Introduction
For many pregnant women and their medical team, an emergency arising during pregnancy is a critical and stressful situation. In rural areas, these situations have the added complexity and increased risks of occurring without immediate access to maternal and neonatal intensive care units or obstetricians and neonatologists available at a tertiary perinatal centre (TPC). Antenatal transfer of obstetric patients to a hospital capable of providing optimal perinatal care is a necessary process in rural areas for emergency and high risk presentations. Antenatal or in utero transfer is preferred as there are improved outcomes for at-risk neonates who are born in TPCs, compared to post-natal transfers1. Women who do not deliver after their transfer are faced with organising their own return transport home or local accommodation. Furthermore, there is limited public transport, and there are currently no provisions for accommodation of their partners or family. In South Australia, approximately 18.6% of women (n=3678) giving birth delivered in rural or remote areas2. This proportion has been decreasing over the years and may be associated with closure of rural maternity units, workforce participation and safety concerns3. Globally, approximately 15% of women experience life-threatening complications during their pregnancy or labour4. In South Australia, obstetric complications requiring medical assistance are recorded for 43.9% of women who give birth2. However, the severity of the complication is not reported, and it is unknown how many of these women reside rurally because they may be retrieved or transferred to TPCs and therefore, the location of obstetric emergencies is not recorded.
Women with a singleton pregnancy greater than 37 weeks and deemed to be low risk can deliver in rural areas, but it is best practice that women with high risk pregnancies are encouraged to move nearby to a TPC from approximately 37 weeks5. The decision to determine if a woman fits into the low risk category is a clinical judgement, and no specific criteria exists regarding who is low risk. Data from Queensland reports that nearly 66% of women with a low risk pregnancy end up delivering in their rural area; of this low risk population, 13% require antenatal transfer and 11% are transferred in the intrapartum period6. Despite best efforts, women are often still living in rural communities when an obstetric emergency occurs due to the unpredictable nature of pregnancy, the cost of relocating and the disruption to their lives. The main reasons that women are likely to be transferred from a rural hospital to a TPC in an emergency are preterm premature rupture of membranes (PPROM; defined as rupture of membranes prior to 37 weeks gestation), premature labour with intact membranes (defined as regular contractions or dilatation of the cervix greater than 4 cm prior to 37 weeks gestation), pre-eclampsia and antepartum haemorrhage (APH)7,8. Women with high risk pregnancies who are transferred acutely because of the likelihood of imminent delivery do not all deliver immediately. In recent decades, the rate of delivery at the accepting hospital during the same admission has been estimated to be 62–64%7,8, and higher rates for those delivering at a preterm gestation (76%)8. One study recently reported a 71% rate of delivery on transfer within 7 days of an emergency obstetric transfer, which suggests a trend toward even higher rates of delivery on transfer9. However, this is a distinct contrast with a study from New South Wales based on data collected in 2010–2011, which concluded that 40% of women delivered at the receiving hospital and 45% were discharged undelivered10.
It has been suggested that screening tests could be used to reduce the need for maternal air transport7. There is good evidence that reviewing serum levels of interleukin-6, foetal fibronectin testing and performing vaginal ultrasound can provide a satisfactory degree of predictive value for preterm birth beyond digital cervical examination and patient history11. Vaginal ultrasound and interleukin-6 blood testing are not routinely available in rural hospitals due to clinician skill levels and the availability of pathology laboratories. However, foetal fibronectin is available in hospitals and is accurate in predicting spontaneous preterm birth within 7–10 days of testing among women symptomatic of preterm labour before advanced cervical dilatation12. Accurate identification of patients who will require transfer is a clinical judgement, but the urgency of their transfer can depend on the clinical indications and resource allocation available. Undoubtedly, the neonatal and obstetric benefits of a transfer must be balanced against maternal preference and healthcare expenditure.
The present study was based in a regional area in South Australia known as the Riverland. The Riverland is a large rural region covering 9386 km2, approximately 255 km north of a TPC in South Australia. Three hospitals in the region provide maternity services for a population of approximately 42 000 people13. In terms of obstetric care, the region is serviced by general practice obstetricians, a locum sole obstetric practitioner and no neonatologists. Women with a low risk singleton pregnancy, >37 weeks, may deliver in these hospitals5. In the situation where a clinician determines that a pregnant woman necessitates an emergency transfer to a TPC, the transfer of that patient is negotiated between individual receiving hospitals and the emergency transport required (MedStar/Royal Flying Doctor Service). The most acute emergencies are transferred via a MedStar helicopter and the less acute emergencies are transferred via the Royal Flying Doctor Service planes.
There is no published data on the factors that influence decision making in pregnancy-related transfers, and a lack of recent research that looks at rural transfers in Australia. The aim of this study was to explore the clinical reasons and number of obstetric transfers from a rural area and determine the outcomes of transfers in terms of timing and location of delivery. As a secondary outcome, the association between delivery after transfer and clinical reasons for transfer was also examined.
Method
Participants
Participant information was included in the study and analysed based on a search of hospital coding data. The inclusion criteria were all women from the Riverland transferred antenatally for a pregnancy of >20 weeks gestation for acute admission to a TPC from 1 January 2010 to 31 December 2015.
Procedure
Data were collected from a review of patient medical records and was entered into a spreadsheet by the principal investigator (AR). The clinical reasons for transfer and demographic data were obtained by review of case notes, copies of antenatal records and hospital coding data. Demographic data (including age and postcode) and admission data (including reason for admission, principal diagnosis on transfer, length of stay and mode of transport for transfer) were recorded from hospital coding data. The clinical reason for transfer, management at the original hospital and obstetric history, including parity and location of birth if delivery did not take place as part of the transfer, was recorded from the hospital case notes. The outcome in terms of time to delivery and actual delivery on transfer was recorded from the discharge summary included in the hospital case notes. Records regarding the total number of births per year were supplied from the relevant hospitals including the number of births per year.
Data analysis
The data were analysed using SPSS Statistics v23 (IBM; http://www.spss.com). Summary descriptive statistics were calculated for the maternal demographic statistics and details of the acute presentation. Adjusted odds ratios were calculated after multiple logistic regression analysis. Hosmer–Lemeshow goodness-of-fit tests, residual and influence analyses were performed. The logistic regression models presented adequately fitted the data. Significance was accepted at the 5% confidence interval on two-tailed tests for all measures.
Ethics approval
This study received ethics approval from the South Australian Department for Health and Ageing Human Research Ethics Committee (HREC/15/SAH/143).
Results
During the study period, there were 160 acute antenatal transfers. Five women were transferred twice during their pregnancy and one woman was transferred three times. Over 5 years, there were approximately 1669 births from this region, giving a region-wide transfer rate of 87 transfers per 1000 births. There were 32 neonates transferred during the same time period. A total of 149 (93.2%) transfers occurred before 36 weeks’ gestation; and of these, 99 (66.4%) delivered before 36 weeks (Table 1). Indications for transfer are shown in Table 2.
The median gestation at transfer was 33 weeks (interquartile range 30–35 weeks). There were no deliveries during transfer. Seventy percent of women had more than one indication for transfer, and 6.9% of women had greater than four recorded reasons for transfer. The number of indications was not associated with likelihood of delivery on transfer (p=0.77).
Out of the women who were ≤34 weeks pregnant (n=106), 67 were transferred primarily due to premature labour (63.2%), and of these 22 had a foetal fibronectin test performed (32.8%). There were 12 positive results and 10 negative results. There were 80 women (75.5%) who were administered tocolytic medication who were <34 weeks pregnant, and 66 (62.3%) who were given antenatal steroids.
Table 1: Descriptive statistics for acute antenatal transfers (n=160) from Riverland region, South Australia, 2010–2015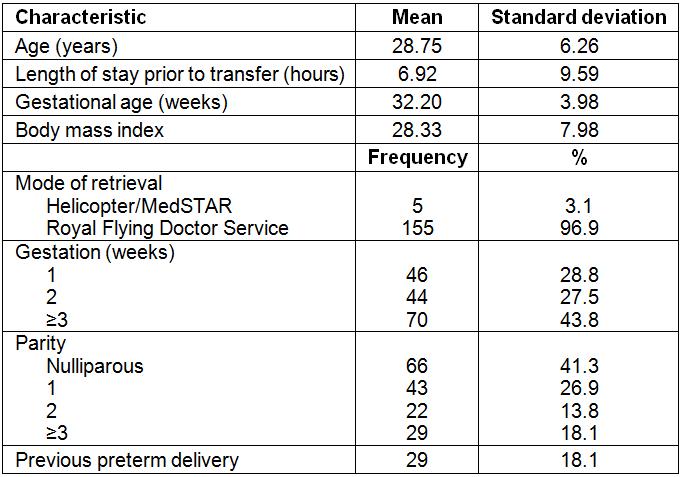
Table 2: Indications for retrieval for acute antenatal transfers (n=160), and assessment results, from Riverland region, South Australia, 2010–2015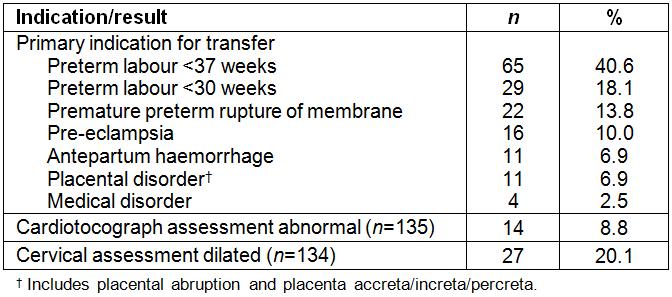
Outcome after transfer
There were 56 (35.0%) women who delivered at the hospital to which they were transferred. Of the remaining 104 women who were discharged while they were pregnant, 45 (43.3%) women eventually delivered at their rural hospital and the remaining 59 (56.7%) were stabilised and delivered post-discharge in the TPC as part of a planned admission. For women who delivered at the TPC, the mean number of days until delivery was 4.34 (standard deviation=9.54) and the majority (n=35, 62.1%) delivered within 24 hours.
No women who were transferred for PPROM, and one woman transferred for pre-eclampsia, returned to their rural hospital for delivery. A significant proportion (n=31, 86.7%) of women transferred for preterm labour were discharged while pregnant and returned to their rural hospital for delivery (χ2=39.5, degrees of freedom=8, p<0.005).
A logistic regression analysis was performed to assess the impact of several factors on likelihood of delivery on transfer (Table 3). Pre-eclampsia and PPROM were associated with increased likelihood of delivery on transfer. Gestational age, total number of risk factors, placental problems, premature labour and cervical dilation did not make a significant contribution to the model.
Table 3: Factors associated with delivery on transfer at receiving hospital for acute antenatal transfers (n=160) from Riverland region, South Australia, 2010–2015 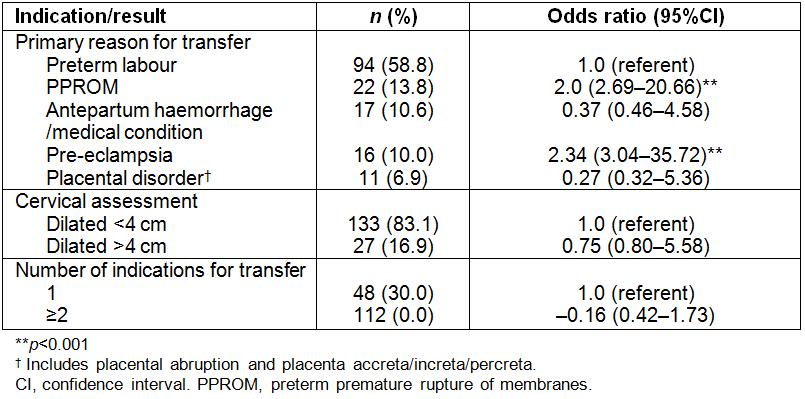
Discussion
The present study presents demographic data on emergency obstetric transfers from the Riverland. Despite a notable proportion of women requiring emergency obstetric transfer during their pregnancy, only 35% delivered their baby at the receiving hospital.
The main reasons for transfer in the present study were preterm labour, PPROM, pre-eclampsia, APH and placental disorders (which refer to placental abruption and placenta praevia). This is mostly consistent with the main reasons for transfer reported by Roberts et al8. They reported that pre-eclampsia was one of the main reasons for transfer and was associated with a significantly greater likelihood of delivery on transfer. The present study found that delivery on transfer was more likely if the primary reason for transfer was pre-eclampsia or PPROM. Delivering on transfer was not associated with preterm gestation, evidence of preterm labour including cervical dilatation >4 cm or an increasing number of indications for transfer. A large proportion of women were discharged from the TPC and eventually delivered their baby in their rural hospital. The present study reports a substantially lower rate of delivery on transfer compared to previous research (35% v 62–71%)7,8 but does report a similar delivery outcome to more recent research by Goh et al suggesting that this may reflect a trend over time to a decreasing ratio of delivery to transfer10. One reason for the differences in delivery on transfer rates may be that, in this region, a large proportion of women have a planned admission to a TPC from 37 weeks if they have a high risk pregnancy5. Therefore, those women with clear indications for early delivery in high risk pregnancies should have relocated to be living closer to a TPC. The guidelines state that high risk women of <37 weeks with multiple pregnancies should deliver in a TPC; however, what constitutes ‘high risk’ is not specified, therefore, there are no clear guidelines about when to transfer.
Goh et al reported that the number of total indications for transfer was associated with likelihood of delivery on transfer, which was not supported in this study10. In this population, it appears that pregnant women are being transferred based on specific emergency presentations rather than cumulative risk factors.
Nearly a third of women who met the criteria for foetal fibronectin testing had this test performed. In addition, of patients who met the criteria for the use of the foetal fibronectin test, 10 women with a negative result were still transferred to a TPC, suggesting that clinicians are not relying on this test to determine probability of impending delivery. It is unknown whether a more diligent approach to the use of foetal fibronectin testing would decrease the number of transfers to TPC for impending delivery that result in a return to the rural hospital for delivery. The rates of emergency transfers may also reflect the available staffing at the time of the incidence, the level of clinical expertise and available resources, which were not able to be assessed.
This study is limited by its retrospective design and reliance on documentation in hospital records. Potential sources of bias could be reduced by multiple researchers reviewing the data sources. The data was collected from only one region in rural South Australia and may not reflect the experience in other rural areas, which may differ in terms of resources, personnel and distance from a TPC. The study contributes as a foundation for further research to determine if the current care model is adequately supporting the clinicians and patients involved in emergency obstetric transfers, particularly because such a high proportion return to their rural area while still pregnant. A qualitative component that directly addresses the issues faced by clinicians with regards to obstetric emergency transfers would improve the external validity of this study.
Conclusion
This retrospective, population-based clinical evaluation of all maternal transfers in a rural region of South Australia provides a foundation for understanding the burden of obstetric emergency transfers on the healthcare system, rural women and their families. In general, there is a lack of rigor around maternal transfer, which is a substantial and expensive intervention in pregnancy. The number of women from regional areas who have been identified antenatally as high risk and relocated closer to tertiary hospitals should have the effect of reducing the number of emergency transfers; however, this has never been evaluated. This study provides updated information about outcomes of women who are transferred in an obstetric emergency, the clinical reasons for their transfer and the association between reason for transfer and outcome. Birth is an unpredictable event and rural hospitals and doctors still must maintain high level obstetric skills to manage the number of emergency transfers. Rural clinicians should be supported to develop and maintain vital skills in managing emergencies in pregnancy and a high rate of transfer needs to be coupled with adequate support services for rural women and their babies. Further information about the decision making involved in transfer is important for improving education around this issue.


