Introduction
Why are rural people in very diverse situations around the world so persistently and consistently disadvantaged in terms of access to health services, as well as health outcomes? Beyond the obvious geographical challenges of distance and topography, are there other explanations for this global phenomenon1? To answer these questions, we need to consider rural health within a broader theoretical framework. The field of rural health has to date been described predominantly by health practitioners as they grapple with the practical challenges of delivering services, separate to and in isolation from other fields of study that could broaden the discourse2,3. Without a theoretical framework, rural health research may well remain a pragmatic array of well-intentioned attempts to address the intractable issues that are faced by those living and working in rural areas. Theory enables us to understand situations, behaviors or phenomena in terms of the underlying and often invisible processes that influence them.
All thought is more or less consciously shaped by a pre-existing theoretico-ideological field … To deny the need for theoretical definition prior to any concrete research is to adopt a perspective which is narrowly empiricist and thus devoid of any scientific value. (Castells, 19764)
This article argues for critical realism as a suitable candidate theory, helpful for articulating, analysing and acting on the factors that contribute to rural health outcomes.
Rural versus urban
The concept of ‘rural’ implies its complement, ‘urban’. But this dichotomy limits a more complex understanding, and could be regarded as a diversion from understanding rural issues from an emic perspective5,6. There is no single, universally preferred definition of ‘rural’, nor is there a single rural definition that can serve all policy purposes or the particular needs of every situation in relation to its specific context7. Definitions of ‘rural’ and ‘rural health’ vary according to context and perspective, and are the outcomes of diverse needs and ways of thinking. A wide range of pragmatic definitions are used to frame epidemiological studies, differentiate interventions and allocate resources5,8,9, but these have little implication for theory beyond the immediate identified need. For example, exploring the definition of ‘remote’ in an Australian context, Wakerman reviewed geographic and practice-based definitions in published articles and websites, and found no single appropriate definition10. Although the discussion stressed that ‘social, economic and demographic changes are critical to the conceptualization of remoteness’, a working definition is offered that is only relevant to the position of medical practitioners. It is clear that while pragmatic definitions are necessary, they cannot contribute to theory in isolation, but rather that inclusive and robust theory may be more likely to produce inclusive, robust definitions.
The health of rural populations
The idea that the health of populations is determined by many factors in the social and economic environment outside of the formal healthcare system, as articulated by Virchow as long ago as 184811, came to be known as ‘social medicine’ with more recent proponents such as Allende12, McKeown13 and Farmer et al14. A starting point for broadening the definition of rural health extends the approach to health from an individual level to a population level, as articulated by Rose15. For example, despite overwhelming evidence-based ‘proof’ from randomized controlled trials that they work for individuals, heart rehabilitation programs have been spectacularly ineffective at a population level.
The approach used towards the prevention programmes in this instance reflects core positivist assumptions in its lack of focus on unobservable phenomena, its impoverished conception of the social, contextual and personal and its reliance on a narrow body of empirical evidence16.
At a population level, a complex interplay of many different factors influence health. The ‘social determinants of health’ is now a familiar phrase for broadening the notion of rural health to include its antecedents17. The word ‘social’ in the phrase ‘social determinants of health’ could imply that these determinants are simply to do with the way that human beings interact with one another, as implied in previous quotation. Alternatively, it could signal a broader set of factors that play a role in health, including historical, political, economic and environmental forces, in addition to strictly ‘social’ ones. The landmark WHO Commission on the Social Determinants of Health, which produced its seminal report in 2008, clearly states that ‘avoidable health inequalities arise because of the circumstances in which people grow, live, work, and age, and the systems put in place to deal with illness18. The conditions in which people live and die are, in turn, shaped by political, social, and economic forces.’ The WHO’s conceptual framework for the commission on the social determinants of health includes contextual issues such as governance, macroeconomic policies and social policies as structural determinants in a linear model19. Despite this, the concept of ‘social determinants’ depoliticizes and underplays the influences of the political economy of health, in terms of which inequities in health are caused and perpetuated by a global market system that favors a small elite at the expense of the vast majority of the world’s population20.
In contrast to traditional approaches to social justice21, the ‘capability approach’ of Amartya Sen is more people centred and agency oriented22,23. Following critiques from the perspective of the political economy of health24,25, the political determinants of health were eventually articulated by the Lancet Commission on Global Governance for Health in 201426. A critical response to this report suggested that the Commission did not go far enough, that it should strengthen WHO ‘as the legitimate supranational global health organization’ and ‘oppose multinational companies and other private interest groups in international health policy making by WHO’27. A follow-up commentary by Kickbusch 10 years later emphasized the need to ‘bring together a public health perspective reared on causality, evidence, determinants, and interventions with a lens that deals with the nature of power, systems, wicked problems, uncertainty, and complexity’28. Gill and Benatar, tackling global health governance and power, laid the blame with the global market that commodifies and privatizes health care, and propose greater global solidarity towards the ‘development of sustainability’ that includes addressing climate change29.
However, in rural and remote areas it is clear that geographical situation and dynamics play a major role in health behaviors, access to services as well as health outcomes. With respect to access to health services, Tudor-Hart’s ‘inverse care law’ states it clearly:
The availability of good medical care tends to vary inversely with the need for it in the population served. This inverse care law operates more completely where medical care is most exposed to market forces, and less so where such exposure is reduced. The market distribution of medical care is a primitive and historically outdated social form, and any return to it would further exaggerate the maldistribution of medical resources30.
This observation applies as much to urban–rural comparisons as to the private–public dichotomy in systems of care to which he ascribed the inequities. It is the understanding of the theoretical implication of this physical context that the present article explores. Hence the phrase ‘rural determinants of health’, which this article describes, seeks to differentiate these aspects from the more general ‘social’ perspective and understand them in more detail.
The search for appropriate theory
A distinct theoretical framework needs to guide future interventions. In a seminal article in the Australian Journal of Rural Health, Bourke et al challenged the ‘deficit’ view of rural health, emphasizing the need to move from describing the problems to solving the problems based on the assets of rural communities2. In another article, the same authors explained the need for theoretical approaches to drive research and new knowledge in rural health, and examined existing contenders including the social determinants of health, population health, evidence-based practice and community development31. They concluded that theory is needed to make implicit assumptions explicit, and to integrate ‘the social, psychological, economic and spiritual aspects that are important’, as well as understand the inter-relationships between them. This was followed by a proposed framework for analysis, developed through a series of workshops and examination of the literature, to understand rural and remote health in the Australian context using Giddens’ theory of structuration as a guide in understanding structure and agency32. The six key concepts of the framework included geographic isolation, the rural locale, health responses, broader health systems, broader social structures and power relations.
Farmer et al similarly reviewed theories from several disciplines in order to explain empirical phenomena using social and geographical theories of place33. Sociologists, anthropologists and geographers have been concerned with rural issues as social scientists, and extend a topographical understanding of spatiality to social relations and practices. Early sociological explanations for rural relationships included gemeinschaft, meaning family and community relationships, and human ecology5, before political and economic issues were acknowledged as significant. Sociologists talk of a ‘relational understanding’ of rural health that, in terms of poststructuralist theory, includes multiple forms of situated knowledge, meaning and identity34. Issues of social cohesion and community resilience feature in interdisciplinary studies of rural communities35. The complex relationship between natural and social entities has been the focus of much work in this field36, and the actor–network theory of Latour has been influential in understanding these dynamics37. From a feminist perspective, Katz uses the term ‘critical topography’ as part of ‘minor theory’ to describe the sedimentary overlaying of historical and other social and economic processes such as globalization that give rise to the characteristics of particular places38. She goes on to describe a metaphorical ‘feminist counter topography’ in which contour lines connect places by virtue of being at the same altitude, that are very different and distinct geographically and historically, in an analogous way to which certain processes such as globalization and power affect distant communities similarly.
Many classic anthropological studies examine the unique detail of social relationships while situated in a rural context and seek to generate analyses. However, no single theoretical framework predominates, as anthropology has ‘in the past decade largely renounced theory: it has been either all ‘experience-near’ ethnography or epistemological qualms’39. An anthropological lens applied to rural health practitioners contributes yet another understanding of the social aspects of rural health, with metaphors of a ‘frontier mentality’ and an ‘escape from the urban jungle’ by professionals emphasizing the urban–rural dichotomy40. Social capital, involving trust, social networks and reciprocity within communities, applies equally to rural residents as to health professionals such as nurses who are embedded in rural communities41. A fascinating perspective using psychoanalytical theory challenges urban biases on power, space and time, characterized as ‘urban narcissism’, and how they ‘may contribute to an ongoing, cumulative microtrauma for people in the rural world’42.
Rural geography also has much to contribute to discourse in rural health from the perspective of social science43,44. Geographers particularly understand the difficulties of defining what is meant by the term ‘rural’, and appreciate the economic and political forces that impact the livelihoods and lifestyles of rural citizens, as well as the changing nature of rurality in the light of climate change, food insecurity and increasing urbanization, particularly in low- and middle-income countries45. Rural development as a field of study and intervention is also concerned with health, but similarly does not subscribe to a single theoretical framework to analyse all phenomena46. Economic models rather than theory predominate in the literature, in which rural development is seen as a branch of ‘development economics’ and subject to strategies and assumptions guided by organizations such as the World Bank. Alternative theoretical frameworks for development emphasize the tenuous relationship of many rural people to land ownership, and control over the means of production47.
A number of theories of inequalities in health come closer to framing rural health more appropriately, in terms of understanding the persistent disadvantage of rural people48. Similar to health processes and outcomes, the digital divide can be regarded as a prime example of this49. But in seeking comparisons researchers often simultaneously perpetuate the urban–rural dichotomy, which may be seen as a diversion from understanding and framing rural health in its own right in relation to a wider set of parameters. Social analyses attribute health inequalities to class differentials, as originally described by Marmot50. However, as Smith and Schrecker noted, ‘the inherent contradictions within capitalism and between economic policy goals and policy commitments to reducing health inequalities’ have not been clearly debated48. Power differentials exist not only between rural and urban communities51, but also in terms of class, gender and race52 as well as the hegemony of western medicine vis-à-vis indigenous knowledge systems. To return to the original question, how do we understand and explain the persistent and intractable disadvantage of people in rural areas all around the world in terms of health access, quality, resources and outcomes?
Critical realism
In order to construct a more inclusive theoretical framework for rural health, it may be helpful to look to philosophy for guidance. Scambler and Scambler offer an introduction to critical realism as a way of not only understanding health inequalities, but of acting and intervening to reduce them53.
Roy Bhaskar, the philosopher who developed this theory, described our existence in terms of a ‘layered’ or ‘stratified’ reality, in three levels: what is empirical, what is actual and what is real54,55, as portrayed in Figure 1. Assuming that there is an objective reality external to humankind, he insists that we should not conflate this reality (ontology) with our experiences of it (epistemology), which is what he calls the ‘epistemic fallacy’. Further, critical realism distinguishes between ‘actual’ events that take place in the world, on the one hand, and both the natural mechanisms and social structures, which he describes as ‘real’ and immutable, on the other.
Far from being a philosophical indulgence in semantics, this distinction is crucial: the so-called ‘structural’ forces that influence our lives are just as real as the ‘actual’ events that they bring about, and that can be observed. Significantly, critical realists understand structures such as social class, gender and race as no less real than the laws of physics for being invisible or intangible. By asserting that these structures are unchangeable, however, Bhaskar rejected determinism and described these structures as ‘tendential’ rather than causal. So critical realists would have a problem with the phrase ‘social determinants of health’ as betraying a linear kind of thinking, whereas they hold that ‘actual’ events emerge from much more complex dynamics in which ‘real’ structures and mechanisms exert a biasing or ‘tendential’ influence.
Weinstock argued that the distribution of resources for health should be seen in the context of a range of social goods that cannot be easily isolated for their effects on health in a consequential way56. Spiegel et al advocated changing the term ‘social determinants of health’ to ‘social determination of health’57, involving the ‘4 S’ elements of (bio)security, sovereignty, solidarity and sustainability, in order to avoid targeting only individuals and communities as the site of population health interventions, when causes of the problems are at a structural and ‘intermediate’ level.
The importance of Bhaskar’s theory is that it avoids the trap of dualistic thinking between the sciences and the humanities, by providing a framework that enables both subjective and objective phenomena to be understood simultaneously, not exclusively. It rejects the philosophy of idealism, which holds that reality is immaterial and mentally constructed, asserting instead that there is a reality that exists independent of its human conception. As Price explained, interdisciplinarity in critical realism accepts that phenomena occur in open systems involving a ‘multiplicity of mechanisms emergent at different layers of reality’58. Other meta-theories such as positivism make the assumption that ‘constant event patterns’ within closed systems59 are reproduced and reproducible in widely different contexts. However, in critical realism, the social, economic and historical mechanisms at the level of the ‘real’ are uncontrollable and therefore unpredictable at any moment in time, as they operate in open systems. All other existing theories of rural health, as already described, rely primarily on empirical evidence as ‘fact’, and underestimate the significance of the ‘real’ mechanisms that result in ill health.
Because critical realism, like other critical perspectives, is focused on a concern for social justice and equality, it posits that we can better understand and explain these tendencies through the identification of structures and mechanisms at the level of the real, and that this understanding will help to bring about change and social justice. Bhaskar et al gave Marxism a philosophical foundation, for example, by casting historical materialism and class struggles in the realm of the ‘real’, namely the mechanism by which the ruling class maintains dominance over wage laborers in a capitalist system60.
Applying a critical realist approach to rural health, there are certain immutable aspects in the physical world that dominate the epistemology as a result of the lived rural experience, such as geographical distances and the topography of the rural landscape. This shapes the ‘actual’ events related to health in a significant way, to the extent of being deterministic rather than merely influential. But no less significant are the social, political and economic forces at a global, national and local level that amplify the marginalization of rural citizens. Rural areas are often described as the ‘periphery’, which is understood not only in a geographic but also in a social and political sense47. The ‘real’ structures that perpetuate disadvantage and impede social justice for rural people are less visible than the geography but may be more pernicious, such as the extractive nature of the global economy, or the tenuous relationship of many rural dwellers with the land that they occupy.
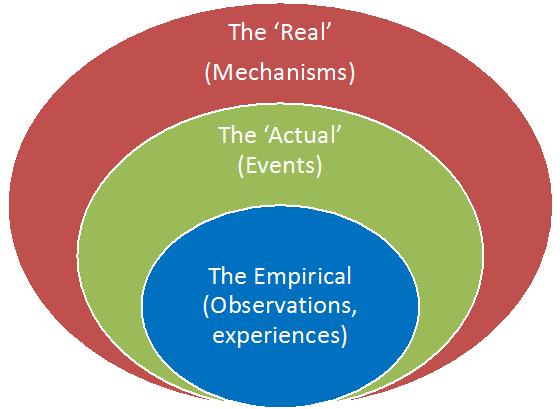 Figure 1: Diagrammatic representation of the levels of critical realism.
Figure 1: Diagrammatic representation of the levels of critical realism.
A critical realism case study
To illustrate how critical realism can be used to understand how the ‘real’ can underpin the ‘actual’, the following case study is offered for consideration.
The Ubombo water crisis
In November 2015, the district of Umkhanyakude in KwaZulu-Natal, South Africa, was experiencing a severe drought, and the people were becoming desperate. A former rural ‘homeland’ of KwaZulu in the apartheid era, it is one of the poorest districts in the country, recording an average life expectancy of 50 years in 2003, an unemployment rate of 43%, and human development index of 0.43 in 201461. The rivers, springs and boreholes had long since dried up, and communities had to rely on the daily supply of water from mobile water carriers. One such community, centerd around a small village called Ubombo, was particularly at risk because it was spread along the top of the Lebombo mountain range, where water supply had always been a problem for the district hospital and the community. This was despite the presence of the enormous Jozini dam in the valley below, which has not supplied water to local communities to any great extent. To add pressure to an already tense situation, the water trucks started coming around less frequently, until they stopped coming altogether in some areas. The community reached the end of its collective tether.
In the middle of the night on 3 November 2015, hundreds of local people got up and spread out along the national road that ran through the district. They used the only non-violent strategy that was available to them: obstruction. They hauled thousands of stones, some of them enormous, onto the road to block the flow of traffic and attract the attention of the media and the politicians (Fig2)62. And then they melted into the night, back to their homes. In the morning, the reaction was immediate: the police were called, the media took photos, the national news broadcast the story, and the stones were eventually cleared. But the water trucks never arrived.
The second part of the story concerns the hospital at the top of the mountain, a little distance from the initial protests along the national road. Over the previous few weeks the doctors had been seeing more and more cases of gastroenteritis and malnutrition as a result of the drought, as households had less water to go around. But a few days after the national road was cleared, they woke up on 6 November to find both access roads to the hospital completely obstructed by stones, and a protest in progress outside the hospital gates with a large group of people burning tyres and singing protest songs63,64.
The hospital CEO went out to meet with the protesters, and she was immediately recognized and acknowledged. ‘The problem is not with you m’am’, the protesters insisted, ‘we respect the work that you and your staff do and thank you for it. But the lack of water supply is a health issue, and people are dying, and nothing is happening. We are blockading the hospital because we need to bring the attention of the politicians to this crisis. And we need action, not more words. We will remove the stones when the water trucks return to their previous schedules.’
The journalists asked questions. Why surround the hospital? What about innocent people who may need emergency care? What about pregnant women who may need to deliver, or people needing to collect medication? Were the protesters not the same people whose family members might need to reach the hospital, or need help themselves?
The hospital remained isolated for a whole week, with food drops for the patients and staff from helicopters, until the Member of the Executive Council for Economic Development, Tourism and Environmental Affairs finally intervened and the crisis was eventually resolved after a lengthy negotiation. However, the water situation continues to this day.
How does this story relate to theories of rural health? In unpacking the particular and the generalizable aspects of the case study, the actual series of events can be differentiated from the perspectives of observation or experience, and the real forces that led to the Ubombo water crisis can be articulated.
 Figure 2: Tweets posted during the Ubombo water crisis.
Figure 2: Tweets posted during the Ubombo water crisis.
The empirical (observed, experienced)
The telling of the story and the way it is told already portrays events from a certain perspective, namely that of the author and the journalists quoted. In pretending to be objective, it would imagine that the storyteller is impartial, even absent or at least transparent. But every series of actual events is seen and told through a variety of different lenses, each of which represents varying degrees of involvement, bias, partiality and power. Ubombo is not a fictional village, but a place where the author worked as a doctor and lived with his family for a decade, and built a house in the community that they visit from time to time. His daughter was working as a doctor in the hospital at the time of the water crisis, and experienced the siege first-hand. So this disclosure invests the story with a particular bias of (medical) agency and power, but the story could have been explained in many different ways depending on who told it.
It appears there were differing perspectives of the problem at the level of experience held by the various role-players. Everyone knew that the drought was a major problem, but the health workers in the hospital appear to have seen and experienced the seriousness of it in terms of children and adults that they admitted to hospital as a direct result of insufficient and dirty water. The health managers appeared to view it as a responsibility of local government and the Department of Water Affairs that was outside of their control, while the politicians appeared to view the community as peripheral and of no political consequence. The journalists sent to cover the story may have portrayed only the most alarming aspects and images of the protests. Community members on the other hand, who were persistently and directly affected by the drought, became increasingly desperate because they were dependent on the water trucks, with no access to alternatives. This disparity in perspectives on the issue could be seen as a cause of the crisis, and they diverged further as the water tankers withdrew, until the political agency of the whole community was activated.
To relate this issue of positionality to the field of rural health as a whole, the overwhelming view represented in the literature is that of the medical establishment in high-income countries such as the USA, Canada, UK and Australia. As noted by Bourke et al earlier, this most often conforms to a deficit view, particularly when discussing the situation in low- and middle-income countries2. Community views are seldom published, and when they are the publication is usually mediated by western-trained academics65, which may reproduce and amplify the power differentials.
The actual
In view of the widely differing perspectives on the issues, the actual series of events is surprisingly difficult to pin down neatly. That there was a shortage of water as a result of the drought with inaction on the part of those responsible for water supply is undisputed and can be measured quantitatively. That this led the community to desperate measures and non-violent protest is also common cause. It is also part of the actual events that the protest blocking the roads caught the attention of the media and the politicians, and this eventually resulted in a negotiated end to the crisis, at least temporarily. But beyond these bare bones, the details of the events rely to such a degree on who experienced or witnessed them that they are difficult to distinguish from empirical observations. But describing the actual as separate from the empirical allows us to account for the multiplicity of human experience and a ‘world’ of knowing that is relative, whilst still acknowledging an absolute reality independent of human thought and narrative.
Bhaskar went beyond this duality by identifying and naming as ‘real’ the social structures and forces that conspired to bring about the actual events, even though they are intangible and abstract. Rather like gravity, the effects of which can be observed while it remains invisible and intangible as such, the ‘real’ plays an undeniable role in determining how and why things happen the way that they do. So, in trying to understand how the events came about, let alone why, it is necessary to uncover the ‘real’ forces that conspired to create the crisis.
The real
There are some significant aspects to this story. First, the scene is deliberately set in a middle-income country struggling with the historical legacy of violence and political iniquity. In contrast to much of the published literature on rural health, which often ignores these historical and contextual complexities beyond the urban–rural dichotomy, the Ubombo community lay at the centre of the ‘perfect storm’ of geographical, historical, political and economic tensions that exemplified the structural influences of both a human and non-human nature. Not only did the rural nature of the terrain make water supply to the scattered community challenging, but also the people living on the mountain had no way of accessing water by themselves after the springs and underground sources dried up. Historically and politically, the area had been part of the KwaZulu ‘homeland’, a grand apartheid scheme for ‘separate development’ built on colonial boundaries, which resulted in its becoming one of the most deprived districts in the country. As a rural district, and by most definitions a remote one, access to housing, water, sanitation, transport, education and employment opportunities, which urban dwellers often take for granted, were particularly scarce. Class differentials then come into play, as the elite can afford to access these services at a price, or at a distance.
Second, while most of the rural health literature focuses on health services, the issues around which this story revolves are intersectoral and systems-based, including political action, media, water and sanitation, health and transport. Health services were disrupted and incapacitated, serving to demonstrate their ineffectiveness in the light of the overwhelming structural issues that concentrated into a crisis. The relative place of curative medicine is magnified in this narrative: some estimates in a high-income country of the contribution of clinical medicine to health outcomes is only between 10% and 20%66,67 compared to socioeconomic factors of up to 45%. In a rural environment, physical or geographical factors play a more significant role.
Third, agency in terms of health was situated not in the hospital or its professionals, but in ordinary citizens of a marginalized rural community. In their surprisingly respectfully interaction with the hospital CEO, while not denigrating the role of clinical services, they dramatically highlighted the importance of the structural determinants of their health, in particular the water supply, by continuing to sing protest songs and burn tyres. The non-violent protest shifted some of the power for a time to community mobilizers and out of the hands of the professionals.
Discussion
This article has argued that the academic field of rural health needs appropriate frames of thinking to address the intractable challenges and ethical-moral issues in which the practical events, the ‘actual’, are immersed. The ‘real’ issues need to be discerned, articulated, described and characterized if the field is to make headway in addressing the actual on-the-ground inequities inherent in rural health. Humphreys et al, noting the limitations of systematic reviews in dealing with these complex ‘wicked’ problems, suggest that they require a ‘sustained and collaborative synthesis’ that embraces ‘ambiguity, complexity and context’68.
It is easy to feel overwhelmed by the complexity and enormity of tackling these intangible ‘big picture’ issues, and difficult to know where to start. With whom does the dialogue begin, if there are so many diverse perspectives? Airhihenbuwa and Webster asserted that interventions in a community should focus on culture rather than individual behaviors, and proposed a model that includes cultural identity, relationships and expectations, and cultural empowerment69. Since a critical realist approach involves values, it calls for action. Bhaskar later developed the concept of ‘dialectical critical realism’, indicating the imperative for interaction, dialogue and debate with those most affected, as well as advocacy for change70. The ensuing discourse between the ‘agents’ is seen as a continuous process through which individuals and organizations can change in response to feedback, even to the extent of changing social structures71. Many rural doctors and other health professionals see themselves and act as agents of change, within local and maybe regional networks, but few are prepared to get involved at the wider levels of politics and economics, which operate nationally and globally. Whereas in small rural communities, individual ‘charismatic leaders’ can make disproportionate impact on health72, and often create the platform for others to contribute their efforts productively, an entirely different level of leadership and commitment is needed at national and global levels to tackle the real forces impacting on rural health.
In Norway, a ‘joined up’ National Strategy to Reduce Social Inequalities in Health, launched in 2008, was characterized by its ‘commitment to reducing health inequalities by tackling the distribution of resources at a structural level’73. The strategy addressed poverty, education, living conditions, working environments and child welfare, as well as more proximate risk factors such as health behavior and lifestyle. But despite the comprehensiveness of the strategy, health inequalities unfortunately remained static after 10 years, possibly as a result of a failure to tackle the ‘causes of the causes’74, including political decisions at an international level.
The HIV epidemic in South Africa is a relative success story, particularly since the introduction of anti-retrovirals by government health services from 2003 in response to intense activism by the Treatment Action Campaign, a civil society organization75. What was once a terrifying, life-threatening disease, marked by distressing opportunistic infections and dread, has essentially become just another chronic disease that is controlled by daily medication. Exposing the ‘real’ by identifying and tackling some of the political, economic and social drivers of the epidemic collectively has enabled it to be brought under control, and the needless disruption or loss of millions of lives avoided. Nevertheless, persistent gender and economic inequality continue to cause the incidence of new infections to remain high.
The rural determinants of health
Using the theory of critical realism, the ‘actual’ events in the field of rural health can be understood at the level of the ‘real’ in terms of immutable determinants on the one hand, such as the geographic and historical issues that frame the field, across a spectrum through the political and economic determinants that do change or are changed over time, to the social and cultural determinants that are the subject of much of the dialectical engagement that Bhaskar suggests.
As already noted, however, the playing fields are not equal: rural areas are persistently and systematically disadvantaged on several levels that impact on health, in low- as well as high- income countries1. In Figure 3, this bias is illustrated as an uphill struggle against the immutable geographical and historical determinants that ‘weigh down’ the field of rural health to the left of the diagram. Articulating the real forces in operation uncovers the inequities inherent in our systems, to which specific resources and attention need to be addressed. While geographical factors can be mitigated by efficient and appropriate transport systems, for example, the historical antecedents of actual rural issues are more difficult to moderate.
Most open to deliberate and direct control are the health systems on the right of the diagram that limit or enable access to the resources, human and other, that people need to stay healthy. In the middle are political and economic forces that influence the broader allocation of limited resources most often in favor of the urban elite, and to the detriment of the rural poor. These forces are to a certain extent open to political lobbying, advocacy and activism, as in the South African HIV and AIDS example. Ignoring the other influences in this example and the case study means that the actual problem of inequality persists despite some shorter term improvements, as noted in the case study. The image portrays the rural determinants of health with equal weighting, whereas it is clear that different factors will play a lesser or greater role in different situations and contexts.
Understanding this range of contributors to the Ubombo water crisis might have given the health professionals a greater sense of agency during the protests, by engendering a sense of solidarity with the community members who were striving for better health. Systems for emergency water supply, for example, could have been developed collaboratively. Understanding the bigger intersectoral picture could have stimulated the health managers in the district to work laterally with their peers in local government and the Department of Water Affairs, proactively looking for opportunities to ensure the water supply in the longer term. Faced with a united cohort of middle managers advocating for their respective areas of responsibility, the politicians might have responded earlier with the resources needed, taking responsibility for reversing the historical disadvantage of the communities that had been neglected during the planning of the nearby dam. The crisis as a whole could have been a political opportunity to improve the living conditions in one of the poorest districts in the country. However the economic, power and class disparities that weaken solidarity between those involved, as well as the changing global climate, will not transform quickly, and these ensure that the water issues have continued to recur each year to date.
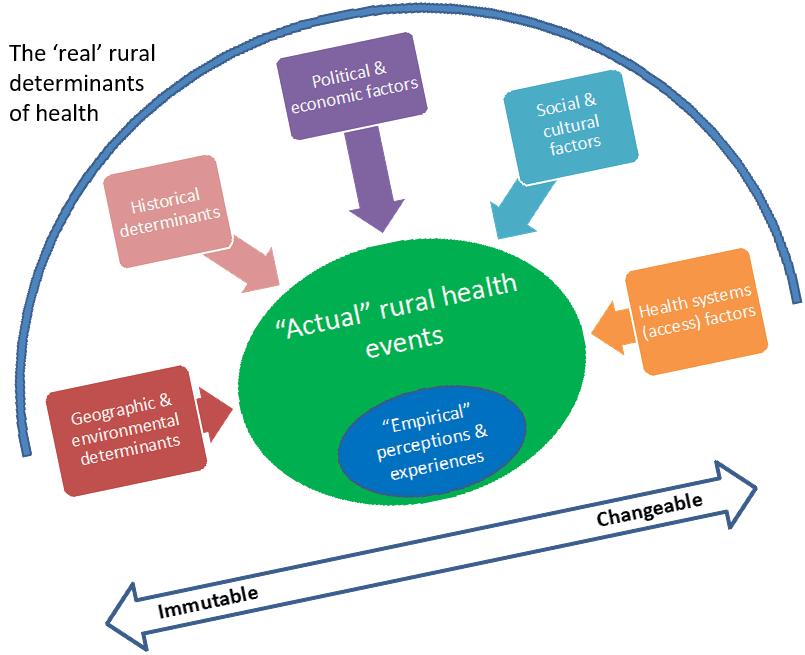 Figure 3: Diagrammatic representation of the rural determinants of health.
Figure 3: Diagrammatic representation of the rural determinants of health.
Conclusion
Why are rural people so persistently and ubiquitously disadvantaged in terms of their health? It may be because the ‘real’ determinants of rural health, unacknowledged and invisible as they are, are nevertheless extremely powerful, amplifying one another by virtue of their synergistic effects. Although it is not feasible to propose that a single, all-encompassing theory can explain all the complexities of rural health, critical realism offers a holistic framework to consider a broad set of options while acting within the pragmatic realities of rural practice. It allows us, whatever our experiential and political viewpoint, to view rural health as being framed by the geography and history of place, impacted by the politics and economics of a region, and experienced as socially and culturally distinct. Within this comprehensive perspective it becomes apparent that there exists a bias or set of forces in each of these ‘real’ arenas operating persistently to the disadvantage of rural areas. The resulting ‘actual’ events of health or illness, both individually and collectively, emerge as a result of an interplay of these forces with the resources of the health system, over which agents in the system, such as citizens, health workers, managers and policymakers, have some direct control.
Acknowledgements
This article was first presented at the 13th Wonca World Rural Health Conference held in Delhi, India, in April 2018. The author is grateful to Professor David Sanders of the University of the Western Cape, South Africa, for his comments on an earlier draft of this manuscript.
References
You might also be interested in:
2022 - Managing hospitalized patients with bacterial infections: the price-to-pay upon site of infection
