Introduction
Although a cheap and effective vaccine for measles is available, every day measles kills about 360 children worldwide1. Measles is considered the leading cause of death among children, and rubella causes fetal death or congenital anomalies2. Measles eradication was planned in 1980s after the eradication of smallpox; however, WHO concentrated on polio eradication first3. After a commendable achievement on a polio-free South-East Asian region (SEAR) by March 2014, WHO is now focusing towards measles and rubella elimination by 20204. As a part of this initiative, India introduced measles and rubella (MR) vaccination in the routine of the Indian national immunization schedule as two doses: the first at age 9 months and the second at age 16–24 months5. In addition to attaining the minimum 95% of herd immunity level in the community, supplementary immunization activity was launched to vaccinate children aged between 9 months and 15 years5. At the same time, there was a negative campaign going in social media against this initiative. Despite this, India introduced one of the world largest immunization campaigns on MR vaccination, with the aim to cover more than 95% of children between 9 months and 15 years6. India introduced this program over four phases in 36 states, including seven union territories7. As part of phase 1, this was first implemented in the highly performing southern Indian states, including Tamilnadu, on 5 April 20172.
The Rural Health Training Centre of Pondicherry Institute of Medical Sciences is located in Chunampet, Kanchipuram district, which has been working continuously with 25 staff for the health care of rural and remote communities for more than 15 years. Interns (training doctors) and students are posted on a rotation basis as residents in this center. The Rural Health Training Centre also covers adjoining 20 villages by active routine surveillance and outreach activities. As a part of surveillance, it was planned to assess the coverage of MR vaccination after the supplementary immunization activity campaign. Serology-based monitoring is ideal and confirmatory, but in practice it is very difficult to carry out and hence a WHO-recommended rapid surveillance method was used to assess the coverage of MR vaccination in the rural area of Kanchipuram district, Tamilnadu8.
Methods
Data collection was done immediately after phase 1 of the MR vaccine campaign (within 10 days). Data collection was based on the WHO-recommended 30/7 rapid monitoring method. Using this method, 30 clusters are selected from the study population and seven samples are selected from each cluster using any standard probability sampling method. In a rural area where household details are not available, a street is randomly selected from the center of the village and then a house selected in that street (first house), and then subsequent nearest houses will be surveyed from that point. A survey has to be completed within a month to ensure the data are as uniform as possible8.
In the present study, 30 villages around the Rural Health Training Centre were selected8. Villages were selected based on the convenience of distance (Fig1). After reaching the selected village, one street was randomly selected. After selecting the first house randomly from that street, subsequent nearby houses were selected until the sample size was attained. The first available seven children aged between 5 years and 16 years, and the first available seven children in the age group of 9 months to 5 years (a total of 14 children in each village), were included in the study from each village. Data collection was done using a pre-tested questionnaire. This questionnaire was developed in English and translated to the local language (Tamil) and then back-translated to ensure quality. This questionnaire was pre-tested with 10 participants and modified before starting the main study. The questionnaire consisted of questions relating to demography and sociodemographic details, vaccination history, adverse event history and awareness about vaccination. Children were classified into ‘vaccinated’ or ‘not vaccinated’ based on the vaccination card and/or vaccine mark in the finger and/or information from the parent (WHO ‘card or history’ method)8. Data were collected by a team of trained interns and medical social workers.
Data were double-entered in Epidata software and analyzed using the Statistical Package for the Social Sciences v22.0 (IBM; http://www.spss.com). Chi-squared testing was used to find out the association. To find out the strength of association and confounding factors, a crude odds ratio was generated for all variables and an adjusted odds ratio was generated using binominal logistic regression model by entry method for the significant variables. Mapping of the villages was done using QGIS v7.2.2 (QGIS; http://www.qgis.org) (Fig1).
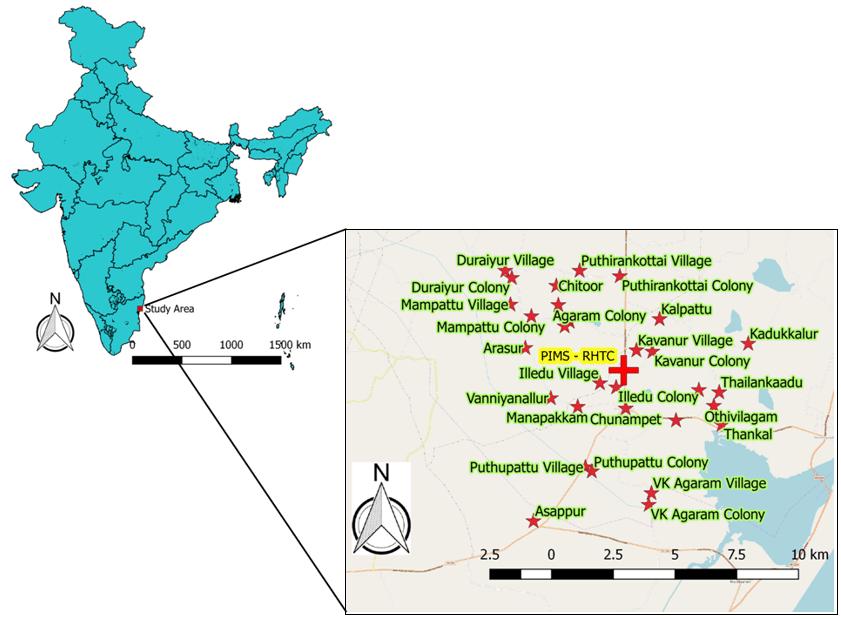 Figure 1: QGIS mapping of 30 villages in southern India, surveyed after supplementary immunization activities of measles and rubella vaccination campaign in April 2017.
Figure 1: QGIS mapping of 30 villages in southern India, surveyed after supplementary immunization activities of measles and rubella vaccination campaign in April 2017.
Ethics approval
Required ethics principles were followed by taking consent from the participants, adopting the principles of the Declaration of Helsinki9. Abiding the ICMR 2017 guidelines, after providing the participants information sheet, a written consent was obtained from the parent or legally acceptable/authorized representative and an oral assent was obtained from the children aged 7–15 years. Confidentiality of the data was ensured at all levels. Coding of personally identifiable information was done. Data were maintained in a password-protected file. As this is the authors’ field practice area, the response from the community was good and no invasive tests were carried out in the survey.
Results
In this study with a total sample of 420 children, 380 children (90.5% (range 87.4–93.0%)) were found to be vaccinated and 40 children (9.5% (range 7.0–12.6%)) were found to be unvaccinated. Most of the people came to know about the MR vaccination through auxiliary nurses and midwives followed by teachers (Table 1). The main reason for not getting vaccinated was fear of an adverse event following immunization or fear of injection (Table 1). Reasons for not vaccinating the children were significantly associated with use of a smartphone by at least one of the parents (adjusted odds ratio (OR) 2.1 (1.1–4.2)), a better literacy level among mothers (adjusted odds ratio for high school and above 5.2 (1.1–24.8) and poor literacy level among fathers (adjusted odds ratio for illiterate 3.6 (11.1–11.5)) (Table 2).
The main finding in this study was that, despite the various negative propaganda disseminated in the social media, the coverage of vaccination by the healthcare providers was near optimal (90.5%), which shows the strength of the public health system in this rural area of southern India. This is the first study about MR vaccination coverage, and there are a paucity of similar studies in the literature. The present findings correlate with the government report published at the end of the campaign, claiming 96% MR vaccination coverage10. Auxiliary nurses and midwives played a major role in disseminating the information about the campaign in the rural areas (Table 1). They are grassroots health workers working at the village level, who usually cover 5000 people (four or five villages) at the subcenter under the supervision of the medical officer in charge of the primary health center. This center usually covers a population of about 30 000. As this program targeted and was implemented mainly in the schools, school teachers also played a major role in providing information regarding MR vaccination.
The main reasons for not getting vaccinated were fear of injection and adverse event following immunization (Table 1). There were several rumors circulating in the social media, warning parents not to allow their children to get vaccinated. Even minor adverse events were magnified in the media, adding public tension. In this study, it was found that those using smartphones (at least one of the parents) and the mothers with higher educational qualifications were associated with not vaccinating their child and a lower acceptance rate11. This is called vaccine hesitancy, which is common for both developed and developing countries12. Bethou and Chandrasekaran have raised a concern about the success of the MR campaign in southern India due to negative social media propaganda11. They also documented that this is a classic example of how false information in social media can have a negative effect and create a dent in the entire public health mechanism. Palanisamy et al have found that those who have good social capital and trust in their neighborhoods have better acceptance rates than those who trust social media6. The Government of India has also identified that, during phase 1, negative messages on social media, inadequate communication material for parents and teachers, suboptimal advocacy and inadequate sensitization of private and government school principals were the challenges faced7. One more finding in the present study was that fathers with lower education are associated with not vaccinating their children; the exact reasons need to be explored further.
Table 1: Main source of motivation for measles and rubella vaccination and reasons for not getting vaccinated among survey participants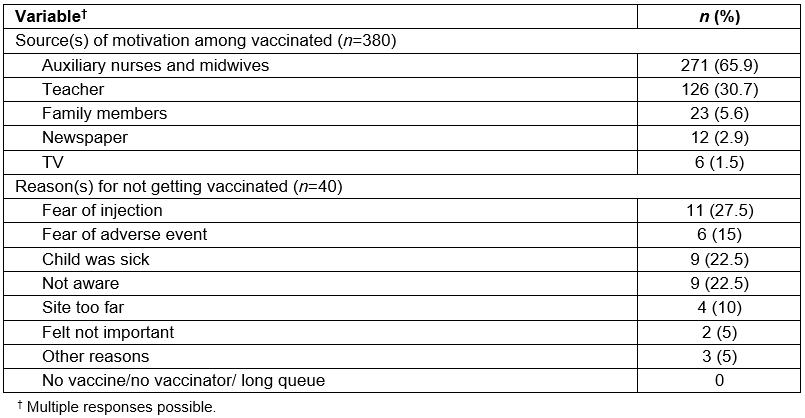
Table 2: Factors associated with measles and rubella vaccination failure in a rural area of South India after phase 1 of supplementary immunization activities in April 2017, binominal logistic regression model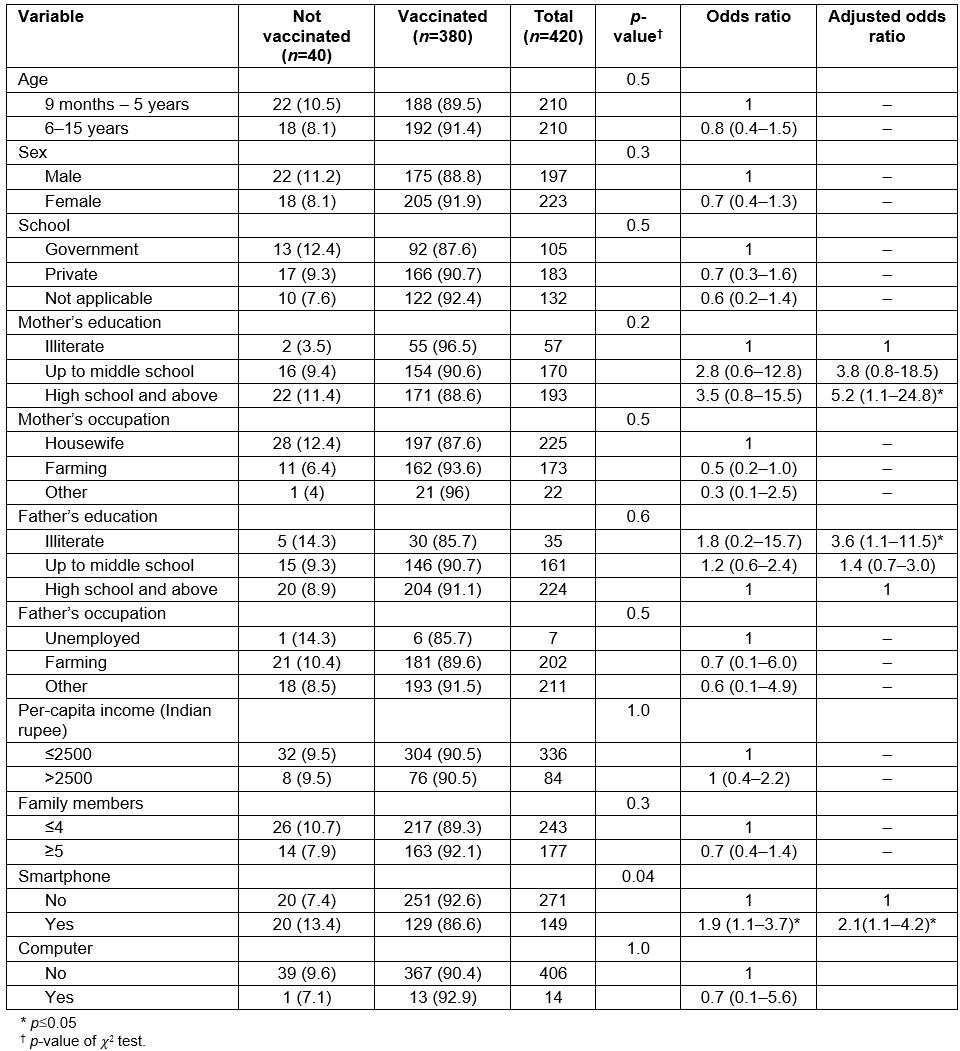
Discussion
In accordance with modern technology, public health policy makers should think about and plan information education and communication activities to tackle negative propaganda through social media. Legal measures may also be planned if there is any active negative campaign in the social media, but with caution. In the long run, proper health education and awareness will help the community to take a positive decision towards vaccination. As a way forward it is recommended to assess the coverage based on serology. Mixed-method and qualitative research may bring more details on the perception of healthcare providers and people’s views about MR vaccination in future.
A strength of this study is that it was done immediately after phase 1 of the MR campaign to determine the coverage of vaccination in a rural area of southern India using a WHO-recommended method. This survey was conducted independently, which makes the observations free from reporting bias and conflict of interest from government agencies. This is the first study to report the coverage other than government reports. One of the limitations in this study was reliance on history and/or vaccination card and/or fingermark for the confirmation of vaccination, which is not as robust as confirming with serology.
Conclusion
The coverage of MR vaccination in a rural area of southern India was near optimal during phase 1 of the studied MR vaccine campaign.

