Introduction
For the past 10 years, skin cancer has been the most frequent malignant neoplasm in Brazil and worldwide. Each year, there are more new cases of skin cancer than the combined incidence of cancers of the breast, prostate, lung and colon1,2. There were an estimated 188 000 new cases of skin cancer in Brazil in 20163.
In the USA, on average, one person dies from melanoma every hour4. Non-melanoma skin cancer (NMSC), despite having low mortality, may cause physical and psychological damage to patients because these cancers mainly affect regions of the face, disfiguring the patients5.
Skin cancer prevention consists of raising awareness in the population through educational programs and evaluation by a health professional. Skin cancer prevention and screening programs have been implemented by several health facilities, although the costs/benefits of this practice are still under discussion6.
BCH is a tertiary hospital located in the city of Barretos in the state of São Paulo, 430 km away from the capital city, São Paulo. The prevention department of BCH runs some prevention programs for cancers such as breast, prostate, cervical, oral, colon and skin cancers. The skin cancer prevention program comprises educational activities and medical assistance conducted at the hospital and at a mobile unit (MU).
In the literature, there are few reports of the use of MUs in skin cancer prevention programs. There is one MU in Switzerland, which only performs medical evaluations7, and one in Australia, where primary prevention activities are conducted8.
The BCH MU has visited more than 700 cities in nine states in Brazil in the past 10 years. The BCH MU includes a medical outpatient module and a small surgical center. In addition to skin cancer screening, the MU also offers care for the prevention of cervical and prostate cancers. It has the potential to provide medical assistance and minor skin surgeries. The medical assistance is provided by a general practitioner specialising in skin cancer, and an oncological surgeon. The MU’s methodology has previously been published9.
The objective of the present study is to evaluate the use of the MU as part of a skin cancer prevention program, 10 years after the implementation of this prevention program using an MU in remote areas of Brazil.
Methods
The database of BCH was used. These data refer to data collected by the BCH Prevention MU.
The data relate to patients who were seen at the MU from 2004 to 2013. The data for 2004–2007 have already been published, and were complemented with data from 2008 to 20139.
The collected data consist of the total number of appointments, the number of procedures performed (biopsy, excision, cryotherapy), and the number of referrals made (in some cases, due to the size of the lesion or the clinical condition of the patients, they were referred directly to the regular Barretos unit, and the procedure was not performed at the MU). Age, sex and staging of the malignant lesions were other variables for which data were collected. The data are described as absolute and relative frequencies.
Ethics approval
All the informed consent terms were signed by each patients and are currently archived in the prevention department under supervision of the local ethics committee (approval number 377/2010).
Results
A total of 45 872 patients with suspected skin cancer were evaluated at the MU from 2004 to 2013, with an average of 4587 patients seen per year at the MU. Of these, 8954 surgical procedures (excision and/or biopsy) were performed. These patients had a mean age of 64 years, and 50.3% were men and 49.7% were women from nine Brazilian states (São Paulo, Minas Gerais, Goiás, Mato Grosso, Mato Grosso do Sul, Tocantins, Pará, Rondônia, Santa Catarina) (Table 1). The youngest patient was a 21-year-old man, from the state of Rondônia, with a diagnosis of squamous cell carcinoma. The oldest patient was a 99-year-old woman, from the state of Minas Gerais, with a diagnosis of basal cell carcinoma. Among the patients undergoing surgical procedures, 7098 (15.5%) received pathological confirmation of the malignancy. The other 38 774 (84.5%) patients without suspected skin cancer lesions were instructed to continue follow-up with their general practitioner. In relation to malignant lesions, 81.5% had basal cell subtype, 14.5% squamous cell, 1.7% melanoma, 0.7% metatypical, 1.2% Bowen disease, and 0.4% had two other subtypes (dermatofibrosarcoma and Merkel cell) (Table 2). Among the nonmelanoma cancers, 85.7% were diagnosed at stage 0 or 1, whereas 85.9% of the melanomas were diagnosed at stage 0 or 1 (Table 3). Two cases of Merkel cell carcinoma were diagnosed, one patient at stage 2; the other patient chose to continue treatment at a different hospital unit, and hence the BCH do not have follow-up data. Two cases of dermatofibrosarcoma were diagnosed, one at stage 3; the other patient also preferred to continue treatment at another hospital unit.
Table 1: Gender, age and state of origin for patients evaluated at Barretos Cancer Hospital mobile unit, 2004–2013 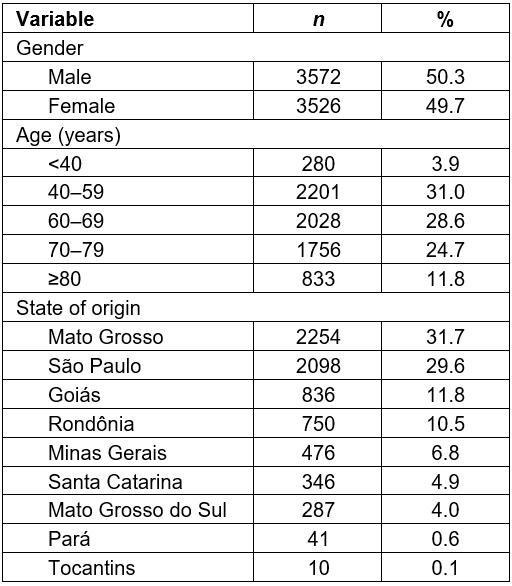
Table 2: Skin cancer subtype for patients evaluated at Barretos Cancer Hospital mobile unit, 2004–2013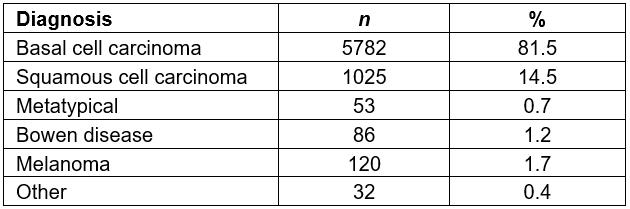
Table 3: Clinical stage for skin cancer of patients evaluated at Barretos Cancer Hospital mobile unit, 2004–2013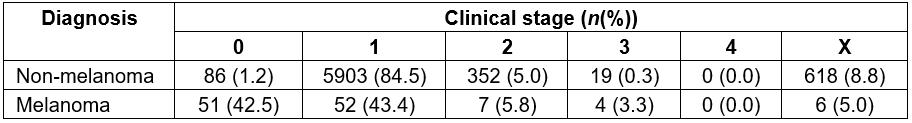
Discussion
Brazil, a developing country with a large territory and significant social inequality, has an insufficient health system designated the universal health system (sistema universal de saúde, SUS). The SUS, whose pillars are equity, universality, comprehensiveness, decentralization and social monitoring, cannot provide quality assistance to the entire Brazilian population for several reasons. One of the reasons may be the difficulty in retaining physicians in regions far from large urban centers. For example, in the state of Amazônia, there is one dermatologist for every 90 000 residents10. There is an unequal distribution of physicians in Brazil, with the majority preferring to live in large cities11. Several policies have been attempted to retain physicians in peripheral regions; the most recent was the More Doctors Program adopted in 2014, a program highly criticized by clinicians and that still awaits effectiveness data12.
In Brazil, in the 1970s, some federal incentive programs for the colonization of the northernmost regions of Brazil were carried out by the federal government through tax incentives and facilitated credit. This led to migration of European descendants, who lived in southern Brazil, to colonize the northern region, whose main labor market in this region was and is still agriculture13.
In addition to the scarcity of physicians in remote areas, which can delay an early diagnosis of skin cancer, is the important factor of tropical climate. A high incidence of UV radiation and an annual mean temperature of approximately 24°C14 promote the development of skin cancer. In addition, 17% of the Brazilian population works and lives in rural regions15.
The hottest regions of Brazil (north and central eastern) were colonized mainly by European descendants, with type I and II Fitzpatrick skin types16, and these people work in agriculture. These factors have accentuated the incidence of skin cancer in this region17,18.
BCH receives patients from all over Brazil, and every appointment and treatment is free of charge. Approximately 4000 appointments each day are held at the hospital, which has a medical team of 350 specialized health professionals. The hospital has been conducting work on prevention, diagnosis, treatment and research in oncology and is recognized at national and international levels19,20.
The skin cancer prevention program implemented by BCH comprises educational and care components. In addition to several lectures targeting the general population, it also trains health professionals from several cities in Brazil. These health professionals receive training for 3 days on the prevention, diagnosis and treatment of skin, oral, breast, prostate and cervical cancers.
The patients seen at the MU are screened by the city’s nurse, who received prior training at BCH. During the training conducted at BCH, these health professionals learn how to conduct screening of the population in their cities. When a patient with a complaint of a skin lesion comes to the city’s health unit, the health professional, usually a nurse, initiates the screening, and if the nurse suspects the skin lesion to be a malignancy, the patient is referred for assistance at the MU, whenever it is at the patient’s city. There was a significant improvement in the screening conducted by the nurses after the 3-day training was implemented at BCH. The percentage of patients with skin cancer detected by the nurses after the training increased from 12% to 30%.
The MU visits the Brazilian cities once a year. There is the option for the local nurse to refer a patient with a suspected lesion to another oncology department, which is routine for places where MU does not visit. However, the operation of these services at the places visited by the MU is difficult, due to either the absence of specialists near these cities or difficulties in transportation to the nearest referral center. Therefore, the majority of the patients identified by the nurse prefer to wait for the MU.
The MU has been well received by the population in these cities, mainly due to the convenience of the unit – the MU is capable of training, and diagnosing and treating skin cancer in a patient’s own city, without the need for travel and, consequently, without unnecessary patient costs. A total of 92% of the lesions diagnosed at the MU are treated at the MU itself. Only 8% of the patients must be referred to the BCH, mainly due to lesion size. These patients immediately receive a date for their appointment at the BCH, and the Health Bureau of their own city is responsible for their transportation. At present, the BCH has 17 MUs, but only one performs skin cancer surgeries.
With the implementation of this prevention program by the BCH through the MU, it was observed that, during the 10 years of operation, a flow of referrals to the MU and expectation for arrival of the MU to the cities was generated. All of the assistance provided at the MU is free of charge.
BCH prevention department staging data (Table 3) were compared with the general BCH data (Table 4) – cases that are referred to BCH by basic health units, not through the skin cancer prevention program from BCH. In these referrals, the patient already has a biopsy with a positive result, with the diagnosis made by the health team of the municipality. This may have generated some delay, both in diagnosis (because there are not enough specialists in Brazil)10, and in delays due to the bureaucracy of the Brazilian health system. Connecting a patient with a specialist physician begins with a request from the general practitioner to the municipal health department, and this requests the state health department to look for a vacancy for the patient in an oncological hospital. These requests are time consuming.
Through these data, it was observed that the patients diagnosed by the prevention department, whose objective is to offer the opportunity of a specialized treatment in their municipality, not requiring referrals to other referral centers, presented 0.3% staging 3 and 4 in relation to NMSCs and 3.3% for melanomas. For patients referred to the BCH by a local doctor in their city, 1.4% of patients with staging 3 and 4 were NMSCs and 27.3% staging 3 and 4 for melanomas, a significant difference. For 505 patients with these NMSCs, lesions were larger than 5.0 cm in the skin – that is, they should have been easy to diagnose, rather than have a late-stage diagnosis with consequent increased mortality. In relation to melanoma, there was a very important difference in the number of late diagnoses (27.3% v 3.3%).
Skin cancer prevention initiatives are highly cost effective and may also be cost-saving. There is a significant cost burden of skin cancer for many countries, and health expenditure for this disease will grow as incidence increases. Public investment in skin cancer prevention and early detection programs show strong potential for health and economic benefits21. A cost%u2010effectiveness evaluation of the Australian SunSmart program demonstrated a reduced burden of disease and high cost%u2010effectiveness22.
Opportunistic screening for skin cancer for the general population has insufficient evidence to support its practice since it does not provide a reduction in the overall mortality of the screened population6. It is indicated for the high risk population: Fitzpatrick I and II skin type men and women older than 65 years, atypical moles, more than 50 moles, a personal history of melanoma or a strong family history of melanoma23,24. The MU provides assistance to remote communities of patients previously selected by a local health team, while performing a punctual actions like small surgeries, and some longitudinal actions, such as cancer education training for health professionals in these communities.
With the aim to improve this prevention program, the BCH initiated a skin cancer screening modality through teledermatology in 2014. Its methodology and results will be published soon.
Table 4: Clinical stage of skin cancer, Barretos Cancer Hospital Registry, 2004–2013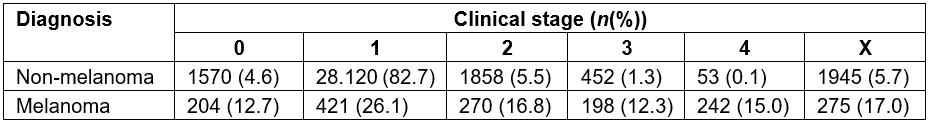
Conclusions
This study demonstrated a significant number of skin cancer cases diagnosed and treated by the MU, showing that the MU positively contributes to the early diagnosis and treatment of skin cancer among populations residing in remote areas of Brazil.
References
You might also be interested in:
2018 - Health Disparities in Rural Communities: Challenges and Opportunities
2001 - The impact of health system reform on remote health in Cambodia and the Philippines