Background
Rural populations are aging. In rural, non-metropolitan areas of the USA, 19% or more of the population is aged 65 years or more compared to 15% of those of the same age range in non-rural areas1. Rural areas also have a larger percentage of those aged 85 years and older2. Living in rural areas as one ages often means less availability of and access to medical services and a lack of healthcare providers1,3. The implication on rural-residing older adults is significant as they have higher rates of chronic conditions and frailty4. Additionally, these rural older adults have limited access to goods and services and often have lower incomes than urban-dwelling older persons5. This combination of increased numbers of rural-residing older populations1, along with greater chronic health conditions and limited health resource access, creates increased economic and workforce strain on those existing and limited support systems.
The aforementioned health disparities and inequities necessitate providers working together across disciplines. These multidisciplinary efforts are frequently used in practice, but often lack synergy and collaboration. Although ‘multidisciplinary’ and ‘interdisciplinary’ often used interchangeably, there are distinct differences between them6. Multidisciplinary practices focus on the dominance of each individual discipline. Interdisciplinary efforts are better suited to address rural health disparities and inequities due to a primary focus on person-centered care. Rather than being housed in individual disciplines, interdisciplinary partnerships can improve rural health resource access through practitioners working and learning from each other and thus blending the complementary skills of individual disciplines to increase care’s holistic nature7. By removing silos among health professionals, the impact of health resource shortages in rural areas can be reduced.
Purpose
Interdisciplinary teams are a way to address the complex issues of aging, and this approach is particularly critical to aging in rural places8. The goal of this commentary is to present a conceptual partnership model that integrates nursing, gerontology, and public health disciplines for support of rural-residing older adults. The importance of interdisciplinary approaches that ultimately enhance the quality of life of rural-residing older adults is described. Benefits of discipline pairings and total integration of these pairings provide a comprehensive overview of the strength of interdisciplinary partnership integration for improving rural health resource access.
Partnership integration
Interprofessional collaborations in health are inescapable in today’s increasingly complex healthcare environment. More work is needed to understand how disciplines can work together to address chronic disease, long-term complex health issues9, and transitions of care10. Researchers continue to define interdisciplinary models and analyze the health impact of such models, but this literature is limited to a small pool of interdisciplinary studies11.
In general, the steps toward interdisciplinary efforts begin with identifying the complementary nature of work provided within pairing of specific disciplines. An innovative model that expands and develops collaborative relationships with researchers, rural hospitals, area health education centers, and other public and private agencies outside of and within the aging network improves health resource access for rural-residing older adults. Public health, gerontology, and nursing disciplines presented as pairs/dyads are incorporated as a conceptual interdisciplinary model. This illustrates the integration of these types of disciplines, and their interactions with each other as well as how all three disciplines interact together. These descriptions can help health professionals apply the presented model to their own rural settings through the development of specific goals and objectives that leverage the strength of each discipline and interaction.
Public health and gerontology
This dyad illustrates the importance of prevention and education and an understanding of the aging process to promote health, reduce health disparities, and increase health equity in rural-residing older adults. Recognition of the influence of the environment upon the older individual and population is enhanced by field-based practice. Whereas public health includes a focus on social determinants of health, gerontology recognizes the impact of social support in healthy aging.
Public health and nursing
While the public health and nursing dyad also focuses on health-related prevention and education, this partnership addresses the healthcare needs of disadvantaged and rural populations through the provision of quality care within the complex practice-based environment of an evolving healthcare system. As older adults are often shuffled between their home and healthcare facilities, education, communication, and coordination of care during these transitions are critical to supporting older adults within the community through their interactions with the healthcare system. Public health and nursing partnerships are critical in accessing and coordinating community services for older adults and identifying gaps in services in rural areas.
Gerontology and nursing
This dyad focuses on assessment, treatment, and rehabilitation for improved functioning and healthcare needs of older adults using a gerontological lens that includes the social, psychological, and environmental factors that influence the health of older people. Also, key focuses of this dyad are needs related to quality of care (ie health care and overall wellbeing) and quality of life in assisted living and skilled nursing facilities. Pairing these disciplines can also address social isolation, lack of public transportation, and even the lack of skilled nursing that may occur in many rural environments.
Interdisciplinary integration
There are clear benefits of using the dyadic approach. For public health and gerontology, community engagement is a crucial component of this dyad’s practice outcomes. Practice outcomes for public health and nursing include improving population health by emphasizing prevention and attending to multiple determinants of health. Gerontology and nursing practice outcomes utilize person-centered and strengths-based approaches for optimum health achievement12. Integrating all three of these disciplines provides rural-residing older adults with the expertise needed for person-centered and community-level health-related resource access, as shown in Figure 1. By integrating three complementary professions with different training and foci, practitioners can compound disciplinary strengths, cover weaknesses in knowledge and expertise, and provide smooth transitions for older adults through the continuum of care. This is especially critical in rural environments because personal, financial, and professional resources can often be scarce.
Interdisciplinary approaches provide more comprehensive health support for rural older adults than any one discipline in isolation. Reducing health disparities and increasing health equity for this population are strengthened through interdisciplinary knowledge and practice. Protecting and enhancing the health of populations through person-centered care are reinforced through knowledge exchange among nursing, gerontological, and public health practitioners.
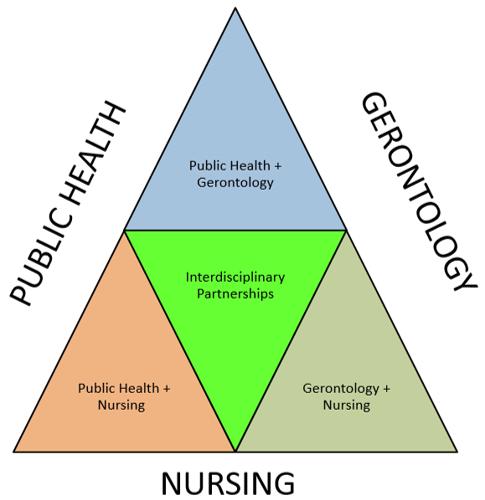 Figure 1: Partner integration conceptual model.
Figure 1: Partner integration conceptual model.
Steps for developing an interdisciplinary partnership
According to O’Sullivan, the development of interdisciplinary partnerships is a step-by-step process. Initially, community partners should be recruited and a needs assessment conducted. Depending upon the needs of the community, disciplines to be included in the integrated partnership can be determined. Disciplines would then work to move from disciplinary to cross-disciplinary to multidisciplinary to interdisciplinary approaches13.
Example of model use
There is wide recognition that individuals who live in rural environments that lack sufficient health-related resource access can experience significant health inequities14. The following example is of a project using a mixture of clinical and non-clinical disciplines to improve rural health resource access.
A community engagement framework was used to develop and evaluate the needs of rural residing older adults. Partnerships were developed with surrounding healthcare systems, community health centers, rehabilitation, extended care facilities, home health, and tele-health. To address the lack of knowledge or training in creating interdisciplinary teams, providers were educated about the importance and ways of developing interdisciplinary collaborations12. This required an investment in learning about the contribution of roles and skills by partnered disciplines, and teamwork. Education on the blending of disciplines’ philosophies, jargon, and techniques takes time, so advanced planning and full team engagement is essential for long-term success12.
Summary
Allocating shared resources, roles, responsibilities, and expenses provides more economic and capacity efficiency. This process of sharing is more crucial at a time when entities experience limitations in sustainable resources, especially in rural areas. The application of interdisciplinary teams enables practitioners to address the complex issues experienced in rural-residing communities.





