Introduction
The application of technology in medical practice has expanded exponentially over the past 20 years. Digital devices are increasingly being used in medicine, from prevention to palliative care, through diagnosis and treatment, and they can often readily be adapted to the specific requirements of different cultures, regions and countries1.
Telemedicine is a branch of health care that provides long-distance clinical services for a number of different medical specialties. One of the most important subspecialties of telemedicine is the digital diagnoses of skin disease. This approach is being widely used as a cost-effective alternative to conventional dermatological screening of patients living in more remote regions. The medical impact of teledermatology is now being felt in improvements in patient care, clinical research and in better physician education2,3. Moreover, the use of teledermatology in remote areas has minimized the shortage of resources and is widely accepted by patients, and by the professionals who use it, including dermatologists, primary care physicians and nurses4.
Improvements in digital communication are happening constantly, with the incorporation of refinements of imaging and analytical software that can be rapidly incorporated into medical care worldwide5. With the continual evolution of digital and smartphone technology for screening skin lesions, strong evidence is emerging that a diagnosis by telemedicine is comparable to that made using standard medical services in relation to both the effectiveness and patient outcomes1. Summarizing, digital technologies should be reliable, safe, and cost-effective for providing a high diagnostic accuracy for analyzing suspicious skin lesions5.
In recent years advanced telecommunication platforms with high resolution images have been enhancing the delivery of dermatologic care6. This new era of teledermatology requires both high diagnostic accuracy and reproducibility for two distinct purposes: first, the findings are used to treat patients with limited alternatives for medical assistance and, second, it is important to have reliable findings that will be incorporated into clinical research for improving medical procedures.
The aim of this study was to determine whether the diagnosis of suspected skin cancer lesions performed using digital photography with a conventional smartphone application (app) that has been designed exclusively for this purpose was accurate and reliable in comparison to the findings of the face-to-face consultations.
Methods
This was a prospective study drawn from a population of 49 individuals monitored by routine skin cancer screening in the Cancer Prevention Department at Barretos Cancer Hospital during 2016. All patients were evaluated by a dermatologist who took a biopsy or excised the lesion and provided a differential diagnosis with an evaluation of the likelihood of the lesion being benign or suggestive of malignancy.
Prior to performing the surgical procedure, each lesion was photographed with a smartphone, using an installed app developed exclusively for teledermatology (Telederma; https://teledermato.inovaeinstein.com.br). The Telederma app allows the registration of patients’ personal data, clinical history and characterization of the morphological features of each lesion. All clinical information was entered into fields provided by the app and two images of each lesion were photographed from at least two angles. These data were then stored for further analyses using a secure web-based companion program that was developed together with the Telederma mobile app. This program provides access for all patient data together with each image of photographed lesions (Figs 1–3).
A second physician, a dermatologist specializing in skin cancer, assessed all the clinical information and respective images and provided an independent diagnostic opinion of all lesions examined in the study. Menus in the app allow the physician to report on probable diagnosis (eg lesion likely benign or malignant) and also select opinions related to the quality of the images of each lesion (high, intermediate or poor quality). Dichotomic diagnostic scoring of benign versus malignant lesions was included in the app’s pull-down menus since the application was primarily developed for an oncological hospital. However, other menu options could be selected for reporting if required. For example, the option ‘bad quality photo’ could be selected in instances when the lesion image could not be resolved, making it impossible to provide a diagnostic hypothesis.
After independent evaluation by two physicians, one in a conventional face-to-face examination and the other using teledermatology images, the results were compared by statistical analysis. SPSS Statistics v19.0 for Windows (IBM Corporation; http://www.spss.com) was used. A p-value of less than 0.05 was used as a cutoff for statistical significance. The accuracy, sensitivity, specificity, together with positive and negative predictive values between the two examiners in comparison to the histopathological findings of all biopsies as the diagnostic gold standard, were calculated. The agreement between the physicians was obtained through the Kappa concordance index. In this comparison, the images considered to be of ‘poor quality’ were excluded from the analysis.
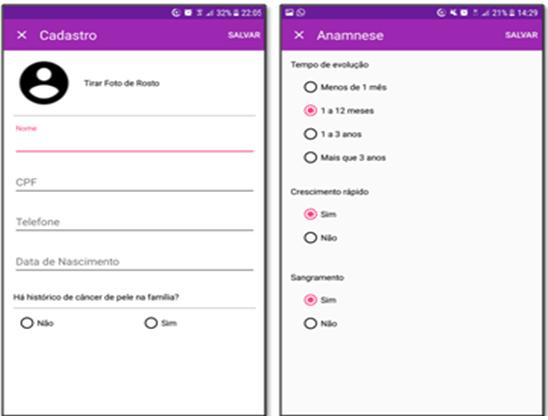 Figure 1: Display of personal data and clinical history pages of the smartphone app used in this study.
Figure 1: Display of personal data and clinical history pages of the smartphone app used in this study.
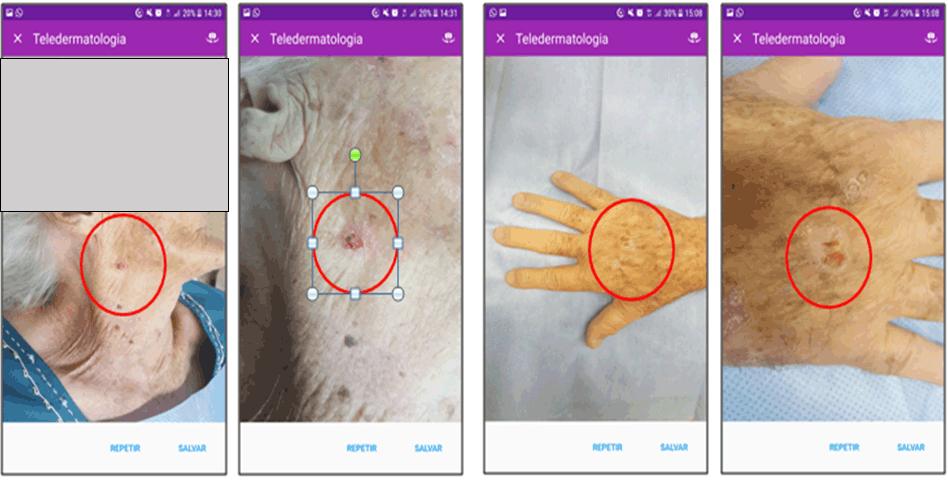 Figure 2: Squamous cell carcinoma (face and hand) – short- and long-distance photography – rendered on study smartphone app.
Figure 2: Squamous cell carcinoma (face and hand) – short- and long-distance photography – rendered on study smartphone app.
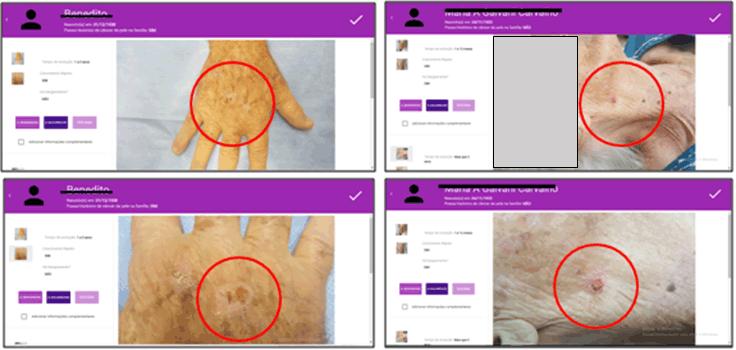 Figure 3: Website display of squamous cell carcinoma from Figure 1.
Figure 3: Website display of squamous cell carcinoma from Figure 1.
Ethics approval
This investigation was approved by the ethics committee of the Barretos Cancer Hospital, in Barretos, Brazil (N:1151857). The participation in this study was voluntary, anonymous and confidential. All data were handled only by the investigators.
Results
From 49 patients, 10 were excluded from the analyses because two cases showed bad quality images and eight patients did not attend the medical appointment. The youngest patient was aged 39 years and the oldest patient was aged 91 years (average of 68 years).
The lesions were mostly found on the face (69%), followed by upper limbs (15%), scalp (8%), trunk (6%) and lower limbs (2%).
The histopathological findings of the biopsies showed that 71% of lesions were malignant, with 32% being squamous cell carcinoma (SCC) and 68% being classified as basal cell carcinoma (BCC), and 29% were considered benign (Table 1).
The accuracy, sensitivity, specificity, positive and negative predictive values of the two skin specialists with the histopathologic examination of biopsies as the gold standard for diagnosis are described in Table 2.
The inter-observer kappa value between face-to-face examination and histopathological examination was 0.549, and between teledermatology and pathology was 0.556. The inter-observer kappa value between face-to-face examination and teledermatology showed excellent agreement at 0.958.
Table 1: Case distribution of patients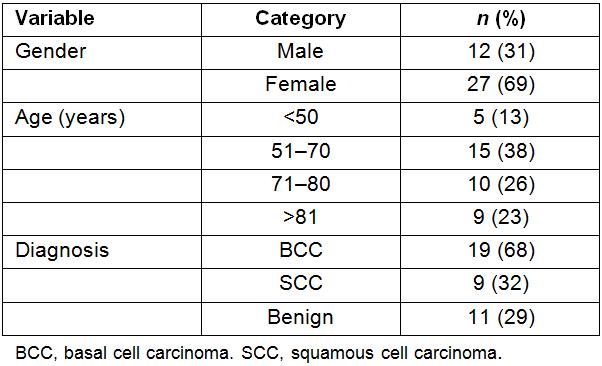
Table 2: Comparative performance of face-to-examination and teledermatology with histopathological diagnoses as the gold standard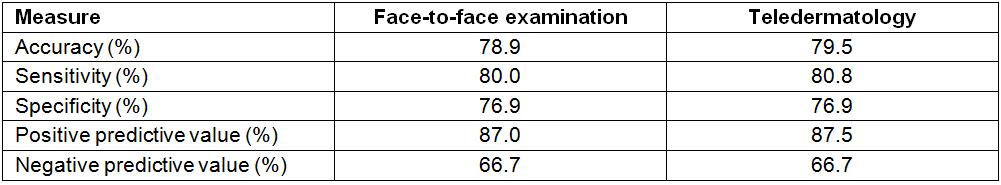
Discussion
The preliminary results herein reported are very encouraging and suggest a potential usefulness of the smartphone with the Telederma app. Despite the limitation of the small sample size available, the percentage of poor resolution images was very small and can be partially attributed to lack of experience using the smartphone for capturing high resolution images. As teledermatology becomes standard practice for rural communities the authors believe that this minor limitation will be rapidly overcome. Another strength of this study was the similarity of diagnoses between the two independent skin specialists in comparison to histopathologic examination, showing that teledermatology has a great potential to be included as part of the routine of medical management of skin lesions in remote areas without experienced dermatologists.
The WHO defines telemedicine as the delivery of healthcare services, where distance is a critical factor, by all healthcare professionals using information and communication technologies for the exchange of valid information for diagnosis, treatment and prevention of disease and injuries, research and evaluation, and for the continuing education of healthcare providers, all in the interests of advancing the health of individuals and their communities6,7. Teledermatology has been shown to be one of the most effective forms of telemedicine in several studies, including this present analysis, with an equivalence in the accuracy of the diagnosis in comparison to the traditional medical consultation system. Moreover, this type of long-distance management of skin lesions is accepted favorably by the patients4.
Access to specialized medical services in remote areas and even in larger centers can be a recurring problem in many parts of the world. Teledermatology can help to overcome the distance between the patient and the specialist8, thereby reducing the time for the diagnosis and surgical treatment in comparison to the traditional care system for patients living in remote regions9-11. For example, in Brazil, the fifth largest country in the world, with a public health system (called SUS) that is responsible for more than 100 million people, the number of doctors per capita is similar to that of developed countries, with an average of 2.1 physicians per 000 inhabitants. However, unfortunately there is a disproportionate concentration of physicians in metropolitan areas, leaving remote areas, such as the Amazon region, having only one medical doctor for every 10 000 inhabitants12. Moreover, according to the Brazilian Society of Dermatology, only 3% of dermatologists working in Brazil are active in the north region13.
Although skin cancer has a relatively low mortality rate, there are expected to be 1547 deaths due to melanoma and 1769 due to non-melanomas in Brazil in 2018, and a higher overall incidence of both skin cancers, with 175 000 non-melanoma and 6000 melanoma cases projected14. Because these tumors mainly affect regions of the body that are highly exposed to the sun, such as the face and neck, the preferred treatment, which is surgical resection of these lesions, can result in physical and/or psychological sequelae in patients15. Thus, if cases of skin cancer can be recognized and referred more rapidly to the clinic there is an increased chance of minimizing surgical procedures. In this scenario, teledermatology is emerging as an efficient and reproducible tool to aid in the early diagnosis of malignant skin lesions16,17.
Other countries have also found teledermatology to be a very effective strategy in more rural areas. A study carried out in rural areas of Colombia showed that this approach was particularly helpful in forested regions, where dermatology specialists are not presently available18. In Egypt, teledermatology was assessed and found to be highly reliable, emphasizing a better use of this tool, especially in distant regions, where there is a lack of a proper dermatological service(19}. In Cardiff, UK, it has been observed that teledermatology can play a role in bridging the gap between community-based primary care, and hospital-based secondary care. The results from the first 4 years of their study suggest that teledermatology was effective at improving both patient care and operational costs19.
The application presented in this study was designed to function as a telemedicine platform that can store both clinical and sociodemographic data and also capture and store images of all suspicious lesions for later dermatologic evaluation. Despite the limitation of the small sample size, the results of this pilot study demonstrate the broad utility of this application for screening in remote regions of Brazil, with results similar to those found in the literature based on populations from other countries17,20.
The interobserver kappa value between face-to-face findings and teledermatology was 0.958, which is excellent. However, the kappa values of face-to-face examination and teledermatology versus the histopathological results were 0.549 and 0.556 respectively, showing only moderate agreement. This is most probably due to the low number of participants, which is a limitation of the study as discussed previously. The sensitivity and specificity found for both face-to-face examination and teledermatology were over 75%, including the overall accuracy, which demonstrates the effectiveness and reproducibility of the application developed to aid the diagnosis of skin cancer. However, the lower negative predictive values for both approaches (66.7%) underscore the need for confirmatory histopathologic analyses of all suspicious lesions.
Another important discussion point concerning the application of teledermatology is the consideration of which health professional is best able to carry out this approach. Most projects involving teledermatology have ensured there was the prior training of the health professional, including nurses and general practitioners21,22. These studies have shown that empowering nurses to undertake teledermatological work, such as data collection and photographing lesions, allows the physician in the clinic to concentrate on acute care, prescribing, follow-up and medical procedures23-25.
The smartphone application developed to aid the diagnosis of skin cancer showed great potential and reliability, and can be used as another ancillary tool for the early diagnosis of skin cancer.
Acknowledgements
We sincerely thank the Amigos da Oncologia e Hematologia Einstein (AMIGOH) for website and application development and support.