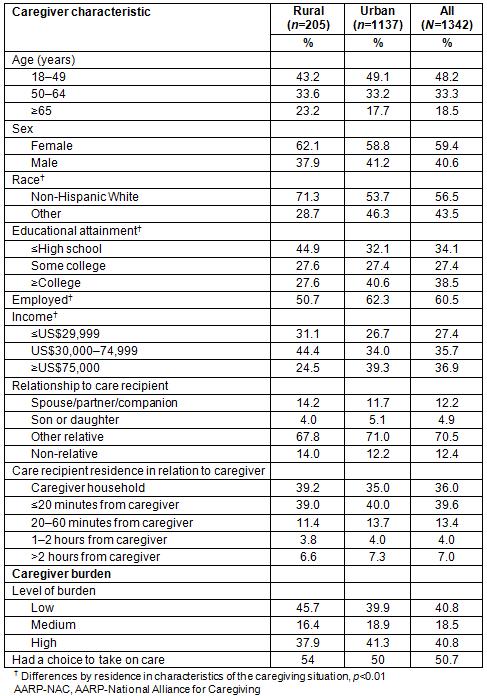
Table 2: Caregiving-related effects, AARP–NAC survey, 2014
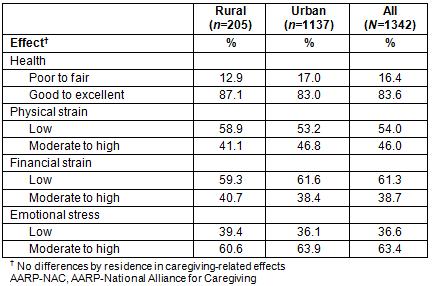
Table 3. Factors associated with caregiving-related effects, AARP–NAC survey, 2014
Discussion
The present article offers the first national examination of rural caregivers. Previous research on caregivers has not explored differences by residence (eg Trivedi, et al8), while rural research has been limited to small sample sizes and narrow geographic regions (eg Goins, Spencer, and Byrd31). While self-determined definition of ‘rural’ is a limitation of the study, the present findings contribute important insight into the burden level of rural caregivers nationally.
The demographic profiles of rural and urban caregivers differed, with rural caregivers containing proportionately more non-Hispanic White than minority persons. Other differences, including lower rates of employment, lower education, and lower income, all associated with fewer resources, suggest a greater likelihood of caregiver strain.
Surprisingly, only self-reported health was linked to rural residence, which may have had a protective effect in multivariable analysis. The finding of no difference in burden between rural and urban caregivers parallels similar findings in a Canadian population32. Differing cultural values, such as an emphasis on family and familial relationships, in rural caregivers may affect their self-perceived health status. Rural caregivers often feel believe that family members should be responsible for care33. Surveys of rural caregivers have found that many report satisfaction and find motivation in their caregiving role34. Additionally, caregivers may become used to their current situation and not realize the emotional or physical strain of caregiving, thus under-reporting may be an issue35.
The present study confirms the work of previous research that indicated that caregivers with higher levels of burden were more likely to report physical, emotional and financial strain36,37. The findings also confirm the known relationship between income and health38; as income levels increased, caregivers were less likely to report their health as poor or fair. These caregivers may be able to afford more support services and provide fewer caregiving hours, lessening their burden.
These findings highlight the importance of understanding the characteristics and needs of rural caregivers, which can help policymakers target services and interventions to better assist these individuals. Rural caregivers are generally poorer, with significant financial and geographic barriers to support services23. While the present study shows that rural caregivers may not exceed urban caregivers in the burden of caregiving or their need for support services, this type of informal caregiving may be more needed in rural areas due to resource constraints. Beyond social support services, rural areas face significant shortages of healthcare workers such as pharmacists and family medicine physicians, who usually help with care coordination services39. Innovative interventions such as internet-based interventions have improved information delivery and social support for family caregivers40. The use of telecommunication is one tool for increasing access for rural caregivers and their recipients41,42. However, the limited availability of internet access in rural areas may limit the feasibility of technology-based interventions for many rural caregivers. Telephone-based interventions may work better for rural caregivers43.
Several limitations to the research presented here should be noted. The use of publicly available data limits flexibility in the research design. First, as noted earlier, the definition of 'rural' is self-selected and reflects respondent perspectives rather than a standard geographic measure. Second, the rural–urban distinction pertains to the caregiver, not the recipient of care. The survey was conducted by telephone using landlines, and thus may have under-represented younger caregivers. All information provided is self-reported and thus reflects respondent perspectives. Finally, caregiver burden was measured objectively, by number of hours per week spent caregiving and number of activities of daily living. Caregiver burden measured through subjective appraisal, where the caregiver believes they are unable to contend with all of the demands required, may have also been instructive for this study.
Despite limitations, the findings provide cause for concern for the future need of caregiving. Caregivers with lower incomes were more likely report poor or fair health, yet there is limited public financing to support family caregiving interventions (Table 3). Continued funding of federal initiatives for family caregivers such as the Older Americans Act, the National Family Caregiver Support Program, and the Lifespan Respite Program are critical for easing the caregiving burden42. One program within the Patient Protection and Affordable Care Act (which was subsequently repealed) was the Community Living Assistance Services and Supports (CLASS) Act, which would have created a national voluntary long-term care insurance program administered by the federal government. This Act would have assisted care recipients and their caregivers through a cash benefit to hire and train family caregivers. Use of this could lead to fewer unmet needs and greater consumer and family satisfaction, and future policies that emulate this program would be beneficial44. Consumer-directed models such as this may be particularly helpful for rural caregivers, who may require different types of support and services than their urban counterparts45. The AARP Public Policy Institute suggests several new policy initiatives to address the current and future needs of caregivers such as, but not limited to, reimbursing caregivers through Medicare and Medicaid, increasing the reach of the Family and Medical Leave Act, and adopting policies to prohibit discrimination of workers with caregiving responsibilities46.
Conclusions
The present research highlights the need for additional national studies with a larger sample of rural caregivers. Out of the 1342 respondents, only 205 respondents were rural. Thus, the sample of rural caregivers was too small to examine regional or race effects of caregiving in rural areas. This illustrates the need to target certain areas or particular demographics of rural America. Measures of formal and informal support systems, beyond traditional respite care, may be instructive to garner a more thorough picture of the level of assistance available to rural caregivers.


