Introduction
Cancer outcomes in Australia have been reported as among the best in the world1. However, a growing body of research has demonstrated there are large disparities in cancer outcomes between Indigenous Australians (Aboriginal and Torres Strait Islander people) and non-Indigenous Australians. Indigenous Australians are more likely to be diagnosed with advanced stage disease1,2, receive less optimal treatment2,3, be diagnosed with more aggressive cancers4 and have poorer cancer survival5,6. The reasons underlying these disparities are thought to be multifactorial and include higher prevalence of comorbidities7,8, greater social disadvantage9, restricted access to cancer and support care services10, and differences in cultural understandings of cancer and its treatment11,12.
Receiving a cancer diagnosis and subsequent treatment may present numerous psychological, physical and practical challenges for the patient13-15 and their family16,17. ‘Supportive care’ is a broad term used to refer to services, both generalist and specialist, that may be required by those affected by cancer. Supportive care addresses a wide range of unmet needs across the continuum of care and is increasingly seen as a core component of evidence-based clinical care18. Needs assessments identify and prioritise unmet needs from the patient’s perspective and the degree to which they require assistance from services. As such, unmet needs assessment can lead to better patient outcomes and provide the evidence necessary to redesign services and improve resources for people with cancer19.
A study undertaken in the state of Queensland, Australia20 developed and validated a culturally specific tool to assess the unmet supportive care needs of Indigenous cancer patients and reported the prevalence of unmet needs among this group. The most frequently reported moderate to high unmet needs in this study were money worries (29%), and unmet needs related to physical and psychological concerns20.
While these results identified the unmet needs among Indigenous cancer patients in Queensland, to date no information on the unmet needs of Indigenous cancer patients is available for the other Australian jurisdictions. As Australian states and territories differ in their geography and socioeconomic indices, which are likely to impact upon access of cancer and healthcare services, the assessment of the unmet needs of Indigenous cancer patients in other states/territories is warranted.
The purpose of this multicentre study was to use a culturally specific tool to assess the supportive care needs of Indigenous Australian cancer patients and describe the prevalence of unmet need across the participating jurisdictions.
Methods
Study setting, patients and procedure
This multicentre study involved a tertiary metropolitan hospital in Victoria, regional cancer care and chemotherapy outreach centres in New South Wales and Northern Territory, and the Cancer Council Western Australia regional cancer support coordinator program. These institutions (referred to here as ‘centres’) vary in terms of geographic location, demographics of their service population, access and types of services they provide.
Patients were Indigenous Australians diagnosed with cancer within the previous 5 years, aged 18 years and older.
Local staff (cancer care coordinators, Indigenous liaison officer, registered nurses and social workers) recruited patients who were attending one of the study centres over a 12-month period (2014–2015). The patients’ supportive care needs were assessed during a face-to-face interview held at a time convenient to participants. Staff made appropriate referrals for participants if unmet needs were identified during the interview. There were eight interviewers across the study sites, of which two were Indigenous Australians. The interviewers received standardised training using materials that were co-developed, conducted and guided by an Aboriginal senior researcher (GG). Recruitment strategies were adapted at each site to capture the local context. All participants provided written informed consent and were advised that withdrawing from the study would have no consequences for their treatment and care.
Instrument and data collected
The culturally specific and psychometrically tested Supportive Care Needs Assessment Tool for Indigenous Cancer Patients (SCNAT-IP)20 was used to assess the needs of the patients recruited into the study. This tool has 26 items across four domains: ‘physical and psychological’ (11 items), ‘hospital care’ (4 items), ‘information and communication’ (6 items), and ‘practical and cultural’ (5 items). It uses a five-point scale to measure unmet need: 1=‘no need’, 2=‘satisfied with the help received’, 3= ‘needed a little more help’ (referred to as ‘low need’), 4=‘needed some more help’ (‘moderate need’) and 5=‘needed a lot more help’ (‘high need’). For this study, moderate and high needs were collapsed into one category (‘moderate to high need’).
At the time of the needs assessment, the staff members also captured patient-reported sociodemographic information. This included age at cancer diagnosis (categorised as 45 years or younger, 46–59 years, and 60 years or older), marital status (married or partnered v other), main language spoken at home (English v other), education level (higher than completion of year 10 v year 10 or less completed) and employment status (employed v not employed). Address information was also collected, including each patient’s community name, postcode and state. This information was then used to assign patients an Accessibility/Remoteness Index for Australia (ARIA+) 2011 score, which was then categorised into one of five remoteness categories21. Due to small participant numbers, these were collapsed into three categories: ‘major city’, ‘inner/outer regional’ and ‘remote/very remote’. Residential information was also used to assign patients to a percentile of the Socio-economic Indexes for Areas (SEIFA) Index of Relative Socio-economic Advantage and Disadvantage (IRSAD)22. These were then categorised as ‘most disadvantaged’ (percentile 1–33), ‘moderately disadvantaged’ (34–66), and ‘least disadvantaged’ (67–100)22.
Clinical data were extracted from medical charts using a standard form in Northern Territory, New South Wales and Victoria. In Western Australia, clinical data were obtained from referral letters or self-reported. Clinical data collected included cancer type, date of diagnosis (categorised as less than 1 year prior to interview, 1–2 years prior to interview and more than 2 years prior to interview), cancer stage (localised, regional spread, distant metastatic spread, not applicable and unknown stage), comorbidities (diabetes, hypertension, cardiovascular disease, renal disease and respiratory disease), number of comorbidities (0, 1, 2–5), current treatment (had started but not completed a regime of chemotherapy, radiotherapy or hormone therapy at the time of interview) and past treatment (past receipt of surgery, completed chemotherapy or completed radiotherapy at any time prior to the interview).
Data analysis
Participant demographic and clinical characteristics are described. For each SCNAT-IP item the proportion of patients who had no unmet need (no need or satisfied need), little need, and moderate to high need are reported. Also reported are the proportion of patients who did not have unmet need for any of the 26 SCNAT-IP items; had at least one moderate to high unmet need, overall and within each SCNAT-IP domain; and had at least five items with moderate to high unmet needs. The median number (interquartile range (IQR)) of moderate to high unmet needs reported by patients is also presented.
For most of these outcomes, the results are presented for the multicentre study overall (n=145) and for Northern Territory (n=75) and New South Wales (n=46) separately. For comparison, the results for the previous Queensland study20 are also presented. This information is not reported separately for Victoria and Western Australia, due to small participant numbers in these jurisdictions.
Statistical analysis was conducted using the Statistical Package for the Social Sciences v20 (IBM Corporation; http://www.spss.com).
Ethics approval
The study was approved by the Human Research Ethics Committees of Charles Darwin University, Northern Territory Department of Health and Menzies School of Health Research (HoMER 13-2038) and by the relevant states and territory institutional human research ethics committees (HREC/13/HNE/466; HREC-058/14; SSA/13/HNE/531), including the Aboriginal Health and Medical Research Council of New South Wales (ref. 938/13) and the Western Australian Aboriginal Health Research Ethics Committee (ref. 544).
Results
Patients’ characteristics
A total of 284 cancer patients were identified across the four participating jurisdictions (Fig1). Of those, 198 (70%) patients were approached and 86 (30%) patients were missed (did not answer telephone calls, failed to attend appointments or no staff member was available to approach the patient). Of the patients approached, 170 (86%) patients were eligible for the study and, of these, 145 (85%) were interviewed.
Patient demographic and clinical characteristics are described in Table 1. Patients (57% female) were diagnosed at a median age of 57 years (IQR 47.5–64.5 years). On average, interviews were conducted just over 5 months after cancer diagnosis (median 158 days, IQR 53–497 days). The most common cancers among participants were digestive system (23%) and breast (21%) cancers; 36% of patients were diagnosed with localised disease. Most patients lived in inner or outer regional areas (33%) or in remote/very remote areas (48%), and the majority of patients lived in the most disadvantaged areas.
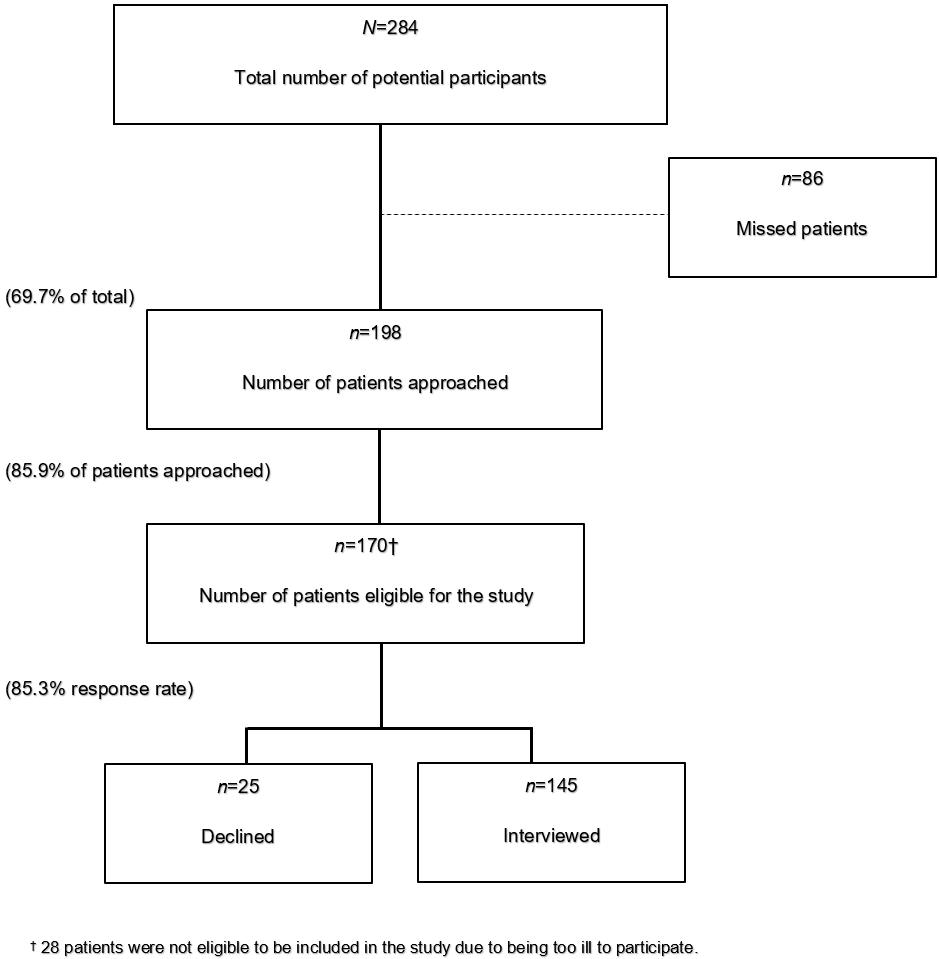 Figure 1: Patient recruitment flowchart.
Figure 1: Patient recruitment flowchart.
Table 1: Demographic and clinical characteristics of Indigenous cancer patients in multicentre study across Australia (N=145)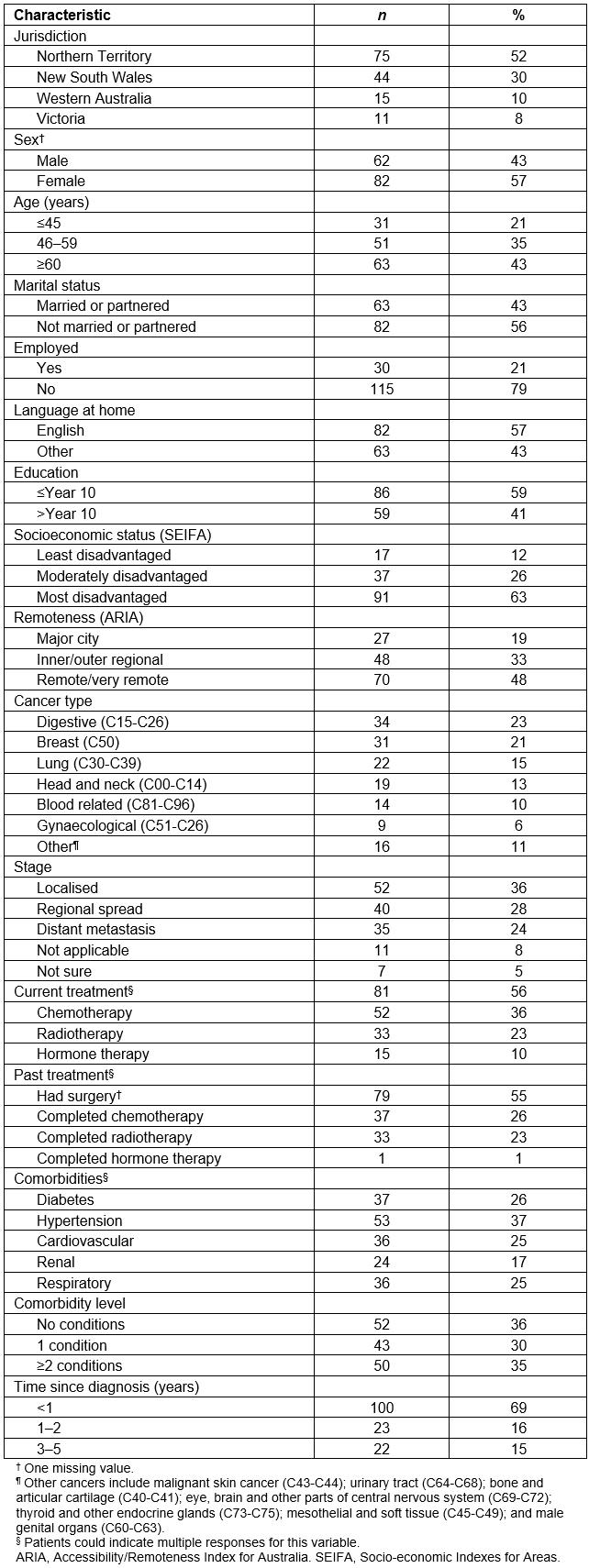
Proportion of needs by domain and items
There was a wide variation in the unmet needs reported by Indigenous cancer patients across study jurisdictions. Overall, 65% of patients reported at least one moderate to high unmet need, 20% of patients had moderate to high unmet needs on five or more items and only 16% of patients reported no need or satisfied need across all SCNAT-IP items. A greater proportion of patients reported moderate to high unmet needs in the physical/psychological domain (46%) and the practical/cultural domain (34%) than in the information/communication domain (23%) or the hospital needs domain (16%). This pattern was also observed separately for Northern Territory and New South Wales patients (Fig2).
While across the jurisdictions the most frequently reported moderate to high unmet need item was ‘money worries’ (20%) from the practical/cultural domain (Table 2), there were differences in terms of priority of the unmet need items. In the Northern Territory, for example, unmet need with ‘money worries’ was reported by 23% of patients (rank 1) compared with 16% in New South Wales (rank 7) (Table 3).
Table 2: Proportion of unmet need among Indigenous Australians cancer patients 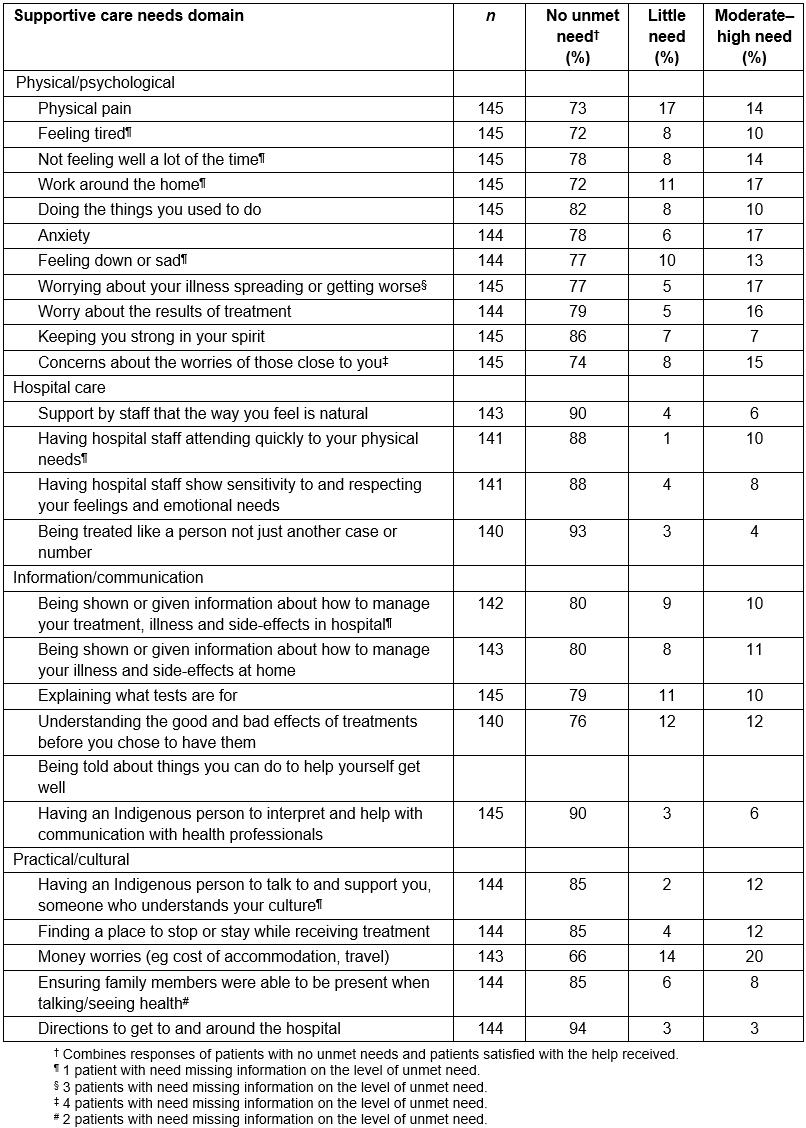
Table 3: Ten most frequently reported moderate to high unmet need items across three jurisdictions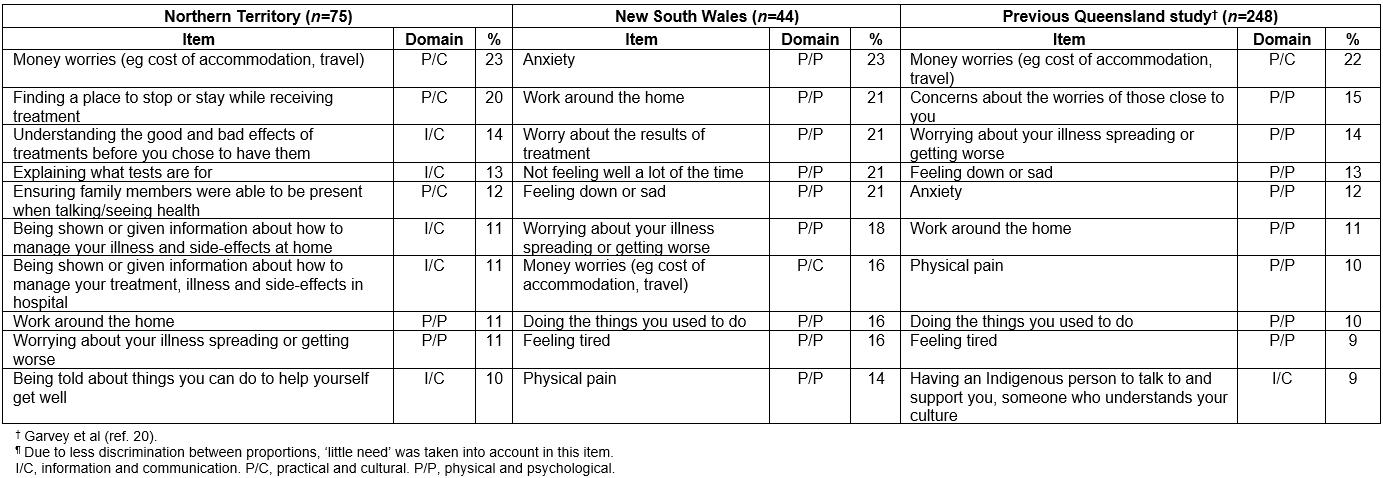
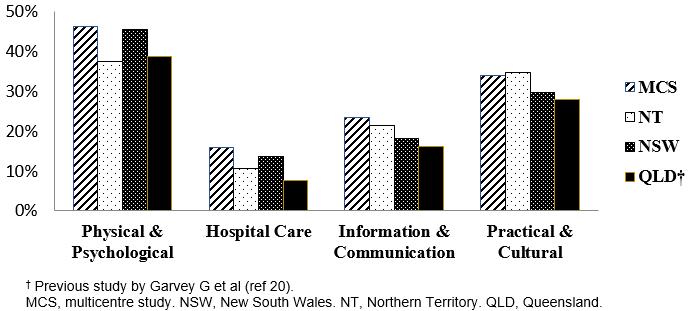 Figure 2: Proportion of unmet needs by domain and jurisdiction.
Figure 2: Proportion of unmet needs by domain and jurisdiction.
Comparison to previous Queensland study
Similar to what has previously been reported in Queensland20, patients in the current multicentre study were more likely to report unmet need in the physical/psychological domain and the practical/ cultural domain than in other domains (Fig2). Also, patients in the current multicentre study most commonly reported unmet need with money worries (Table 2). Unmet needs related to information/communication were more frequently reported in the current multicentre study (Table 3).
Factors associated with unmet needs
In the present study, most patient demographic and clinical characteristics (ie age, sex, place of residence, area-level socioeconomic disadvantage, cancer type, stage at diagnosis, current treatment receipt and comorbidity) were not associated with moderate to high unmet need. Exceptions were that a higher proportion of patients who had respiratory disease reported moderate to high unmet need with ‘money worries’ compared to those without this comorbidity (9% v 24%, p=0.047) and a higher proportion of patients with renal disease reported moderate to high physical and psychological unmet needs than those patients without this comorbidity (50% v 25%, p=0.023).
More patients who had been diagnosed with regional spread or distant metastatic cancer reported moderate to high unmet hospital care needs (23% v 8%, p=0.026) when compared to those diagnosed with localised disease. A greater proportion of patients diagnosed with respiratory cancer than those diagnosed with digestive system cancers and breast cancer had moderate to high domain need, except in the hospital care domain. The unmet domain needs for the three most common cancers in this sample are described in Figure 3.
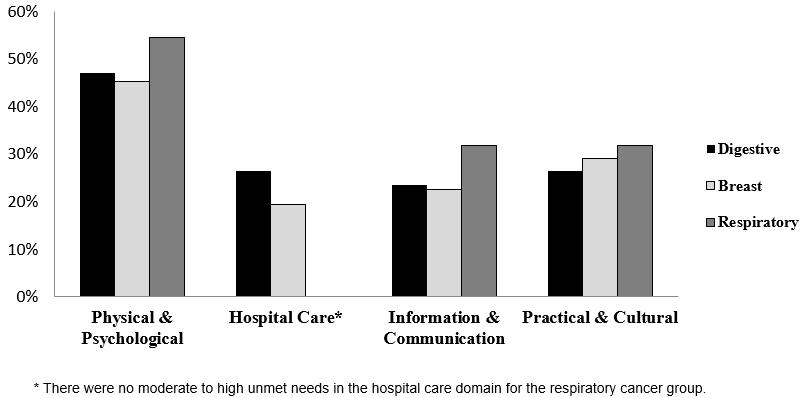 Figure 3: Proportion of patients with moderate–high unmet needs by cancer type.
Figure 3: Proportion of patients with moderate–high unmet needs by cancer type.
Discussion
This study describes, for the first time, the unmet supportive care needs of Indigenous Australians diagnosed with cancer across multiple jurisdictions using a culturally specific and validated tool (SCNAT-IP). The present study findings suggest that many Indigenous Australians diagnosed with cancer have unmet needs that have not previously been identified or addressed by cancer services.
This study found that the physical and psychological domains contained the most commonly reported needs consistent with previous research with non-Indigenous Australians 23-25. This probably reflects the life-changing nature of a cancer diagnosis for all patients. For Indigenous Australians with a cancer diagnosis this is likely to be exacerbated by their social and economic circumstances. Physical and psychological needs among the patients in the current study were related to managing the impact of a cancer diagnosis on their daily life (work around the home), stress about prognosis and mortality (worry about the cancer spreading or getting worse) and anxiety. Patients most commonly required assistance with their physical pain.
The practical/cultural domain also ranked highly in terms of unmet needs, and these needs must be considered in providing optimal cancer care to Indigenous patients. In the practical/cultural needs domain, the most frequently reported unmet need item was ‘money worries’. This result is consistent with the findings in the authors’ previous study of unmet support needs among Indigenous adults conducted in Queensland 20. It is also consistent with other Australian studies where the financial burden was found to be an important issue for cancer patients while travelling to receive treatment, or for other care expenses13,26. Cost is a barrier to accessing healthcare services for both Indigenous and non-Indigenous Australians27-29. In 2016–17, 8% of people aged 15 years and over delayed access to health care due to concerns about the associated costs 30. Other practical and cultural unmet needs reported by participants of the present study were ‘Having an Indigenous person to talk to and support you, someone who understands your culture’ and ‘Finding a place to stop or stay while receiving treatment’.
Interestingly, in the communication/information domain, a high proportion of participants (>76%) indicated not having any unmet needs. This is a positive finding, particularly given the reported communication/information challenges cancer service providers identified when communicating with Indigenous patients11,31. However, the discrepancy could also arise because the needs assessment is capturing people’s desired or perceived needs for additional information, and these depend upon a broader level of understanding of possibilities within the health system 32,33. As such, efforts to improve the utility and cultural appropriateness of cancer and health promotion information are still needed34,35. Participants in this study had access to Indigenous staff (liaison officer and/or social workers) and were commonly escorted (approximately 88%) to the hospital by a family member or friend. This support may have assisted with information provision and effective patient–clinician communication.
It was also positive that 90% of participants reported that they had no unmet need related to language interpretation, despite 43% of participants speaking a language other than English as their main language at home. It may also reflect the fact that most of the participants who speak a language other than English as their main language at home were from Northern Territory and interpreters are available and accessible for the study interview at the Northern Territory study site.
Implications for practice, policy and research
The reported variation in unmet needs across some jurisdictions highlighted the need for locally tailored cancer services, programs and policies. Practical and logistical barriers (eg travel and treatment expenses or finding appropriate accommodation) to attend hospital or other cancer-related appointments can reduce the likelihood of patients to undergo and complete their cancer treatment. In Australia, optimal cancer care pathways recommend assessing supportive care needs at every step of a patient’s pathway. Recommendations and initiatives to improve the identification and monitoring of unmet needs for Indigenous cancer patients include routine screening using culturally appropriate tools20, facilitating access to cancer care for rural and remote communities through tele-oncology models36 or providing informative discharge summaries for continuity of care at community level37. More recently, an optimal care pathway for Aboriginal and Torres Strait Islander people with cancer38 has been developed to assist health professionals to provide optimal patient-centred care, including assessing and addressing their supportive care needs38. While qualitative explorations into patient experiences and perceived barriers and enablers to optimal cancer care are essential, needs assessment tools that can systematically and reliably quantify patient needs are also critical. When implemented into routine care, such tools are a reliable and quick method to identify high-need patients who may require complex care. This can enable timely referrals to appropriate services and in turn result in improved outcomes for people diagnosed with cancer20. A needs assessment tool also allows for the measurement of unmet supportive care needs over time to assist evaluation of changes in policy, practices or services. This study provides a baseline measure of the extent of unmet supportive care needs among Indigenous Australians with cancer and, by providing a means by which to prioritise these needs, may inform the development of targeted approaches to improve cancer care and outcomes for Indigenous Australians.
Strengths and limitations
This multicentre study used a validated and culturally relevant assessment tool to identify patients’ needs and quantify the extent to which they remain unresolved. The interviews were conducted by trained staff members who were routinely in contact with patients and were able to establish a rapport with patients. Face-to-face interviews were employed as the authors have previously found this approach helps increase recruitment and completion rates, although it could also influence participants to respond more favourably to ‘please’ the interviewer. Participants were encouraged to answer truthfully by assurances that their responses would not affect their treatment or care, their anonymity would be protected, and only aggregated study findings would be shared beyond the research team.
The generalisability of these findings may be limited given the small sample size, and patients were recruited via a number of strategies and mostly from regional cancer services. Previous reports found that geographical isolation was associated with increased prevalence of unmet supportive care needs19. In Western Australia, recruitment was conducted via referral programs specifically for cancer patients with high needs. It is unclear if the needs of these patients reflect the needs of Indigenous cancer patients in Western Australia more broadly. It is possible that this recruitment strategy amplified the proportion of patients with moderate to high unmet needs; however, as the Western Australian patients constituted only 10% of study participants, the bias is likely to be modest. In Western Australia, cancer type and diagnosis date were extracted from referral letters or self-reported. This may mean that some patients were closer or further away from diagnosis than what has been reported; however, it is not possible to quantify this. In a previous Queensland study the authors found that cancer type was reported with reasonable consistency to medical charts39. Due to lack of statistical power, the authors could not explore further jurisdictional differences or undertake detailed examination of unmet needs by cancer type. Assessment of a more homogeneous sample of patients (ie same cancer type, stage of disease) would be difficult to achieve but could provide a deeper understanding of disease-specific unmet needs. Despite these limitations, the study highlights the variation of unmet needs across jurisdictions and provides evidence of common domains of unmet needs.
Conclusion
The findings of this study provide a snapshot of the unmet needs of Indigenous cancer patients in four jurisdictions in Australia. Most Indigenous Australians with cancer have at least one unresolved supportive care need. While there was variation in items that were most commonly reported as unmet, these items were primarily related to physical/psychological and practical/cultural concerns. The implementation of culturally appropriate needs assessments into routine care can help to ensure patients are receiving optimal cancer care and are being referred to appropriate services. The findings from this exploratory study may also indicate that some of the areas of unmet need are quite challenging for health practitioners to deal with themselves. There is a need for change at a health system level where access to social welfare and cultural support have links with community-based health services. Information on unmet needs may be used to map out priority areas for intervention, resource allocation and service redesign.
Acknowledgements
This study was funded by the NHMRC-funded Centre of Research Excellence DISCOVER-TT (#1041111), and the Cancer Council NSW STREP Ca-CIndA (SRP 13-01, with supplementary funding from Cancer Council WA). AD is supported by a Menzies Early Career Accelerator Fellowship. GG is supported by a NHMRC Early Career Fellowship (#1105399). PCV was supported by the Australian National Health and Medical Research Council (Career Development Fellowship #1083090). The views expressed in this publication are those of the authors and do not necessarily reflect the views of the funders.

