Introduction
There is growing evidence that medical students who have had undergraduate rural experiences will enter rural medical practice at higher rates than those not participating1,2. Some medical students may also enter medical school with pre-existing interest in a rural career3: students entering medical school from a rural background are likely to continue this rural trajectory4. However, Playford et al (2016) have shown that a substantial proportion of students expected to be on a rural trajectory will have no rural experience after graduating5. It is not known whether this is due to lack of interest or lack of opportunity.
Given the new Commonwealth and state interest in encouraging rural training pathways after graduation, it is important to gauge pre-graduate’s level of interest in rural options. The first step in the pathway is rural internships. Therefore the present study asked pre-graduating medical students about their levels of interest in a rural internship, given that 2016 was the first year when 10 full rural internships were offered in Western Australia, in addition to the 108 single 10-week-term rural intern rotations.
Method
All penultimate and final-year medical students at both Notre Dame University and the University of Western Australia were invited to participate via a secure survey link circulated using Facebook and rural club contacts in May–June 2016.
Information was requested about factors known to be associated with rural work: rural background (years spent rurally), rural clinical school (RCS) participation, rural health club membership and pre-existing intention to work rurally. The survey then asked students to rate their likelihood, on a five-point Likert scale, of applying for a full-year rural internship in a Western Australia Country Health Service (WACHS) hospital or for an urban internship based on the rural internship rotations the urban hospital offered.
Ethics approval
Ethics approval was granted by both universities (016122F and RA/4/1/8369).
Results
A total of 140 medical students responded to the survey, representing both universities and all invited years, with response rates of 19–23% per year group. Not all respondents completed all questions. Students with a rural background of 5 years or more (50/140, 36%), those with RCS experience (65/140, 46%) and those associated with SPINRPHEX, a national rural student health network (84/140, 60%), were disproportionately represented in the sample.
All remaining survey items were affirmatively answered: 112 of 140 (80%) intended to work rurally after their postgraduate training, 70 of 140 (50%) came into medical school with this intention and 98 of 140 (70%) had been influenced by their medical school experiences.
With respect to intern work (Table 1), 59 of 140 (42%) were likely/very likely to consider a full rural internship with WACHS whilst 59 respondents (42%) were unlikely/very unlikely to apply for these same positions. A total of 100 of 138 (72% were likely/very likely to consider an urban internship based on its rural rotations. An overlap of 47 students were likely/very likely to consider both options.
Logistic regression showed that, after controlling for all other factors, the remaining independent predictors of intending to choose a full-time rural internship were pre-existing interest on entering medical school (odds ratio (OR) 2.881, confidence interval (CI) 1.209,6.864 p=0.017) and intention to practise rurally as a consequence of medical school (OR 5.154, CI 1.929,13.771, p=0.001).
Table 1: Likelihood of applying for internship for a full year in a Western Australian rural hospital or to a metropolitan hospital based upon rural rotations offered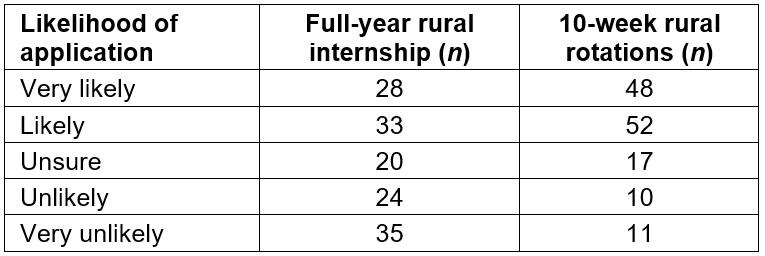
Conclusion
There is considerable rural interest in a subset of Western Australian medical students who already have high rates of rural experience in terms of background, club membership and RCS participation. They are clearly interested in long-term rural work, of which full-year rural internship may play a part. Identifying these students with rural intentions in medical school may assist in the allocation planning process.

