Introduction
Research capacity building has been reported as a desired goal of rural health organisations1 as it has the potential to create locally driven research evidence that is relevant to the development of policy or able to influence client care. Research in rural areas presents its own set of challenges, and a need for specific rural training has been identified2. Several programs have been undertaken within the Australian rural health context to improve research capacity3-10.
While these programs broadly consider the context in which research activities occur, there is no research available within the published literature that explores or demonstrates the role of research within the structure of a rural health organisation. Understanding the place of research within an organisational structure is important in the support and growth of research activity, because a lack of structural organisational support for research is likely to be reflected in the culture of the organisation. Structural support for research may be seen in ways such as the inclusion of research in the position descriptions of staff, business plans or other documents where there is a clear indicator of research capacity building, which can be measured and performance can be reviewed annually11,12. Clearly positioning research within a job description is attaching individual responsibility for research. Organisational ownership of research may be evidenced in other ways, through celebration of research in newsletters or inclusion of research in annual reports12.
Health services are state funded within Australia and, at a state level across New South Wales (NSW), there has been an emphasis on research in rural areas13, with a need for ‘structures and processes … to maximize communication, productive collaboration and knowledge transfer across all aspects of health and medical research’14. These structures may be physical structures such as research units or specialist teams14. However, a critical realist perspective acknowledges that structures may be less tangible and may include societal constructs such as organisational norms or workplace cultures15. In many ways a research culture is harder to evidence; however, an active research culture within an organisation may be seen in the way an organisation acknowledges and celebrates research12.
This article outlines the findings of a research study conducted in 2016 in rural NSW, Australia, which explored the place of research within an Australian rural health organisation or local health district (LHD), as defined by references to research within the organisation’s strategic, operational and other documents. The LHD in which this study was conducted is a single coordinated public health organisation that services a rural and outer regional portion of the state and is responsible for the provision of publicly funded health services. The LHD contains a mix of small health facilities, known as multi-purpose services, and small hospitals, with few large hospitals. The LHD provides clinical services and is able to determine its own service priorities in association with the NSW Government, with which the LHD has a service agreement.
The region has links to up to six universities, although these relationships were primarily viewed as a mechanism for teaching and training in a reciprocal arrangement with universities and the organisation collaborating for clinical education placements. While the organisation can set its own priorities in regard to research, the LHD was aware that it was not particularly active in research.
Study goals and objectives
This study sought to answer the following research questions:
- Is research identified within the strategic documents of the organisation? If so, at what level of the organisation is responsibility for research attributed?
- Is research identified within the position descriptions of staff? If so, at what level of the organisation are staff expected to conduct research? At what level is research activity occurring?
- Is there evidence of research activity elsewhere within the organisation structure?
Methods
Study design and methodology
This qualitative mapping study was conducted using a critical realist underpinning. Critical realism allows an examination of organisational and societal constructs and has been used to examine complex policy areas within health systems15,16. The use of critical realism was intended to provide an understanding of the organisational structures in place, empirical and non-empirical, which may include policy structures, cultural norms, power imbalances and legislative frameworks17. The authors also sought to generate an understanding of the likely agency of the individual to be able to undertake research at all levels of the organisation, bearing in mind the influence of the structures identified.
The study drew from the following data sources:
- publicly available documents from the organisation’s public internet pages
- internal documents available from the organisation’s intranet
- position descriptions from the publicly available NSW Health electronic recruitment (eRecruit) system
- records of research governance approvals, where research has been approved to be conducted within the organisation, to identify staff currently involved in research.
Documents retrieved included:
- strategic plans for facilities, work units or clinical specialties
- operational plans at the facility, work unit or clinical specialty level
- staff newsletters and internal communiques
- annual reports including financial reports
- external (internet) and internal (intranet) webpages
- departmental reports
- meeting minutes
- organisational charts.
Documents released during the 2015 calendar year, or strategic planning documents with a stipulated date range spanning 2015 (eg plans covering 2014–2018), were included. Internet and intranet pages were included as available at the time of study. Research governance approvals were considered for all studies approved or active within the LHD during 2015.
All internet and intranet pages were manually searched by the lead researcher (DS). Pages and documents that contained relevant information were downloaded for further analysis.
All position descriptions for positions advertised within the LHD between November 2015 and February 2016 were downloaded as PDFs from the NSW Health eRecruit website. Any additional documentation accompanying the position descriptions was also captured.
Research governance records were examined by one co-researcher (JR). Data were extracted into an Excel spreadsheet and sent to the lead researcher for further analysis.
For the purposes of this study, specialist physicians, referred to as visiting medical officers (VMOs), and students conducting research whilst on placement within the LHD, were considered as if they were LHD employees. This is because the LHD had traditionally employed the majority of its medical workforce under a visiting contractor arrangement, thus these physicians are in essence the medical workforce of the organisation. Students on placement are bound by the same policies and codes of conduct as staff and work under direct supervision of staff within the organisation.
Data management and analysis
Data from web pages and positions descriptions were imported into NVivo qualitative data analysis software v10 (QSR International; http://www.qsrinternational.com) for management and analysis. Content analysis was used to identify the terms ‘research’ or ‘evaluation’ within the documents and the context of its use. The term ‘evaluation’ was included to reflect that ‘evaluation’ and ‘research’ are used interchangeably; however, each instance was examined to ensure the document referred to service or program evaluations rather than the evaluation of clinical outcomes in the course of routine care. Research was defined as any project that would or potentially could require submission to a human research ethics committee for approval. All documents that were included because they referred to research or evaluation that could be considered equivalent to research were subsequently included. No further distinctions between research and evaluation were made within the analysis.
The lead researcher developed linkages between references to research, where research was mentioned or described within the organisation’s documents, to assess congruence between organisational responsibility for research, documented research activity and positional expectation of research. This was completed by the use of secondary thematic analysis via a thematic map, where the context of references to research were initially coded, then like codes were grouped to form themes18.
Rigour
All initial coding of the data was completed via NVivo software and undertaken by the lead researcher (DS), with the resultant codes and thematic map reviewed by two other researchers (SK, EW). The other researchers (JR, DL) reviewed the completed analysis to ensure veracity of the information and interpretation with respect to the organisational structure.
In terms of reflexivity, the lead researcher reflected on his role in research training within the public health system in NSW. In designing the study, collecting the data and undertaking the analysis, the lead researcher bracketed his beliefs about research capacity building to minimise the impact on the interpretation19. This was assisted by a process of reflective memos and discussions with co-researchers throughout the iterative data analysis process.
Ethics approval
Ethics approval for this project was granted by the Greater Western Human Research Ethics Committee (reference LNR/15/GWAHS/126), with governance approval from the hosting LHD and informed consent to access the LHDs documents provided by the LHD’s chief executive.
Results
A total of 1654 internet (public domain) or intranet (non-public domain) pages were searched. From these, 151 strategic, operational and other documents were downloaded for further examination. In total, 159 position descriptions were retrieved during the data collection period. Research governance approvals showed 53 projects active in 2015, with 19 projects approved that year, and 34 projects approved prior to 2015 but still active.
Research activity in the local health district
The majority of research approved to be conducted within the LHD was externally initiated and led by an external principal investigator (Table 1). Approximately one-third of all projects were initiated within the LHD and a similar number engaged LHD staff as members of the research team.
Within the LHD, medical practitioners were most active in research, notably VMOs and medical students under VMO supervision. As these projects were conducted through the LHD they came under the auspices of the organisation. Any projects initiated and approved within the university sector, as might happen with a conjoint appointment, were deemed external projects. Registered midwives and health promotion staff were also active, while allied health services and pharmacy were only involved in one research project respectively.
Table 1: Research activity as determined by research governance approvals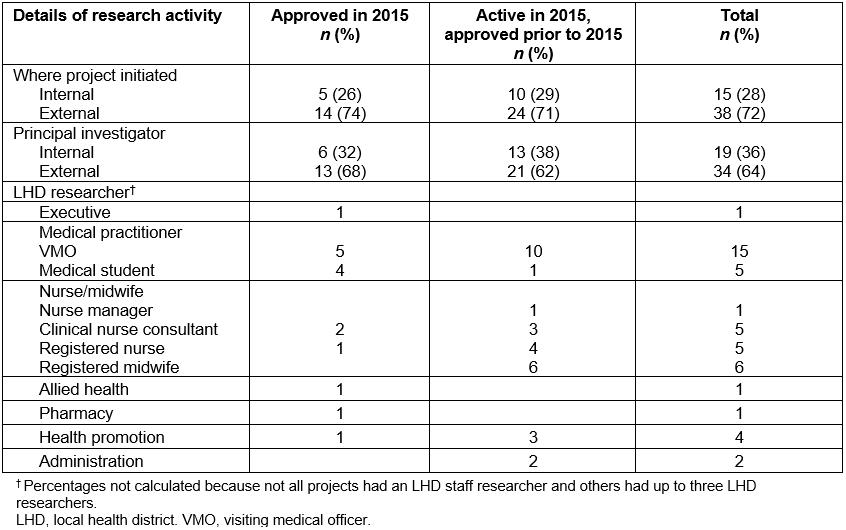
Positional responsibility for research
Examination of position descriptions (n=159) can be seen in Table 2. The majority of medical, allied health and administrative roles did not contain positional responsibility for research or service evaluation activities. Registered nursing and midwifery roles indicate an expectation of participation in or contribution to research; however, this is not noted in enrolled nurse or assistant-in-nursing roles. While only a small number of executive and management roles were advertised, the majority of these contained some level or responsibility for conducting research, participating in quality activities or managing those who do undertake research. No health promotion positions were advertised during the data collection period.
It should be noted that some, but not all, position descriptions were accompanied by a schedule of other organisational responsibilities, which indicated that all staff were expected to ‘participate in, and where applicable lead … quality improvement activities’.
Table 2: References to research or evaluation within position description, by profession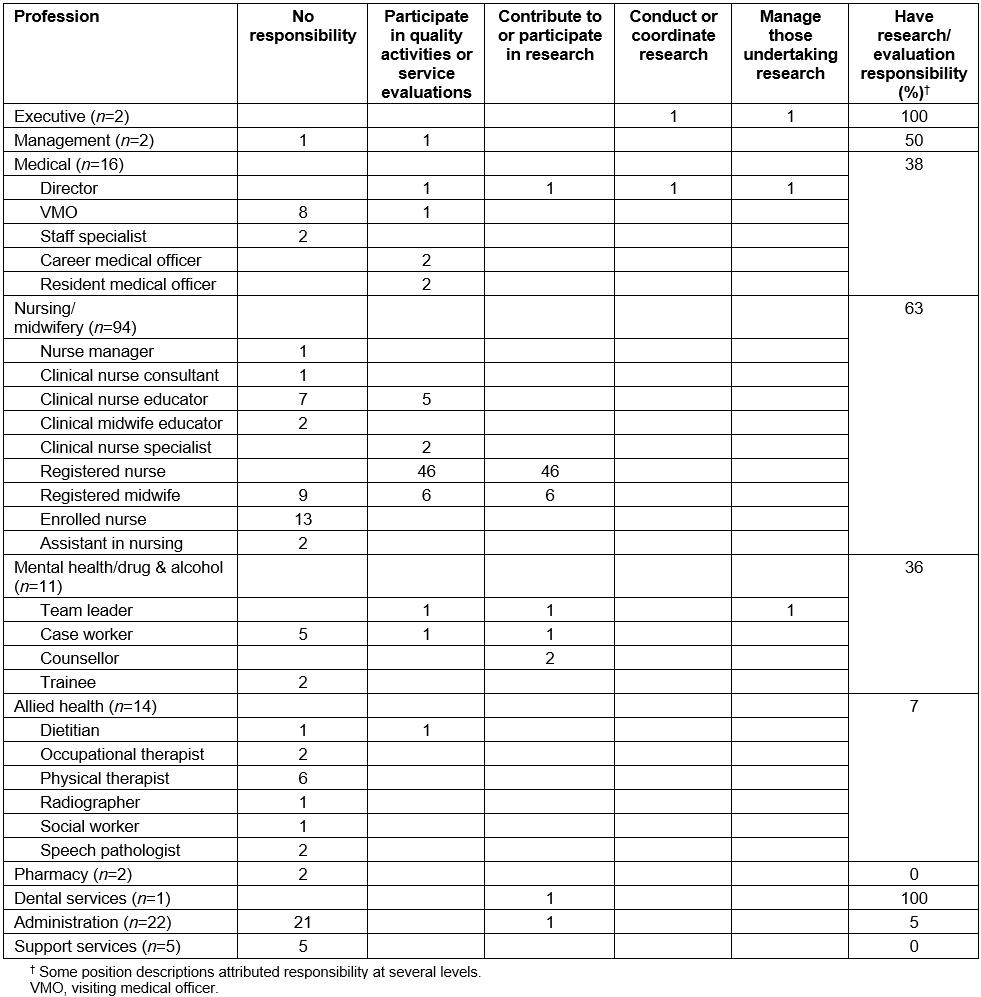
Research within strategic, planning and operational documents
Exploration of the organisation’s strategic and operational documents revealed a number of themes relating to the conduct of research activities within the organisation:
- challenges, resources and needs
- collaboration
- strategic direction.
These themes are explored below, with reference to the key documents within which the relevant information was located.
Challenges, resources and needs: A number of challenges were identified within planning and operation documents. These include a perceived lack of strategic support and coordination, as described by the organisation’s board:
A challenge in [the organisation] is a lack of strategic [organisational] support in relation to research. There are a number of research projects being undertaken within [the organisation] however these projects are not being managed or led by [the organisation’s] staff.
LHD board minutes
This lack of strategic support is associated with another challenge, as reflected in the organisation’s service agreement with the NSW Government, which identified a lack major research facilities and organisations based within the LHD, either as LHD-controlled entities or independent medical research institutes within the LHD.
One concern for the establishment and continuance of research endeavours was a perceived lack of dedicated resources, as reflected in the organisation’s rehabilitation clinical services plan:
Delivery of best practice, innovations and research are limited by a lack of resources to drive these initiatives.
LHD rehabilitation clinical services plan
Resourcing for research activities was addressed in the organisation’s service agreement, which outlined the need to ensure ‘business, human resources, information technology and financial service processes support research activities’. This extended to appropriate support staffing for research administration, which included research ethics and governance functions. Under the current structure, research activities fell under the oversight of the organisation’s clinical governance unit.
Funding for teaching, training and research was outlined in the organisation’s service agreement, and in the 2015–16 financial year attracted 0.5% of the organisation’s annual budget. It is not clear from the strategic and operational documents what activities or resources were within the scope of that budget, or what proportion of that budget was available for research activities.
Along with these challenges, established needs related to research were identified, including a need to:
- ‘Provide training for clinician researchers and facilitate access to research support’ (service agreement)
- ‘Expand innovative use of information technology to manage information and make it appropriately accessible for research’ (internal communique)
- ‘Explore teaching and research opportunities, including joint academic and clinical appointments, to enhance the knowledge and skills of the workforce and drive the research agenda’ (mental health clinical services plan).
Collaboration: The organisation’s documents demonstrated an interest and effort in engaging partners for ongoing research. Identified research collaborators included six universities with a presence in the LHD, either via a facility within the LHD’s geographical region or by teaching and training links. Other collaborators included state government health education bodies, local governments, technical colleges and federally funded primary healthcare organisations.
Collaboration was viewed within the documents as means of moving towards best practice. This was exemplified within the LHD’s palliative care plan, which referred to the practical ways in which research collaboration could be realised into the future.
Over the medium term [the LHD] should seek to identify possible research partners and conduct research on practical, practice related issues focused on palliative care in a rural setting. Utilizing and promoting the rural research capacity building program through the [NSW Health] Education and Training Institute or establishing links with tertiary institutions to conduct two research projects per annum on palliative care in a rural setting. … Over the longer term [the LHD] should investigate the feasibility of establishing a Centre for Rural Community Nursing (including palliative care) in conjunction with a suitable tertiary institution.
LHD palliative care plan
It is important to note that the language around collaboration was future-focused, reflecting a desire to collaborate rather than an existing collaborative relationship with the identified partners.
Strategic direction: Under the terms of the organisation’s service agreement, the LHD had a number of clearly defined roles in regard to research. The organisation was required to undertake research ‘relevant to the provision of health services’. This extended to:
- fostering a dynamic and supportive research culture through strategic leadership and governance
- attracting and retaining high quality clinician researchers
- providing training for clinician researchers and facilitating access to research support
- ensuring business, human resources, information technology and financial service processes support research activities
- attracting clinical trials by removing the barriers to undertaking clinical trials in LHDs.
The organisation’s strategic plan outlined the importance of research activities, particularly in the development and implementation of new models of care, with a focus on accessibility, sustainability and relevance to rural communities. The plan outlined the markers for evidence of achievement of this goal, with a focus on implementation of models of care that minimised patient travel and length of stay along with improved Aboriginal health indicators.
The appointment of a board-level research and innovation committee is a clear indication of the intent to develop a strategic approach to research. This committee had responsibility to:
- predict and strategically plan for change and draw on partnerships to research, develop and implement new and/or innovative models of care which will be sustainable and relevant to rural communities within the organization’s geographical region
- identify potential projects and make recommendations with regard to seed funding of projects, and the monitoring and evaluation of outcomes of projects
- ensure projects have a solid base in evidence, theory, experience or example and are implemented within a research framework
- ensure development and implementation of projects are done with active community and clinician engagement and input to ensure openness, transparency and accountability.
LHD board research and innovation committee terms of reference
While the research and innovation committee had strategic responsibilities, the executive and board of the organisation as a whole had monitoring and reporting responsibilities for research activity, research collaborations, applications for ethical review and research governance.
Below board level strategic documents indicated a planned approach to research for certain professional groups or clinical areas. The LHD’s nursing and midwifery clinical educators framework indicated a need for clinical nurse and midwifery educators to collaborate internally with key staff, including clinical nurse consultants, to identify research opportunities. Similarly, the organisation’s falls prevention plan (2013–15) discussed the need to ‘support the conduct and dissemination of research to advance falls prevention policy and practice’. The organisation’s aged care clinical services plan discussed the need to continue to support aged care research to assist the development of evidence based practice. The organisation’s rehabilitation clinical services plan specifically indicated a need for research into the development of telehealth as an outreach model of care and as a method of home based therapy. The organisation’s surgical services plan indicated that pathology services are able to assist with ‘education, training, research and advice’, but there were no further references to research within that plan.
Of the facility and health services operational plans, only one facility’s health service plan specifically addressed research, with a vision that both theoretical and translational research is ‘imbedded and supported’. The importance of translational research activities was particularly outlined within the plan, with repeated references to the ability of this form of research to inform practice.
Proactively promote the development of more translation research activity to inform the continual improvement of clinical practice.
LHD facility health service plan
Discussion
This research examined the place of research within a large rural health organisation’s structure. It is important to understand the structural context within which research may be conducted, as this structure may facilitate or inhibit the activity of research and the development of clinicians as researchers.
It is clear that the LHD as a whole had both an obligation and a willingness to conduct and support research. Strategic leadership across the organisation is an important component of rural research capacity building20 and in this study the organisation acknowledged a lack of strategic leadership and coordination of research activities. While there was evidence of strategic level planning to address this need, operational-level documents did not contain evidence of how this strategic direction would be enacted. In effect, the lack of operational priority created a situation where research activity was driven largely by the agency of individuals.
It is unsurprising, then, that research activity within the organisation was most evident in a group with a greater amount of individual agency. Medical practitioners, in this instance VMOs and students under VMO supervision, were the largest contributors to research activity within the organisation, despite research not being specifically listed as a positional responsibility within VMO position descriptions. The mechanisms by which this activity occurred can be observed at several levels. As VMOs are essentially private contractors to the health service, they have a high degree of autonomy in regard to their workload, roles and responsibilities. This autonomy is also a function of the positional power associated with the medical profession within health services. However, professional autonomy or individual agency is not the sole enabler of research activity. The activity seen may reflect a culture of research within the medical profession. Academic publication is seen as a means of career advancement within parts of the medical profession21,22, and this may also be a driver of research activity.
Nursing staff, in contrast, were seen to have the greatest positional responsibility for research, but undertook very little research activity. Compared to the high levels of positional and professional autonomy afforded their medical colleagues, many nursing staff had little autonomy in determining their workload and time priorities. Protected research time is a known enabler of nursing research23. In the absence of a supportive structure such as a research-focused business plan, there was limited agency for the nurse with an interest in or responsibility for research to turn that interest into research activity. The nursing culture towards research has been described as ‘indifferent’, due in part to research that has not led to practical change24, so the organisation’s focus on translational research – that is, research that explores the process and outcomes of implementing research findings into a clinical setting – and new models of care may be a productive way of engaging nurses as researchers.
There was limited research activity for allied health professions. Allied health services have been described as ‘research emergent’, lacking a history and culture of research25, and this may be evidenced by a lack of responsibility for research within the position descriptions of the majority of allied health professionals. While a need for research training for allied health staff was identified, training alone will not be sufficient to increase allied health research, with a broader organisational support involving leadership, supportive policies, coordination and recognition of research activities required26.
Having research outlined within a position description is one feature of health research capacity building11, although within most position descriptions reference to research was staff ‘practicing in a research-informed manner’. This descriptor was particularly prevalent in nursing roles and absent in those for professions such as allied health. Reference to active involvement in research within position descriptions was occasionally ambiguous, with references to ‘contributing to research’ or ‘participating in research’, with the latter able to be interpreted as being a research subject rather than a researcher.
The presence of research in strategic plans and position descriptions may seem like an enabler for research, but this is countered by the lack of research focus in facility and work unit operational or business plans, which presents a significant structural barrier to research activity. Successful research capacity building contains activities and structural supports at the individual, team, organisation and supra-organisational levels11, and in rural health it is organisational supports rather than individual factors that have been demonstrated to be critical in non-completion of research endeavours27. Operational plans that enable and support the individual to pursue research activities will not only allow the individual to meet the obligations outlined in their position descriptions, but also assist the organisation to meet its strategic goals and obligations for research.
While the organisation’s service agreement referred to research that is relevant to health services, the organisation’s strategic plan indicated a single strategic focus on research into new models of care. There is a long history in health services that ‘what gets measured gets done’28,29, and a focus on research that only develops new models of care may limit the scope of research into other areas of potential benefit to the health service and health consumers.
The sole facility service plan containing references to research provided an example of the value and importance of research being emphasised at the facility level. A similar emphasis may have been excluded from the service plans of smaller facilities to reduce the expectations on a small generalist workforce. Such a decision may inhibit the ability of staff within these smaller facilities to actively engage in research activities, to the detriment of the LHD’s strategic focus; in rural health, need is a driver of innovation30,31, and smaller facilities are often sites where new models of care are developed. The focus on translational research within the facility service plan indicated a desire for the majority of research occurring within that space to have immediate practical application32.
Resourcing for research was identified as a challenge for implementing research within the LHD. Research activities are block funded along with teaching and training. As there is no clear delineation for the proportion of this funding dedicated to research activities, there may be competition for this limited funding. With the state potentially changing to activity-based funding for teaching, training and research33, organisations will need to consider the role of research and the ability to conduct, host or collaborate on research activity at a level that will attract and maintain funding, and the approaching timeframe adds a level of urgency to this necessary discussion.
One of the challenges within rural health organisations is research that is conducted within, but not for or by, the organisation. Limited engagement of local staff within these research projects leads to few opportunities for research capacity building within the organisation. The present study did not explore the designs or content of research being conducted by external agencies, such as universities or non-government organisations, within the LHD. The organisation’s service agreement emphasised attracting clinical trials, and across the strategic planning documents there are references to a need to balance locally relevant research endeavours and allowing larger scale endeavours with little immediate local relevance. A move to activity-based funding for research may lead rural health organisations to critically examine the cost–benefit of engaging in clinical trials given the relative lack of direct benefit to the organisation.
As an organisation without a large research unit, the LHD relied on collaboration in many of the research endeavours identified. This type of collaboration has been described as a means for health researchers to access needed expertise1,26. The fact that known collaborators are identified within the documents indicates the LHD has existing collaborative relationships in place; however, it is not clear if these collaborations are strategically driven or have developed on an ad hoc basis. A collaborative model of research is more consistent with successful research capacity building11,12,20 and the ability of LHD staff to interact with experienced researchers is more likely to assist in the development of research skill in rural clinicians. In addition to external collaboration, there exists an opportunity for increased internal collaboration. Those already active in research, such as VMOs, could collaborate with others in the LHD, in effect becoming research ‘champions’ (eg involving a junior medical officer in a project that a student and VMO had instigated). Extending beyond a single profession, encouraging collaboration between allied health and existing researchers within the LHD in a multidisciplinary cooperative would be an appropriate means of building allied health research capacity26. These collaborative strategies can provide expertise and support, in some respects offsetting the lack of a critical mass of researchers needed to build allied health research capacity26.
One strategy within the organisation was to train and attract clinician researchers, and there was a small pool of researchers responsible for approximately one-third of the LHD’s research activity. Training for these individuals is desired, but few options for training were identified beyond formal supported research training programs such as NSW Health’s Rural Research Capacity Building Program9,27. Identifying training needs via a research training needs assessment is a key element of research capacity building11. The role of the clinician-researcher can be a challenging one34,35, and organisational support not only for training but for the conduct of research is required for successful research completion10,23,27,36.
Limitations
This study was limited to documents relevant to the year 2015. Although attempts were made to capture planning documents that were released prior to that year, it is possible that not all relevant documents were found. This study relied entirely on documents available on the public internet or internal intranet of the LHD and therefore documents held on individual network drives were not accessed or included.
This study included documents that referred to both research and evaluation. Other synonymous terms may have fitted the definitions of research or evaluation used in this study, and as a result these documents may have been included.
Conclusion
This study has found that, in a rural health organisation in NSW, Australia, a lack of operational planning for research leads to a reliance on individuals to drive research activity. There appeared to be a mismatch between positional responsibility for research and research activity conducted, with personal agency a key factor in activity.
In this study, the majority of the rural research conducted did not engage local staff as researchers. Rural health organisations face challenges including a limited numbers of skilled researchers, limited resourcing and an acknowledged lack of organisational support and coordination. In such a setting, collaborative links become increasingly important.
Rural health organisations have an opportunity to create a positive research culture by ensuring the potential to engage in research is reflected in the operational plans for all facilities and work units. Engaging existing researchers as ‘champions’ and enabling internal collaboration will strengthen research activity and build research capacity.
References
You might also be interested in:
2014 - Community preparedness for highly pathogenic Avian influenza on Bali and Lombok, Indonesia





