Introduction
Globally, health workforce is maldistributed in terms of not only practice location, but also vocational mix, with growing numbers of subspecialist practitioners and fewer generalist practitioners1. There is growing evidence that health systems with a generalist orientation consistently achieve a better and more equitable distribution of health outcomes across the population regardless of patient socioeconomic or geographic constraints2-7, and help curb the rise in healthcare costs through greater integration and reducing the trend towards more and more expensive services per individual and per visit8. Of particular relevance to the rural context is the evidence that a primary care-oriented workforce can help to prevent and manage the growing burden of chronic disease in poorer and/or rural community settings9, as well as addressing the needs of an ageing population with growing multi-morbidities10.
Training more generalist medical practitioners, particularly primary care physicians, is recognised as an important strategy for addressing vocational and geographic maldistributions11. A number of medical schools worldwide are focused on producing rural and/or generalist medical practitioners, though few track their graduates to determine if they do actually choose long-term rural or generalist careers. The Northern Ontario School of Medicine in Canada, with a mandate focused on improving the health of urban, rural and remote communities across the region, found 62% of their Doctor of Medicine graduates chose family practice training, with a further 33% training in other general specialties12. The University of Missouri’s School of Medicine in the USA, which developed a Rural Track Pipeline program to promote the supply and retention of rural physicians statewide, found graduates were more than two times more likely to choose family medicine than graduates of the traditional program track13. While not systematically tracking their graduates, medical schools in South Africa14, Scotland15 and New Zealand16 also have curriculums focused on long-term rural and/or generalist careers.
These findings are broadly aligned with graduate outcome studies from two rurally orientated medical schools in Australia: the Flinders University School of Medicine (FUSM) and the Rural Clinical School of Western Australia (WARCS). The FUSM surveyed postgraduate year (PGY) 5–7 graduates to compare vocational career choices of those who had undertaken their entire PGY 3 in an urban teaching hospital versus those who had undertaken PGY 3 in a rural primary care practice or a rural tertiary referral hospital17. They found graduates who had spent time in the rural teaching sites were significantly more likely to have entered rural practice, and more likely (though not statistically significant) to choose general practice (57% v 38%). The WARCS, a partnership involving University of Western Australia and University of Notre Dame Australia medical schools, which bases students for one academic year in a rural location, surveyed their PGY 10 graduates and found the majority identified with general practice and other rurally related colleges18. However, this study made no comparison with the vocational career choices of other non-rural clinical school Australian medical graduates to identify differences in college choice.
The James Cook University (JCU) medical school is another Australian medical school with a mission to produce graduates who meet the regional, rural and remote medical workforce needs of the local region. Established in 2000, the undergraduate Bachelor of Medicine, Bachelor of Surgery (MBBS) program has a geographically distributed model of linked rural clinical schools located across northern Australia. The JCU medical school’s overall aim is to produce a high proportion of graduates who choose not only to practise in rural and remote areas of northern Australia, but also generalist careers.
JCU medical school graduates all experience 6 years of training in rural or regional clinical schools and a minimum 20 weeks of placement in small rural or remote locations. While previous studies have shown JCU graduates to be significantly more likely to practise rurally than other Australian medical graduates19,20, there has been no investigation of whether their choice of vocational career is any different. Promisingly, however, collation of final year student exit survey data from 2016 to 2017 does show JCU medical student practice intentions at time of graduation were for predominantly generalist rather than specialist careers. Specifically, 24% of final year JCU medical students reported a firm intention to undertake a purely generalist career (rural generalist medicine or general practice), while 39% intended to undertake a generalist discipline (‘generalist specialist’) in surgery (15%), adult internal medicine (9%), paediatrics (7%) or emergency medicine (8%), not including 16% still undecided.
The JCU medical school graduated its 13th cohort in 2017. This study investigated the postgraduate qualifications and current career choices of the first seven graduating cohorts (PGY 5–11). The study explores in some depth the key influences that shaped graduates’ vocational choice, and analyses whether JCU graduates are more likely to choose generalist careers than Australian medical graduates with a similar level of experience.
Methods
Design
This analysis of postgraduate qualifications and career choice for the first seven MBBS cohorts is part of an ongoing longitudinal cohort study that will continue to provide information about JCU medical graduate outcomes. A cross-sectional study design collected data from JCU MBBS graduates who had consented to be contacted between PGY 4 and 10 (2005–2011 graduating cohorts). Consent for further contact was obtained from the annual exit survey of year 6 students, which has been conducted since 2005 (the exit survey includes a page requesting students to provide their permanent email and mobile phone details). Overall, 409 of the total 530 graduates in the first seven cohorts consented to contact for further studies, such as the present study.
Participants and data sources
In early 2016, a survey was administered by SurveyMonkey and telephone to all 409 JCU MBBS graduates who had consented to participate. The survey asked respondents a variety of questions, including ‘Please name all academic or medical qualifications that you have obtained in Australia or overseas since graduation (eg FRACP, MPHTM, DrPH)’ and ‘Which specialist training course have you completed/been accepted into?’
Additional free-form comments were sought by asking participants to ‘… write a short paragraph describing chronologically how key influences – including personal interest, certain people, specific experiences, a job opportunity, an intended career direction, etc – resulted in you choosing this particular specialty’.
Comparison group data (medical practitioners aged <35 years and working in Australia in 2015) was sourced from the Australian Department of Health’s national health workforce database21. The Data Tool function of the website was used to display the distribution of registered medical practitioners’ ‘primary specialty’, excluding those who had ‘not stated’ their primary specialty when registering. Table 1 describes the distribution of primary speciality for the 5353 medical practitioners registered in 2015, aged less than 35 years, who had stated their primary specialty.
Table 1: Comparison of current vocational career choice for 178† JCU MBBS graduates (2005–2011) in 2015 and Australian medical graduates in 2015 aged <35 years (not including non-specialist hospital-based practice)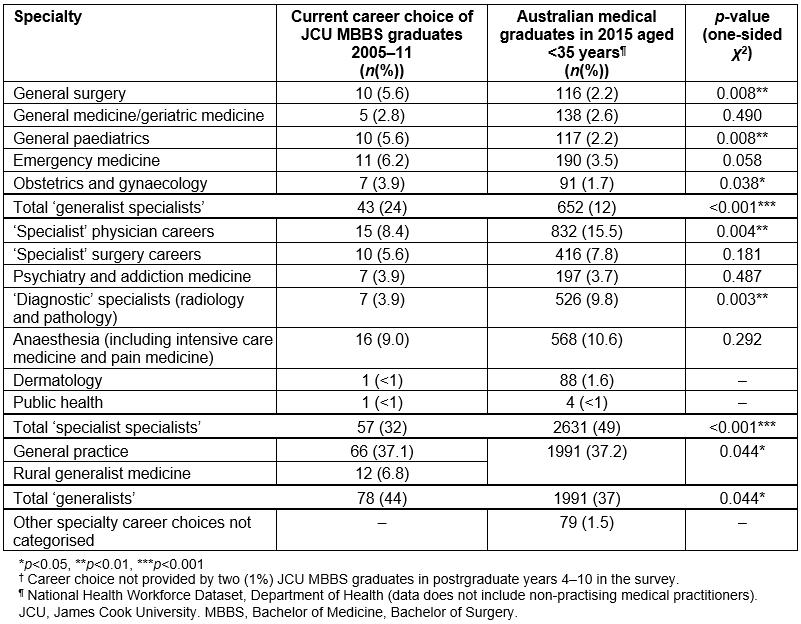
Data analysis
All data were coded numerically and entered into the Statistical Package for Social Sciences, v20 (IBM; http://www.spss.com). Analyses included (1) simple descriptive statistics to show postgraduate qualifications and career choice, (2) bivariate analyses (one-sided χ2 tests) to test whether JCU MBBS graduates are more likely to choose a generalist rather than specialist career compared to other Australian medical practitioners of similar length of work experience (age <35 years) and (3) content analysis undertaken on the graduate responses to the open-ended question.
Categorisation of medical careers into ‘generalist’, ‘generalist specialty’ and ‘specialist specialty’ careers used in this analysis is consistent with the 2012 Australian Medical Association (AMA) position statement on fostering generalism in the medical workforce, which states that a generalist specialist is one that retains a broad and undifferentiated scope of practice, such as a general physician or surgeon22. The categorisation of disciplines such as obstetrics and gynaecology, which are not specifically described in the AMA position statement, was decided through discussion between all authors. The categorisations chosen are described in Table 2, which also provides a complete list of JCU medical graduate career choices, including surgical and medical subspecialties. Graduates undertaking careers in general practice or rural generalist medicine were regarded as ‘generalists’, while traditional specialties were divided into the more generalist ones such as general surgery, general medicine including geriatric medicine, emergency medicine and general paediatrics (‘generalist specialties’) and more specialised careers such as medical and surgical subspecialties, obstetrics and gynaecology, anaesthetics, pathology, radiology and public health (‘specialist specialties’).
A priori content analysis was undertaken to group the variety of responses given in the open-ended question asking participants to ‘… write a short paragraph describing chronologically how key influences resulted in you choosing this particular specialty’ into common themes (Table 3). Content analysis of the free text responses involved identifying and counting key phrases and general themes about the key influences for respondents choosing their current medical discipline, and selecting specific graduate quotes that succinctly described these themes. The content analysis of the open-ended question was conducted by the author TW, and the analysis checked by TSG and SL for investigator triangulation; differences were resolved through discussion between authors.
Table 2: Categorisation of medical careers into ‘generalist’, ‘specialist’ or ‘specialist generalist’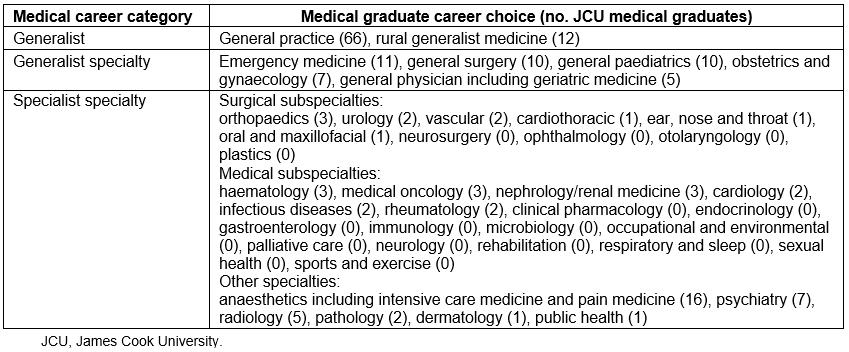
Table 3: Key factors and influences leading to current vocational career choice of James Cook University MBBS graduates (2005–2011)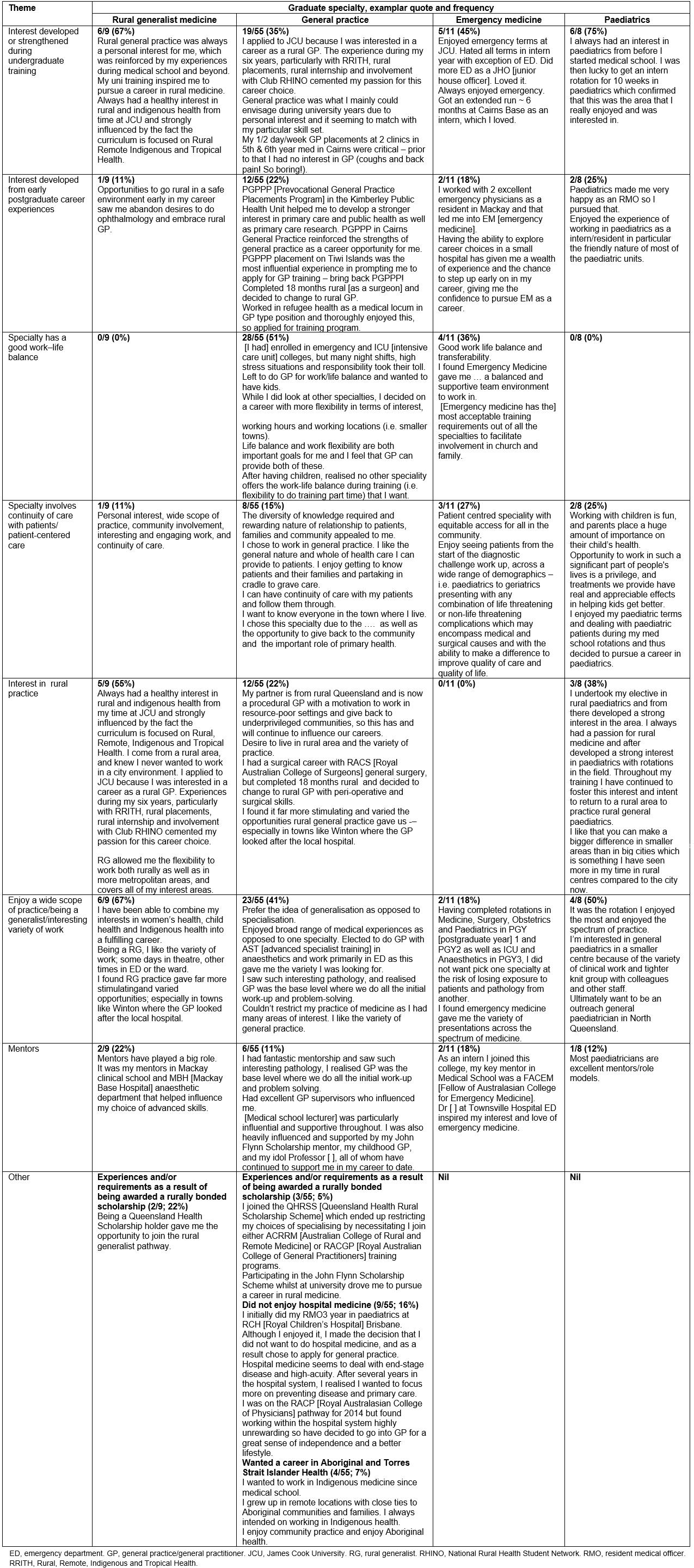
Ethics approval
Ethics approval for the study was granted by the JCU Human Research Ethics Committee (H1804).
Results
Description
Four hundred and nine graduates who had reached at least PGY 4 and had provided current email or mobile phone contact details in their exit survey at graduation responded to a 2016 survey. However, emails and/or text messages to 111 graduates were not sent successfully, resulting in 180 providing a response, and thus an effective response rate of 180/298 (60%). Of these, 34 (19%) graduated in 2005, 27 (15%) graduated in 2006, 30 (17%) graduated in 2007, 24 (13%) graduated in 2008, 16 (9%) graduated in 2009, 28 (15%) graduated in 2010, and 21 (12%) graduated in 2011 (and thus were at the beginning of PGY 4 when the study was undertaken).
Of the 180 respondents, 86 (48%) reported having achieved (not just currently enrolled in) a postgraduate fellowship, with a number of graduates having obtained two or more fellowships. General practice (FRACGP) was the most common (48, 27%), followed by internal medicine (FRACP; 12, 7%), rural medicine (FACRRM; 11, 6%), surgery (FRACS, 7, 4%), emergency medicine (FACEM; 6, 3%), anaesthetics (FANZCA; 4, 2%), obstetrics and gynaecology (FRANZCOG; 4, 2%), radiology (FRANZCRad; 2, 1%) and pathology (FRCPA; 1, <1% and FRCPath; 1, <1%), while two were undertaking non-specialist hospital-based practice. Other postgraduate qualifications included a PhD and nine (5%) Masters of Public Health and Tropical Medicine, as well as postgraduate diplomas in Child Health (15, 8%), Surgical Anatomy (3, 2%), Clinical Education (3, 2%), and Diving and Hyperbaric Medicine (<1%). (A description of Australian medical fellowship qualification acronyms is available at https://healthengine.com.au/info/australian-fellowship-qualifications.)
Bivariate analysis
Compared to a group of Australian medical graduates with similar years of experience, JCU medical graduates are significantly more likely to choose careers as ‘generalists’ (general practice/rural generalist medicine (p=0.044)) or ‘generalist specialists’ in general surgery (p=0.008), general paediatrics (p=0.008), emergency medicine (borderline significance, p=0.058) and obstetrics and gynaecology (p=0.038), but less likely to be ‘specialist specialists’ such as in a medical subspecialty (p=0.004) or a ‘diagnostic’ specialty such as pathology or radiology (p=0.003) (Table 1).
Content analysis
The key influences on JCU medical graduates’ current career in rural generalist medicine, general practice, emergency medicine and paediatrics were grouped under seven common themes (Table 3). These were ‘interest developed or strengthened during undergraduate training’, ‘interest developed from early postgraduate career experiences’, ‘specialty has a good work–life balance’, ‘specialty involves continuity of care with patients’, ‘interest in rural practice’, ‘enjoy a wide scope of practice/being a generalist’ and ‘mentors’. Graduate comments that typified each common theme for each of the four chosen specialties are reported verbatim from the completed surveys.
Discussion
Overall, the JCU medical program produces significantly higher proportions of generalist and ‘generalist specialist’ medical practitioners compared to Australian medical practitioners of similar experience. These disciplines include general practice/rural generalism, general surgery, obstetrics and gynaecology and general paediatrics, with a borderline significant trend towards more graduates choosing emergency medicine careers. Conversely, the JCU medical school produces a smaller proportion of graduates choosing specialist careers, in particular, medical subspecialties.
While JCU medical graduates chose generalist and generalist-specialist careers more than Australian medical graduates of similar experience, the proportion of these careers are similar to those reported in a 2008 study of 15 graduates of the Flinders University School of Medicine’s (FUSM) rural clinical training site in Darwin17. For example, comparing vocational career data between JCU and FUSM graduates from the rural tertiary site, there were similar percentages (given the very low sample size of FUSM graduates) in general practice (JCU, 44%; FU, 53%), emergency medicine (JCU, 6%; FU, 13%), obstetrics and gynaecology (JCU, 4%; FU, 7%) and anaesthesia (JCU, 9%; FU, 13%).
There are a number of possible reasons why training medical graduates in regional and rural sites results in proportionally more generalists and ‘generalist specialists’, and fewer specialists. One likely reason is self-selection: students are attracted to medical schools having a rural focus because of interest in a rural career. For example, a 2016/17 JCU evaluation23 found that 81/207 (39%) of final year JCU medical students initially applied to the school at least partly because of an interest in rural medicine. The content analysis of the present study also supports this finding, with a number of graduates commenting they were initially attracted to the medical school for its focus on rural medicine and, to a lesser extent, Aboriginal and Torres Strait Islander health. Then, through undergraduate experiences, this attraction later developed into a desire for a rural career, often as a rural general practitioner (GP) or as a rural generalist. Thus, these findings add to the evidence base relevant to addressing medical workforce maldistribution, suggesting selection criteria for admission into medical school should be broadened to allow preferential selection of applicants with intentions for a rural and/or generalist career24.
The JCU medical school has mandatory generalist medicine experiences across years 1 to 6, which include primary care settings in rural practices and in Aboriginal community-controlled health services. Generalist specialist experiences occur in years 2–5, often in rural and tertiary hospital emergency departments, birth suite, general medicine and general surgery rotations, while subspecialist rotations in medicine and surgery mostly occur only in year 6. Graduate comments on the influence of these experiences on career choice include:
Experiences during my six years, particularly with RRITH [Rural, Remote Indigenous & Tropical Health – year 2 subject], rural placements, rural internship and involvement with Club RHINO [JCU rural health club] cemented my passion [for general practice].
I always had a healthy interest in rural and indigenous health from my time at JCU and strongly influenced by the fact the curriculum is focused on Rural, Remote, Indigenous and Tropical Health.
I applied to JCU because I was interested in a career as a rural GP;
I wanted to work in Indigenous medicine since medical school.
In particular, the content analysis suggests ‘rural intent’ evolved into a ‘desire for a rural career’ through positive experiences on undergraduate clinical placements and hospital rotations, typically in smaller, rural hospitals and medical centres where preceptors have more time to mentor and develop relationships with students as positive role models. All JCU medical graduates have experience in smaller hospitals in rural or remote locations in their undergraduate clinical placements, and many continued to practise in smaller, more rural towns in their early career20. This study identifies that a number of JCU medical graduates mentioned undergraduate rural and remote experiences as being one of the most influential in later choosing a career in rural generalist medicine, general practice, paediatrics and emergency medicine. With the JCU medical curriculum requiring a minimum of 20 weeks clinical placement in smaller rural and remote communities, the range and personal impact of such experiences for JCU medical graduates are likely to be considerably greater than for most Australian medical graduates. Comments provided by the JCU graduates support this:
My 1/2 day per week GP [general practice] placements at 2 clinics in 5th & 6th year med in Cairns were critical – prior to that I had no interest in GP (coughs and back pain! So boring!).
Enjoyed my GP placements while in med school, especially the rural ones.
Two years as a student [at Darwin Clinical School] and two years working in Northern Territory led me to love the area and choose a specialty that would suit.
At the very least, rural placements would help to demystify the many aspects of rural practice. It also appears that other aspects of a rural placement – positive experiences in rural and remote community settings and relationships with ‘generalist’ role models – may influence graduates to work in such settings and pursue a generalist orientation to their training.
The content analysis findings also show an interesting combination of nature and nurture influencing career choice. The majority of JCU graduates reported preferring a specialty that involves one or more of a wide scope of practice, good work–life balance and continuity of care with patients. At least some of the ‘nature’ influences may be associated with the medical school’s selection process, which is focused towards choosing applicants with strong inter-personal and communication skills, self-reliance and a commitment to helping the rural and regional population of northern Australia including underserved Aboriginal and Torres Strait Islander populations.
Furthermore, it may be possible that the JCU medical school, compared to other Australian medical schools, is selecting proportionally more applicants with intrinsic motivations leaning towards independent practice, patient-centred care and community-based service rather than hospital-based practice. For example, JCU graduates commented:
I was on the RACP pathway for [year deleted] but found working within the hospital system highly unrewarding so have decided to go into GP [general practice] for a great sense of independence and a better lifestyle.
I like that you can make a bigger difference in smaller areas than in big cities which is something I have seen more in my time in rural centres compared to the city now.
[I chose general practice because of a] desire to live in rural area and the variety of practice.
Indeed, 9 of the 55–JCU medical graduates currently working as GPs had entered their internship wanting to practise hospital-based medicine, but changed after some years because they did not enjoy the hospital system, citing its regulated processes and focus on end-stage disease and high acuity. Thus, the realities of a hospital-based career, chosen before or during their undergraduate medical course, did not align well with their personal attributes, internal drivers and (wide-ranging) skills sets. This is a similar finding to that of a survey of 6795 doctors graduating from UK medical schools in 2008: 56% agreed that general practice was currently ‘a more attractive career prospect than hospital medicine’25.
This and subsequent outcome studies from the JCU program could allow a more nuanced approach to medical workforce planning in northern Australia as they provide insights into how to address current workforce needs and gaps by specialty. Documenting patterns of practice of graduates is an important strategy in evaluating progress towards addressing workforce needs. In fact, schools with a social accountability mission should continually critically self-evaluate by reporting the extent to which their graduates are meeting this mandate26,27. In many cases, this means considering patterns of practice, whether geographic (eg what proportion are working in designated rural or remote areas), or other indicators of practice with underserved populations (eg working in Indigenous communities or in Aboriginal community-controlled health services). Documenting career choice (eg how many are practising in primary care) is also important, but these outcome measures only tell part of the story.
The workforce needs of the region the school serves also warrant consideration: which communities need what skills, and how can these best be met? A rurally orientated school with a large proportion of graduates practising in rural and remote areas is commendable, but further analysis is needed; for example, do graduates have the knowledge, skills and attitudes needed to meet the regional health priorities, and are they practising where they are most needed? Integrated needs-based health service and workforce planning might be required to address the needs of less desirable rural communities that potentially miss out on the benefits of new graduates. This may require consideration of what is the most desirable mix of generalist versus specialist careers for the local region, and appropriate training programs and career pathways, for example increasing the preparation of graduates for remote as well as rural practice, as recently recommended by Wakerman and colleagues28. It also requires an understanding of community needs and the workforce needed to meet these needs, while taking into account the changing demographics in both the communities and the healthcare workforce.
A final and pivotal step is to develop training pathways appropriate to regional needs. For example, recent regional training hubs funding from the Australian Government will allow JCU to further build and connect regional specialist training pathways across northern Queensland and support medical training from internship to fellowship.
The recently established Tropical Australian Academic Health Centre is a collaboration between five hospital and health services, the Northern Queensland Primary Health Network and JCU, which aims to embed research into health service delivery and thereby improve quality and efficiency of health care, enhance recruitment and retention of professionals in the region and encourage greater investment in the north.
JCU’s postgraduate general practice training program, Generalist Medical Training, commenced in 2016, providing postgraduate medical education and training in general practice and rural medicine across all of Queensland except the south-eastern corner. With a footprint covering the majority of rural and remote Queensland, this program aims to better connect the training pipeline from medical school to a career in general practice, with a special emphasis on remote and underserved communities.
The JCU medical school has had a substantial impact on the progression of graduates into rural and remote practice through such pathways. While the JCU program currently produces only about 15% of the yearly total of Queensland medical graduates, these graduates constitute almost 30% of the new rural Queensland workforce. Health Workforce Queensland’s 2015 Minimum Dataset report29 comments, ‘The impact of the introduction of medical degrees at the other Queensland universities can be seen quite clearly, particularly the number of graduates from JCU working in remote, rural and regional Queensland. In terms of feeding the pipeline of graduates into remote, rural and regional practice, the performance of JCU is particularly noteworthy as they generally have the second lowest number of graduates each year …’
Many JCU graduates have trained with Queensland Health’s Rural Generalist Pathway30, a supported career pathway for junior doctors to train in rural and remote medicine. The pathway, which joins evidence with policy to achieve professional recognition, credentialing and industrial recognition, was introduced at the same time as JCU’s first graduating cohorts entered vocational training. This fortunate timing has brought symbiotic benefits for both JCU graduates and the pathway, although the real beneficiaries have been Queensland’s rural communities, which have benefited from the increased supply of rural doctors; but there is more to do.
Limitations
While the actual response rate to the survey is reasonable at 60%, only 180 of the total 530 JCU medical graduates in the first seven cohorts responded to this survey, so this may not be a representative sample. However, compared to all JCU PGY 4–10 medical graduates with a career choice identified in the College of Medicine and Dentistry longitudinal tracking database (499 of 530), the study sample has similar proportions. This applies to gender (64% female v 60%, respectively), and to graduates choosing general practice (37% v 34%), general surgery (6% v 6%), anaesthesia/intensive care medicine careers (9% v 7%), obstetrics and gynaecology (4% v 5%) and emergency medicine (6% v 5%), although proportions choosing rural generalist medicine (7% v 12%) were somewhat different.
In addition, the current career of JCU graduates is described based on qualifications achieved and current training programs, whereas the data for all Australian medical graduates are only for the former, and thus the two data sources might not be entirely comparable. While comparison with the Australian Institute of Health and Welfare’s National Health Workforce dataset is somewhat limited, it is the best comparator dataset available for medical career choice. Finally, the higher than average uptake of JCU graduates choosing rural generalist careers in Queensland would also likely influence the total proportion with generalist careers.
The qualitative aspect of the present study was undertaken as content analysis of just one open-ended question. The purpose of content analysis is to organise and elicit meaning from the data collected to draw realistic conclusions from it; in contrast to other qualitative research methods, it is not linked to any particular theoretical framework31. Thus, while the content analysis provides additional insights to the quantitative findings of the present study, it has limited ability in eliciting deeper qualitative understandings.
Conclusions
The JCU medical program produces significantly more medical generalists and ‘generalist specialists’ but fewer specialists compared to similarly experienced Australian medical practitioners, and thus a medical workforce more aligned to local population needs for northern Australia. The authors contend this is likely to be at least partly due to the JCU medical curricula focus on providing students with a wide range of generalist experiences and its focus on rural, remote, Indigenous and tropical health. As most JCU MBBS graduates choose a regional, rural or remote career, the practice requirement for generalist skillsets in smaller rural and regional hospitals and medical centres also likely contributes.
In addition, the findings suggest many JCU MBBS graduates have chosen a career that is not only compatible with regional, rural or remote practice, but also involves continuity of care with patients, a wide scope of practice and a good work–life balance. A number of graduates reported that they came to the JCU medical school because of their intention for a rural medicine career, and many commented that their career choice was influenced by undergraduate and early career experiences in smaller rural and regional hospitals and health centres. It is likely that JCU medical graduates’ early career experiences, personal attributes and drivers differ from those of most other Australian medical graduates.
These findings add to the evidence base suggesting the selection criteria for admission into medical school should be broadened to preferentially select applicants with intentions for a rural and/or generalist career. Furthermore, critical aspects of the ‘rural pipeline’ can be developed first in undergraduate training – in particular, extensive rural placement experiences in generalist and generalist specialist disciplines, and continuing all the way to the end of postgraduate training. Other aspects of the ‘rural pipeline’ were also identified as important: selection and support of appropriate students, role modelling and identity formation. To ensure that community needs are being met, consideration needs to be paid not only to outcomes relating to the geographic locations where graduates practise (eg rural/remote) but also to their choice of specialty and the balance of generalist versus specialist careers.
Acknowledgements
The authors are grateful for the efforts of all JCU medical graduates who consented to contact for future studies in the annual year 6 exit survey.



