Introduction
Chronic heart failure (CHF) has reached epidemic proportions in Australia1. Typically CHF develops in frail elderly individuals who have suffered an acute or sustained insult to the structural efficiency of the heart due to the presence of underlying heart disease and/or hypertension2. However, it is also more common in individuals with disproportionately high levels of cardiac disease or its risk factors (eg lower socio economic status)3. As such, this epidemic is particularly significant for older people, males and Aboriginal people, groups who comprise a greater proportion of the population in rural and remote Australia4,5. Recent evidence suggests that mortality from CHF increases with increasing geographical remoteness. Rates are reported to be between 20% and 50% higher in rural areas compared with major cities6. Any attempt to quantify CHF in Australia must account for the overall poor cardiovascular health of Indigenous Australians7. In Aboriginal people, CHF may occur at a much younger age and disease aetiology is more commonly related to infectious or environmental causes (rheumatic disease, hypertension and atherosclerosis)7. Aboriginal people are also less likely to contribute to the CHF population over 65 years due to their reduced life expectancy compared with non-Indigenous Australians. In 2001, the life expectancy of male and female Aboriginal people was 56 years and 63 years, respectively. This compares unfavourably with the non-Indigenous population who can expect to live 76 years (males) and 82 years (females)7. Although no comprehensive data of CHF prevalence in Indigenous populations has been published, mortality statistics indicate that death rates from CHF in Aboriginal populations are three times higher than those of non-Indigenous populations, suggesting that prevalence rates are also likely to be much higher7.
Despite national recognition that CHF is a significant health issue8 there is a paucity of reliable information quantifying the dimensions of the problem. Data from national records such as The Australian Bureau of Statistics (ABS) census, the Health Insurance Commission discharge records, and Medicare prescription records do not provide an accurate measure of the problem due to under-recording of new cases or misdiagnoses where symptoms are masked by disease co-morbidity such as diabetes, chronic airways disease, hypertension, alcoholic diseases and chronic renal failure1. Inaccuracies in ABS census data are further compounded by the self-reporting nature of surveys that, in a disease under-recognised within the medical community, is even less likely to be accurately reported among the general population9.
Currently the prevalence of CHF in Australia is unknown. Therefore the main aim of this study was to determine if potential rates of CHF differ between urban and rural parts of Australia. The significance of the study is two-fold: first, little is known about the prevalence of CHF; and second, the increased risk of CHF in non-urban areas and among Aboriginal populations has important implications for service planning and for secondary prevention.
Methods
The methods used for this study were adapted from a previously described model to determine the burden and distribution of CHF in Australia on a state-by-state basis1. In contrast to our original report, these updated data are derived directly from the exact statistics of the 2001 ABS Census as opposed to an extrapolation of 1996 ABS Census data for the year 2000. Moreover, we have addressed one of the main limitations of our original analysis: weighting for the effects of Australia Indigenous population who have very poor rates of cardiovascular health including CHF, and a detailed analysis of the distribution of CHF in rural and remote communities.
The method for this study, therefore, involved using age and sex stratified data for Indigenous and non-Indigenous Australians obtained from the 2001 ABS Census Total Resident Population Figures10. Conservative age and sex stratified CHF prevalence estimates derived from international (United Kingdom, Sweden, New Zealand, and the Netherlands) well-validated data11-16, were then directly standardised to the age and sex stratified Australian population over 45 years of age in each ABS statistical subdivision (SSD). SSD is the general purpose spatial unit used by the ABS and are the largest and most stable spatial unit in each state10.
For the purposes of this study, data were grouped into three arbitrary geographical areas using SSD boundaries. These were labelled capital cities; larger urban centres (non capital cities and towns with a population > 20 000); and rural and remote regions (areas outside capital cities and large urban centres). Our CHF population prevalence estimates were then weighted to reflect the proportion of Indigenous people residing in each geographical area.
In the absence of CHF prevalence rates for Aboriginal and Torres Strait Islanders, estimates were adjusted based on CHF Aboriginal mortality data obtained from the Australian Institute of Health and Welfare17. This was considered to be a minimal starting point for the estimate of the burden of this disease7,18. The proportion of Aboriginal people in each geographical region10 was stratified by sex but not age, and weighed accordingly. The Aboriginal and non-Aboriginal estimates were then combined to derive total CHF estimates for each of the nominated areas. We have reported results as estimates of case numbers, prevalence rates, odds ratios and 95% confidence intervals.
Finally, all of the large urban centres (non-capital cities and towns with a population >20 000) in this study were allocated an Accessibility and Remoteness Index of Australia (ARIA) score19. ARIA is a geographical index that defines remoteness as accessibility to goods and services and opportunities for social interaction across Australia, based on road distance from populated towns. For each populated location, distances are converted to a continuous measure, ranging from 0 for high accessibility, to 12 for extreme remoteness. ARIA measures are grouped into 5 categories; highly accessible, accessible, moderately accessible, remote and very remote, using natural breaks in these 0 to 12 continuous variables. The ARIA values reported here are for 2001 ABS SSD.
Wherever a large urban centre comprised a range of ARIA areas a mean ARIA score has been presented. A schematic diagram of the method is presented (Fig 1).
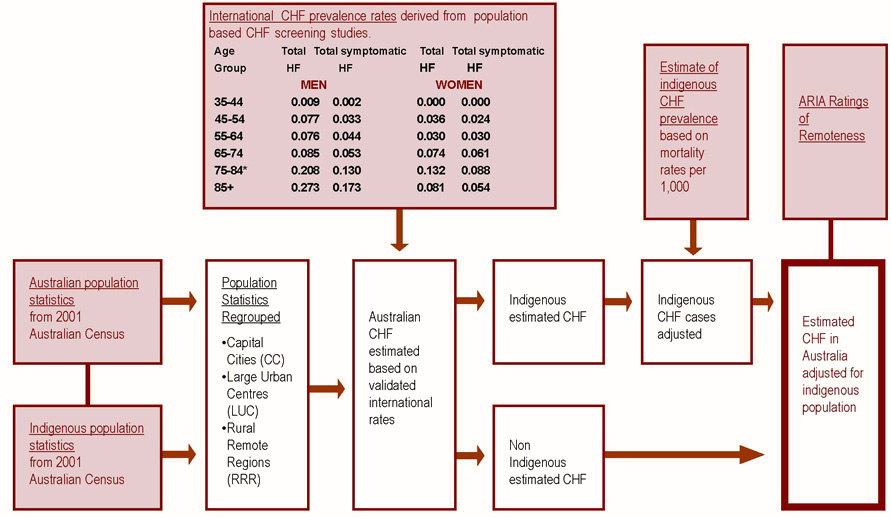
Figure 1: Method for estimating chronic heart failure cases in Australia in 2001.
Results
Estimated prevalence of chronic heart failure
Overall the estimated prevalence of CHF in Australia in 2001 was 17.87 per 1000: estimated rates ranged from 13.98 per 1000 in the Australian Capital Territory (ACT) to 29.50 per 1000 in rural Northern Territory (NT) (Fig 2). With the exception of Queensland (QLD) and Tasmania (TAS), estimated CHF prevalence rates within each State were higher in the rural and remote regions (19.84/1000) and large urban centres (19.01/1000) than in capital cities (16.94/1000). This was highly significant (OR 0.47 [95% CI 0.46 to 0.47] p <0.001). In the Australian states QLD and TAS, large urban centres had the highest estimated prevalence (18.95/1000 & 19.53/1000).
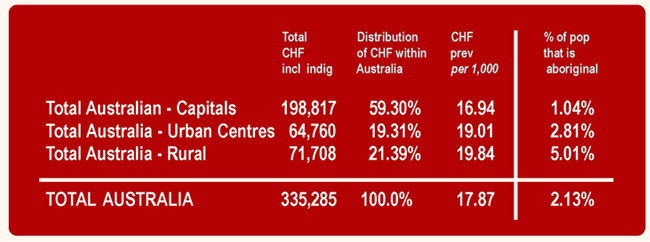
Figure 2: Estimated distribution and prevalence of chronic heart failure and percentage of Indigenous population in Australia.
Figure 3 shows that estimates of CHF prevalence rates in specific large urban centres varied even more widely: from 11.94 per 1000 in the rural cities of Kalgoorlie/Boulder to 26.02 per 1000 in Hervey Bay.
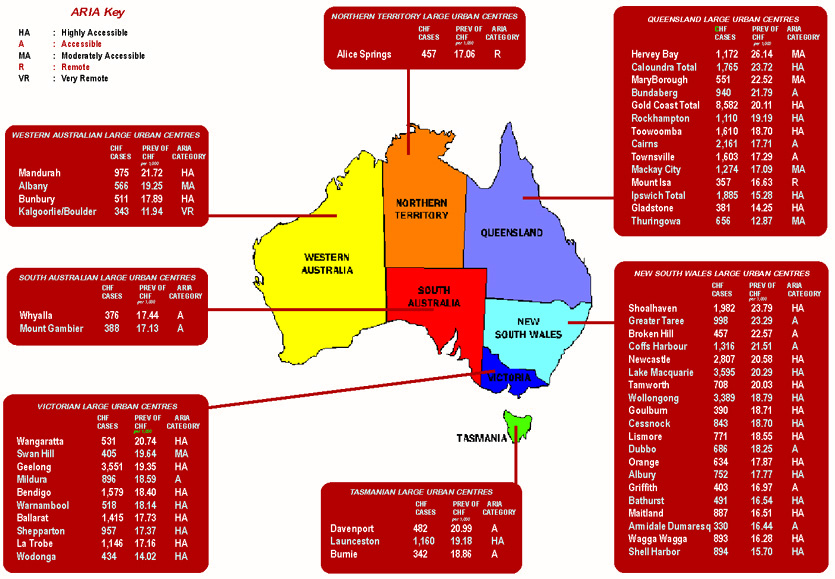
Figure 3: Estimated cases and prevalence of chronic heart failure in large urban centres.
Estimated chronic heart failure cases
In 2001 there were 335 280 estimated cases of CHF in Australia. Approximately 60% (198 817 cases) resided in capital cities, 20% (64 760 cases) lived in large urban centres and 20% (71 708 cases) in rural and remote regions (Fig 2). The larger states of New South Wales (NSW) (114 984), Victoria (VIC) (80 503) and QLD (62 754) were estimated to have more total cases of CHF than the other states. Total cases in the capital cities of these states were also larger.
Demographically, CHF affected more males (54%) than females. This sex difference diminished as age increased (ie, more males affected than females but an 'older' profile in females overall)1. Estimated CHF cases were calculated for all large urban centres in Australia, the majority of which are concentrated in the eastern states. Estimated cases of CHF in large urban centres ranged from 327 in Armidale, a rural university town, to 8522 in Gold Coast City which is a large urban centre favoured by retirees (Fig 3).
The relative spread of cases within states and territories had three distinct patterns. First of all in VIC, Western Australia (WA), South Australia (SA), and the ACT over 70% of the estimated CHF population was situated in the capital cities. Relatively few cases were located in other large urban centres (3-14%), but a higher proportion was from rural and remote regions (16-25%) (Fig 4).
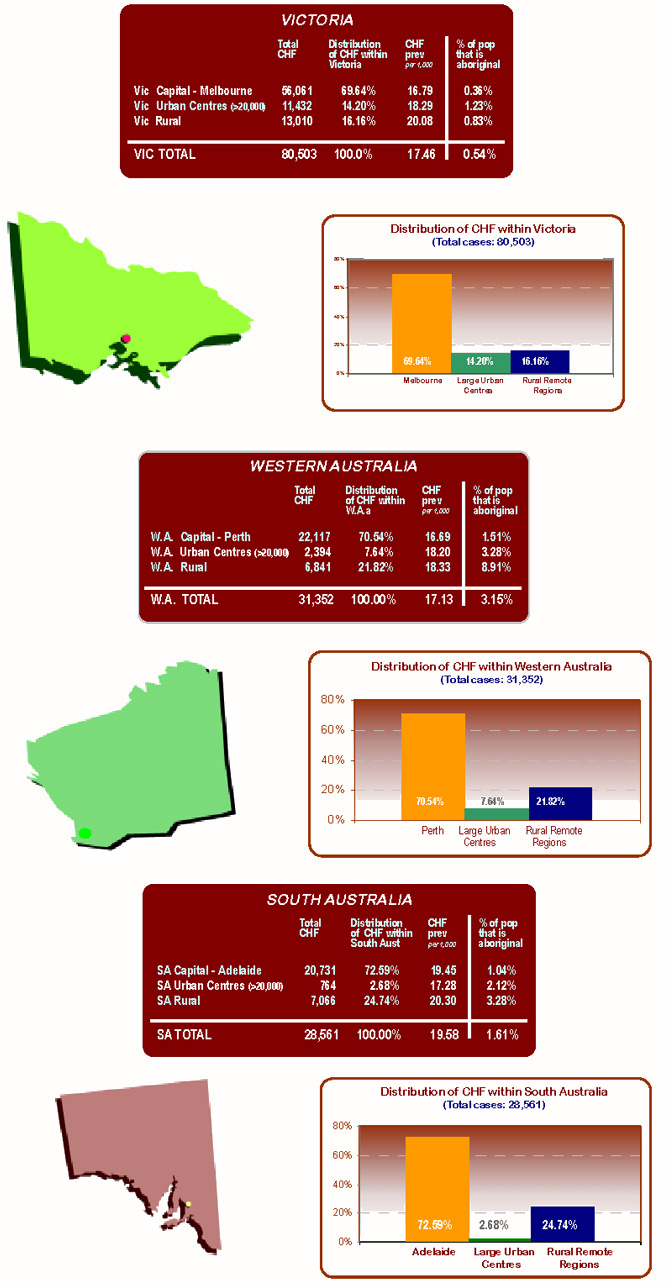
Figure 4: States and Territories with high chronic heart failure within capital cities.
In comparison, in QLD, TAS and NT, the majority of the estimated CHF patients (59-62%) lived outside the capital cities, either in rural and remote regions or large urban centres (Fig 5).
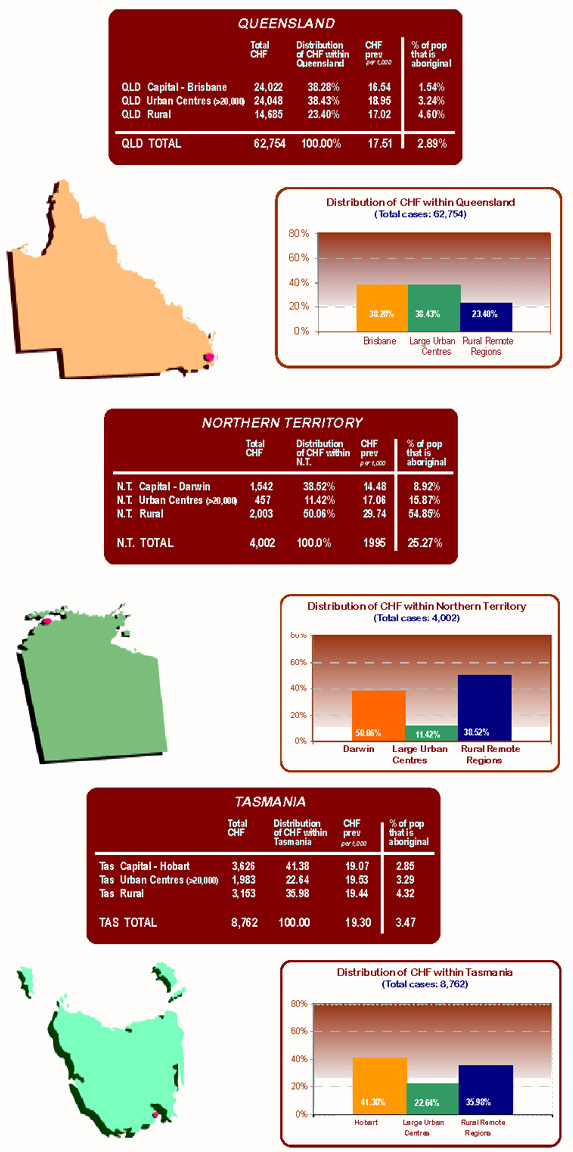
Figure 5: States and Territories with high chronic heart failure prevalence within capital cities.
The State of NSW had a unique distribution pattern. The majority of the CHF population was estimated to live in the capital Sydney (58%) and the remainder of cases were evenly distributed between large urban centres and rural and remote regions (21% each).
Accessibility of large urban centres
ARIA estimates of remoteness are presented (Fig 3). Remoteness categories for large urban centres ranged from very remote in Kalgoorlie/Boulder to highly accessible in Gold Coast City, Geelong and Mandurah. All of the cities in the State of NSW are at least accessible or highly accessible. This was in contrast to WA, NT and QLD which all contained cities with a high prevalence of CHF patients who were remote or very remote from services.
Discussion
The importance of these findings is that while a majority of CHF may occur among people living in cities (because this is where the population is centred) a disproportionate number of cases are estimated to occur among people living outside these cities. Largely a reflection of the age and socio-demographic profile of this section of the population, it is unfortunate that many of affected individuals living in rural and remote regions have little or no access to specialist CHF services.
Overall, we found a high estimated prevalence of CHF across Australia and when the data were stratified by remoteness and accessibility there were higher CHF prevalence rates outside capital cities. Our approach, using overseas data and weighting for the impact of the Aboriginal population, had not been previously attempted. In this analysis, we estimated there were 335 000 cases of CHF in Australia in 2001; a figure that is consistent with other contemporary estimates of the burden imposed by CHF including those derived from the CASE study (320 000)9, the BEACH data (380 000)20, and official Australian Institute of Health and Welfare estimates (325 000)8. Our study data are distinctive, given that they provide a much more comprehensive view of the likely concentrations of patients beyond large population centres. The estimated whole of population prevalence rate for CHF in 2001 was 17.87 per 1,000 or approximately 2% of the total population which is consistent with UK, US and European estimates21. As our results do not include those individuals with asymptomatic left ventricular dysfunction, these estimates remain conservative12.
A significantly higher prevalence of CHF was evident in rural and remote regions (19.84/1000) and large urban centres (19.01/1000) compared with capital cities (16.94 /1000). Given that mortality rates from CHF are higher in remote regions6, and current specialist CHF services are largely located in capital cities22,23, there is an urgent need to reconsider the way CHF is managed across Australia.
The results make it clear that different strategies are needed in different states and regions. In VIC, WA, SA and the ACT, where it is estimated that over 70% of cases occur in the capital cities, a larger concentration of services located in the capitals may be justified. However in NSW, QLD, TAS and NT, such an arrangement is likely to exacerbate the inequities in access to health services such as cardiology and diagnostic services. NSW, QLD and TAS all have a high proportion of estimated CHF cases concentrated in large urban centres. Regionalised CHF management centres may be more applicable in these States.
Another factor that needs to be considered is the variation in prevalence of CHF between rural and urban populations of Australia. Our estimates indicate that CHF was more prevalent in rural and remote regions and large urban centres than in capital cities. This is due to a higher concentration of older and/or Indigenous people living in these areas10. Higher prevalence rates occurred in locations favoured by retirees (Caloundra, Shoalhaven, Coffs Harbour and Mandurah). Lower rates occurred in remote cities with younger populations such as Mt Isa and Kalgoorlie/Boulder, where industry and employment are an attraction for younger age groups.
Given that CHF is associated with bleak quality of life24, recurrent and life-threatening acute decompensatory episodes, exacerbations of concurrent disease states (eg respiratory or renal failure)25 and has a worse prognosis than many forms of cancer21, it is imperative that all affected individuals are exposed to effective pharmacologic and non-pharmacologic treatment strategies. For rural and remote patients, implementation of some of the recommended programs for the management of CHF, such as nurse-led home visiting programs25, may be unsustainable due to the distances between population centres. This may widen the gap between the quality of care offered to urban Australians and the care available to non-urban dwellers. As acute-care centres providing specialist cardiac care are becoming more concentrated in centralised areas, and local regional hospitals are being down-graded, rural and remote patients are also more likely to need to travel greater distances, at some expense, to receive CHF management.
The findings from this report have highlighted some of the complexities that define the distribution of CHF in Australian rural and remote regions. Not only does consideration need to be given to the location of services, but also to their composition and design. The idyllic rural retirement destinations of Australians will eventually need improved health infrastructure, especially for cardiovascular services, as the migration of the baby-boomers to these regions increases. In areas where Indigenous CHF populations are high, such as Alice Springs and Mt Isa, specialised Indigenous cardiac services are a key to a solution for this problem and must involve the principles of self-determination. Also, because male patients living in remote regions are very low consumers of primary healthcare but constitute 54% of the CHF population, consideration should be given to male-focused cardiovascular care in rural and remote areas26.
Limitations
While this study represents another important step forward in terms of quantifying the burden of CHF in Australia, we acknowledge the limitations of having to derive our estimates from overseas data, highlighting the fact that in the future the dimensions and particular the Australian features of the disease need to be measured with rigorous epidemiological methods. It is important to stress that these results may vary according to age and sex structure between the three geographical locations. Confounding factors likely to increase CHF prevalence and morbidity rates within a specific population cohort, which have not been considered in these estimates, include differences in socio-economic status, rates of smoking and other risk factors for heart disease, community health, acute care services, admission thresholds for hospital admission and climatic factors. Funding and infrastructure is required to support screening of 'at risk' individuals, including the Indigenous population, to determine actual prevalence rates of the disease.
Conclusion
These data highlight the significant diversity that must be accounted for in providing equitable access to CHF services in rural Australia. Accurate referencing of current CHF service locations against the distribution of the Australian CHF population to determine the extent of any patient-service mismatch is essential. Consideration may need to be given to a variety of solutions for the management and funding of CHF, including multidisciplinary approaches and the use of information technology to bridge the distance between very remote communities and centres of care. Due to the extreme variations across geographic regions of Australia in regard to sex, age, cultural backgrounds, socioeconomic status and access to services, we caution against making policy recommendations in relation to CHF using a blanket approach for rural Australia.
Acknowledgements
Robyn Clark is a PhD scholar supported by the National Institute of Clinical Studies and the National Heart Foundation of Australia. Professor Simon Stewart is supported by The National Heart Foundation of Australia and the National Health & Medical Research Council of Australia. We wish to thank Ms Jacqui Howard for the design and artwork presented in the figures and maps associated with this article.
References
1. Clark RA, McLennan S, Dawson A, Wilkinson D, Stewart S. Uncovering a hidden epidemic: a study of the current burden of heart failure in Australia. Heart Lung Circulation 2004; 13: 266-273.
2. Colucci WS, Braunwald E. Pathophysiology of heart failure. In: E Braunwald (Ed.). Heart disease. A textbook of cardiovascular medicine. Philadelphia: WB Saunders, 1997; 394-420.
3. McAlister FA, Murphy NF, Simpson CR et al. The influence of socio-economic deprivation on primary care burden and treatment of heart failure in Scotland. BMJ 2004; 328: 1110.
4. Australian Bureau of Statistics (ABS). Census of population and housing. (Online) 2005. Available: http://www.abs.gov.au/ (Accessed May 2005).
5. Anderson I, Thomson N. Health of Indigenous Australians: a rural perspective. In: D Wilkinson, I Blue (Eds). The New Rural Health 1st edn. Melbourne: Oxford. 2003; 110-126.
6. Australian Institute of Health and Welfare. Rural, regional and remote health: a study on mortality. AIHW Cat. no. PHE 45. (Rural Health Series no.2). Canberra: AIHW, 2003.
7. Australian Institute of Health and Welfare. The Health and Welfare of Australia's Aboriginal and Torres Strait Island Peoples: Australian Bureau of Statistics (ABS) Cat 4704.0. Canberra: ABS, 2003
8. Australian Institute of Health and Welfare. Heart, stroke and vascular diseases - Australian facts 2001. AIHW Cat no. CVD13. Canberra: AIHW, 2001.
9. Krum H, Tonkin AM, Currie R, Djundjek R, Johnston CI. Chronic heart failure in Australian general practice. The Cardiac Awareness Survey and Evaluation (CASE) Study. Medical Journal of Australia 2001; 174: 439-444.
10. Australian Bureau of Statistics (ABS). 2001 Census Basic Community Profiles and Snapshots. (Online) 2001. Available: http://www.abs.gov.au/ausstats/abs@census.nsf/ddc9b4f92657325cca256c3e000bdbaf/7dd97c937216e32fca256bbe008371f0!OpenDocument (Accessed 15 December 2005).
11. McDonagh T, Morrison C, Lawrence C et al. Symptomatic and asymptomatic left-ventricular systolic dysfunction in an urban population. Lancet 1997; 350: 829-833.
12. Morgan S, Smith H, Simpson I et al. Prevalence and clinical characteristics of left ventricular dysfunction among elderly patients in general practice: cross sectional survey. BMJ 1999; 318: 368-372.
13. Neilson OW, Hilden J, Larsen CT, Hansen JF. Cross sectional study estimating prevalence of heart failure and left ventricular systolic dysfunction in community patients at risk. Heart 2001; 86: 172-178.
14. Mosterd A, Reitsma JB, Grobbee DE. ACE inhibition and hospitalisation rates for heart failure in The Netherlands, 1980-1998. Heart 2002; 87: 75-76.
15. Doughty R, Yee T, Sharpe N et al. Hospital admissions due to congestive heart failure in New Zealand. New Zealand Medical Journal 1995; 108: 473-475.
16. Shaufelberger M, Swedberg K, Koster M et al. Decreasing one-year mortality and hospitalization rates for heart failure in Sweden: Data from the Swedish Hospital Discharge Registry 1988 to 2000. European Heart Journal 2004; 25: 300-307.
17. Australian Bureau of Statistics. The health and welfare of Australia's Aboriginal and Torres Islander Peoples. Cat no.4704.0. Canberra: ABS, 2003.
18. Australian Institute of Health and Welfare. Death rates for health failure. (Online) 2004. Available: http://www.aihw.gov.au/cvd/statistics/deathratetableAge.cfm (Accessed July 2005).
19. Commonwealth of Australia. Measuring remoteness: accessibility/remoteness index of Australia (ARIA). (Online) 2003. http://www.gisca.adelaide.edu.au/ (Accessed 7 December 2005).
20. Britt HC, Miller GC. The BEACH study of general practice. Medical Journal of Australia 2000; 173(2): 63-64.
21. Stewart S, MacIntyre K, Hole DA et al. More malignant than cancer? Five year survival following a first admission for heart failure in Scotland. European Journal of Heart Failure 2001; 3: 315-322.
22. Driscoll A, Worrall-Carter L, McLennan S, Dawson A, Stewart S. Variability and sustainability of heart failure management programs in Australia. In: The National Institute of Clinical Studies (Ed). Heart Failure Forum 2004: Improving outcomes in chronic care. (Online) 2004. Available: http://hff2004.docuserve.com.au/cgi-bin/readcsvplus.pl?config=heartforum.pl&Surname==driscol&sort_a=Surname&template=0 (Accessed July 2005).
23. Australian Institute of Health and Welfare. Medical labour force. Report no.: AIHW Cat. No. HWL 15. AIHW: Canberra, 1998.
24. CONSENSUS Trail Study Group. Effects of Enalapril on mortality in severe congestive heart failure: results of the North Scandinavian Enalapril Survival Study (CONSENSUS). New England Journal Of Medicine 1987; 316: 1429-1435.
25. Stewart S, Blue L (Eds). Improving outcomes in chronic heart failure: a practical guide to specialist nurse intervention. 1st Edn. London: BMJ Books, 2001.
26. Franciosa JA, Wilen M, Ziesche S et al. Survival in men with left ventricular failure due to either coronary heart disease or idiopathic dilated cardiomyopathy. American Journal of Cardiology 1983; 51: 831-836.
Abstract
Introduction:
Chronic heart failure (CHF) develops in frail elderly individuals who have suffered an acute or sustained insult to the structural efficiency of the heart due to the presence of underlying heart disease and/or hypertension. It is also more common in individuals with disproportionately high levels of cardiac disease or its risk factors, for example lower socioeconomic status. As such, this epidemic is particularly significant for older people, males and Aboriginal people; groups who comprise a greater proportion of the population in rural and remote Australia. The aim of this study is to determine if the rates of CHF differ between urban and rural Australia.Method: CHF prevalence rates derived from well validated international CHF prevalence data were applied to the Australian Bureau of Statistics Census data for 2001 and weighted to reflect the proportion of Aboriginal people in each geographical stratum.
Results: Australia wide, the estimated prevalence of CHF was 17.87 per 1000, ranging from 13.98/1000 in the Australian Capital Territory to 29.50/1000 in rural Northern Territory. Overall, CHF was more prevalent in rural and remote regions (19.84/1000) and large urban centres (19.01/1000) than in capital cities (16.94/1000) (p<0.001). High prevalence rates were also noted in the idyllic rural locations favoured by retirees. In Victoria, Western Australia, South Australia and the Australian Capital Territory over 70% of the estimated individual cases were located in capital cities. In New South Wales, Queensland, Tasmania and the Northern Territory the highest proportion of cases occurred outside capital cities.
Conclusions: The main significance of these findings is that while a majority of heart failure may occur among people living in cities (because that is where most people live), a disproportionate number of cases occur among people living outside these cities (due to age and other socio-demographic risk factors) where services may be fewer and less accessible.
Key words: Australia, chronic heart failure, epidemiology.






