Introduction
Geographic disparities in access to health care have been well described in Canada, and individuals living in rural regions report significantly more barriers to service access and lower rates of service utilization1. A rural place of residence has been associated with lower uptake of evidence-based therapies2,3 and poorer disease-specific and overall health outcomes, such as increased perinatal mortality4 and hospitalization for heart failure5.
Disparities in HIV care, specifically, have been reported among individuals living in rural regions of North America6. Rural place of residence has been associated with increased mortality among people living with HIV7, late diagnosis of HIV8, and later uptake of novel antiretroviral agents9. Data on HIV-related outcomes are lacking for rural Canada and are even more limited for northern Canada. Although limited prior research has assessed for similarities between rural and northern communities in Canada, similar health resource challenges may exist in rural and northern regions. Recognizing similar challenges to health and wellness in rural and northern Ontario, the Ontario Ministry of Health and Long-Term Care has developed a strategic plan that addresses both rural and northern health care10. Identified barriers to health care in northern Canada, encompassing rural and non-rural regions, include the low number of specialist physicians per capita and long travel distances between northern regions and major urban centres11. In addition to long travel distance, significant costs of travel, including those associated with childcare, can also be a barrier to care and this can have a particularly significant impact on women living with HIV. Qualitative research involving women living with HIV across British Columbia, Canada, has found that for women living in smaller communities, social distance, such as experiences of racism, classism and sexism when accessing care, can also be an important barrier to care. These social distances along with physical distances to services can create a socio-spatial environment that is not accessible for some women living with HIV12.
For people living with HIV, experiences of HIV-related stigma can create additional barriers to care. HIV-related stigma has been demonstrated to negatively affect quality of life13,14, increase psychological distress15,16, and decrease medication adherence17, access to health care18-20 and social interaction21. Furthermore, women living with HIV have been found to be disproportionately affected by barriers to care, such as stigma, and these barriers may be exacerbated in rural regions where HIV awareness is often limited22. This is particularly important in a rural context as HIV-related stigma has been well described in high-prevalence rural regions23. In both low- and high-prevalence regions, low rates of HIV knowledge have been identified as a contributor to high rates of HIV-related stigma, and low levels of HIV knowledge have been reported in rural regions of Canada and the USA24-26. High rates of HIV-related stigma coupled with significant concerns over confidentiality in rural areas can act as a significant barrier to service access27,28. Less is known about the impact of HIV-related stigma in northern Canada, but this represents an important area of inquiry.
This study aimed to assess geographic differences in experiences of HIV-related stigma among women enrolled in the Canadian HIV Women’s Sexual and Reproductive Health Cohort Study (CHIWOS). This study compared experiences of HIV-related stigma between women living with HIV who reside in northern and southern regions of Ontario, Canada, and also between those living in rural and non-rural regions of Ontario. The hypotheses were that (1) living in a northern region is independently associated with higher HIV-related stigma and (2) living in a rural region is independently associated with higher HIV-related stigma.
Methods
The Canadian HIV Women’s Sexual & Reproductive Health Cohort Study
CHIWOS is a prospective, multisite cohort study that operates within a community-based participatory research methodology (CBPR), along with GIPA (greater involvement of people with HIV/AIDS) and MIWA (meaningful involvement of women living with HIV/AIDS) principles28-32. This methodology recognizes power imbalances embedded within research and aims to mitigate them through shared community–academic ownership of this work with the goal of improving the health and wellbeing of women living with HIV. As one component of this methodology, peer research associates (PRAs), who are women living with HIV trained as researchers, were instrumental in the study design, recruitment, data collection, analysis, interpretation and knowledge translation29. For this specific analysis, peer co-researchers and co-authors helped to refine the research question, guide selection of covariates and interpret the findings. CHIWOS is grounded in a Critical Feminist framework and guided by a Social Determinants of Health framework33, as described elsewhere29. The primary aim of CHIWOS is to assess the proportion, distribution and patterns of use of women-centred HIV care, along with the factors associated with its use and the impact of such use on health outcomes. A full description of the cohort and a detailed description on recruitment have been published previously34,35.
Study population and recruitment
This analysis included baseline cross-sectional data from women living with HIV in Ontario aged ≥16 years who enrolled in CHIWOS between 27 August 2013 and 27 April 2015. Participants were excluded if a stigma score could not be calculated due to missing data. Participants were recruited through PRA networks, HIV clinics, AIDS service organizations, community-based organizations, networks of the CHIWOS national steering committee and Community Advisory Boards, online social media and peer referrals33. Non-random purposive sampling was used to enrol women consistent with the geographic distribution of where women with HIV were living. Additional purposive sampling was carried out to target harder-to-reach women, including women living in northern Canada, Indigenous women, women not in care and trans-women.
Data collection
Participants completed an online questionnaire (FluidSurveys software; http://fluidsurveys.com) in either English or French administered by a PRA in person, by phone or by Skype. The questionnaire included information on socio-demographic characteristics, HIV-related medical history, health care and service utilization, sexual and reproductive health, stigma and discrimination, substance use, experiences of violence and abuse, wellness, resiliency and quality of life34.
HIV Stigma Scale
The construct of HIV-related stigma includes the prejudice, discounting, discrediting and discrimination that are experienced by people living with or perceived by others to have HIV36. Berger et al37 describe a conceptual framework of perceived HIV-related stigma where perceptions of stigma act as an intermediary between precursors to stigma and possible responses to perceived stigma. This framework informed the development of a psychometrically validated HIV Stigma Scale37, which contains four domains: personalized stigma, disclosure concerns, negative self-image, and concern with public attitudes about people with HIV. The original HIV Stigma Scale contained 44 Likert-type items that were each scored from 1 to 4 (strongly disagree to strongly agree).
Subsequently, a shortened 10-item version, representing all four domains, was created and validated38. The primary outcome was derived from a modified version of this shortened HIV Stigma Scale. In the CHIWOS questionnaire, an additional response option of ‘neither agree nor disagree’ was added as a neutral midpoint to the HIV Stigma Scale because some women may have ambivalent feelings towards some of the items and a neutral midpoint does not force them to choose to agree or disagree. This created a 5-point scale, which was scored from 0 to 4 (strongly disagree to strongly agree). The total score is the sum of each item and ranges from 0 to 40 and the mean stigma score served as the primary outcome for this study. This scoring differs from the unmodified stigma score, which consisted of a 4-point scale and score ranges from 10 to 40. Cronbach’s alpha was 0.87 for the entire scale and 0.90, 0.77, 0.90 and 0.82 for the personalized stigma, disclosure concerns, negative self-image and concern with public attitudes about people with HIV subscales, respectively.
Primary explanatory variable – geographic region of residence
Geographic region of residence was assessed in two separate analyses. The first analysis examined the impact of living in a northern region of Ontario on HIV-related stigma. Participants were categorized as living in a northern region if they lived in the geographic region covered by the Northwestern or Northeastern Local Health Integration Networks39. Participants living in all other Local Health Integration Networks were categorized as living in a southern region.
The second analysis examined the impact of living in a rural region of Ontario on HIV-related stigma. City size was determined by manually categorizing self-reported city, town or area of residence into rural versus non-rural based on populations from the 2011 Statistics Canada Census Profile40. Participants from a city, town or area with a population of <30 000 people were defined as rural based on the Statistics Canada definition of a small population centre41.
Covariates
Potential covariates (Table 1) were selected on the basis of reported associations with HIV-related stigma in the literature42-45 and statistical methods (see below) were used to determine inclusion in the final models. Recreational drug use (substances used for recreational/non-medicinal purposes, including illicit drugs, over-the-counter drugs taken in excess of the directions or prescribed drugs taken in excess of prescription) and marijuana use were removed from the model that included northern region as the geographic variable due to collinearity. For descriptive statistics, age was analysed as a continuous variable. All other variables were analysed as categorical. Alcohol use was categorized into no history of binge drinking or heavy alcohol consumption and history of binge drinking or heavy alcohol consumption. Injection drug use (IDU) was categorized into no IDU history, former IDU and current IDU. Participants with missing values of covariates were excluded from the analysis where missing values represented <5% of the total number of participants. For the alcohol variable, response options of ‘don’t know’ and ‘prefer not to answer’ were collapsed into one category and included as a response option because this total was >5% of the participants.
Table 1: Participant characteristics for overall, northern, southern, rural and non-rural regions of Ontario Statistical analysis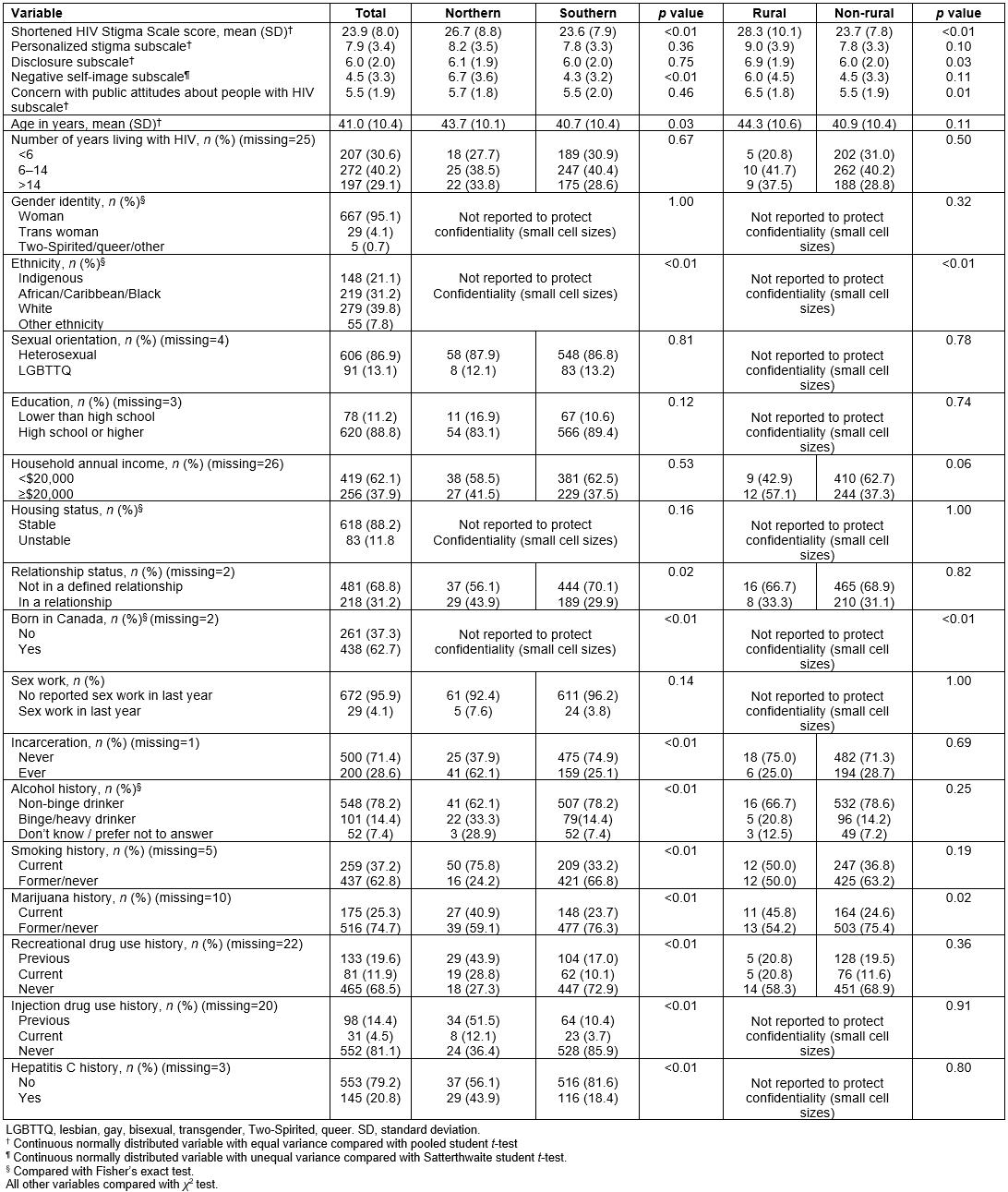
Data quality was assessed by examination of means, medians, minimum values and maximum values for continuous data and frequencies for categorical data. Descriptive statistics were performed for all characteristics for the entire study population and by geographic region. For all statistical analyses, all p values were reported as two-sided p values. All statistical analyses were conducted using SAS v9.4 (SAS Institute, https://www.sas.com).
Categorical variables for participants from northern and southern regions and rural and non-rural regions were reported as frequencies and proportions and compared using a χ2 test or Fisher’s exact test if cell sizes were <5. Continuous variables were assessed for normality by evaluating skewness and kurtosis. Normally distributed continuous variables with equal and unequal variances were compared using pooled and Satterthwaite Student’s t-test, respectively, and were reported as means and standard deviations (SD). Assumptions of normality for stigma score subscale scores were based on normality testing for the overall stigma scores.
Assumptions for linear regression were verified. Normality of residuals was tested by examining skewness and kurtosis. Outliers were identified by visual inspection of plots of Studentized residuals, and a sensitivity analysis was performed with outliers removed. A straight-line relationship and homoscedasticity were assessed by plotting residuals against predicted values. Collinearity was assessed and variables with a variance inflation factor >10 were removed.
A linear regression model was developed to examine the effect of geographic location on the stigma score. A change of estimate strategy was used to identify potential covariates that resulted in a >10% change in the beta-coefficient of geographic region and these covariates were retained in the multivariable linear regression model. Individual unadjusted and adjusted parameter estimates are presented with 95% confidence intervals (CIs).
Ethics approval
All participants provided voluntary informed consent. Primary ethics approval for CHIWOS was obtained from Women’s College Hospital (approval number 2011-0024-E), Simon Fraser University/University of British Columbia (approval number H12-03326), and McGill University Health Centre (approval number 11-102-GEN) from their respective research ethics boards. The study also received administrative review and approval from the University of Toronto.
Results
Participant characteristics
Sixteen women were excluded due to incomplete stigma scale data. Of 701 women included in the analysis, 66 (9.4%) were from northern regions and 635 (90.6%) were from southern regions. Twenty-four (3.4%) were from rural regions and 677 (96.6%) were from non-rural regions. Participant characteristics are described in Table 1. Data on participant characteristics where cell sizes were ≤5 are not presented in accordance with the study’s privacy policy to reduce the risk of inadvertent identification of participants based on demographic characteristics.
In comparison to participants from southern regions, participants from northern regions were older, and more likely to identify as Indigenous, be in a defined relationship, be born in Canada, have a history of incarceration, report substance use (alcohol, smoking, marijuana, recreational drug use and IDU) and be hepatitis C-co-infected. In comparison to participants from non-rural regions, participants from rural regions were more likely to identify as Indigenous, be born in Canada and report marijuana use.
Participants from northern regions had higher mean stigma scores than participants from southern regions (26.7 [SD 8.8] vs 23.6 [SD 7.9]; p<0.01) (Table 1). Scores for the ‘negative self-image’ subscale were higher among northern participants. All other subscale scores were not significantly different between northern and southern participants. Participants from rural regions had higher mean stigma scores than participants from non-rural regions (28.3 [SD 10.1] vs 23.7 [SD 7.8]; p<0.01). Scores for the ‘disclosure’ subscale and the ‘concern with public attitudes about people with HIV’ subscale were higher among rural participants. All other subscale scores were not significantly different between rural and non-rural participants.
Association between geographic region and shortened HIV Stigma Scale score
In univariate analysis, living in a northern region was significantly associated with higher stigma scores (Table 2). Covariates that led to a >10% change from the unadjusted beta-coefficient of northern were ethnicity, incarceration history, alcohol history and IDU. After adjusting for these potential confounders, northern region of residence remained significantly associated with a higher stigma score. A total of four outliers were identified and a sensitivity analysis excluding these outliers did not significantly alter the results. With these other factors constant, living in a northern region was associated with a 3.05 (95% CI 0.77, 5.32) point increase in the mean stigma score. In the multivariable model, Indigenous ethnicity, other ethnicity and history of incarceration were also significantly associated with higher stigma scores. Former injection drug use was associated with lower stigma scores.
In univariate analysis, living in a rural region was significantly associated with higher stigma scores (Table 3). Covariates that led to a >10% change from the unadjusted beta-coefficient of northern were ethnicity and household income. After adjusting for these potential confounders, rural region of residence remained significantly associated with a higher stigma score. After excluding four identified outliers in a sensitivity analysis, there was no significant change in the findings. With these other factors constant, living in a rural region was associated with a 4.83 (95% CI: 1.37, 8.28) point increase in the mean stigma score. In the multivariable model, Indigenous ethnicity, other ethnicity and household income <$20,000 were also significantly associated with higher stigma scores.
Table 2: Univariate and multivariable linear regression modelling of shortened HIV Stigma Scale onto putative predictors with northern region as the geographic variable (n=680)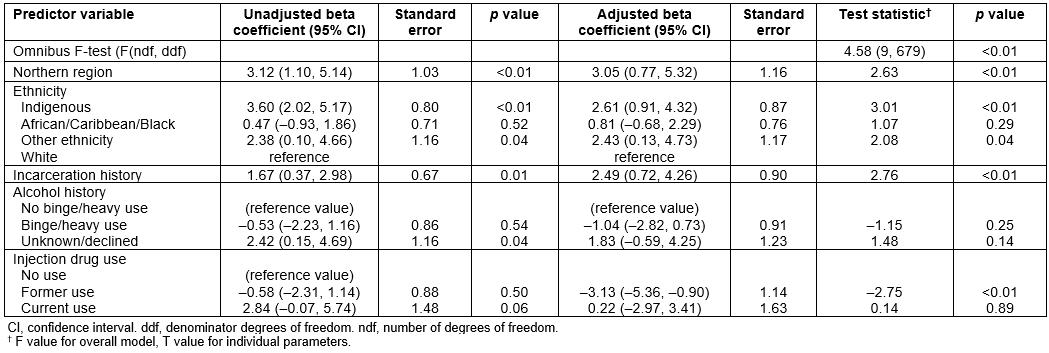
Table 3: Univariate and multivariable linear regression modelling of shortened HIV Stigma Scale onto putative predictors with rural region as the geographic variable (n=675)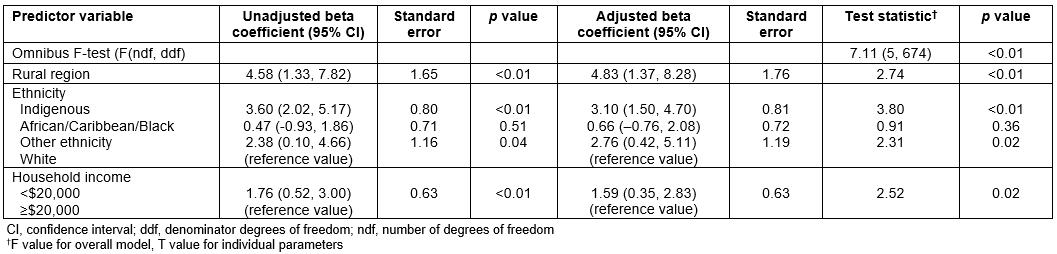
Discussion
Living in northern regions and living in rural regions of Ontario were found to be independently associated with increased perceived HIV-related stigma (higher stigma score) compared to living in southern or non-rural regions. This finding is congruent with prior research identifying stigma as a greater barrier to HIV service utilization in rural compared to urban areas of North Carolina, USA43. Assessing HIV-related and health outcomes in northern and rural Canada is of increasing importance as HIV rates in some of these regions are increasing46. Individuals living in rural regions report lower rates of service utilization and more barriers to service access1,19. As HIV-related stigma can further affect service utilization and health outcomes, this study helps to identify one mechanism through which geographic barriers can lead to poor HIV-related outcomes. Understanding how to support people with HIV living in northern and rural communities and facilitate access to care is crucial, and addressing HIV-related stigma is one important target for intervention. Comprehensive evidence-based programs are needed to address HIV-related stigma, such as those guided by the conceptual framework described by Thapa et al47. General HIV education, peer support programs and interventions targeted to care providers are all needed to reduce HIV-related stigma in rural and northern areas48-50.
Although gaps have been identified in HIV care for people living in rural regions, this finding suggests that northern Canada, including non-rural regions, may have unique challenges for people living with HIV. This finding is particularly important, given the paucity of data on HIV outcomes in northern Canada. The large geographic area in northern Canada can lead to several challenges in the delivery of HIV care and support services, particularly as most models of HIV delivery have been developed in urban settings. The number of physicians and specialists per capita is lower in northern regions of Canada and even larger urban centres are geographically very isolated from the major Canadian cities and their academic centres10. Travel times to seek HIV-specific care may be higher in some northern non-rural communities than in southern rural communities and this can lead to decreased service utilization even in non-rural regions of northern Canada.
Women living with HIV in northern and rural regions of Canada may receive care from providers with less experience in providing HIV care and support for the associated psychosocial complexities. As a significant amount of HIV-related stigma is experienced in healthcare settings51, and good communication with healthcare providers can play an important role in reducing psychological distress for women living with HIV16, this may partially explain the association between geographic location and experiences of stigma. Fragmented HIV care, particularly for people who need to travel long distances to access different services, may also lead to inadequate holistic support for people living with HIV and an exacerbation of experiences of stigma.
Interestingly, using a change in estimate variable selection method, different covariates were identified for inclusion in multivariable models when examining northern region and rural region as the predictor of interest. This suggests that there may be regional variation in how experiences of HIV-related stigma intersect with other types of stigma, and future studies can examine the pathways through which geographic location contributes to HIV-related stigma. Indigenous and other ethnicity were both significant predictors of HIV-related stigma in both models. As many women living with HIV in northern and rural Ontario are Indigenous, experiences of racism may also be contributing to and intersecting with experiences of HIV-related stigma52,53.
Prior research has highlighted increased HIV-related stigma associated with depression in rural areas in comparison to non-rural areas54, positing that rural areas may have less access to HIV prevention, care and support services. In this study, there were significant differences in the ‘negative self-image’ subscale between women in northern and southern Ontario. This may suggested a link between depression and HIV-related stigma in northern areas in addition to rural areas. However, given the large proportion of Indigenous women in northern Ontario, this finding may also reflect experiences of residential schooling and subsequent intergenerational trauma. Social support has been consistently associated with lower HIV-related stigma and self-acceptance55, and the finding that negative self-image was higher in northern areas may be linked with the social isolation and lack of HIV-specific support services, including peer support, for people with HIV in northern areas. Shame is another facet of HIV-related stigma that may be associated with internalized stigma and negative self-image56. Northern contexts may have less HIV education and exposure to people with HIV, therefore less community acceptance, which could be internalized by people with HIV with negative impacts on one’s self-image.
For women living with HIV in rural areas, the stigma subscales that differed significantly from women in non-rural areas included ‘disclosure’ and ‘concern with public attitudes about people with HIV’. This may reflect challenges in confidentiality and privacy in small communities as well as decreased local HIV awareness. Another study conducted in North Carolina also demonstrated increased concern regarding HIV disclosure for people living in rural regions compared to those living in urban regions57.
Current substance use was not found to be a significant predictor of HIV-related stigma. Other studies have found mixed results with regard to substance use and HIV-related stigma: while some report substance use to be associated with higher levels of stigmatizing attitudes towards people living with HIV58, others have reported lower HIV-related stigma among people who use drugs22. The discordance suggests that people who use drugs may have different coping strategies to decrease stigma, or may experience drug use stigma that could overshadow HIV-related stigma. Former IDU was found to be associated with decreased HIV-related stigma and this may suggest that engagement in comprehensive care that addresses both HIV and addictions comorbidities can provide women with the support necessary to address experiences of HIV-related stigma. In addition, many women who have formerly used injection drugs have become engaged as peers to support other women living with HIV. The benefit of engaging people living with HIV as peer research assistants/associates has previously been described59, and empowerment through this process may also reduce the perception of HIV-related stigma.
One limitation is the addition of a neutral midpoint as a response option in the stigma score. Although conceptually, this may allow for participants to select a response that better reflects their perceptions, the psychometric properties of the instrument may be altered through this addition. However, all data in this study were collected using the same response options, and there was adequate internal consistency within this study. Future research will further explore the psychometric properties of the stigma score with this altered response option structure within CHIWOS. This will be particularly important because most of the prior research on the psychometric properties has been demonstrated in predominantly male samples.
A second limitation is that other potential predictors of HIV-related stigma were not captured in this study. For example, social isolation, training experiences of care providers, and visible adverse effects of antiretroviral medications such as lipodystrophy may also affect experiences of HIV-related stigma. Furthermore, this study did not look at the intersection of HIV-related stigma with stigmas associated with race, gender, sexual orientation, substance use or other psychiatric comorbidities.
Another limitation is the cross-sectional nature of this research. Experiences of HIV-related stigma may vary over the lifespan of a woman living with HIV and additional longitudinal research is needed to better understand the factors that affect changes in experiences of HIV-related stigma.
One strength of this study included the community-based participatory research methods that allowed for recruitment of marginalized women, who are often not captured in studies and may experience higher levels of HIV-related stigma. PRAs administered the survey, which may also have allowed participants to feel more comfortable and provide more accurate responses60. Data collection on psychosocial determinants of health, such as housing status, incarceration history, and detailed substance use history, allowed for the assessment of a more complete set of potential predictors of HIV-related stigma than has been possible in prior studies.
Conclusion
In conclusion, living in both northern and rural regions of Ontario was associated with higher HIV Stigma Scale scores. These geographic discrepancies in experiences of HIV-related stigma highlight the need for region-specific programs to reduce HIV-related stigma and to support people living with HIV who are affected by HIV-related stigma.
Acknowledgements
The CHIWOS research team would like to especially thank all of the women living with HIV who participate in the research and entrust CHIWOS with their experiences of HIV treatment, care, and support. We also thank the entire national team of co-investigators, collaborators, and PRAs. We would like to acknowledge the three provincial Community Advisory Boards, and the national CHIWOS Aboriginal and African Caribbean and Black Advisory Boards, and our partnering organizations for supporting the study. In particular, we would like to thank Jasmine Cotnam for her contributions and review of this manuscript in its final stages. DJ is supported by an Ontario Women's Health Scholars Award (Council of Ontario Universities) and the University of British Columbia Clinician Investigator Program.

