Introduction
Diabetes mellitus is one of this century’s major healthcare challenges. It is placed among the top 10 causes of death, accounting for 10.7% of the worldwide mortality for any reason between 20 and 79 years of age1.
As reported by the International Diabetes Federation, the world prevalence of diabetes in 2017 was 451 million people aged between 18 and 99 years. This prevalence is on the rise, so 693 million people aged between 18 and 99 years of age are estimated to have the disease in the year 2045 if the current tendency persists1. However, it is worrying that 50% of diabetic patients are not aware of their disease, according to some estimates, which makes it difficult to potentially prevent the complications that may arise from diabetes1.
Diabetic retinopathy (DR) is the leading cause of blindness in working-age adults in most developed countries2 and it meets the necessary requirements for a screening program, both for the characteristics of the disease and for the validity of the available diagnostic tests3. As estimated by the International Agency for the Prevention of Blindness, in 2015 there were 145 million diabetic patients with some degree of retinopathy and 45 million of them suffered from some kind of sight-threatening retinopathy4.
Only 50% of diagnosed diabetic patients have periodic ophthalmic examinations, which is particularly evident in rural areas.
The implementation of telemedicine in the field of the diagnosis of diseases is more and more widespread, which facilitates the exchange of information among professionals. Consequently, this is an advantage for those patients who live in rural and remote areas, who then do not have to travel unnecessarily5.
Objectives
The objectives of this study were to:
- determine the prevalence of DR in a sample of diabetic patients and to classify the patients with DR according to the type and severity degree of the disease
- evaluate the degree of satisfaction of the diabetic patients with respect to the DR screening through teleophthalmology
- evaluate the degree of satisfaction of the professionals who conduct the diagnostic test in the screening program.
Methods
Setting of the program
The present article evaluates the satisfaction of both patients and professionals through two respective surveys. This study comes from the implementation of a DR screening program by the Regional Health Department in Castilla y León, Spain. This Spanish central region is the third largest one in the European Union, covering an area of 94 233 km2. Its population is approximately 2.4 million6.
Our program is not just a screening program; it is also a follow-up program like one being conducted in the UK7. The workflow is as follows: the diabetic patients are given an appointment at the healthcare center. This center is located 60 km from the reference hospital where the ophthalmologists are. Upon the signature of informed consent, the patients have three-field photographs taken under pharmacological mydriasis, according to the Joslin Diabetes Center proposed protocol8. All the retinographies are sent through a teleophthalmology system to a reading center to be assessed by the ophthalmologist, who draws up a diagnostic report, indicating the appropriate attitude according to the existence or absence of retinopathy, its type and severity.
The retinographies that show signs of DR and/or other unexpected pathological findings not related to retinopathy are defined as pathological.
The following three groups are considered sight-threatened patients: those who have severe non-proliferative diabetic retinopathy (NPDR), those who have proliferative diabetic retinopathy (PDR) and those who have suspected macular oedema regardless of the type of retinopathy. These three groups of patients are referred for an in-person assessment by the ophthalmologist whereas those diabetics without retinopathy and those who have less severe degrees are followed up in the healthcare center, in a coordinated work between primary care professionals and ophthalmologists.
Study sample
The number of diabetic patients in the sample was 114 (15.2%) out of 752 diabetic patients from the rural area, who had initially taken part in the DR screening program.
To select the sample, a consecutive non-probability sampling technique was used, so the diabetic patients who underwent the screening were selected as they attended the consultations at the healthcare center between the months of February 2017 and May 2018. The surveys were provided to the patients by two healthcare nurses who had not participated in the screening program.
Concerning the sample of health professionals, 10 people were responsible for taking and sending the images of the fundus to the reading center. The sample of professionals comprised four men and six women. There were two physicians, seven nurses and one x-ray technician. In terms of their personal experience in performing retinographies, four had been involved for less than 1 year, five between 1 and 5 years and the remaining one for longer than 5 years.
Concerning the questionnaires, the patients completed them in person, whereas the professionals received them via email and completed them anonymously.
Questionnaire design
Patient satisfaction survey: The survey was made by using a series of questions validated by the Catalan Health Service to evaluate the satisfaction of the patients at the primary care consultations9. The aspects assessed, through a set of nine closed questions in Likert format, were related to the information about the program the patients received, the organization of the center, the way the test was conducted and the reception of the results. Another two questions were added to the previous ones. One of them was based on a 0 to 10 scale. The other one assessed whether the patients preferred to continue getting their check-up done at the healthcare center or going to the hospital.
The items of the questionnaire were as follows:
- Facility to make an appointment at the healthcare center to conduct the test.
- Time devoted to conduct the test.
- Explanations received before conducting the test.
- Explanations received during the test.
- Explanations received after conducting the test.
- The feeling of being in good hands during the test.
- Treatment received during the test.
- Waiting time to receive the results.
- Tolerance to pupil dilation.
- Score, on a scale from 0 to 10, for degree of general satisfaction with the activity.
- Willingness to continue having the check-up at the healthcare center.
Healthcare professional satisfaction survey: A set of 10 closed questions and Likert format was used to assess professionals. The aspects assessed were related to their training, the way the test was carried out, the support from their managers and the influence of the activity on the relationship with their patients. Another two questions were added to the previous 10 ones. One of them, to grade general satisfaction degree with the activity, was based on a 0 to 10 scale. The other item assessed whether they would like to continue performing the activity. An open question was also included to collect the improvement suggestions in the implementation of the screening program.
The items of the questionnaire were as follows:
- I am aware of the importance that the screening program has for the early diagnosis of DR and the prevention of blindness in diabetic patients.
- I consider I have received enough theoretical and practical training to perform the activity.
- I find it easy to handle the retinograph and the computing equipment that we use in this program.
- I consider that the fundus images I can get have enough quality to be evaluated at the reading center.
- I consider the patients are well informed about the program when they come to get their tests done.
- I feel confident in front of the patients when performing this activity.
- I feel I have enough support from the professionals in charge of the implementation of the screening program.
- I am afraid of the pupil dilation procedure of patients.
- The activity allows me to improve the doctor–patient relationship with the screening program users.
- I find it easy to combine this activity and my daily care-providing work.
- Score, on a scale from 0 to 10, your degree of general satisfaction with the activity.
- Would you like to keep performing this activity?
Measurements
The variables taken into account when evaluating patients were sex, age, type of diabetes, years of development of the disease, type of treatment and retinography result (NPDR, PDR, other pathologies).
The measurement scale used for the patients was ‘bad/average/good/very good’.
In the case of Healthcare professionals, the measurement scale was ‘totally disagree/disagree/neither agree nor disagree/agree/totally agree’.
Ethics approval
This research project has been evaluated and assessed by the Ethics and Medical Research Committee within the Health Area Valladolid East. The approval number is PI 18-1146.
Results
In terms of sex, 58.8% of the total sample were males and the remaining 41.2% were females. The median age was 68.69 years, with a standard deviation of 9.85. In terms of diagnosis, 98.2% were type 2 diabetics and the remaining 1.8% were type 1 diabetics. The average time of the development of the disease was 9.8 years ± 8.43 years. Regarding the treatment, 5.3% did not receive any pharmacological treatment, 76.3% were treated only with oral antidiabetics, 3.5% only with insulin, and the remaining 14.9% received combined treatment.
Pupil dilation was not rejected by any patients and the informed consent was signed by 100% of the patients.
The retinographies were reported as normal by the reading center in 75 patients (65.8%) and as pathological in 38 patients (33.3%). Only one case was considered unfit for assessment (0.9%).
Figure 1 shows that the prevalence of DR in the present sample was 15%. Of the patients with retinopathy, 88.2% had the non-proliferative type (46.7% mild degree, 40% moderate degree and 13.3% severe degree) and the remaining 11.8% had the proliferative type. Suspected diabetic macular oedema was diagnosed in five of the patients with retinopathy (29.4%).
Of the total DR patients 29.4% met the criteria for ophthalmological referral.
Other unexpected pathological findings not related to retinopathy were found in 26 patients (23% out of the cases fit for assessment). The most frequent ones were age-related macular degeneration, pathological papillary excavation, epiretinal membrane, branch retinal vein occlusion, myopic maculopathy and asteroid hyalosis/synchysis scintillans.
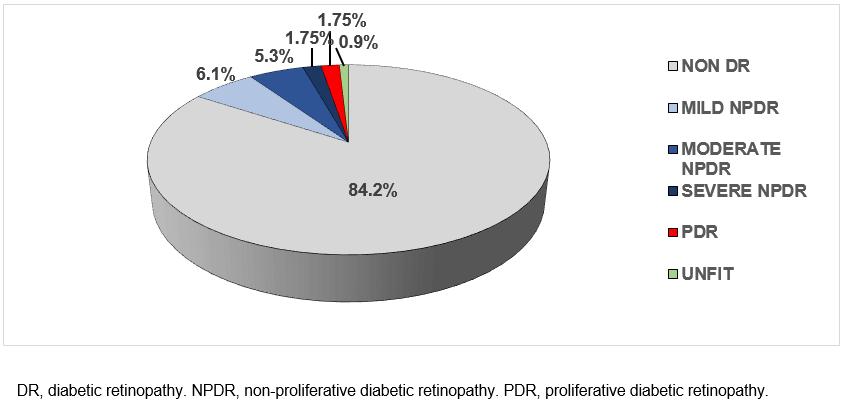 Figure 1: Retinography results for diabetic patient sample (n=114).
Figure 1: Retinography results for diabetic patient sample (n=114).
Patient satisfaction survey
In the first nine questions, a four-point scale was used: ‘bad’ (0), ‘average’ (1), ‘good’ (2) and ‘very good’ (3). Table 1 summarises the percentages of the sample answer to every question, alongside the mean and the standard deviation of the scale values. In questions 5 and 8, there were slightly fewer responses (5 and 11 cases, respectively). This was due to the fact that the respondents did not answer, so those values were considered missing. For the rest, valid N is the total number of respondents (114).
In general, it has been shown that there were hardly any negative answers from patients, except for questions 8 and 9, where some answers were ‘average’ (14.6% and 10.5%). Most answers to every question were ‘good’. The highest percentage was for question 9 (tolerance; 76.3%), which, however, shows the lowest mean (1.97) due to the fact discussed above. Next was question 8 (waiting time; 64.1%), which showed the second lowest mean (2.07) for the same reason.
Among the other seven questions, the option ‘good’ appeared, especially in question 1 (facility; 64.0%, mean: 2.36). The least common percentage is shown in question 7 (treatment received; 43.9%), were there is a high percentage of ‘very good’ answers (54.4%; mean: 2.53, the highest of all).
In question 10 the patients were asked to grade their degree of general satisfaction on 0 to 10 scale. The answers ranged from 3 to 10, the mean being 10 points, which was the most answered value too (50.9% of the 114 participants). Answers with a value of eight or higher were given by 93.9% of respondents. The mean of the general satisfaction degree was, therefore, very high: 9.23 (95% confidence interval (CI): 9.03–9.43, standard deviation: 1.07).
Question 11 (continuity) was affirmatively responded by 100% of all participants.
Table 1: Descriptive analysis: variables for questions 1 to 9 of patient satisfaction survey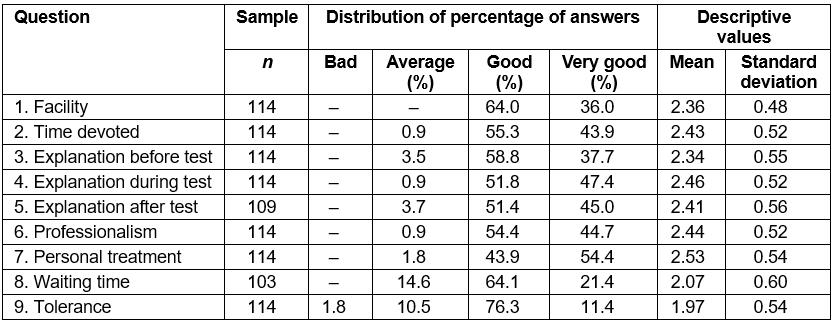
Healthcare professional satisfaction survey
In the first 10 questions for healthcare professionals, a five-point Likert scale was used, from 1 (‘totally disagree’) to 5 (‘totally agree’). Thus, number 3 was the central value representing an indifferent position.
Table 2 summarises the percentages of responses within the sample of healthcare professionals to every question, alongside the mean and the standard deviation of the scale values.
On the whole, the study results show an overall tendency towards agreement; however, the following points are noteworthy.
There were five questions (1, 2, 4, 6 and 9) in which the degree of agreement was very high – the mean values ranged between 4.9 and 4.0 – because most of or all respondents showed their agreement or total agreement.
For three questions the agreement decreased as some respondents showed some degree of doubt. For example, in both questions 3 and 7 there were 10% of indifferent respondents as well as another 10% of them who disagreed. The highest disagreement was expressed in question 10, which accounted for 40%.
Particularly high dispersion levels appeared in question 5, where all options were covered in such a way that agreement and disagreement values reached 40% each.
Interestingly, question 8 – the only question that asked about a negative emotion: fear – showed 60% of disagreement or total disagreement. This means the healthcare professionals reacted positively towards the method.
In order to evaluate general satisfaction degree, in question 11 healthcare professionals were asked to choose a value on a 0 to 10 point scale. Their answers ranged between 7 and 10, the median being 8. This is also the most repeated value (44.4% of respondents). The mean of the general satisfaction degree was high: 8.22 (95% CI: 7.48–8.97, standard deviation: 0.97).
Finally, question 11 (continuity) was affirmatively answered by all respondents, except for one.
The following suggestions were put forward by the professionals to improve the implementation of the screening program:
- Motivate healthcare professionals at the healthcare centers as well as make them fully aware of the importance of screening for DR.
- Report to primary care family physicians about the importance of obtaining informed consent from the patients.
- Assure the quality control of the technology implemented in the healthcare centers, in order to ensure it works properly.
- Ask the program managers to support the professionals who work in the program.
Table 2: Descriptive analysis: variables for questions 1 to 9 of healthcare professional satisfaction survey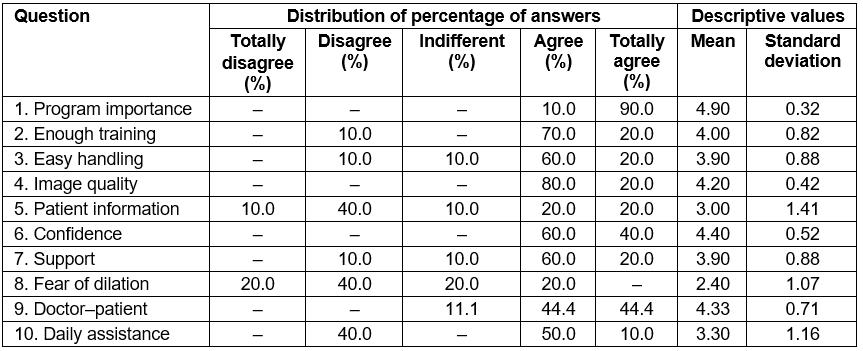
Discussion
Ungradability
These study findings show that the examination of the fundus eye under pharmacological mydriasis improves the quality of the images for their subsequent assessment. In the sample, less than 1% of the retinographies were considered ungradable. This fact contrasts with other studies where the screening was done without pupillary dilation and their percentage of ungradable retinographies was about 14%10.
Thus, the present study findings are in concordance with those of Banaee et al11, who compared the quality of the fundus photographs taken in a sample of 149 diabetic patients with dark irides before and after the instillation of one drop of tropicamide. They found a high rate of ungradable images in these patients (38.1%) and demonstrated that the instillation of only one drop of tropicamide improves the quality of fundus photographs (4.6% of ungradable images), which is not furthered by adding more drops. They claimed that this strategy can be used in teleophthalmology programs.
In addition to the low percentage of ungradable images, the good tolerance to mydriasis reported by this study’s patients is confirmed by the absence of secondary effects in the sample, which is another advantage.
Prevalence
The prevalence of DR in the sample of the diabetic patients who participated in this study (15.2%) is within the broad range of prevalence showed by different studies performed in Spain (between 5.8% and almost 30%)12.
An alarming fact is the high percentage of DR patients with a form of sight-threatening retinopathy (29.4%), which is a criterion of referral to be assessed by an ophthalmologist. It is paramount to reach the largest screening coverage because early diagnosis and early treatment for retinopathy can reduce the incidence of severe loss of vision in over 50% of cases of macular oedema and over 90% of cases of proliferative retinopathy13. In this way it is possible to come close to WHO’s objective to eliminate blindness cases due to avoidable causes by 202014.
Satisfaction
The satisfaction survey is a highly useful quantitative instrument to obtain information directly from the users of a screening program. On the whole, the items related to the organization of the center and the professionals who conducted the test were labelled by patients as good or very good. Such a high degree of satisfaction may favour the participation of future users in the program, thus increasing the impact of the program population-wise. The satisfaction survey also allows detection of the strong points and the areas for improvement of the program15.
The high degree of general satisfaction of patients with this activity is concordant with the results obtained in other studies. Boucher et al compared the satisfaction of a sample of 291 diabetic patients examined through teleophthalmology with their satisfaction after clinical examination with an ophthalmologist. Almost all of their surveyed patients (98.6%) found the telemedicine-based screening to be acceptable/very acceptable. Most of them (95%) claimed that they preferred to have their next screening examination the same way, being referred to an ophthalmologist in the event of being diagnosed with DR during the screening16.
A similar study in Kenya17 found that diabetic patients preferred a teleophthalmology approach over traditional clinical exams with an ophthalmologist for future DR screenings.
Limitations
However, those aspects related to the reception of the results should apparently be improved in our study. In a study published in 2009, Mª José García Serrano et al conducted a telephone satisfaction survey to a sample of 64 screened patients. The overall satisfaction level was 8.38 out of 10 and a statistically significant relationship was found with receiving the screening result via phone18. We decided to incorporate every diagnostic report into the respective patient's clinical history so that we could personally let the patients know about their results at the follow-up consultation.
Conclusion
In accordance with the high percentage of patients diagnosed with vision-threatening DR in this study, an early diagnosis of this complication of diabetes is strongly suggested.
In order to do so, increasing awareness and implementing training events within the healthcare professional community is paramount. Starting healthcare education campaigns aimed at patients is highly advisable too.
Teleophthalmology improves accessibility of patients and promotes screening in rural areas, far away from reference ophthalmologists, with high satisfaction of both patients and professionals, increasing the quality of health care provided to patients.
References
You might also be interested in:
2011 - Attitudes of GPs towards Older Adults Psychology Services in the Scottish Highlands
2009 - Pandemic influenza containment and the cultural and social context of Indigenous communities





