Introduction
Australia faces a critical shortage of medical practitioners in regional, rural and remote communities1. Despite an increase in the number of undergraduate training positions, the proportion of medical graduates pursuing a career in rural practice has diminished2.
Medical education in Australia is undertaken in four phases: undergraduate, prevocational (intern and resident), vocational training (registrar) and continuing professional development3. The Medical Board of Australia requires all medical graduates to undertake an internship, a year of supervised general clinical experience, prior to awarding general registration as a medical practitioner4.
The Queensland Rural Generalist Pathway (QRGP) was established in 2007 to reinvigorate rural practice in Queensland5,6. The recent Collingrove Agreement defines a rural generalist as ‘a medical practitioner who is trained to meet the specific current and future healthcare needs of Australian rural and remote communities, in a sustainable and cost-effective way by providing both comprehensive general practice and emergency care and required components of other medical specialist care in hospital and/or community settings as part of a rural healthcare team.’7 Rural generalists can train with either the Australian College of Rural and Remote Medicine (ACRRM) or the Royal Australian College of General Practitioners (RACGP), the latter also requiring completion of the Fellowship of Advanced Rural General Practice (FARGP)8,9. Both colleges require rural generalist trainees to undertake a year of general prevocational training (postgraduate year 2), a year of Advanced Skills Training (AST – ACRRM) / Advanced Rural Skills Training (ARST – RACGP) and 2 years of vocational training as a rural GP registrar in addition to internship. While placements in emergency medicine, medicine and surgery are mandated for all interns by the Medical Board of Australia, both colleges require additional prevocational placements: anaesthetics (ACRRM), obstetrics and gynaecology (ACRRM) and paediatrics (ACRRM and RACGP)8,9.
QRGP trainees are predominantly placed at regional referral hospitals that provide general prevocational training in a regional/rural context. Regional hospitals deliver Clinical Service Capability Framework level 4/5 clinical services (moderate to high complexity inpatient and ambulatory care) provided by specialist medical practitioners supported by trainee registrars and resident medical officers10. QRGP trainees are offered prevocational placements in anaesthetics, obstetrics and gynaecology, and paediatrics to ensure they are adequately prepared for rural generalist practice.
The QRGP was so successful that the then Health Minister, the Honourable Lawrence Springborg MP, directed the QRGP to double its intake from 40 in 2014 to 80 in 20165, challenging the capacity of the QRGPs training Hospital and Health Services (HHS) to provide the prevocational experience necessary for trainees to progress to vocational training in rural general practice8,9.
Extended rural clinical placements (longitudinal integrated clerkships) have shown great utility in undergraduate medical curricula, promoting rural medicine as a career endpoint and increasing training capacity while providing comparable training outcomes to placements in specialist units in larger hospitals1,11. Results from a West Australian prevocational rural general practice placement program12, the Federal Prevocational General Practice Placement Program13 and the Murray to Mountains Program14 suggest that prevocational rural placements have potential to reproduce this success.
The Prevocational Integrated Extended Rural Clinical Experience (PIERCE) was developed to increase the training capacity of the QRGP and strengthen trainee commitment to rural practice by offering an authentic, extended 15-week rural term that provided an integrated experience in anaesthetics, obstetrics and gynaecology, and paediatrics at a rural district hospital. These hospitals deliver Clinical Service Capability Framework level 3 acute health services (low to moderate complexity inpatient and ambulatory care) including medical, surgical, emergency, maternity services, low risk surgery and minor procedures provided by suitably trained rural generalists and GPs. Specialist services are provided on a visiting basis10.
PIERCE had three objectives:
- Increase prevocational training capacity within QRGP prevocational training facilities.
- Strengthen and consolidate trainee commitment to a rural outcome.
- Offer sufficient experience in anaesthetics, obstetrics and gynaecology, and paediatrics to meet Rural Generalist prevocational certification requirements8.
This translational qualitative study sought to:
- explore the experiences and perceptions of QRGP trainees who undertook a PIERCE placement in three Queensland rural district hospitals (Mareeba, Proserpine and Stanthorpe) in 2015, with a matched cohort of trainees who undertook placements in anaesthetics, obstetrics and gynaecology, and paediatrics at a regional referral hospital (Cairns, Mackay and Toowoomba base hospitals)
- evaluate whether trainees believed these placements achieved their objectives and identify elements of the placements that contributed to, or were a barrier to, their realisation
- allow generalisation of findings to other prevocational rural placements.
Methods
Evaluation framework
Given that the external validity and applicability of prevocational rural placements such as PIERCE was a focus of investigation, the study used a realist evaluation framework15 investigating What works, for whom, in what circumstances, in what respects and why? Realist evaluation is designed to evaluate complex social interventions, in which contextual factors are an important determinant of outcome in concert with the mechanisms by which an intervention is believed to work15. It analyses a program in terms of the interaction between the:
- context in which the program is implemented
- mechanisms by which the program is hypothesised to work
- outcomes achieved by the program.
Participants and sampling
Eligible QRGP trainees, allocated to either a 15-week PIERCE placement or to 5–10-week regional hospital anaesthetic, obstetrics and gynaecology, and paediatric placements at their regional referral hospital by their HHS were contacted by email and offered the opportunity to participate in the study.
Trainees were under no obligation to participate. There was no penalty for trainees who chose not to.
Semi-structured qualitative interviews, undertaken by one of the authors (PO), explored the experiences of QRGP PIERCE trainees compared with trainees undertaking regional hospital placements.
Data analysis
Interviews were transcribed, and all identifying information was removed. Transcripts were independently analysed by the principal investigator (DH) and two assistant investigators (EC and JH) using thematic analysis as described by Braun and Clarke16.
Trainees who requested an opportunity to review the outcome of the study were sent a summary of the thematic analysis and offered the option of providing feedback.
Ethics approval
The study design was assessed and approved by the Darling Downs Hospital and Health Service Ethics Committee (HREC/15/QTDD/19).
Results
Of the 10 eligible PIERCE trainees contacted, one declined the invitation to participate. The remaining nine PIERCE candidates agreed to be interviewed.
The study aimed to purposively recruit QRGP trainees undertaking regional hospital placements to match PIERCE participants rotated out of the same HHS. However, there was difficulty obtaining sufficient QRGP trainees in one HHS. To preserve the purposeful sampling of three trainees (one each from anaesthetics, obstetrics and gynaecology, and paediatrics) from each HHS, it was necessary to recruit two non-QRGP trainees. All nine trainees undertaking regional hospital placements contacted for interview agreed to participate.
Thematic analysis16 identified 53 codes and 8 themes in the transcripts (Fig1, Tables 1,2). Illustrative trainee comments are provided in Tables 2–4 to support the major themes identified in the discourse.
At the completion of coding, no new codes were required to explain the results, i.e. data saturation was achieved16.
The lead researcher (DH) is an employee of the QRGP and the designer of the PIERCE placement.
Six PIERCE trainees responded to the opportunity to review the thematic analysis and provide feedback. They were satisfied that the thematic analysis accurately represented their views.
Table 1: Codes and major themes identified in the transcripts†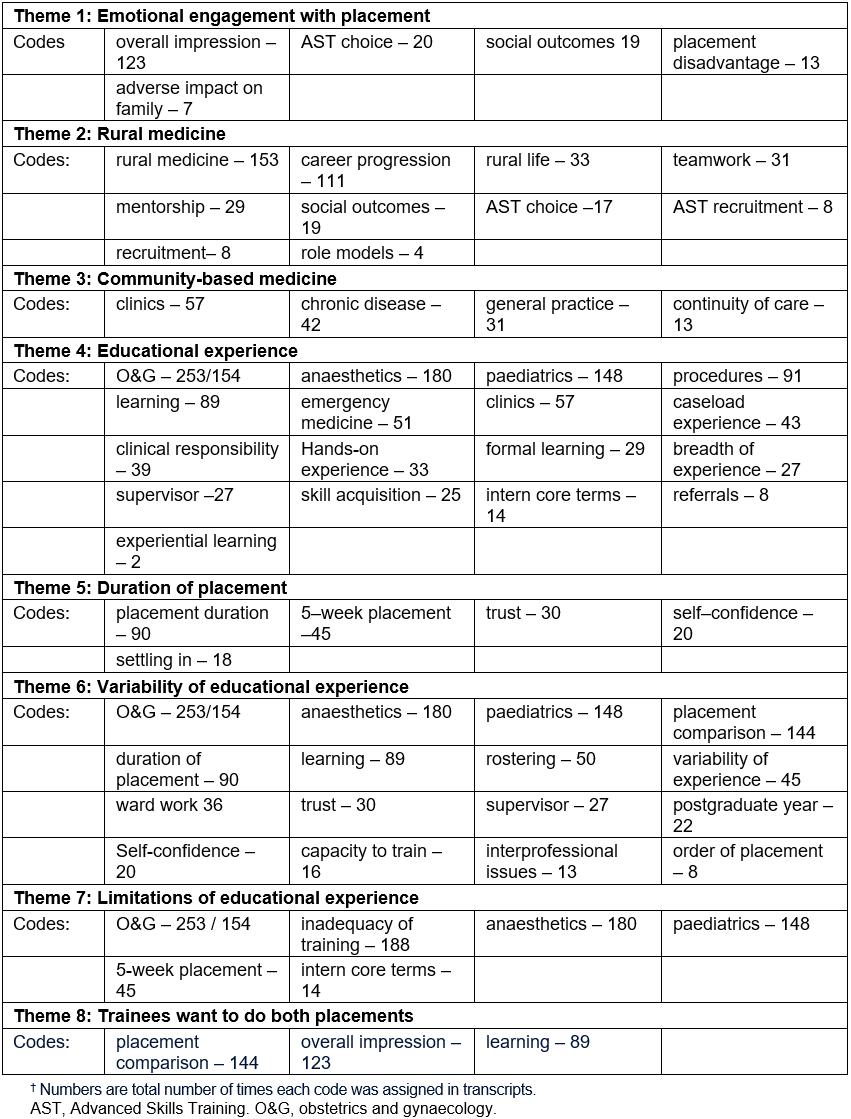
Table 2: Illustrative trainee comments on placement experiences, by theme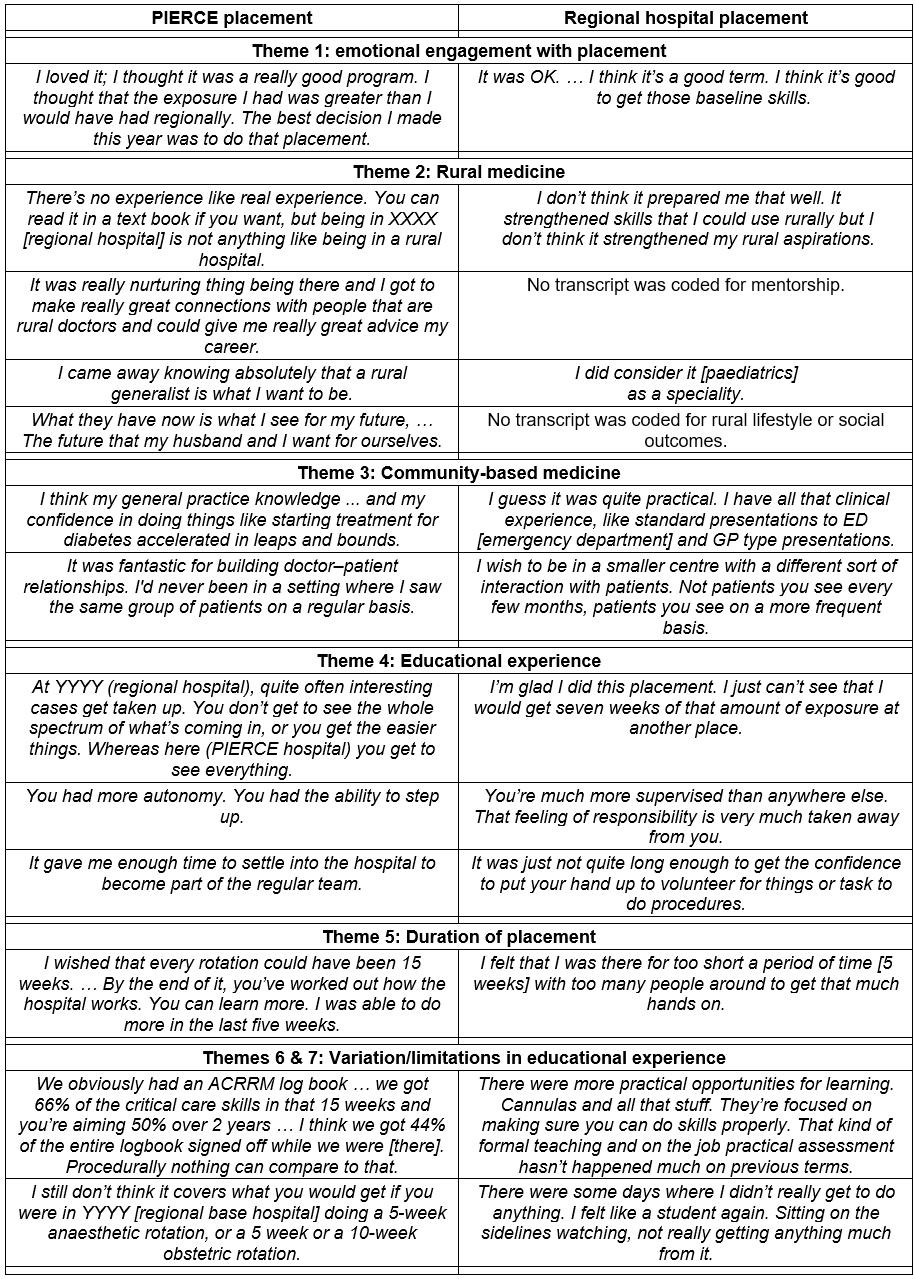
Table 3: A spectrum of learning experiences – types of learning opportunities offered by different prevocational placements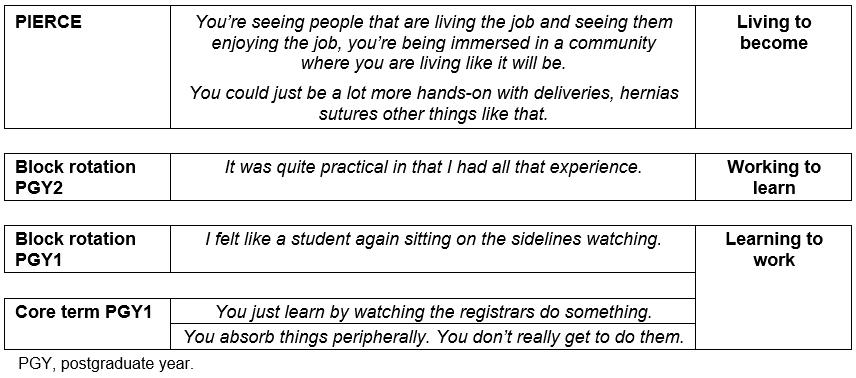
Table 4: Impressions of trainees who had undertaken both rural and regional placements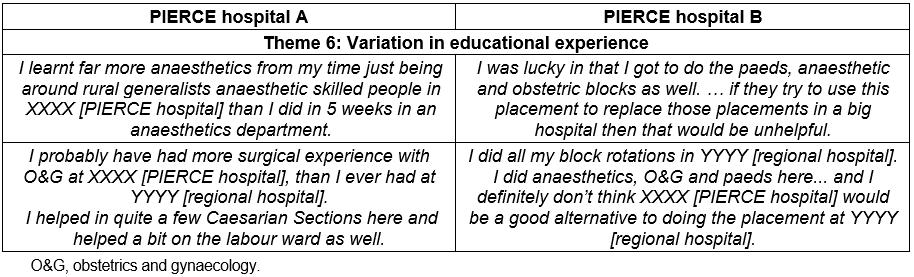
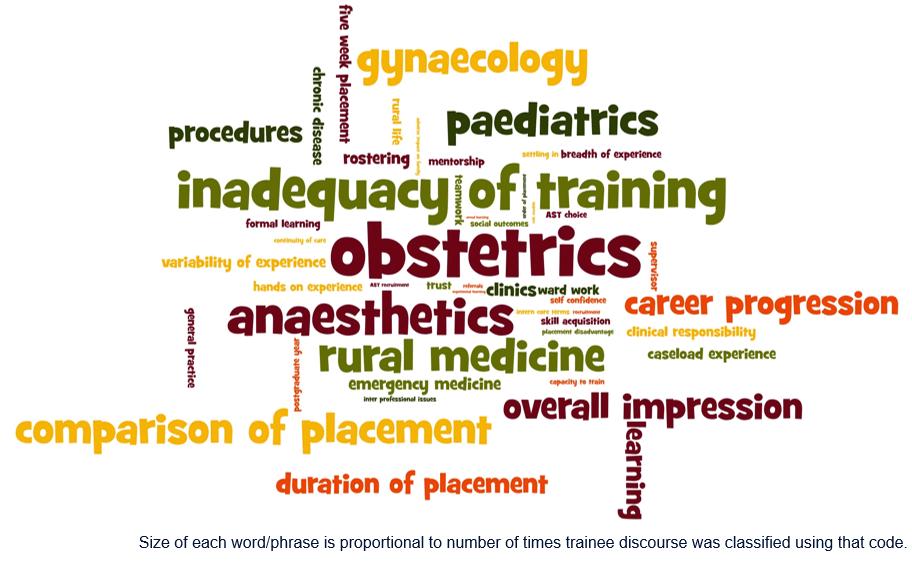 Figure 1: A word salad of transcript codes.
Figure 1: A word salad of transcript codes.
Discussion
1. Increase prevocational training capacity within the QRGP
PIERCE aimed to increase training capacity within the QRGP, as regional hospital anaesthetic, obstetrics and gynaecology, and paediatric placements were a bottleneck for the expansion of the QRGP. The QRGP succeeded in achieving its objective of creating more than 80 intern training positions in 2016, ultimately recruiting 77 interns into the pathway in 2016 compared with 50 in 2015. Ten of the extra positions were created by PIERCE participating facilities, a 45% increase from a high baseline of 22 positions in 2015 to 32 in 2016.
2. Strengthen and consolidate trainee commitment to a rural outcome
PIERCE trainees enjoyed the opportunity to experience rural medicine and the rural lifestyle, experience continuity of care in a community setting and develop mentor relationships with senior colleagues. The placement affirmed trainees’ commitment to rural practice. In contrast, regional hospital placements confused or undermined some trainees’ commitment to rural medicine.
PIERCE trainees strongly identified with their supervisors and the rural lifestyle, highlighting the importance of professional identity formation in junior doctor medical education17. Barnett18 observed that the ideology of academic competence (knowledge) has been quickly replaced by the ideology of operational competence (skills). However, he argues that both are limiting ideologies. Higher education should seek to create individuals whose contribution to society is not purely defined by what they know or what they do. Who are we trying to develop, ‘human beings or human doings?’19. In keeping with the growing emphasis on professional identity formation Cruess et al20 suggest there may be a fifth level to Miller’s pyramid: ‘Is’ (Fig2).
Given the social and political imperative to channel more medical graduates into rural medicine1,21,22, this study adds weight to the growing consensus that rural community-based placements such as PIERCE enhance trainee interest in and commitment to rural practice, making them strategic components of prevocational training1,12-14.
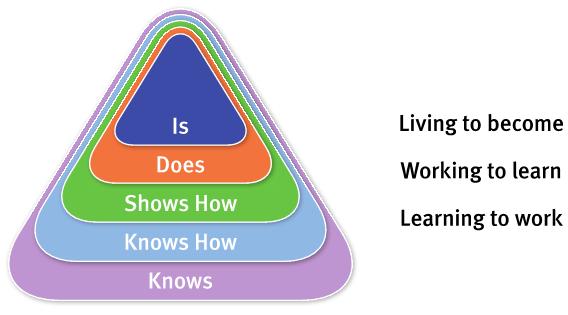 Figure 2: Modified Miller’s pyramid20, including a fifth level: ‘Is’.
Figure 2: Modified Miller’s pyramid20, including a fifth level: ‘Is’.
3. Offer sufficient experience in anaesthetics, obstetrics and gynaecology, and paediatrics to meet rural generalist prevocational certification requirements
PIERCE provided a valued rural training experience that offered a broad caseload, continuity of care and hands-on rural clinical experience in which trainees had more responsibility backed up by highly engaged and supportive generalist supervisors (Fig3), adding weight to the growing evidence that rural prevocational placements offer valuable learning opportunities that are well aligned with the Australian Curriculum Framework for Junior Doctors (ACFJD)23, the ACRRM Core Clinical Training curriculum8 and the RACGP/FARGP curriculum9.
Participants described a spectrum of learning experiences (Table 3). PIERCE trainees emphasised increasing engagement with their senior colleagues’ work as rural clinicians (living to become). Situated Learning24 emphasises that knowledge is constructed within the activity, context and culture in which it is learned. Novices learn by progressively engaging in the work of a community of practice. In contrast, regional hospital trainees emphasised the acquisition of skill and knowledge (working to learn) rather than contributing to the work of the clinical unit. Finally, in some regional hospital placements (especially in postgraduate year 1), trainees’ learning experiences were even more passive, essentially doing clerical work while observing senior colleagues who retained responsibility for decision-making (learning to work).
PIERCE trainees identified a number of learning mechanisms that impacted on the effectiveness of rural placements (Fig3):
- continuity of care and supervision
- quality of participation
- learning environment
- equity in learning and assessment.
These findings mirror those of a systematic realist review of undergraduate rural placements by Thistlethwaite et al11.
Context had a profound effect on the trainee learning experience in both PIERCE and regional hospital placements. Placements varied markedly from HHS to HHS, hospital to hospital, placement to placement, season to season, term to term, supervisor to supervisor and trainee to trainee. Important aspects of the learning context focused learning on the desired outcome: rural and remote medical practice (Fig4):
- supportive social and administrative environments25
- communities of practice24,26
- role models26
- identity formation17,20.
Some trainees observed that regional hospital placements challenged their commitment to rural medicine. When the training experience is misaligned with curriculum objectives the focus of some supervisors and trainees shifts away from the desired outcome (Fig3). Hafferty and Franks27 observed that much of what is taught, and most of what is learned, is acquired informally via everyday interactions within the day-to-day business of medicine – the hidden curriculum. However, they argue the issue is not one of ridding the environment of contaminating values or elements but rather recognising their presence and working with them (p. 865)27. An effective curriculum aligns all the critical elements of success – learning objectives, learning mechanisms, learning context and assessment – so that they are mutually reinforcing.
Assessing the ability of PIERCE or the regional hospital anaesthetic, obstetrics and gynaecology, and paediatric placements to meet ACRRM and QRGP prevocational training requirements was more problematic. Neither the ACRRM core curriculum8 nor QRGP articulate specific learning objectives for these placements beyond the satisfactory completion of a clinical placement in these domains of practice. While a 10-week placement is the gold standard, 5-week placements are acceptable provided trainees attend an accredited course and submit a log of 50 cases in the relevant domain of practice prior to fellowship8. Lacking any formal learning objectives, trainees viewed the utility of placements through the lens of clinical and procedural exposure rather than the more generic knowledge, clinical skills, diagnostic reasoning, communication and management skills emphasised by the ACFJD23 and the ACRRM8 and RACGP9 curricula. Social expectations (the hidden curriculum) distorted trainees’ focus on the curriculum objectives (Fig3).
The untested gold standard for the anaesthetic, obstetrics and gynaecology, and paediatric placements is satisfactory completion of a 10-week placement in a specialist hospital. In this study, neither PIERCE nor the regional hospital placements reliably met trainee aspirations. Given the high variability in the perceived clinical exposure and educational merit of clinical placements described in both arms of this study, time-based definitions of the attainment of educational objectives were unreliable.
The duration of a clinical placement is better thought of as an educational resource, rather than a measure of learning outcome. Trainees preferred longer placements, believing it took about 5 weeks to settle into the placement, understand the job, supervisor expectations and develop sufficient self and supervisor confidence to meaningfully contribute to the work of the unit. After this critical orientation period, learning grew exponentially and the net benefit of trainees’ contribution to the clinical output of the unit outweighed the cost of supervision. Accordingly, trainees did not believe short 5-week placements at regional hospitals were desirable.
A weakness of this study is that the findings are based purely on trainee perception The actual experience trainees obtained in the two arms of the study was not documented.
While none of the PIERCE trainees thought PIERCE was an acceptable substitute for regional hospital placements, a number of proactive trainees recounted impressive clinical exposure during their PIERCE term. One trainee completed 44% of their ACRRM logbook and 66% of its urgent care component, exceeding ACRRM and QRGP prevocational procedural standards that must be achieved by the end of postgraduate year 28, during their 15-week placement. Two trainees obtained nine and ten vaginal deliveries respectively and assisted at several caesarean sections. Even these trainees believed they should also undertake a regional hospital placement. This apparent incongruity is heightened by the observation that trainees from one HHS who had undertaken a rural hospital placement in addition to a regional hospital placement felt the rural hospital provided superior experience. However, trainees from another HHS felt regional hospital placements provided superior experience (Table 4). All trainees who undertook PIERCE instead of a regional hospital placement highlighted the inadequacies of PIERCE. As in undergraduate rural placements, equity of access to optimum training is very important to QRGP prevocational trainees11. Tversky and Kahneman28 identified the phenomenon of loss aversion in which respondents’ perception of an experience is affected by whether they believe they are losing something or gaining something. This framing effect29 has important implications. Offering prevocational rural experiences as an extra clinical experience may enhance their perceived success, providing momentum to the change process required to implement rural placements in an educational system in which the prevailing expectation is that medical education is best delivered in urban teaching hospitals.
This is a small study, which limits the ability to extrapolate findings. However, given that no new codes were required to explain the trainee discourse by the end of coding all transcripts, there can be some confidence that the key elements of QRGP trainee opinion about PIERCE have been identified16. These themes mirror those of prior research into undergraduate rural placements, adding weight to the evidence30 that they are important to the success of rural clinical placements, whether undergraduate or prevocational. This was the purpose of the PIERCE pilot study.
While there is merit in considering the relative frequency of codes to fully understand the discourse of this cohort of PIERCE trainees (Fig1, Table 1), the small sample size means that caution should be exercised when interpreting the relative importance of the codes and themes more generally. Drawing such inferences would require quantitative research of a larger sample of QRGP trainees undertaking PIERCE placements over a longer period of time.
Context had a profound effect on learning outcomes. ‘Set and forget’ definitions of the required educational experience based on a placement type and duration may not reliably deliver the desired outcomes. Further research into how context interacts with educational mechanisms to produce the desired outcomes is warranted to ensure the effective design, implementation and assessment of prevocational rural placements. Such a research program would include further qualitative analysis of prevocational trainee experience, quantitative observational and experimental studies to more fully elucidate the different causal elements, their relative importance and how they interact with each other to produce educational outcomes. The consistency of educational mechanisms (continuity of care and supervision, quality of participation, learning environment and equity of educational experience) and contextual determinants (supportive social and administrative environments, communities of practice, role models and identity formation) observed in this study and previous undergraduate studies indicates these factors are particularly worthy of further investigation. Given that the interaction between causal factors may also be a critical determinant of outcomes, research methodologies that study the relationship between causal factors may be illustrative. Network analysis has developed the descriptive, quantitative and stochastic tools that would enable this type of empirical analysis31-33.
Wearne et al34 observed that significant changes in hospital practice have altered the educational experience of junior doctors21. Junior doctors have less clinical exposure and less responsibility. Continuity of care has been undermined by shorter admissions and delegation of ongoing care to general practice. Junior doctors provide episodic care and as a result have less opportunity to observe and manage the natural progression of illness. Shift work has fragmented the clinical team. Trainees and supervisors no longer work together consistently in the daily business of clinical care, undermining the natural monitoring and management of trainee progress.
Even within the QRGP, the welcome increase in rural trainees has placed increasing pressure on prevocational training. In both arms of this study there were capacity issues that impacted on the availability of training opportunities. These issues were compounded by competition with medical students, registrars and student midwives for learning opportunities and by industrial policy (working hours, on-call arrangements and fatigue). Assumptions about what could be achieved in an anaesthetic, obstetrics and gynaecology, or paediatric placement 10 years ago may no longer apply today.
Distinct learning opportunities described by PIERCE trainees – broad caseload, continuity of care and an authentic role as a valued member of the clinical team, reinforced by closer and more consistent clinical and educational interactions with supervisors – address key weaknesses identified in current hospital-based prevocational training21,34,35.
The need to justify a new type of placement prompted an academic and administrative discourse that sought to compare the performance of rural placements with block rotations in acute referral hospitals. Rural placements were proposed as a way to increase training capacity by substituting rural placements for regional hospital block placements. QRGP trainees rejected this premise. In their view, neither were sufficient. Trainees believed PIERCE and regional hospital placements offered complementary experiences, both necessary for their professional development. PIERCE offered hands-on rural clinical experience in which trainees had more autonomy and responsibility. Proactive trainees benefited most from PIERCE. Regional hospital placements offered more concentrated traditional learning experiences based on observation and the handing down of knowledge and skills by hospital-based supervisors. Learning was less dependent on trainee commitment to seek out learning opportunities.
Rather than arguing for one type of placement at the expense of another, trainees remind us that it is better to capitalise on the complementary learning opportunities that different learning contexts provide.
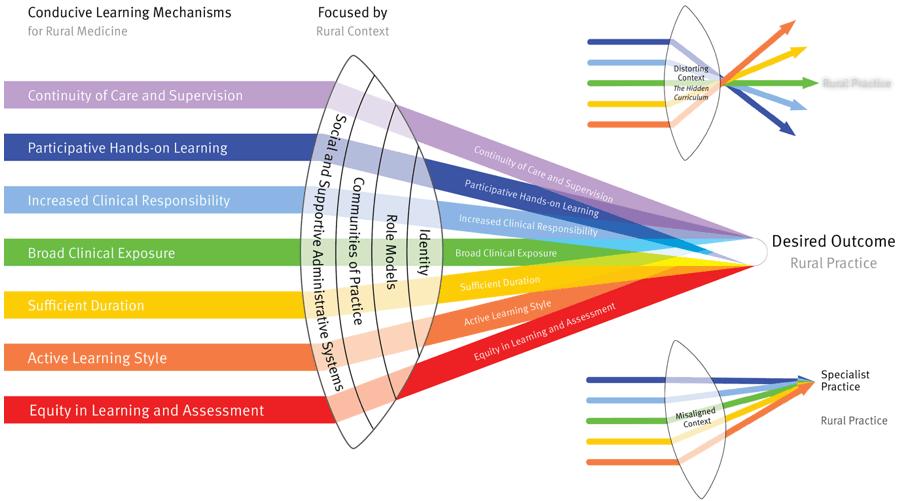 Figure 3: Learning mechanisms and contextual factors contributing to PIERCE.
Figure 3: Learning mechanisms and contextual factors contributing to PIERCE.
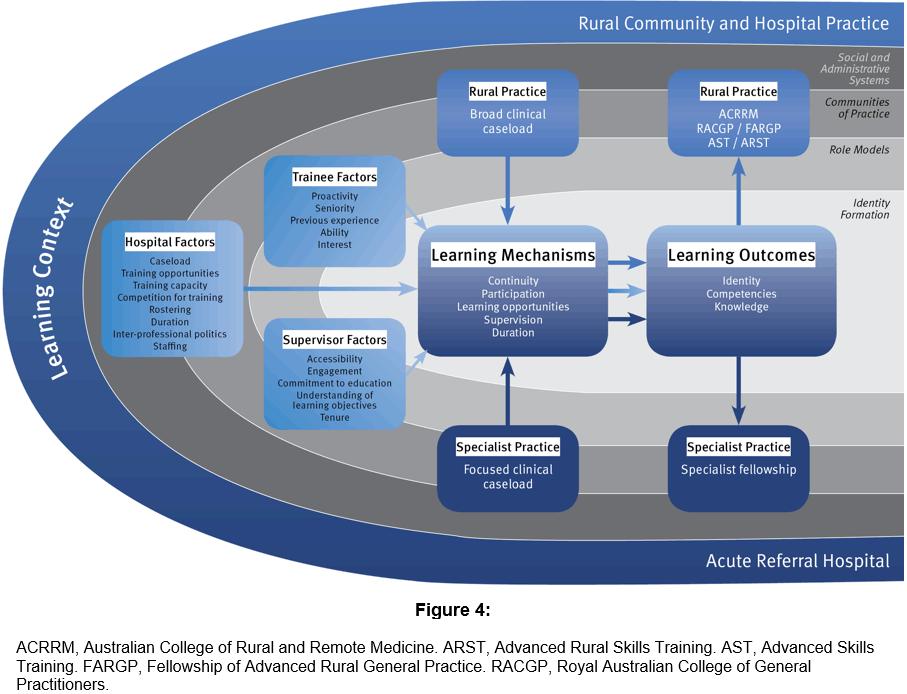 Figure 4: Contextual determinants of the effectiveness of prevocational placements.
Figure 4: Contextual determinants of the effectiveness of prevocational placements.
Conclusion
This study offers insights into the experience of QRGP trainees undertaking prevocational training in preparation for vocational training in rural medicine.
PIERCE provided an enjoyable and valued rural training experience that delivered broad caseload, continuity of care and hands-on rural clinical experience in which trainees had more responsibility, backed up by engaged and supportive generalist supervisors. Just as importantly, the placement promoted trainee engagement with, and contribution to, a rural community of practice, reinforcing their commitment to a career in rural medicine, a critical outcome for the medical workforce needs of rural Australians.
The evidence regarding PIERCE’s utility for training in anaesthetics, obstetrics and gynaecology, and paediatrics was subjective and contradictory. A number of trainees described outstanding clinical experience during their PIERCE placement. Trainees from one HHS who had undertaken both placements believed the anaesthetics and obstetrics and gynaecology experience provided by the rural placement was superior to that of the regional hospital. However, trainees from another HHS believed the regional hospital provided superior experience. All trainees who had only undertaken PIERCE expressed concern about missing out on learning opportunities they believed were available in the regional hospitals. However, it is equally clear that the regional hospital placements, especially the 5-week placements, did not reliably meet trainee expectations either.
Both the PIERCE and regional hospital placements provided opportunities and threats to the attainment of the curriculum objectives of ACFJD and the ACRRM and RACGP/FARGP curricula. Successful achievement of prevocational curriculum objectives is contingent on strategic alignment of the curriculum with supportive learning mechanisms focused by the learning context on the desired outcome – well trained medical practitioners with a commitment to rural medicine.
An astute prevocational training program will optimise the learning experience of QRGP trainees though a suite of placements that as a whole exploit the contextual advantages of different learning environments to meet prevocational learning objectives.
References
You might also be interested in:
2012 - Developing dietetic positions in rural areas: what are the key lessons?