Introduction
Fetal alcohol spectrum disorder (FASD) represents a range of developmental disabilities in the context of prenatal alcohol exposure, with high rates of secondary effects on mental health, daily function and participation1,2. Secondary effects of FASD include anxiety and depression, self-harm and suicide, drug and alcohol dependency, and impulsive behaviours, which can result in adverse outcomes such as contact with the criminal justice system2. The functional impairment resulting from prenatal alcohol exposure may become more apparent at key transition times throughout the lifespan. These include during infancy, on entering formal education, when transitioning to secondary education and during adolescence, and when leaving education and seeking employment3.
The prevalence of FASD in Australia is not known, and likely underestimated because of diagnostic service limitations4. In some Australian populations at risk for prenatal alcohol exposure, FASD prevalence has been ascertained as 194 per 1000 among school-aged Aboriginal children in the remote Kimberley region in the north of Western Australia (WA)5, and 360 per 1000 among juveniles in detention in WA6.
Diagnosing FASD is complex, requiring a process of referral, screening, assessment and multidisciplinary decision making7. Barriers to FASD diagnosis in Australia include lack of awareness of FASD diagnostic criteria, low numbers of trained clinicians and lack of funding mechanisms to support diagnostic teams8,9. In regional areas, further barriers to diagnosing developmental conditions include chronic staffing shortages and lack of coordination of existing services10.
Both missed diagnosis and misdiagnosis of FASD disrupt the capacity of individuals and families to access the services and supports required to fully participate in society, increasing the burden of FASD across the life course11. Early intervention is crucial to mitigate the impacts of FASD12-14; however, the condition is often not recognised until a child enters formal education15. Even when FASD is considered, other barriers may delay recognition of the full extent of an individual’s neurodevelopmental impairments and what this means in their daily life3. When a diagnosis can be made, caregivers of individuals with FASD have described treatment barriers, unmet needs and high levels of parenting stress16. Despite the increasing focus on the needs of those affected, health, education, and social support systems have struggled to adequately support individuals and their families16. Further, research has demonstrated significant gaps in the knowledge of professionals working in the health, education and justice systems17-23. These sectors therefore need to be incorporated in strategies aiming to support the diagnosis and treatment of individuals with FASD.
Addressing fetal alcohol spectrum disorder in the Pilbara
Regional communities often experience a cumulative disadvantage of limited health service access and high rates of childhood developmental disability. A community-based study, ‘Starting on Track’, about implementing the Australian Early Development Index (AEDI) across the Pilbara region of northern WA, reported that in several remote Aboriginal communities a significant number of children (45–85%) were considered vulnerable in one or more developmental domains24. To identify and understand the likely reasons for the high levels of developmental vulnerability reported among young children living in these communities, the AEDI results for 2007 and 2008 were widely disseminated to key stakeholders and extensive consultations were conducted with communities, education, and health professionals to obtain their perspectives. The key issues raised included ongoing infectious diseases (skin, ears and lungs), behavioural and cognitive impairment, and FASD due to mothers drinking in pregnancy25.
Increasingly, between 2008 and 2011, concerns were raised about alcohol use in pregnancy by Pilbara Aboriginal community leaders and service providers. FASD was prioritised as a community concern at the Pilbara Indigenous Women’s Gathering (PIWAC) in 2010. The PIWAC Gathering report highlights ‘the ongoing issues of drug and alcohol abuse in young people, the relationship of such abuse to crime and incarceration, and the lack of resources dedicated to preventative practices’ (p. 5)26. During this period, the CEO of Wirraka Maya Health Service Aboriginal Corporation (Wirraka Maya) was awarded a Churchill Fellowship to conduct a comprehensive study in Canada and the USA examining the impact of prenatal alcohol exposure on parenting and affected children in Aboriginal communities27. The study recommendations formed a foundation for a network of local service providers to address concerns related to FASD (the Hedland FASD Network), as well as the WA FASD Model of Care28. The service providers involved in the Hedland FASD Network are shown in Figure 1. The importance of community-led action to address FASD in a coordinated fashion was further reinforced by the Marulu Strategy, initiated by community leaders in the Kimberley region29.
The community impetus for research to prevent FASD in the Pilbara was supported by stakeholder consultation to inform a FASD strategy for 2015 to 2020, funded by BHP26. The consultations with Aboriginal community leaders, elders, Aboriginal community controlled health organisations and key informants across the Pilbara were conclusive. Both alcohol use in pregnancy (and FASD) and alcohol consumption in the community more generally were a major concern, having an adverse impact on the social and economic development of communities across the region26.
In response to the growing concerns about FASD in WA, the Department of Health and the WA Child and Youth Health Network convened a working group to develop the FASD Model of Care28. The FASD model of care contains a series of recommendations to guide agencies across government and non-government sectors related to prevention, screening, diagnosis, therapy, intervention and care.
These community concerns and policy responses informed the development of two innovative participatory action research projects aiming to reduce alcohol in pregnancy and therefore FASD across the Pilbara. The first project, the Hedland FASD Prevention project, ‘Warajanga Marnti Warrarnja – Together we walk on country’, a partnership between the Telethon Kids Institute, Wirraka Maya, the Hedland FASD Network, and the FASD Community Reference Group comprising respected local Aboriginal elders and community representatives, commenced in 2015. The second project, funded by the National Health and Medical Research Council, ‘Making FASD history in the Pilbara: an evidence-based prevention intervention’, is a partnership between Telethon Kids Institute, Purntukurnu Aboriginal Medical Service, Mawarankarra Aboriginal Health Service, Wirraka Maya, and WA Country Health Services and WA Mental Health Commission, Drug and Alcohol Office. The project is conducted in Port Hedland, Newman, Roebourne and surrounding communities and commenced in 2016. Both projects have been endorsed and supported by the Pilbara Aboriginal Health Planning Forum, which has identified maternal and child health as a key priority and elevated reducing FASD as a primary objective for all health service and relevant interagency stakeholders across the Pilbara.
A key objective of these projects is to implement the recommendations made by the WA FASD Model of Care by supporting local health services staff to develop a localised framework for early diagnosis and support for children with FASD. Such a framework could assist professionals working in a variety of sectors to facilitate access to appropriate services, decreasing fragmented health care and support for families.
This article describes the processes involved in mapping referral pathways, clinical services, family support services and resources to integrate service delivery and clarify the pathway from referral through diagnosis and management of FASD for children, families, carers and service providers.
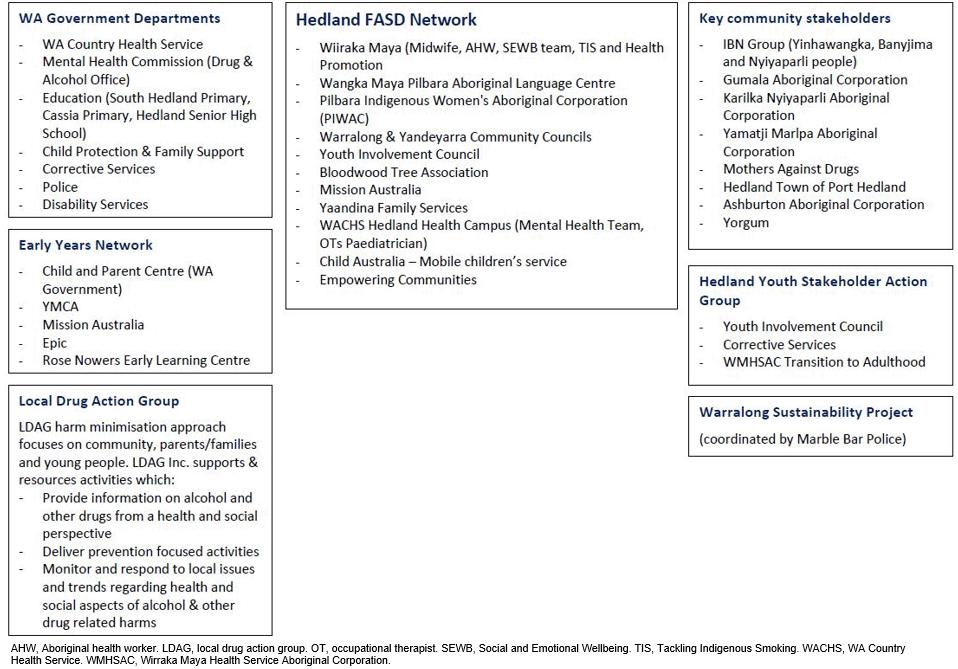 Figure 1: Stakeholders and organisations involved with the Hedland FASD Network (2013–2018).
Figure 1: Stakeholders and organisations involved with the Hedland FASD Network (2013–2018).
Methods
This project was initiated under the auspice of the ‘Warajanga Marnti Warrarnja’ Hedland project to build the knowledge and capacity of workforce and service providers to address FASD in the town of Port Hedland (including South Hedland) and the remote WA communities of Warralong and Yandeyarra.
The development of the referral pathways involved using community participatory action methods (CPAR)30. CPAR has emerged from a tradition of action-oriented research promoted in the 1940s by social scientist Kurt Lewin as a means to facilitate social change and equity in health and wellbeing among diverse populations31. Refinements to this approach over subsequent decades have focused on transformative, empowering and emancipatory elements to redress inequalities for vulnerable and marginalised groups32. Importantly, the principles underpinning CPAR require researchers to involve communities as equal and genuine partners throughout all phases of the research process, thus making it a highly appropriate research approach when working with Aboriginal populations who have historically been excluded from positivistic and biomedical research agendas and outcomes. In contrast, CPAR emphasises mutual respect and co-learning between partners, individuals and communities, and a balance between research and action to increase community and workforce capacity, and catalyse systems-level change33,34.
Strengths and advantages of using CPAR have been highlighted in a number of studies33-37. These include bringing together the diverse skills, knowledge and expertise of all research participants to address complex issues; building on the strengths, knowledge and resources of communities; promoting two-way learning and creating shared understandings and new knowledges derived from both community and stakeholder perspectives; bridging cultural difference through the collaborative processes; instilling ownership and generating uptake and sustainability of resources and models of care; and changing policies and securing funding to address local issues.
To develop a localised framework for early diagnosis and support for children with FASD, information about existing diagnosis, therapy and support services in the Hedland region was collected. This was undertaken via internet searches and phone calls, the Hedland FASD Network meetings and via snowballing. The project team consulted extensively with the Hedland FASD Network members, early childhood and primary health services in Hedland, the WA Country Health Service, education, child protection, justice services, and drug and alcohol services, as well as members of the FASD Community Reference Group. A total of 35 stakeholders were involved in individual consultations.
These consultations were undertaken to identify the multidisciplinary team members and services required in the referral, diagnosis and management of FASD, taking into account the unique and complex circumstance of working with diverse and vulnerable groups in remote communities. In addition, researchers worked to identify validated assessment tools used in the screening process by health professionals as part of their clinical reasoning process.
The first phase of the iterative development occurred between April and August 2016 and involved consultation with the Hedland FASD Network and relevant service providers, using face-to-face meetings, teleconferences and email correspondence. The second phase occurred between September 2016 and February 2017. In addition to ongoing consultations with the FASD Network, expert advice was sought from clinicians and senior health service managers to ensure a comprehensive coverage of all key support services. Clarification was also sought through the disability services, and early years and youth networks.
Ethics
Ethics approval for this study was obtained from the University of Western Australia Human Research Ethics Council (HREC RA/4/1/7869), Western Australia Aboriginal Health Ethics Committee (HREC 664) and the Western Australia Country Health Service Human Research Ethics Committee (HREC 2015/35).
Results
Based on the iterative process of service mapping and consultation, stakeholders identified discrete time points at which screening for risk of FASD may be undertaken. These included the antenatal period (based on prenatal and post-natal risk factors) (0–4 years), early childhood or at enrolment in early learning or pre-kindergarten/school (age 4–6 years) and at entry into child protection or the justice systems. Three referral pathway templates were developed to identify key stages of an individual’s interaction with the relevant service providers. These templates incorporate health, education and justice as the key systems of interaction. The health system template includes information for the antenatal, newborn/postnatal and early childhood periods (in particular 0–4 years). The education system template is intended to provide a guide for children of school age (4–10 years). The justice system template is designed for those working in youth justice and adult services and support (10 or more years).
Within the referral pathways, a standardised sequence of events is detailed, reflecting the chronology of a child development assessment process:
- referral (including the reasons for referral and the source of referrals)
- screening (including professionals that may undertake screening, and the instruments or tools they may use)
- assessment (including professionals or organisations that can conduct assessments, and the standardised assessments they may use)
- service providers (agencies and specific organisations in the region that conduct assessments)
- diagnoses (a list of formal diagnoses that may be made)
- services and funding (including funding agencies and programs for which individuals with a formal diagnosis may be eligible)
- services and support (including therapy and family support service providers in the local region).
The final referral pathways for health, education and justice systems are presented in Figures 2–4.
The final phase involved final edits to and endorsement of the referral pathway schematics and supporting text, by contributing service providers, the Hedland FASD Network and the Pilbara Aboriginal Health Planning Forum. This was achieved through individual telephone consultations and workshopping the pathways at the Hedland FASD Network Meeting. Following endorsement of the referral pathways, they were disseminated via email to all contributing stakeholders, which included an extensive distribution list.
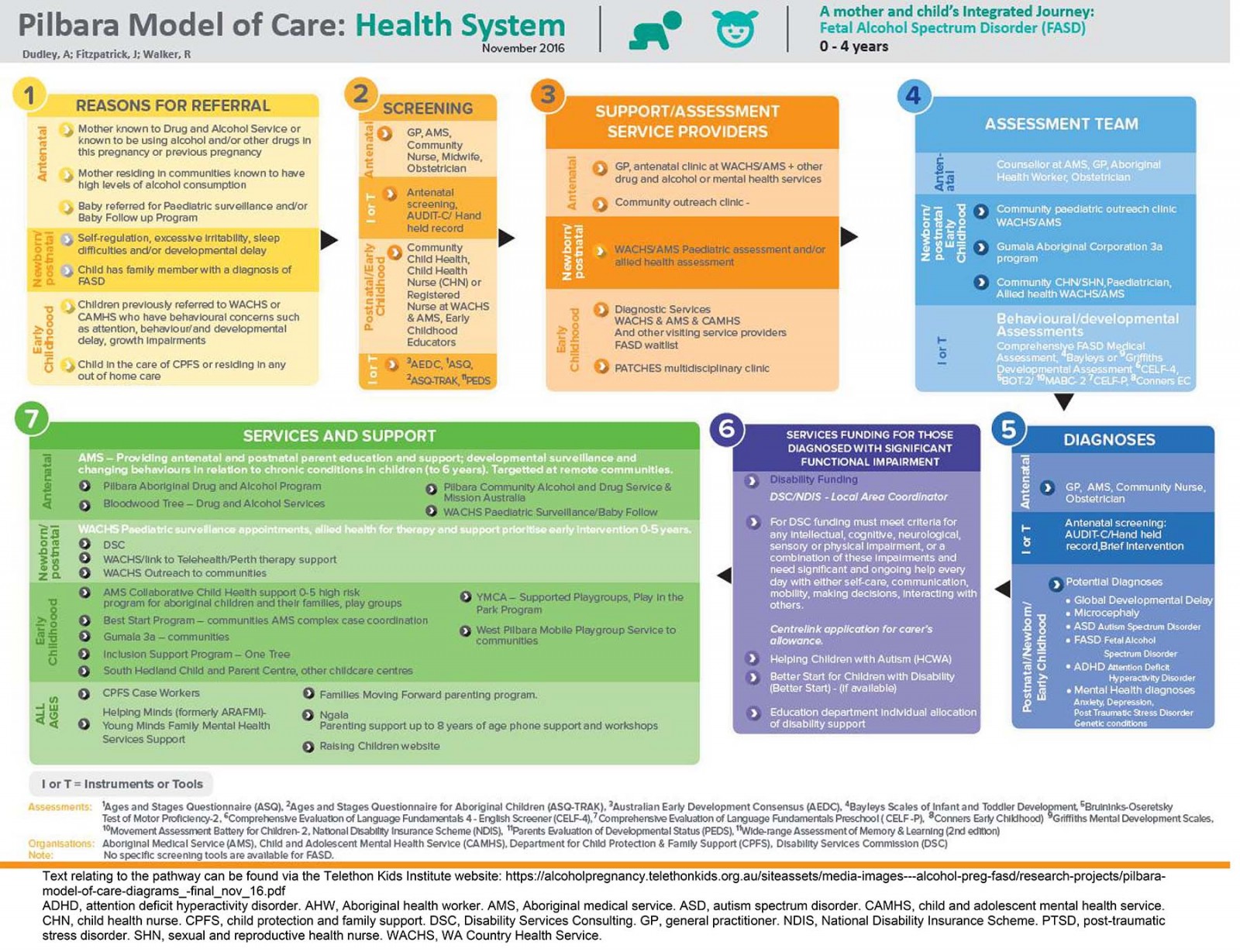 Figure 2: Pilbara Model of Care health system referral pathway for FASD.
Figure 2: Pilbara Model of Care health system referral pathway for FASD.
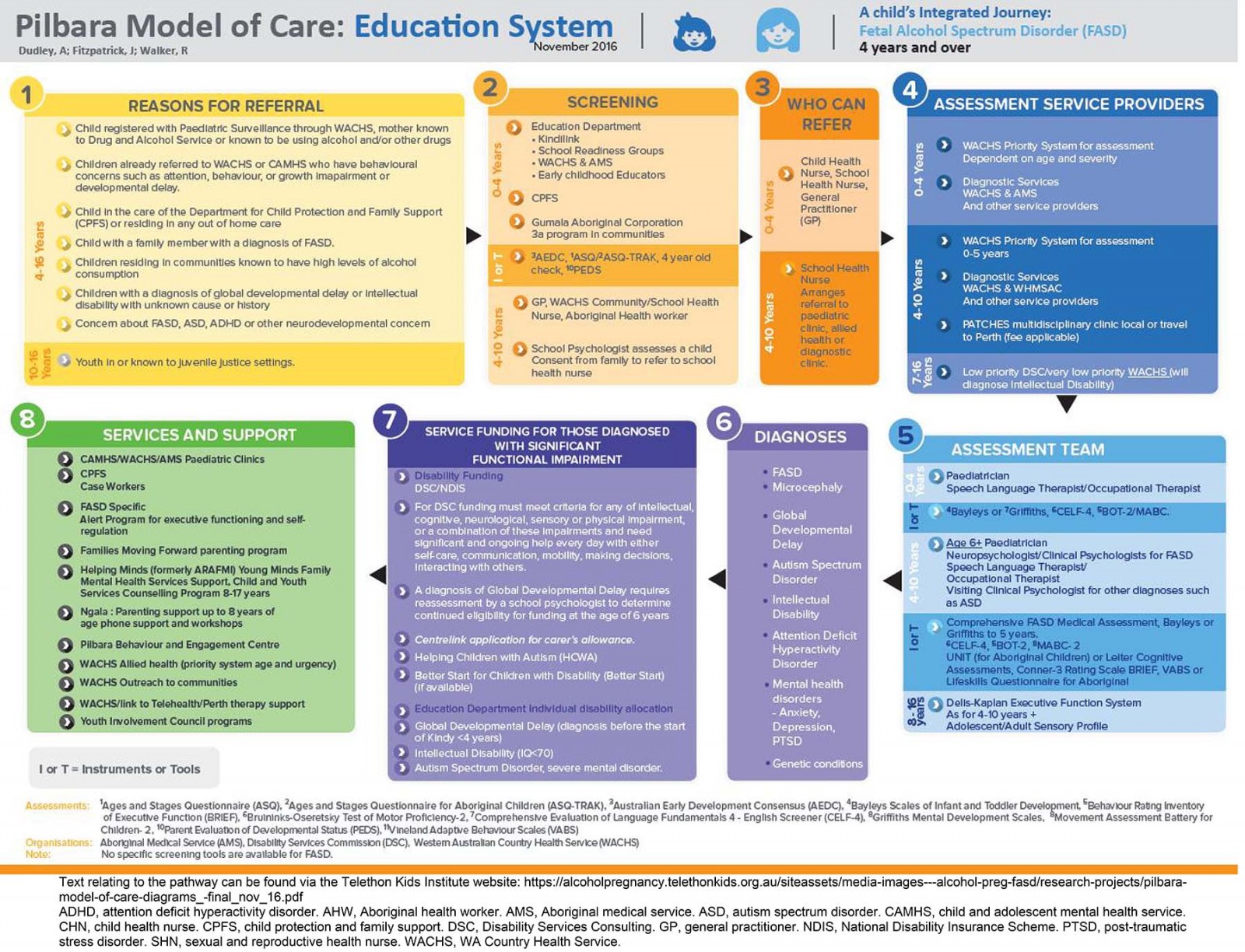 Figure 3: Pilbara Model of Care education system referral pathway for FASD.
Figure 3: Pilbara Model of Care education system referral pathway for FASD.
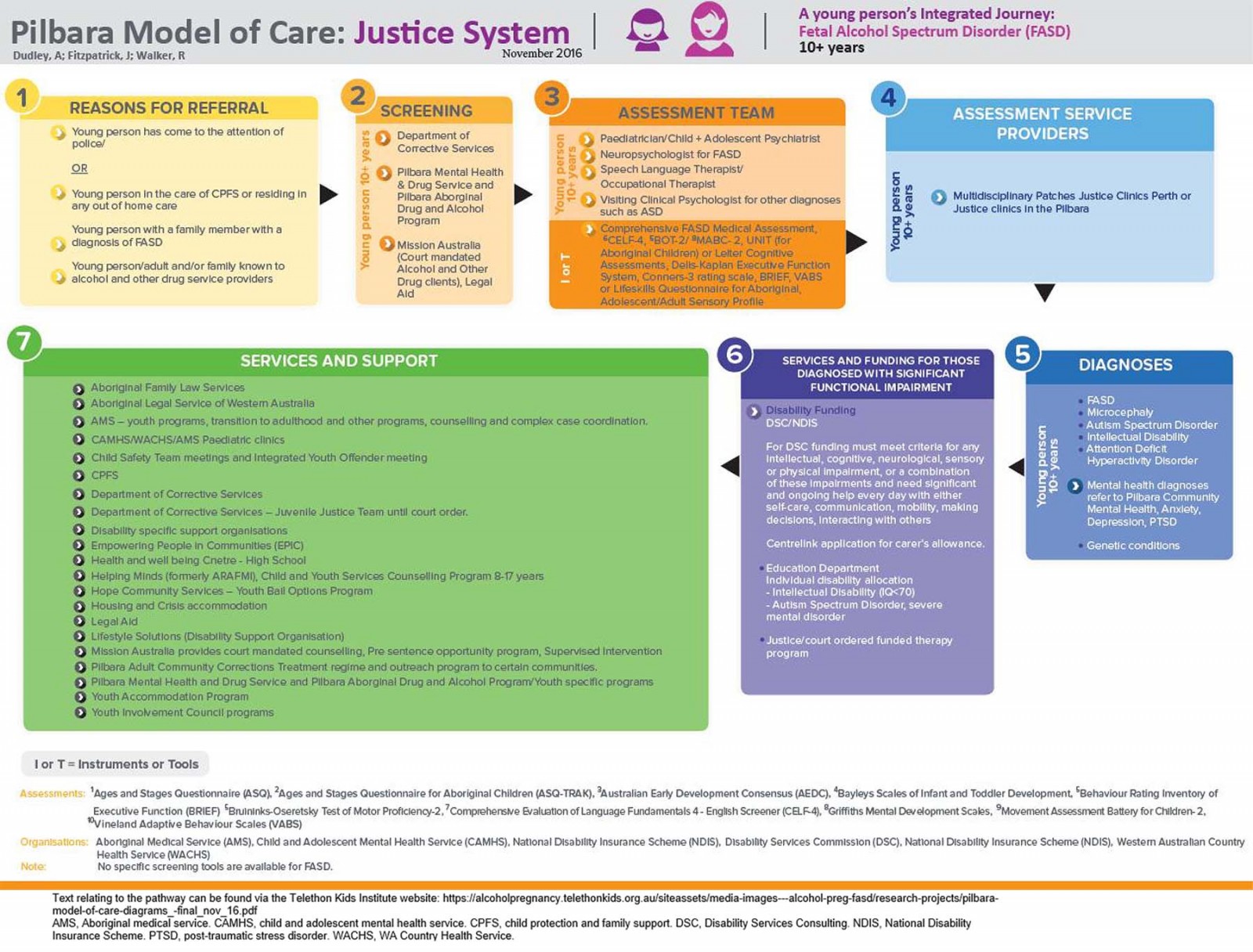 Figure 4: Pilbara Model of Care justice system referral pathway for FASD.
Figure 4: Pilbara Model of Care justice system referral pathway for FASD.
Discussion
This project has enabled the development of a resource to assist professionals working in a variety of sectors with individuals at different life stages. Specifically, the referral pathway schematics are visual aids that easily identify key local services and their integration and involvement in the diagnosis and management of FASD. The identification of assessment tools that can be used in the screening process brings consideration to the clinical process regarding reasons for referral for FASD assessment. Further, the resource can assist professionals to understand the client journey in accessing FASD-related services and supports. Most importantly, by clarifying the pathway from referral through diagnosis and management of FASD, the referral pathway schematics can facilitate early and appropriate intervention and support for children and their families.
A strength of this study is the CPAR approach applied in working with the Hedland FASD Network and FASD community reference group members, and local service providers. Consultation with these stakeholders enabled detailed descriptions and content to be formulated within a client journey framework. Incorporating a life-course approach, models were developed within the health (0–4 years), early education (5–10 years), and justice systems (10 or more years). Certainly, there are many overlaps with pathways for other developmental conditions, and as such the FASD referral pathways could be a resource for a range of conditions. Generalisability of this model is evidenced within a National FASD Consortium funded by the Australian Government Department of Health (FASD Diagnostic Services and Models of Care Grant Opportunity); the referral pathways model described here is currently being utilised to develop FASD service frameworks across several sites including the Pilbara in Western Australia, and in the Northern Territory, South Australia, Victoria and Tasmania.
Future work will evaluate the resource using a RE-AIM framework38,39. This framework encompasses five dimensions that will enable the team to systematically assess the robustness, translatability and public health impact of the application of the referral pathways at individual and organisational levels as well as the credibility, transferability and dependability of the CPAR process from within a critical paradigm40. These five dimensions are:
- reach – the extent of reach to target populations across the Pilbara
- effectiveness – the extent to which it assists professionals in each sector to provide appropriate referrals, and facilitates early intervention and support for individuals with FASD
- adoption – by target settings, organisations, health and interagency staff
- implementation – consistency and cost-effectiveness of applying the referral pathway in different settings
- maintenance – intervention effects on individual parents, carers and children with FASD and in real-world settings (ie public health, schools and justice settings) over time.
The internal and external validity of the research (credibility, transferability and dependability) will be derived through the negotiated consensus and reflexive decisions arrived at between researchers and research participants in developing the referral pathways41, adherence to CPAR principles36, and NHMRC ethical guidelines and values in the conduct of Indigenous research42. The findings of this evaluation will be the subject of a separate publication.
A challenge of implementing the referral pathway, particularly in regional, rural and remote communities, is access to trained medical, psychology and allied health staff. A number of mechanisms are enabling this activity in the WA Kimberley and Pilbara regions, and throughout the Northern Territory. These include upskilling locally based public sector and non-government clinicians through online FASD training (FASD Hub Australia) and the University of Western Australia’s Graduate Certificate in the Diagnosis and Assessment of FASD. In addition, there is access to Commonwealth funding for outreach specialist services including paediatricians and neuropsychologists, and NDIS funding and telehealth paediatric processes to build FASD specialist, allied health and psychology services in regional and remote communities (Patches Paediatrics & Therapy Services).
Conclusion
Early and accurate diagnosis of FASD is crucial to improve outcomes and overall quality of life for children and their families/carers. The development of a framework to clarify local referral and support pathways enables effective integration of services for FASD referral, screening, diagnosis, provision of disability support, and therapy/intervention and management. It is hoped that this resource will facilitate early intervention and parent and carer support, increasing the likelihood of improved outcomes for children diagnosed with FASD.
Acknowledgements
This work was funded by a BHP grant to support FASD prevention, diagnosis and therapy in the Pilbara. The work would not have been possible without the support of the FASD community reference group members, and member organisations of the Hedland FASD Network and Pilbara Aboriginal Health Planning Forum.

