Introduction
Australian Aboriginal people, including children, experience poorer levels of oral health, suffering from more dental caries, periodontal disease and tooth loss, than non-Aboriginal people1,2. Fifty-seven percent of Aboriginal Australians have untreated dental caries, compared to 25% of non-Aboriginal Australians. Aboriginal Australians have a mean decayed surfaces (DS) score of 2.7 compared 0.8 for non-Aboriginal people1. Such large differences in oral health can be attributed to many factors, including limited access to culturally competent dental services, low fluoride toothpaste usage, diets high in refined carbohydrates and limited oral health promotion resources3.
Improving Aboriginal oral health is a priority in both the Australian National Oral Health Plan and the New South Wales (NSW) Aboriginal Oral Health Plan4,5. Providing culturally competent and sustainable oral health promotion plays a key role in this process, especially in rural and remote communities4. Oral health promotion targeted towards Aboriginal people is more likely to be effective if the promotion addresses the social determinants of health, is sustainable, and is owned by the community6.
Cultural competency can be defined as ‘a set of congruent behaviours, attitudes, and policies that come together in a system, agency, or amongst professionals and enables that system, agency, or those professionals to work effectively in cross-cultural situations’7.
Specifically in the delivery of health services and/or education programs in the Australian context for Indigenous people this involves providing programs that are evidence based, culturally and linguistically appropriate, sustainable and enable collaboration with communities and evaluation. These programs should be developed in consultation with Aboriginal community controlled health services and local Aboriginal communities and be tailored to the needs and preferences of the specific communities8.
Therefore, culturally competent oral health promotion should be evidence based, sustainable and developed in consultation with local Aboriginal communities to ensure the needs of the individual communities are met.
In 2013, an oral health service was established for Aboriginal people living in rural and remote communities in central northern NSW, following an invitation from the local Aboriginal community to the NSW Centre for Oral Health Strategy and Poche Centre for Indigenous Health to provide dental services in the region9. It provides preventive oral health services and dental treatment for Aboriginal children and adults in partnership with local Aboriginal community controlled health services. In addition, the oral health service provides vocational training opportunities (Certificates III and IV in Dental Assisting) to train local Aboriginal dental assistants and build the capacity of the local Aboriginal community. Tertiary education pathways in oral health are also offered to increase the number of Aboriginal people in the oral health workforce.
A program of research has been developed to evaluate the oral health service. The program of research includes the development of the oral health service9, the perspective of Aboriginal clients on the oral health service10, a qualitative study involving the clinicians who operate the service11 and a costing analysis12. As part of the development of the oral health service, sustainable and targeted oral health promotion was identified as a high priority by the local Aboriginal community, prompting the development of this study.
This study was developed in consultation with two local Aboriginal community controlled health services and aimed to determine (1) the oral health needs of Aboriginal children aged 5–12 years, (2) the oral health knowledge and attitudes towards oral health of parents/guardians and (3) the perceived barriers and enablers towards oral health promotion for school children by local school staff and community health workers to inform the development of a community-owned oral health promotion program.
Methods
The precede–proceed model of health program planning was used to design a comprehensive survey and guide the collaboration with local communities. The model focuses on identifying predisposing, reinforcing and enabling factors to plan and implement a health promotion program13. This study included an epidemiological assessment of all Aboriginal children aged 5–12 years enrolled in local schools, plus an educational and ecological assessment of the community through oral health questionnaires to record oral health knowledge and attitudes towards oral health to identify these factors and inform a targeted preventive oral health program.
This study took place between May and November 2014, in three communities in central northern NSW with a predominantly Aboriginal population. Three schools participated in this study, which enrolled the majority of Aboriginal children and a majority of Aboriginal students. In each community, a local health centre provided health services for Aboriginal people. All Aboriginal children aged 5–12 years enrolled in local schools, their parents and/or guardians, as well as school staff community health workers, were eligible to participate.
Children with a valid consent received a dental screening, using a standardised protocol developed by the Australian Research Centre for Population Oral Health, which has been used for other epidemiological studies in NSW14. Screenings were undertaken in schools by a single examiner (YD) who was trained in the diagnostic criteria. Criteria for dental caries included pre-cavitation of the enamel, cavitation of the enamel and involvement of the enamel and dentine due to caries. Plaque and gingivitis was assessed using the Silness and Loe Index15. Caries was diagnosed using a mirror, light, blunt probe and compressed air. The data were recorded directly into a specifically designed computer program.
The number of decayed (d/D), missing (m/M) and filled (f/F) teeth (t/T) was used as the measure of caries experience (dmft/DMFT). DMFT refers to permanent teeth, dmft refers to primary teeth and dmft/DMFT refers to the overall caries experience.
All children who received a dental screening also received follow-up dental treatment and preventive care through the local oral health service.
Children were asked to complete an interviewer-assisted questionnaire, which included questions pertaining to their current oral hygiene practices, dental history, self-reported regular consumption of foods and self-reported food knowledge. Parents and/or guardians of participating children were asked to complete an interviewer-assisted questionnaire assessing dental history, oral hygiene practices and attitudes towards oral health. School staff and community health workers were asked to complete an interviewer-assisted questionnaire assessing attitudes towards oral health and perceived barriers and enablers towards various oral health promotion strategies aimed at improving the oral health of Aboriginal children.
Interviewer-assisted questionnaires were completed with the help of interviewers from the local dental team, including an oral health therapist (YD) and local Aboriginal dental assistant (NB). No language barriers were encountered.
Questionnaire responses were analysed using descriptive statistics, including the Statistical Package for the Social Sciences v22 (SPSS; http://www.spss.com). Caries experience, as measured using the dmft and DMFT indices and the percentage caries free, were analysed using the Statistical Analysis Software Enterprise Guide v7.1 (SAS Institute; http://www.sas.com).
Ethics approval
The study was approved by the Aboriginal Health and Medical Research Council’s ethics committee as part of the larger study on the evaluation of the collaborative oral health service in central northern NSW (app. no. 1004-14). A participant information statement was provided to all parents and/or guardians and signed consent was sought for each child’s participation in the study. Verbal assent was sought from the children themselves at the time of the data collection. Results of this study were reported back to the local Aboriginal community at an open community forum.
Results
There were 94 children who were eligible to participate in this study; 88 (93.6%) were screened and 78 (83.0%) completed the children’s oral health questionnaire (Fig1). Table 1 shows the majority of children (77; 87.5%) had dental caries with an overall mean dmft/DMFT for the primary and permanent dentitions of 5.3. There was a mean decay score of 4.7 (d=4.06, D=0.66).
The majority (71; 80.7%) of children presented with level 2 or 3 plaque scores (‘moderate’ to ‘an abundance’ of soft deposits of plaque on the teeth or gingiva), inflammation of the gingiva (66; 75.0%), and nearly a quarter (21; 23.9%) had a dental abscess (infection) associated with a decayed tooth (Table 1).
Of the 78 children who completed the survey, over a third (28; 35.9%) did not own a toothbrush and 19 (24.4%) did not use toothpaste. Only 10 (12.8%) children brushed their teeth in the morning when they answered the questionnaire and half (40; 51.3%) could not remember the last time they brushed their teeth (Table 2).
Table 2 shows that 65 (83.3%) children reported having suffered from toothache at some stage, and 23 (35.4%) reported that dental pain had caused them to be absent from school. Only 35 (44.9%) children reported they had seen a dentist.
A majority of children reported eating fruit (69; 88.5%) and vegetables (59; 75.6%) regularly. There was high, self-reported, regular consumption of sugary drinks (50; 64.1%) and sugary foods (56; 71.8%). School staff (30; 76.9%) also noted that children eat foods high in sugar at school. Twelve percent (10; 12.8%) of children did not consume tap water regularly and five percent (4; 5.1%) of children reported that tap water was unhealthy.
The majority of children thought that fruit (74; 94.9%) and vegetables (69; 88.5%) were healthy and that soft drinks (75; 96.2%) and sugary foods (75; 96.2%) were not healthy.
A total of 32 parents and/or guardians completed the oral health questionnaire (Table 3), with at least one parent/guardian for each child participating. Most parents/guardians were female (28; 87.5%); and the majority identified as Aboriginal (30; 93.8%).
There were 24 (74%) parents/guardians who had noticed signs of dental caries in their child’s teeth, including black teeth, brown teeth and rotten teeth. Sixty-eight percent (22) reported their child had previously experienced toothache; however, only a quarter (8) reported their child had accessed dental treatment regularly. Reasons for not having regular dental treatment included transport difficulties (13; 40.6%), dental services too far away (10; 31.3%) and their child was not in pain (10; 31.3%).
Table 3 shows that a majority of parents/guardians (31; 96.9%) owned their own toothbrush, as did their children (27; 84.4%). While most (31; 96.9%) parents/guardians agreed that toothbrushing helps children’s teeth, only half (17; 53.1%) reported that they helped their children to brush their teeth. Over a third (12; 37.5%) of parents/guardians agreed that dental caries in the primary dentition does not matter as these teeth will fall out anyway. A quarter (8; 25.0%) of parents/guardians did not know if there was much they could do to stop their child from getting holes in their teeth and nearly half (15; 46.9%) did not know that giving a baby a bottle of milk to take to bed as a comforter can cause dental caries.
A total of 37 school staff and two community health workers completed the oral health questionnaire. This was a majority of the school staff and health workers employed in the local schools and community health centres at the time. School staff included school principals (n=3), teachers (n=19), administration staff (n=4) and learning support staff, including Aboriginal education officers (n=11). Eleven of the school staff identified themselves as Aboriginal.
The majority of respondents (36; 92.3%) agreed that most people will usually get problems with their teeth. However, most (38; 97.4%) agreed that keeping their teeth healthy is important to them. When shown a picture of dental caries, almost all (38; 97.4%) had noticed dental caries in children in their school or health centre, and 33 (84.6%) reported that children often complained of toothache.
Eighty-nine percent (35) of school staff and health workers were concerned with the number of children who experienced dental caries in their community and all agreed that action should be to be taken to address this, and supported a community oral health promotion program. A majority (36; 92.3%) were willing to receive training to facilitate such a program.
Table 4 shows the various oral health promotion strategies presented to school staff and health workers. The majority (36; 92.3%) believed that a school-based daily toothbrushing program would be most beneficial, followed by in-school oral health education (32; 82.1%), providing healthy food (24; 61.5%), implementing a fluoride varnish scheme (19; 48.7%) and providing chilled water fountains (16; 41.0%). Perceived barriers to establishing school-based oral health promotion program included time constraints in the school day (21; 53.8%), lack of time in the curriculum (17; 43.6%) and children who might not be willing to participate (12; 30.8%).
Table 1: Demographic characteristics and oral health status of participating Aboriginal children (n=88)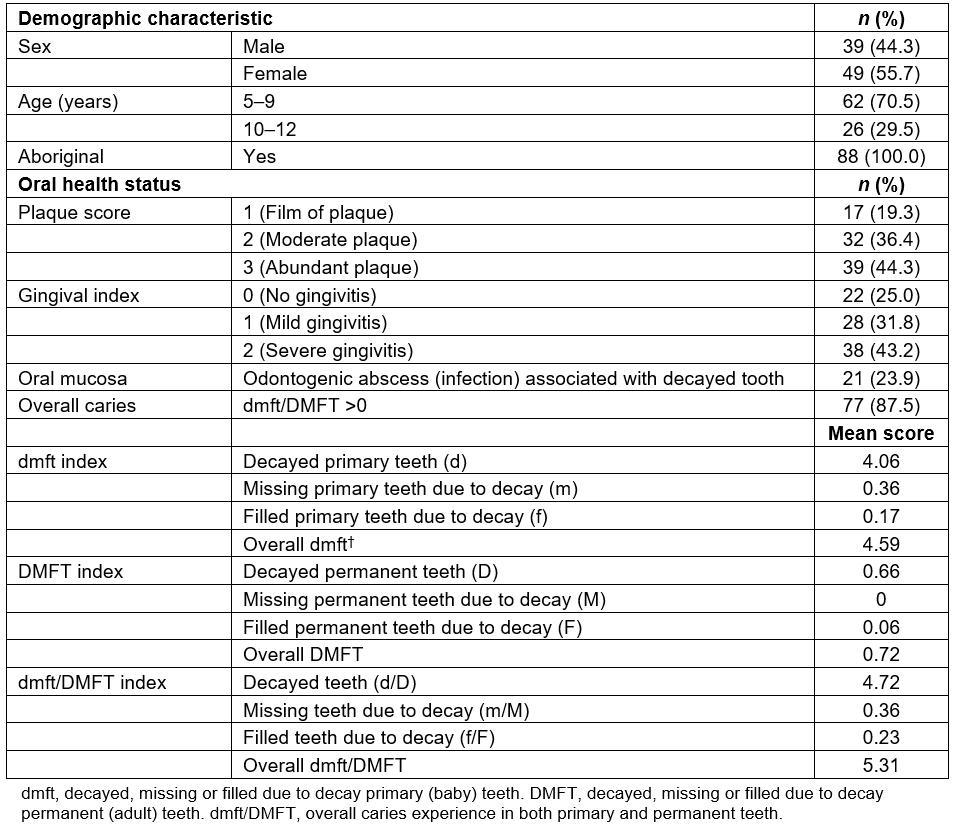
Table 2: Self-reported oral hygiene history, food consumption and food knowledge of participating Aboriginal children (n=78)>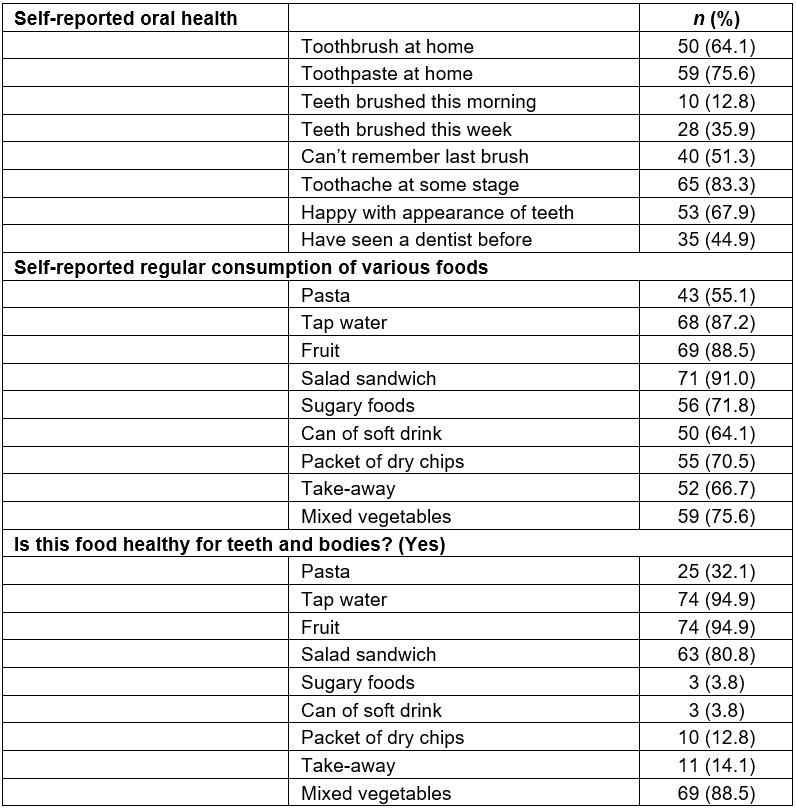
Table 3: Demographic characteristics and attitudes towards oral health of parents/guardians of Aboriginal children (n=32)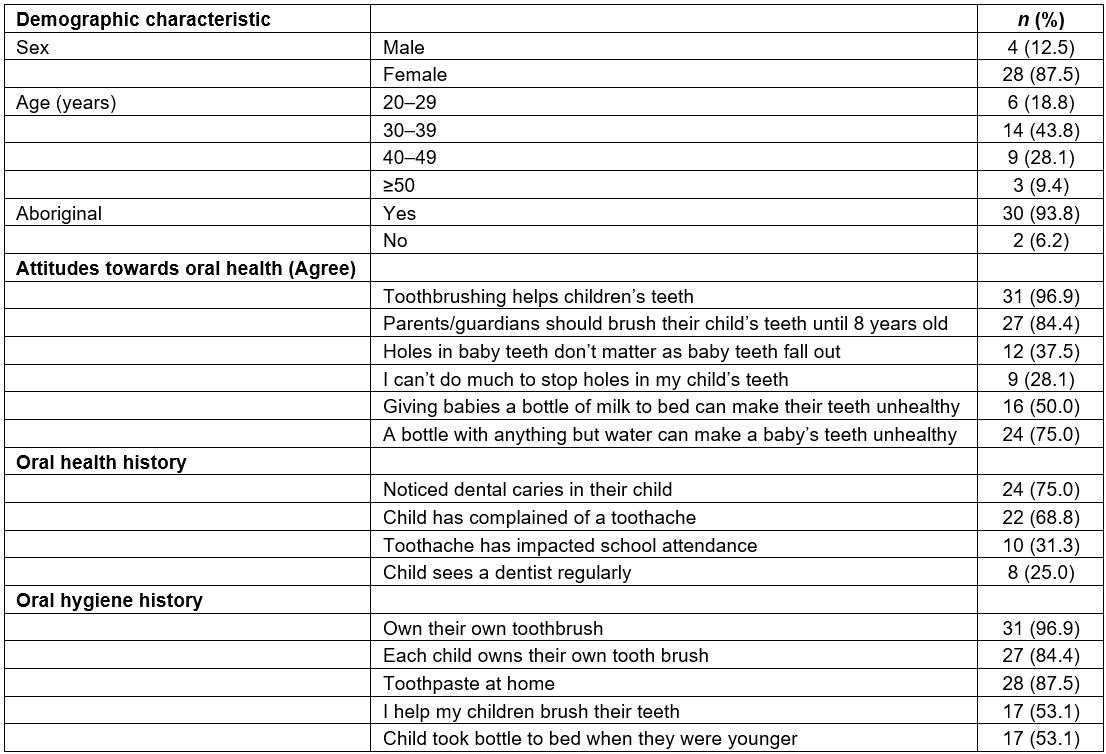
Table 4: Demographic characteristics, attitudes towards oral health and perceived barriers and enablers towards oral health promotion of local school staff and health workers (n=39)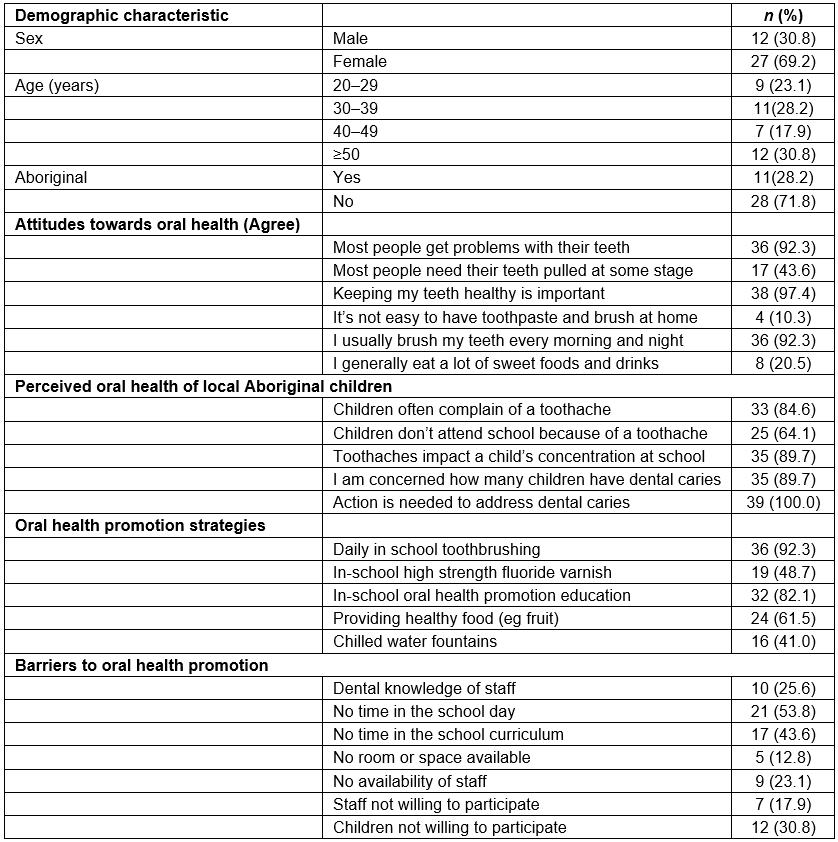
Discussion
This study found that a majority of Aboriginal children aged 5–12 years living in central northern NSW study communities had a high burden of untreated dental disease, with a mean dmft/DMFT of 5.3, which is three times that experienced by non-Aboriginal children in NSW14. Untreated dental caries is clearly a serious problem for Aboriginal children, which progresses rapidly and leads to severe pain, anxiety, infection and sleep loss16. It is clear that dental treatment services are urgently required to reduce the burden of pain and sepsis; however, it is impossible to overcome dental disease through treatment alone. Dental caries is a chronic health problem that can be prevented; therefore, the focus should also be on developing effective, sustainable and culturally competent oral health promotion17.
Over a third of children did not own their own toothbrush and the majority could not remember the last time they brushed their teeth. These toothbrushing rates are comparable to Aboriginal children living in other rural and remote Australian communities2. Furthermore, this study has shown that daily use of fluoride toothpaste is limited in Aboriginal children living in rural and remote Aboriginal communities in NSW. Limited daily toothbrushing with a fluoride toothpaste is a risk factor for dental caries18. The daily use of fluoride toothpaste has been shown to be one of the most effective ways to control dental caries19. Hence regular toothbrushing to apply the toothpaste should be an integral part of any oral health promotion program. School-based toothbrushing programs in Aboriginal communities have shown to increase the number of children who own their own toothbrush and brush twice a day20. The application of high-strength fluoride varnish three times a year can also reduce dental caries21. For example, a fluoride varnish program that incorporated community oral health education was effective in reducing dental caries in Aboriginal children living in remote communities in the Northern Territory, Australia22.
The majority of children stated that fruit and vegetables were healthy foods and that soft drinks, take-away foods and sugary foods were not healthy, indicating a sound level of healthy food knowledge. However, there were high rates of self-reported consumption of sugary drinks and foods, and these are risk factors for dental caries23. Similar findings from the state of Victoria also noted a reliance on sweetened beverages and energy-dense foods in Aboriginal families. The authors advocated evidence-based child nutrition advice for Aboriginal families24. The issue of high consumption of sugary drinks and foods in rural and remote communities is compounded by the poor availability and high cost of fresh foods3.
A concerning finding of this study was that over 12% of children did not consume tap water regularly and that 5.1% identified tap water as ‘unhealthy’. There has been a history of poor water quality in some of the communities involved in this study25. This could be contributing to the notion that water is ‘unhealthy’ and may be increasing the consumption of sugary drinks rather than water. A structured water bottle program for Aboriginal pre-school children has been successful in getting children to drink water rather than sugary drinks in Aboriginal communities in central Queensland26 and could be a beneficial option in a health promotion program.
Parents/guardians demonstrated limited oral health knowledge in regards to baby teeth, infant feeding practices and how dental caries can be prevented. Infant feeding practices such as putting a young child to bed with a bottle containing milk can be a risk factor for early childhood caries27. This demonstrates the need for oral health education, which should be preferably delivered by Aboriginal health workers28,29.
Oral health promotion programs are more likely to be effective in Aboriginal communities if they are well supported and owned by the local community6,30. The positive attitudes of school staff and health workers towards improving oral health and a willingness to support school-based oral health promotion are important enablers in the development of oral health promotion in the future. However, the perceived barriers, including time constraints and participation of students, must be taken into consideration when planning oral health promotion strategies, to ensure local support.
Through this collaboration with Aboriginal communities in central northern NSW, several risk factors for dental caries were identified, including lack of toothbrush ownership, limited daily toothbrushing with fluoride toothpaste, frequent consumption of sugary foods and drinks, and limited oral health knowledge. Oral health promotion strategies for Aboriginal children in rural communities in NSW should target these risk factors, and funding for these strategies should be prioritised by policymakers in relevant health districts.
Based on the risk factors identified, oral health promotion strategies for Aboriginal children living in rural and remote communities in NSW should (1) aim to increase access to and use of fluoride through the provision of free oral health resources, including toothbrushes and toothpaste, school-based toothbrushing programs and the application of fluoride varnish three times per school year, (2) aim to ensure that safe and refreshing tap water should be available and accessible to encourage the consumption of water rather than sugar-sweetened beverages (or chilled water fountains and water-only policies in schools if this cannot be guaranteed), (3) provide culturally competent oral health and nutrition education and (4) provide training programs to build the capacity of local Aboriginal communities and the existing health workforce to ensure that oral health promotion is led and supported by local Aboriginal communities.
Following this study, the results were reported back to local Aboriginal communities at an open community forum (yarn up). The strategies were presented to the local community as a response to the identified need for oral health promotion. The communities supported the development of an oral health promotion program based on these strategies that would be implemented in local schools the following calendar year through the oral health service.
Treatment alone will not solve the problem of high rates of dental caries in Aboriginal children. The focus of resources must be on implementing a public health solution by increasing access to fluoride and reducing the consumption of sugary foods and drinks. These messages are not new and it is disappointing that policymakers have not put resources into preventive programs, to date, in an attempt to close the ‘dental health gap’ between Aboriginal and non-Aboriginal children. Data collected from the three Aboriginal communities involved in this study should be a catalyst to deliver a public health solution to dental disease.
There are limitations to this study, as the consultation process took place in three small, rural and remote communities. However, although the sample sizes were modest, this study represents 94% of the Aboriginal children enrolled in the local schools, at least one parent or guardian for each child, and a majority of local school staff and community health workers. Small numbers precluded detailed statistical analyses. However, response rates were high, indicating collected data should be representative and will be of value for planning purposes. This study collected the baseline data to inform targeted oral health promotion strategies that could be implemented locally in Aboriginal communities in central northern NSW. Future research aims to further develop an oral health promotion program with the local communities, pilot the program in the three schools that participated in this study and evaluate the program.
Conclusion
Aboriginal children living in rural and remote communities in NSW experience high rates of dental caries that can affect general health, quality of life and school attendance. As part of this study, several risk factors for the development of dental caries were identified, including low levels of toothbrush ownership, daily toothbrushing and fluoride toothpaste usage, and frequent consumption of sugary foods and sweetened drinks. Culturally competent oral health promotion strategies are urgently required to address these risk factors, which are well supported by the local Aboriginal community. Funding for these strategies should be prioritised by NSW policymakers to improve the oral health of Aboriginal children in rural and remote communities in NSW.


