Introduction
Access to medical services is inadequate or non-existent for many rural communities across the world. A key strategy to overcome rural medical workforce shortages has been the introduction of rural community placements for undergraduate medical students. This is based on evidence that students who have a positive rural training experience are more likely to choose a rural career1. An Australian Government program introduced in 2002 supports medical schools to provide extended rural placements of at least 1 year for at least 25% of medical students2. With this support, Monash University, through its School of Rural Health, established a range of short and longer-term options for medical students to train in rural areas across north-western and south-eastern Victoria during years 2 to 5 of the medical course. One option included a specific longitudinal integrated clerkship (LIC) in the East Gippsland Rural Clinical School, in south-eastern Victoria3.
The East Gippsland rural longitudinal integrated curriculum (EG-LIC) started in 2004 and was based on the successful parallel rural community curriculum model developed by Flinders University in South Australia4,5 The EG-LIC, which is specifically rurally focused, is part of the international Consortium of Longitudinal Integrated Clerkships, an academic collaborative that fosters the development, delivery and evaluation of integrated clerkship models within undergraduate medical education6. The East Gippsland program is classified as a comprehensive LIC because the year 4 medical course (MBBS) disciplines are delivered in an integrated way, giving rise to year-long continuous professional learning relationships between students, clinicians and the community7,8.
Program design
Students self-nominate for training in the EG-LIC at the end of year 3 of the medical degree at Monash University (which enrols both direct and graduate entry medical students). Students (domestic or international) apply through a placement preference system in which they specify rural and additionally specify the EG-LIC amongst up to 10 rural location preferences.
The LIC students are based in general practice/primary care practices for all of year 4, their penultimate year of the course, in rural towns of <15 000 population. Three to four days per week are spent in their supervising practice and rotating through local hospital specialty placements (psychiatry, women’s health and paediatrics), with one or two days per week involved in peer learning tutorials. The students attend these tutorials in subregional cohorts of up to 10 students learning together throughout the year. Clinical activity in the practice involves parallel consulting with their supervising rural general practitioner9.
The EG-LIC is based in a geographically dispersed region of south-eastern Australia, including small rural towns, small hospitals and services delivered predominantly by rural generalist doctors. It differs from other regional discipline-specific and short-term placements in several ways: immersion in a small community for the entire academic year; integration of curriculum; working together as a functional peer-learning cohort throughout the year; continuity of clinical supervision; continuity of experience in primary and acute healthcare settings within small rural towns; the opportunity to follow patients through the health system, and to develop strong professional relationships with experienced rural generalist physicians. The EG-LIC program involves longer continuous duration of immersion in the same rural general practice than other non-LIC rural general practice training options at Monash University (which provides a maximum of 6 months in rural general practice, which may be either continuous or intermittent).
LICs have been one of the important transformations in medical education across the world7. Based on principles of continuity, they provide opportunities for students to follow patients through several episodes of care over time (eg a pregnant woman is supported throughout her antenatal and intrapartum care) and to enjoy supervision over time by a consistent cohort of supervisors8.
What is known about longitudinal integrated clerkships?
Previous research has mainly focused on describing and validating LICs as a viable form of medical education that increases professional identity, contextualises learning to the health profile of the geographic setting and provides a sense of connection to place10-12. Research also reveals that LICs in small rural communities can sometimes be challenging experiences for students, as they can require learners to balance many synergistic learning relationships in an environment of relative geographic isolation11. Nevertheless, a recent narrative literature review identified that students who undertake LICs develop stronger higher-order clinical and cognitive skills and better patient-centred communication compared to students undertaking traditional hospital-based rotations13.
Apart from the potential difference they make educationally, there is limited evidence about the rural workforce outcomes from LIC programs. One Australian study suggested longitudinal rural clerkships of 1 year’s duration resulted in rurally based graduates choosing more geographically remote work locations than those trained in metropolitan areas14. However, the nature of the clinical learning integration was not described and the study did not adjust for all key confounders to isolate program effects. Several other longer duration rural LICs show positive results on rural workforce outcomes but these studies from Canada and Australia did not have same-school metropolitan-trained control groups, were small-scale or did not account for key confounders15,16.
Furthermore, evidence isolating the effects of a LIC program from the other known factors influencing rural workforce development (such as rural return of service policies and the student’s rural background) is weak2,17. Redressing this gap requires research designs with suitable sample sizes, control groups and analyses that adjust for key potential confounders. This is possible with Monash University’s medical program as it has a large cohort size, graduate tracking has occurred over a long period, data have been collected on major key confounders, and there is a wholly metropolitan-trained cohort of students who constitute a suitable control group.
Recent evidence from Monash shows that rural workforce outcomes can vary based on the setting and duration of immersion (longer periods of immersion in both regional hospitals and rural general practice increase likelihood of rural practice). However, the specific effect of participating in the purposefully structured year-long EG-LIC remains to be determined.
With this background in mind, this study aimed to compare the work location outcomes (regional or more rural) of medical students who completed 1 year of the rural EG-LIC in general practice in year 4 with, first, students having other rural training in year 4 and, second, students having no rural training.
Methods
Study sample
This longitudinal study was based within Monash University medical school, in Victoria, Australia. Monash University graduates over 300 medical students annually through either direct (5 year) or graduate entry (4 year) programs, which converge with the final 3 years of clinical training (termed years 3–5 in this article) common to students from both entry pathways. Eligible participants commenced their medical degree after 2004, had graduated between 2008 and 2016 and were working as doctors in postgraduate years (PGY) 1–9 at the time that work location was observed in 2017.
Rural training and the LIC
Information about the student training location(s), and duration, type and timing of training, was prospectively collected from university administrative systems and verified by regional training coordinators for each student in years 3–5.
Locations were defined using the Australian-standard Modified Monash Model (MMM) rurality scale where ‘rural’ is defined as MMM 2–718.
Duration of rural training was calculated by aggregating all periods of rural training (in weeks) occurring in years 3–5. This consisted of 6- or 12-month periods in years 3 and 4, and was only counted as rural training in year 5 if it comprised more than one rural rotation (longer than 6 weeks), which was considered the minimum period expected to have an influence at that stage of medical training.
Table 1 describes the defined groups applied to the evaluation. In the first instance, univariate analysis compared three groups consisting of those who undertook the year 4 LIC, those who did not participate in the LIC in year 4 but had other rural training elsewhere in year 4 and those who were metropolitan-based only in year 4 (groups 1–3). In additional analyses, each of these groups was subdivided according to whether there was any other rural training in years 3 and/or 5 of the course since duration of rural training is a potential confounder of the effect of the LIC19. Also, the subgroup that had had done rural training in years 3 and/or 5 (but not in year 4) was delineated to account for the potential effects of the timing of rural exposure within the medical degree. These six subgroups (A–F) are outlined in Table 1.
Student characteristics
Rural background was defined as having resided for at least 5 years since commencing primary school in an area classified as rural according to the MMM 2–7. Students self-identifying as having a rural background submit a statutory declaration upon enrolment into medical school.
Other relevant covariates included sex, direct from school or graduate entry (completed another degree prior to entering medicine). All of international student status (domestic or international) and having either a bonded medical place (BMP) or medical rural bonded scholarship (MRBS) were identified as these all have a rural return of service requirement of graduates.
Self-reported interest in working after graduation in a rural area (outside of a capital city or major urban centre); and an interest in becoming a general practitioner (within the top three of 18 specialty preferences) at course commencement were obtained from the Medical Student Outcomes Database20. These data were only available for the 2006–2014 commencing cohorts. To avoid dropping unmatched students from multiple regression analysis, which used listwise deletion, the two ‘interest’ variables were categorised ‘yes’, ‘no’ or ‘unknown’.
Outcome measure
The outcome of interest was the graduate’s main work location, obtained from the Australian Health Practitioner Regulation Agency’s public website annually for 2017 and linked by student first and last name to their characteristics and training information. Approximately 12% of the study cohort who had graduated (2008–2016) were not matched to agency data in 2017. However, 90% of those unmatched were international students (who are highly likely not to be in Australia any more). Thus, the matching rate for domestic students was extremely high, at approximately 98.5%.
Work location was geocoded (by town name and postcode) and categorised using the MMM rurality scale as ‘metropolitan’ (MMM 1) and ‘rural’ (MMM 2–7). Work location was additionally categorised as ‘metropolitan’ (MMM 1), ‘large regional’ (MMM 2, ≥50 000 population) or ‘smaller regional and rural towns’ (MMM 3–7, <50 000 population).
Analyses
Chi-squared tests compared univariate associations between the three groups (defined as per Table 1): the participants of LIC, those with other rural training and those with no rural training. Chi-squared tests were also used to test associations between participant characteristics and ‘working rurally’ within each of these groups. A multiple logistic regression model tested associations between rural work location in 2017 and the six groups of interest (A–E compared to group F in Table 1), adjusting for key student characteristics (calculated as odds ratios (ORs)). A multinomial logistic regression model explored associations between doctors working in metropolitan, large regional (≥50 000 population) or smaller regional/rural (<50 000 population) towns and the six groups of interest (A–E compared to group F in Table 1), adjusting for key student characteristics that may potentially confound associations (calculated as relative risk ratios because the outcome has three levels). Sensitivity analyses using 2016 work location outcomes were also undertaken. StataSE v14.0 (StataCorp; https://www.stata.com) was used for all statistical analyses and p<0.05 was considered statistically significant.
Table 1: Groups applied to univariate and multivariate analysis†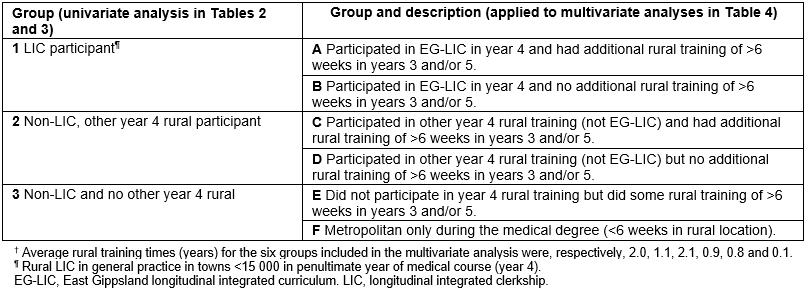
Ethics approval
Ethics approval was obtained by Monash University’s human research ethics committee (CF14/3302 – 201400174).
Results
There were 130 LIC participants with observed (postgraduate) work locations in 2017. In comparison there were 519 graduates who had had a non-LIC rural training in year 4 and 1763 with neither LIC nor year 4 rural training, with observed 2017 work locations.
Compared with students with non-LIC year 4 rural training, LIC participants were more likely to be graduate-entry or international students and less likely to have an interest in working in a rural area at entry to medical school and a rural background (Table 2). Compared with students with neither LIC nor year 4 rural training, LIC participants were more likely to be older, have a rural background, graduate entry enrolment, be rurally bonded, have an interest in working in a rural area or in being a general practitioner at entry to medical school and be less likely to be international students.
The overall rates of working rurally in 2017 were 26.9%, 27.4% and 9.1% respectively for the LIC, non-LIC for other year 4, and non-LIC and non-year 4 rural training groups (Table 3). Between each of these three groups rural background, initial rural interest and age at entry were significantly different (p<0.05).
In Table 4, after accounting for key covariates, LIC participants who had additional rural training of >6 weeks in years 3 and/or 5 of the course (group A) had the strongest odds of working in rural areas (OR 5.04, 95%CI 2.80–9.09). In contrast, LIC participants for whom LIC was their only rural training (group B) were no more likely to take up rural practice than the metropolitan-only group (OR 1.66, 95%CI 0.75–3.68). Among the non-LIC participants with year 4 rural training, students with longer rural exposure (>1 year in years 3 and/or 5 of the course, group C) also had higher odds of working in rural locations than students with shorter rural training (≤1 year, group D) (OR 3.68, 95%CI 2.58–5.23 and OR 2.39, 95%CI 1.48–3.87, respectively).
Students who had participated in the LIC group with additional rural training in years 3 and/or 5 of the course (group A) had the strongest odds of working in smaller regional or rural towns (population size<50 000) (OR 5.62, 95%CI 2.81–11.20). Students in this group (group A) also had strong odds of working in large regional centres (≥50 000 population) as did the non-LIC year 4 rural group (group C) (OR 4.11, 95%CI 1.32–4.95 and OR 4.49, 95%CI 2.81–7.19, respectively).
Overall, rural work was consistently positively associated with rural background, being an international student and having a BMP or MRBS return of service obligation, but negatively associated with being in a later career stage (≥PGY 7) (Table 4). Working in a smaller rural town was positively associated with being a graduate-entry student or having an interest in rural practice when commencing medical school.
When sensitivity analyses were conducted based on the 2016 work location outcomes, very similar associations were found.
Table 2: Characteristics of longitudinal integrated clerkship participants working in 2017, compared with non-participants with or without year 4 rural exposure† 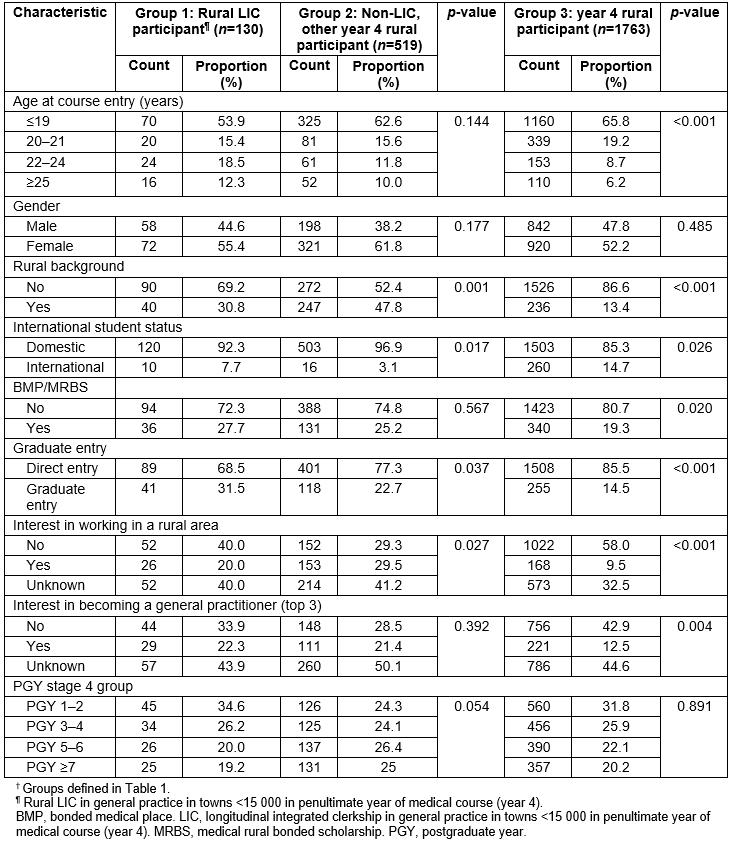
Table 3: Unadjusted (crude) proportions in each group† working rurally in 2017 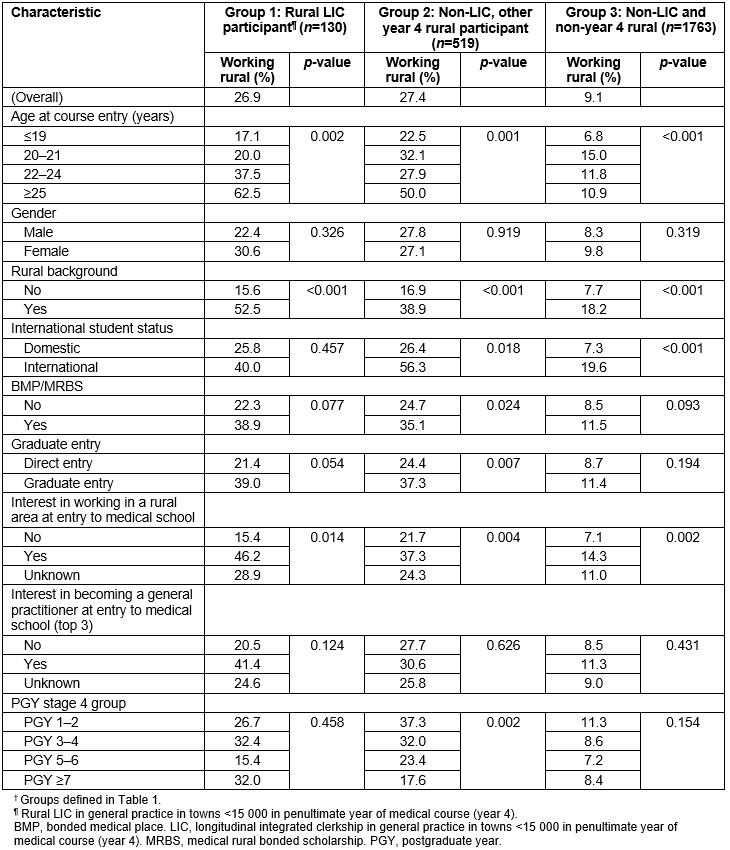
Table 4: Logistic regression models of associations between rural longitudinal integrated clerkship participation† compared with other rural exposure and working rurally (large and smaller rural locations) in 2017 (n=2412) 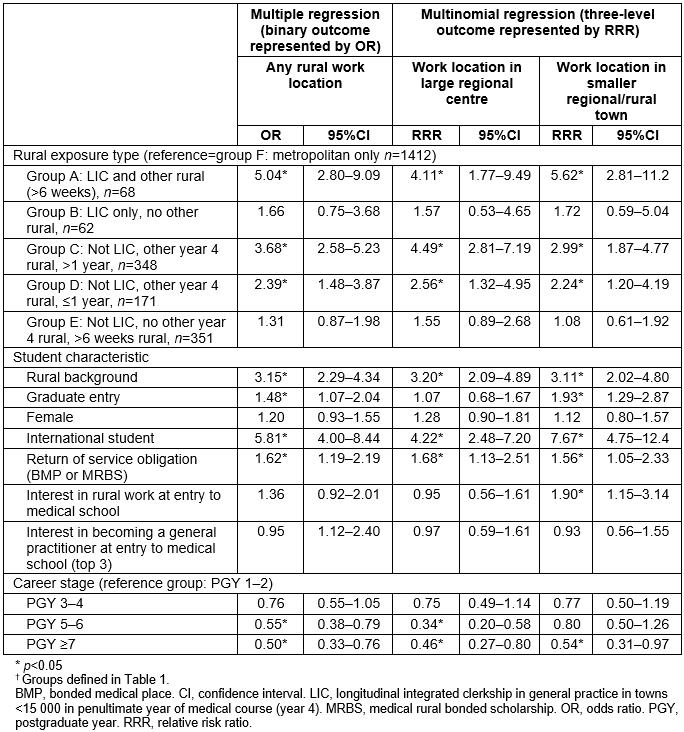
Discussion
The present study shows that students who undertake the EG-LIC and additionally participate in rural training in other years (average rural training duration 2.0 years) are the most likely group to subsequently work in smaller regional or rural towns. This is an important finding because smaller regional and rural (and remote) towns have historically faced the greatest difficulties in recruiting and retaining Australian-trained doctors and still rely heavily on internationally trained medical graduates. This new evidence can help inform the redesign of medical education programs so that they are better geared towards producing graduates who are more prepared to work in smaller regional or rural towns. The present study’s findings are consistent with other recently emerging evidence suggesting that combining medical student training in general practice settings with regional hospital training exposures is associated with greater odds of rural practice. The evidence suggests that the characteristics of medical programs that are associated with optimal rural workforce distribution outcomes include year-long LIC training in general practice in smaller rural towns, together with additional rural training (averaging an extra 1 year’s duration in this study in either year 3 and/or 5 of the course) in regional hospitals and other community settings.
Students whose only rural training was the LIC were no more likely to be in rural practice than those who only trained in metropolitan areas. One explanation for this is that students with limited interest in rural practice may be choosing the intense LIC training because of perceptions about its quality: it has been shown that improved academic outcomes are achieved by students undertaking LICs12,13. Additionally, most (89%) of the students whose only rural training was the LIC were of metropolitan background. To effect a rural work outcome amongst this group may take longer than 1 year, as suggested in other evidence19. Within the program delivered by Monash University, EG-LIC provides opportunities for diversified community-based clinical learning and broad skills acquisition. The EG-LIC differs from other rural immersion opportunities available at Monash University by its integrated curriculum delivery, length of continuity of general practitioner supervision and length of rural immersion in smaller towns further from the capital city than most other rural training opportunities.
This study also reveals that medical students who undertake rural training for more than a year (non-LIC) are more likely to work rurally than students wholly training in metropolitan areas, although the overall odds of rural work aren’t as high as for students who have similar rural training duration but participate in both LIC and additional training in other rural settings. The non-LIC rural training students are also more likely than the EG-LIC group to work in large regional centres, where the workforce need tends to be less acute than in smaller rural centres (although still greater than in metropolitan centres). These findings of improved workforce outcomes in regional cities that are associated with training models centred around regional hospital hubs are consistent with other findings15,16,19. Importantly, however, this study shows that even better medical workforce distribution outcomes are associated with the combination of a purposefully designed LIC rural training in smaller rural centres and additional rural training in regional hospitals and surrounds.
In addition, several salient secondary findings relevant to rural workforce policy were evident. First, the study’s analyses reaffirmed the likely effectiveness in the short term of legislation restricting access by international students to provider numbers unless they practice in districts of workforce shortage – international medical graduates from Monash University were between four and almost eight times more likely to be working in a rural area. Second, students with BMP and MRBS return-of-service obligations were consistently about 1.5 times more likely to be working in a rural area. These findings add to a previous Monash study, demonstrating for the first time in Australian rural workforce literature that these workforce policies play a role in rural workforce supply19.
A limitation of the present study was that many graduates were in pre-vocational and vocational career stages when their work location was measured in 2017. These career stages often impose restrictions on where doctors can work, depending on specialty, and the restrictions may vary by region. While the EG-LIC graduates spanned similar career stages to the rest of the graduates at the time of this study, there are limited opportunities for them to pursue postgraduate non-GP specialty training in the region where they had undertaken the LIC, which further highlights the importance of this study’s findings of improved workforce distribution by this group. Longer-term outcomes data are required to observe associations with postgraduate training and specialty choice, including uptake of rural generalist practice, by the EG-LIC cohort. Also, the association between training in the LIC program and subsequent scope of practice is of interest but was beyond the scope of this study.
A further limitation of this study was its inability to fully explore the effects of prior interest in rural practice, self-selection and student allocation. The EG-LIC is available to all students on an equal basis according to annual placement preferences submitted in year 3 of the course, and preference is given to students who have indicated a desire to spend both year 3 and year 4 in rural placements in the region. Data on the relationship between student preferences and subsequent allocation were not available for this study. The study analyses did, however, adjust for any effect related to student interest in rural practice at the beginning of medical school, thereby reducing the effect of self-selection bias as much as was possible with the available data.
Methodologically this study used a strong longitudinal design, accounting for key measurable confounders and making comparisons between multiple groups defined by differences in rural exposure types and duration. Given these strengths, the findings may be worth considering when seeking to design undergraduate medical training programs with the potential to improve geographic workforce distribution.
Rural LIC programs consistently face cost pressures as universities seek to centralise and consolidate revenue-generating activities to survive in more competitive economic times. The Rural Health Multidisciplinary Training Program (incorporating rural clinical schools) and the recently introduced regional training hubs are Australian Government-funded rural workforce programs; universities in receipt of this funding have opportunities to play an increasingly locally integrated and strong role in shaping national rural workforce development, involving themselves in regional workforce planning and leading the generation of evidence about workforce recruitment and retention, and models of education and health care that add value to rural communities15,21,22. Strong and influential locally representative leadership is a prerequisite for sustaining rural LIC programs, and this study’s data demonstrates the important role that LICs can play in achieving a more distributed rural medical workforce.
Conclusion
Rural LIC placements that immerse students in small communities where they are involved in general practice and hospital care, are strongly associated with graduates subsequently working in smaller regional and rural centres, especially when rural LIC training is combined with further rural training within the medical course. When considered in conjunction with existing knowledge about the strong academic outcomes for LIC program participants, these findings suggest that Australian medical schools – and medical schools in countries which similarly struggle to achieve a well-distributed medical workforce – should consider expanding rural LIC programs and lengthening rural placements, to meet medical workforce needs in smaller rural and remote communities, where unmet healthcare need is greatest.




