Introduction
Health condition self-assessment can be considered a good morbidity and mortality predictor because it reflects the biological, psychological and social aspects of the individual1,2. This indicator has been used in epidemiological studies both because it is easy to be assessed in population surveys and it is considered a good proxy for certain clinical conditions and medical evaluation3,4.
Sociodemographic, environmental and health conditions can influence health self-perception5-8. It is known that there is a higher prevalence of negative health self-perception among individuals exposed to stressful environments, with reduced sleeping time and little time spent on leisure activities (ie situations generally related to urban work9,10). However, in rural areas, the identification of morbidities that affect workers’ health and their general health condition is largely unknown.
Rural areas have low schooling and income, more frequent risk factors, such as hypertension and diabetes mellitus, and poor access to health services11,12. The primary level of health care (basic health units in neighborhoods) is the gateway to the health system in rural areas of Brazil, where a small percentage of the population have private health plans (approximately 6.4%, compared to 29.7% of individuals in urban areas), although there are differences between the regions of Brazil13. In Pelotas, the rural area in the present study, approximately 44% of the inhabitants who had consulted in the past year had used the public health system. Pelotas has inhabitants of mostly German and Pomeranian descent14. This corroborates with the data presented in the research entitled ‘National Survey by Household Samples’15, which shows that in 2015 approximately 77% of individuals living in southern Brazil had white skin color.
The modernization and development of rural areas caused by demographic and epidemiological transition has had an impact on the lifestyle and behavior of individuals16. A consequent increase in smoking, physical inactivity, consumption of alcoholic drinks and the ingestion of unhealthy foods has contributed to a heavier burden of chronic non-communicable conditions, including cardiovascular diseases, diabetes, some types of cancer and respiratory problems17. This is also observed in rural areas18,19. However, the role of rural work on these areas is still not clear.
Considering the need to better explore the impact of rural work and health outcomes in rural areas, this study aims to evaluate the relationship between health self-perception and the occurrence of morbidities according to the type of work in southern Brazil.
Methods
This study is part of a cross-sectional, population-based study applied to individuals aged 18 years or older residing in the rural area of the southern municipality of Pelotas, Brazil, entitled ‘Evaluation of the Health of Adults Living in the Rural Area of the City of Pelotas, State of Rio Grande do Sul, Brazil’, which investigated several health aspects of this population. Pelotas is a medium-sized municipality located in the southern Rio Grande do Sul state, having a population of roughly 340 000 inhabitants, 7% of whom (22 000 inhabitants) live in the rural area, which is subdivided into eight districts and 50 census tracts, according to the last census performed by IBGE – the Brazilian Institute of Geography and Statistics13. Multiple-stage sampling was performed. Of the 50 tracts belonging to the rural area of Pelotas, 24 census tracts were drawn based on the number of permanent households in each district13. Within each tract, with satellite images, the household centers, defined as a cluster of at least five houses located within a radius of 1 km from the center, were identified. The researchers started selecting the households from the center with the largest number of households and, if they were not able to reach the number of households needed in that center, they moved to the second-largest center and so on until they reached the number of 30 households in each tract (total of 720 households), ensuring the representativeness of the sample. More details can be obtained in the study by Gonçalves et al (2018)20. Of the total 1697 individuals considered eligible, 1519 constituted the initial study sample (response rate of 89.5%).
The health self-perception information was measured by the question ‘What do you think of your health condition?’ and was classified as good (very good or good) or not good (fair, poor or very poor). Rural work was measured by the question ‘Do you do any kind of rural work, such as that related to planting, animal husbandry, fishing, or others?’, which was categorized as yes or no, and considered as an independent variable.
To assess the impact of the type of work performed on health, the following morbidities were considered: obesity, depressive symptoms, hypertension, diabetes mellitus, high cholesterol, heart failure or angina, respiratory diseases (asthma or bronchitis) and rheumatic diseases (arthritis, rheumatism or arthrosis). The nutritional status was measured by the body mass index (BMI) calculated on weight measurements in kilograms by square height in meters (kg/m²); those with BMI ≥30 kg/m² were considered obese21. The depressive symptomatology was evaluated by the Edinburgh Postnatal Depression Scale22 validated for the general adult population by Matijasevich et al (2014)23, using an eight or higher cut-off point. The other morbidities were self-referenced by the question ‘Did any doctors or health professionals ever say that you had ...?’ and categorized as yes or no. Finally, the following variables were considered as confounding association factors: age (in full years, categorized as 18–29, 30–39, 40–49, 50–59, or 60 or more); skin color (white, black, brown-skinned or other) and schooling (in full years of study, categorized as 0– 4, 5–8, or 9 or more).
Statistical analyses were carried out by Stata v14.1 software (StataCorp; http://www.stata.com) using its svy command to consider the effect of cluster sampling. Crude and adjusted Poisson regression analyses were performed between health self-perception and independent variables, as well as self-reported morbidities according to the type of work, thus obtaining prevalence ratio (PR) estimates and the respective confidence intervals (95%CI). All analyzes were stratified by sex, and those with p<0.05 were considered to be associated with the outcome.
Ethics approval
The research project was approved by the Research Ethics Committee of the School of Medicine of the Federal University of Pelotas (Process 1.363.979). All participants gave their permission to be part of this study and signed the informed consent to participate. Broadly, the informed consent document communicated the purpose, procedures, risks, and benefits of the study, the subject’s rights in participating in research, and the freedom to decline to participate without any jeopardy. The consent forms were signed in two copies. One was retained by the researcher and the other by the participants.
Results
Out of 1519 individuals constituting the initial study sample, 893 of them who reported being at work at the time of the interview or were working retirees were included in the study. Most respondents were men (59.4%), had white skin color (86.6%), with 5–8 years of schooling (40.1%), and age was 43.6 years (SD±0.52). In addition, 56.9% reported doing any type of rural work, with agriculture being the most reported type (78.5%). The not good health self-perception prevalence was 27.6%, with a significant difference between the sexes (24.2% of men v 32.5% of women, p=0.014) (Table 1).
Table 2 shows the relationship between the type of work performed, not good health self-perception and referred morbidities, stratified by sex. In the crude analysis, individuals who reported performing rural work presented a higher risk of not good health self-perception, which included both men (PR: 1.43, 95%CI: 1.06–1.92) and women (PR: 1.38, 95%CI: 1.09–1.75). When adjusted for age, skin color and schooling, the effect measure decreased and the confidence interval encompassed the unit. The risk of developing obesity (PR: 0.65, 95%CI: 0.47–0.91) and cardiovascular diseases (PR: 0.32, 95%CI: 0.12–0.87) was lower in men who reported doing rural activities. After the adjustment, women who reported doing rural work presented a lower risk for respiratory diseases compared to those who did not perform such activities (PR: 0.47, 95%CI: 0.22–0.97). For the other comorbidities, in general, rural workers presented a slightly lower prevalence than non-rural workers (except depressive symptoms and diabetes mellitus). However, no significant associations were found in males and females in the crude and adjusted analyses.
Table 1: Description of sample according to sociodemographic and health variables among residents in rural area of Pelotas, Brazil (n=893)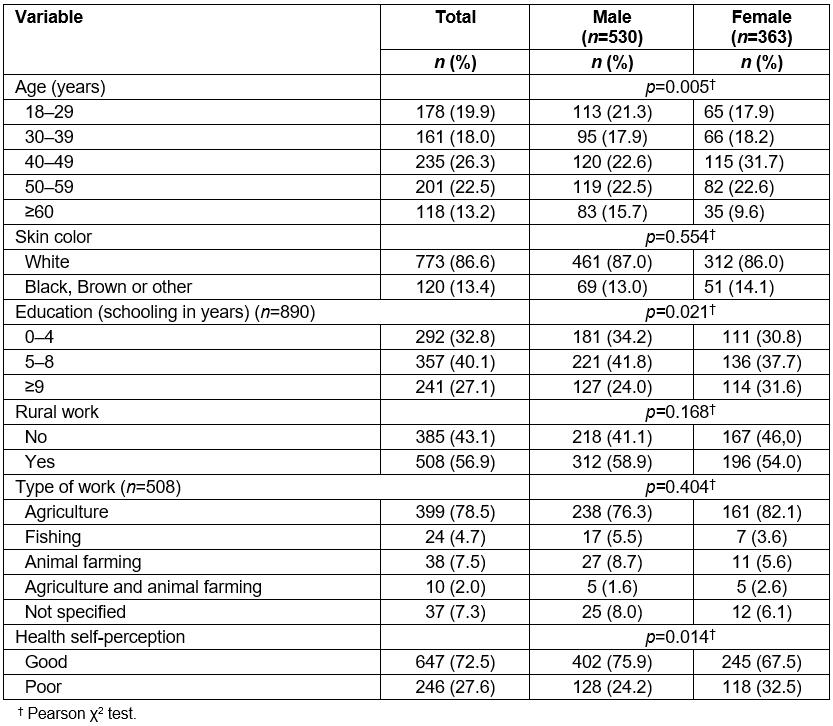
Table 2: Health self-perception and referred morbidity according to occupation type among residents in rural area of Pelotas, Brazil (n=893)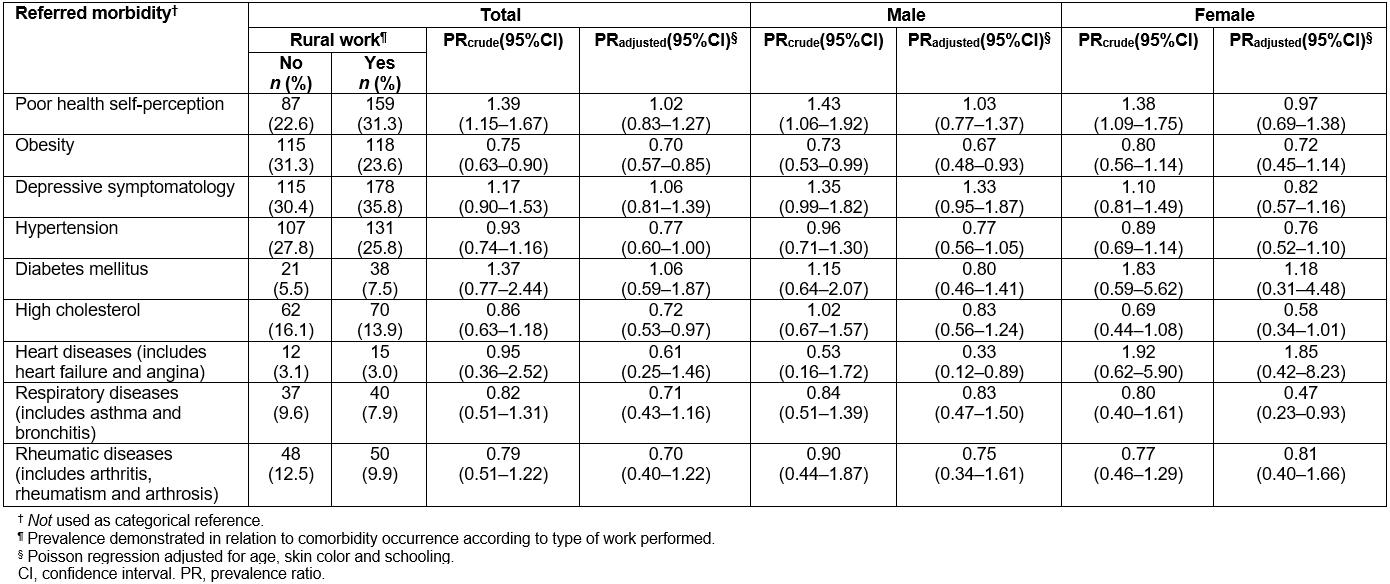
Discussion
In this study, the authors observed a high prevalence of not good health self-perception in a rural population from the south of Brazil. Rural work was associated with not good health self-perception in the crude analyses, but not in the adjusted analyses. Regarding health-specific outcomes, there was a negative association between rural work and the occurrence of some morbidities evaluated in this study (obesity, cardiovascular disease and respiratory disease), with an important distinction between the sexes.
The prevalence of not good health self-perception in this study was similar to that observed in Brazil as a whole24. A study carried out among individuals who performed rural activities (agricultural and livestock production, fishing, hunting or extraction activities, and agricultural or plant mechanical work – a definition also used by the present study) observed that this problem was reported by 34.7% of the workers24.
Despite the knowledge of different characteristics between rural and urban areas11,25, little is known about the role of the types of work performed and their impact on health self-perception. Some studies show a higher prevalence of negative self-perception in health among individuals exposed to environments with markedly urban characteristics9,10. However, individuals who work in rural areas often have a heavy workload and perform exhausting agriculture-related manual labor, such as planting, harvesting, pruning, loading and transporting, and are exposed daily to environmental factors, such as high temperatures, that may lead to greater physical and emotional exhaustion26 and may thus influence the health self-perception of these populations. A study carried out in 2015 and based on data from the National Household Sample Survey revealed that rural workers with an agricultural occupation were less likely to report their health as good. In the present study, although there was a higher not good health self-perception risk in crude analyses, after adjusting for potential confounders the magnitude of the effect decreased and the association lost its statistical significance, thus suggesting a greater impact of socioeconomic and demographic characteristics on rural areas and the choice of type of work performed. According to the final report of the National Commission on Social Determinants of Health, a higher schooling level influences the use of health services, access to treatments, the understanding of health and information problems, and adhesion to healthier lifestyles27. In the present study, the included sample presented higher prevalence of not good health self-perception among individuals with low levels of education (data not shown), a point that could have contributed to the observed results24,27. Therefore, although the prevalence of not good health self-perception is higher in rural workers, it may not be related with the occupation per se, but by the socioeconomic and demographic context.
In general, rural activities were negatively associated with some morbidities, corroborating the findings reported by previous studies28-30. The authors observed that, among men who performed rural work, obesity and cardiovascular disease were negatively associated in both crude and adjusted analyses. It is known that physical activity has a protective role for numerous morbidities31, and it is also known that men living in rural areas report greater physical activity at work32.Thus, it is possible to assume that the rural work reported in this study has a protective role against obesity and cardiovascular diseases. However, it cannot be said that the general health condition of these individuals is good, because not good health self-perception was more frequently reported among rural workers. Thus, the results should be interpreted with caution. Moreover, the findings may result from a reverse causality inherent in cross-sectional studies. It is plausible to think that obese individuals and/or those with heart disease can perform other activities besides rural ones or may have changed the type of occupation after the commencement of these morbidities because rural activities demand a lot of physical effort.
In this study, a negative association between rural work and respiratory diseases among women was observed. These results are not in agreement with those reported in the literature, which demonstrates a positive relationship between pulmonary diseases and rural work30. In rural areas, agricultural activity is associated with several risks, such as exposure to chemicals, and physical risks (pesticides, organic and inorganic dust, noise and sun exposure), which can cause respiratory disorders33. The role of sex in differential rural work has already been reported. Thus, further studies with a deep assessment of the rural work exerted by women are needed to better understand the association observed here.
It is of note that a positive association between rural work, arthritis or rheumatism, and arterial hypertension was already observed in rural workers in Brazil24. However, no such associations were observed in the present study. In part, such differences can be attributed to the particularities observed in the rural area of Pelotas when compared to the country as a whole. When compared to other rural regions, differences regarding the prevalence of general and abdominal obesity34, average score in the Mini Sleep Questionnaire scale of sleep problems35 as well as the ability to reach adequate scores in the Diet Quality Index36 were already observed.
As a limitation, the study may not have had the ability to detect associations with other evaluated morbidities. Also, the non-assessment of labor specificities and the use of personal protective equipment should be considered. The workload and level of exposure to contaminants have not been examined in detail either. Another limitation may be the limited extrapolation of this study’s results to other Brazilian rural areas, given the great heterogeneity among the Brazilian rural areas regarding demographic and morbidity data13. However, although the rural population is composed of German and Pomeranian descendants, the population in the present study is similar to the other regions with respect to less formal education, less access to health services and higher poverty when compared to urban areas. Therefore, the results may be extrapolated to the target population and can provide an initial picture of self-perceived health, morbidities and their relationship with rural work. Further studies in other regions are important to confirm these findings.
Finally, this study was based on self-reporting for health problems, which can incur an information problem. Although the clinical information would have provided more precise information about morbidities, the logistics and costs were an impediment to such a study. Considering the standardized questionnaire and the quality control used in the study, the information problem is non-differential, and thus an information bias is very unlikely. Moreover, the anthropometric measurements and the use of validated questionnaires such as the Edinburgh Postnatal Depression Scale can be considered strengths of this study.
The inclusion of this information could benefit explanations on the study and help understand associations. However, a positive point is that the comparison group also resides in the rural area, ensuring that the associations found are related to rural work. Also, it is important to highlight that this is a population-based study, which evaluated aspects related to the health of a poorly investigated population.
Conclusion
In this study, approximately one-third of the rural population considered their health as not good. The prevalence was higher among rural workers. However, the association between rural work and not good health self-perception seems to be highly dependent on sociodemographic context. These results contrast with the findings considering specific outcomes. A lower prevalence of obesity, cardiovascular disease and respiratory disease was observed among workers, even after adjustment for socioeconomic variables, with an important distinction between the sexes.
The identification of morbidities that affect the health of rural workers and their general health condition evaluated through health self-perception emphasize the importance of improved knowledge on the health condition of these populations. These findings may allow the identification of health determinants expressed in the rural environment and can subsidize the planning of actions directed to health, especially those with specific gender orientation.
References
You might also be interested in:
2018 - Rural medicine ‘cooking up’ longitudinal integrated clerkships


