Introduction
The personal, social and economic costs associated with common mental health disorders and related symptomatology are considerable1,2. Shaped by distal economic and political conditions, population health frameworks identify a layered and interacting array of risk factors in the development of mental health problems3. In rural Canadian settings, globalization and subsequent restructuring have increased many individuals’ and communities’ exposure to various life circumstances that have the potential to endanger mental health4,5. These include job loss, constrained employment opportunities, diminished formal and informal support networks, financial hardship and reduced availability of various federal and provincial services, among others.
Some subgroups of rural residents, such as farmers, may be more vulnerable to compromised mental health6,7. Farming can be stressful, characterized for some by physical demands, long work hours, high debt load, and the need to cope with the unpredictability of weather and other environmental concerns. Farming is an occupation in which the workplace typically overlaps with a residential environment; accordingly, family members of farmers may have increased exposure to occupation-related stressors8.
Despite some attention paid to farm stress in the popular press9, recent Canadian research examining the mental wellbeing of farming populations relative to other rural dwellers is sparse. International research on the topic has shown inconsistent findings10,11 and has mainly focused on men12. A further limitation is the narrow range of mental health indicators typically considered, with depression or psychological distress being the most common. However, sex/gender may influence the manifestation of life strains, with men, on average, more likely to exhibit externalizing symptoms (eg alcohol misuse) and women internalizing symptoms (eg depressive symptoms)13; this makes it important for research to include mental health measures that can capture this diversity in expression. One type of alcohol misuse, binge drinking, is becoming increasingly prevalent among Canadian adults14, and is associated with numerous hazardous personal and social consequences15.
The objectives of the present study were to examine the mental health status and correlates of mental health among rural Saskatchewan women and men with farm/non-farm residence as the primary exposure of interest and depression and binge drinking as indicators of mental health.
Methods
Design and sample
The present study is set in Saskatchewan, a western Canadian province with a population of approximately 1 million people16. In 2016, 8.8% of the Saskatchewan population were farmers, compared to the national average of 1.7%. The majority of Saskatchewan farms produce grain and oil seed17. The data source for this study was the Saskatchewan Rural Health Study (SRHS). The rural population for the SRHS was defined as those persons ‘living in towns and municipalities outside the commuting zone of larger urban centers with a population of 10,000 or more’. The detailed methods for Phase 1 (2010)18,19 and Phase 2 (2014)20 of the study have been published previously. The study base consisted of tax-paying households located in rural municipalities (RMs) and small towns situated in one of four geographical quadrants (south-east, south-west, north-east and north-west) in the southern half of Saskatchewan19. The local councils for the vast majority of these communities (32/36 RMs and 15/16 towns) provided mailing addresses.
Dillman’s method of collecting data, which involves a series of mail contacts with all prospective participants, was utilized to recruit study participants aged 18 years or more21. A key informant in each household was asked to provide household-level information and individual information for each adult living in the household19. The questionnaire included questions on sociodemographics, health status and respiratory health-related exposures. Of the 11 004 eligible addresses, responses were obtained from 4624 households, representing 8261 individuals. In order to maintain a high retention rate for the next study phase, various knowledge translations activities were employed to remain in touch with the study participants and included regular local newsletters/newspaper articles and the presentation of results at local council meetings.
Phase 2 of the SRHS, which provides the data for the present study, was conducted in 2014 and consisted of mailed questionnaires to individuals who participated in the 2010 baseline survey20. Variables measuring depression and stress were added to this phase 2 survey. Initial mailing was done for 4454 households due to 170 households being lost to follow-up after baseline knowledge translation mailings were returned to sender. In the follow-up survey, questionnaires were returned from 2797 households, consisting of 4867 individuals (including 126 new individuals who did not participate in the baseline survey). For the present study, students and retirees were excluded, resulting in a sample size of 3401 individuals.
Measures
Dependent variables: Two indicators of mental health status were used as dependent variables. Depression was measured dichotomously (yes, no) by the question ‘Has a doctor or primary care giver ever said you have … depression?’. Binge drinking behavior (yes/no) was assessed with the question ‘How often in the past 12 months have you had five or more alcoholic drinks on one occasion?’(never, less than once/month, once/month, 2–3 times/month, once/week, more than once/week). Participants who indicated consuming five or more alcoholic drinks at least once a month were categorized as having engaged in binge drinking.
Independent variables: Location of residence (farm/non-farm) was based on answers to the question ‘Where is your home located?’ with the options of ‘farm’, ‘in town’ or ‘acreage’; town and acreage responses were combined to create a non-farm category.
In addition to sex/gender, demographic variables included partner status (partnered: married/common-law; non-partnered: single/separated/divorced/widowed) and age (18–54 years, 55–64 years, ≥65 years). Regarding age, the sample skewed towards older ages, which prevented the examination of younger people (eg 20–30 years) as a distinct group. Also included was a measure of whether household members had access to a regular family doctor or nurse practitioner (yes/no), given that one of the dependent variables (depression) required contact with the healthcare system.
Four variables were used to assess stressors. General life stress was measured by responses to the question ‘Thinking about the amount of stress in your life, would you say most days are: not at all stressful, very stressful, a bit stressful, quite stressful or very stressful?’. The variable was normally distributed and therefore used in its continuous form. Financial strain was a categorical variable assessed on the basis of participants’ response to the question ‘At the end of the month, do you have some money left over, just enough, or not enough?’. Included as physical stressors were two variables reflecting the presence of chronic conditions (none, one condition, two or more conditions) and occurrence of injury. The chronic condition variable was based on participants’ response (yes/no) to the question of whether they had ever been diagnosed with diabetes, heart problems, stroke, cancer, chronic bronchitis, chronic obstructive pulmonary disease, emphysema, sleep apnea or tuberculosis. Occurrence of injury was assessed by the question (yes/no) ‘During the past 12 months, were you seen by a doctor or other primary care giver for an injury?’.
Resources were measured with three variables. Household income (less than C$20,000, C$20,000–C$59 999, C$60,000 or more) was based on participants’ estimate of their total income, before taxes and deductions, of all household members in the past year. Education of the respondent was measured with three categories: less than secondary school, secondary school graduate and post-secondary graduate. Community social support was measured by the question ‘How well do you feel like you are generally supported (socially, emotionally, medically, etc.) by your community?’. Participants were asked to mark their response along a 50 mm line, anchored between ‘no support’ and ‘extremely supported’. Participants’ markings were measured, converted into numerical values (out of 100), and then categorized into tertiles: ‘low support’, ‘medium support’ and ‘high support’.
Analyses
Bivariate and multivariable models were constructed separately for women and men to better investigate whether exposure-mental health associations varied by sex/gender. Initial χ2 analyses examined the distribution of study variables according to farm/non-farm residence within each gender (ie farm women v non-farm women; farm men v non-farm men). Multiple logistic regression analyses were then conducted with independent variables entered in a series of blocks: model 1 – farm/non-farm residence; model 2: demographics and healthcare access; model 3: stressors (general life stress, financial strain, chronic conditions, injury); and model 4: resources (income, education, social support). In model 5, two-way interaction terms between farm/non-farm residence and each exposure were entered into the full model. A variable was retained in the final model if it was statistically significantly associated with the outcome, the main effect of a statistically significant interaction, theoretically important, or if its removal substantially impacted the coefficients of other variables in the model. Only the final logistic regression models are reported here; results based on the incremental addition of variable blocks (models 1–5) are available from the corresponding author upon request. For all logistic regression analyses, generalized estimating equations were utilized to account for household clustering. Statistical analyses were conducted using the Statistical Package for the Social Sciences v21 (IBM; http://www.spss.com) and Statistical Analytical Software v9.02 (SAS Institution; http://www.sas.com). To obtain odds ratio estimates of simple effects within a statistically significant interaction, the LSMEANS statement in PROC GENMOD was used.
Ethics approval
The study was approved by the Biomedical Research Ethics Board of the University of Saskatchewan (BIO #09-56).
Results
The sample consisted of 1701 women (47.8% farm) and 1700 men (53.3% farm). The average age of women and men was 55 years (standard deviation (SD)=12) and 57 years (SD=13), respectively. Table 1 shows the distribution of study variables stratified by farm/non-farm residence, separately for women and men. Among women, a greater proportion of farm than non-farm residents were older, partnered and in the highest household income category. No farm/non-farm differences in women emerged for healthcare access, life stress, financial strain, chronic conditions, injury, educational attainment or social support. Among men, higher percentages of farm than non-farm residents were older and had a secondary school education or less. Farm and non-farm men did not differ in partner status, healthcare access, life stress, financial strain, chronic conditions, injury, income or social support. For both women and men, non-farm residents had a higher prevalence of depression and binge drinking than farm residents.
Table 2 shows the results of the multivariable final models for women, first for depression and then for binge drinking. Regarding depression, there was a statistically significant interaction between farm/non-farm residence and chronic conditions: non-farm women had a higher likelihood of depression compared to farm women only among those with two or more chronic conditions. In addition, several statistically significant main effects were observed, with a higher likelihood of depression associated with younger age (18–54 v ≥65 years), greater life stress, not having enough money at the end of the month (compared to some money) and low social support (compared to high). An increased likelihood of binge drinking in women was associated with non-farm residence, younger age, not having regular access to a healthcare professional, and secondary school educational attainment (compared to post-secondary). There were no statistically significant interactions.
Table 3 shows the results of the multivariable final models for depression and binge drinking among men. A statistically significant interaction emerged for depression, with a greater likelihood of depression among non-farm than farm men only observed among those with a secondary school education. The following variables were associated with increased depression in men: younger age (18–54 v ≥65 years), being unpartnered (compared to partnered), greater life stress, and having two or more chronic conditions (compared to none). Similar to women, binge drinking was significantly elevated in non-farm men compared to farm men. In addition to non-farm residence, binge drinking in men was associated with younger age, having just enough money left over at the end of the month (compared to some money) and higher household income. No statistically significant interactions emerged.
Table 1: Distribution of study exposures by farm/non-farm residence, stratified by gender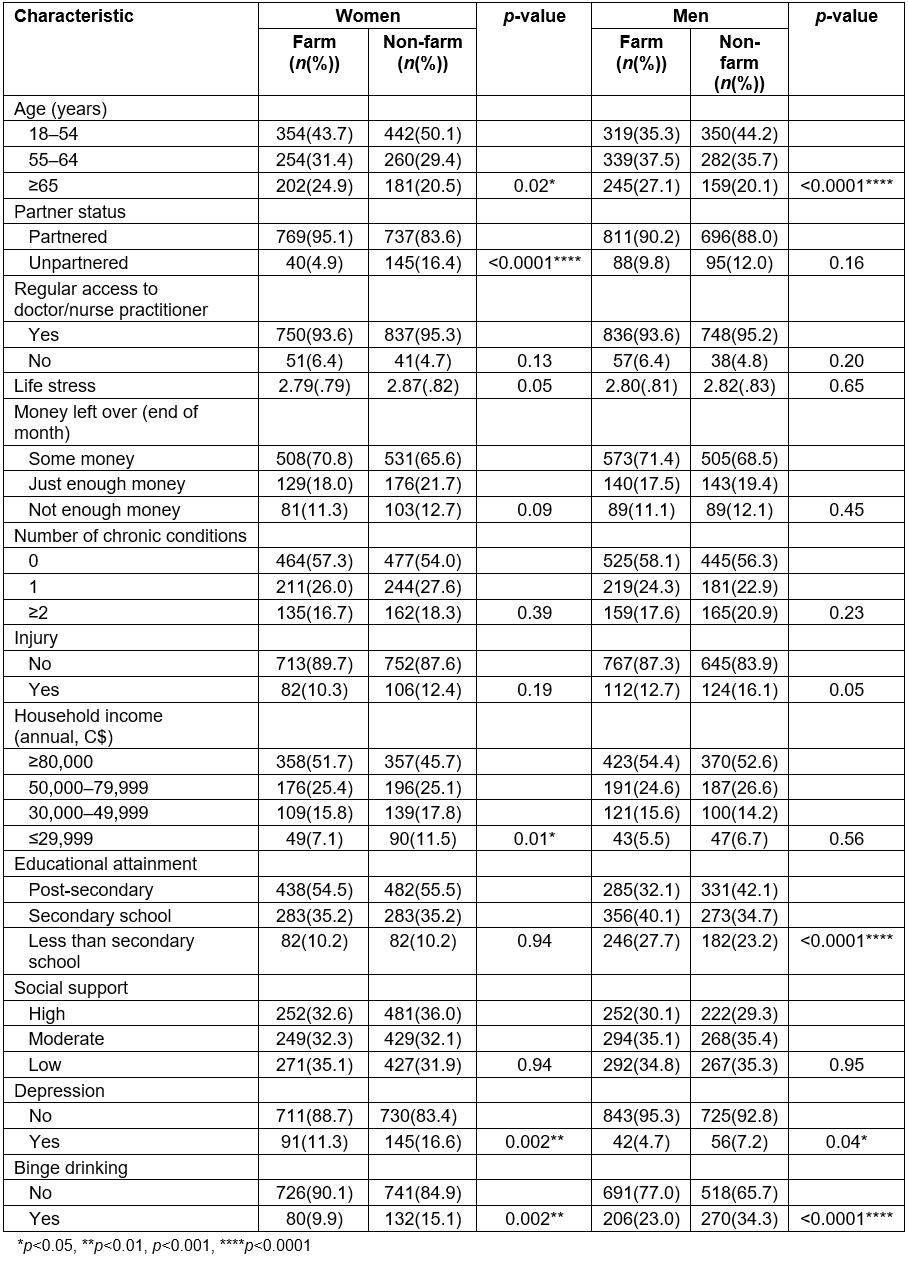
Table 2: Odds ratios and 95% confidence intervals for multivariable adjusted final models for depression and binge drinking in women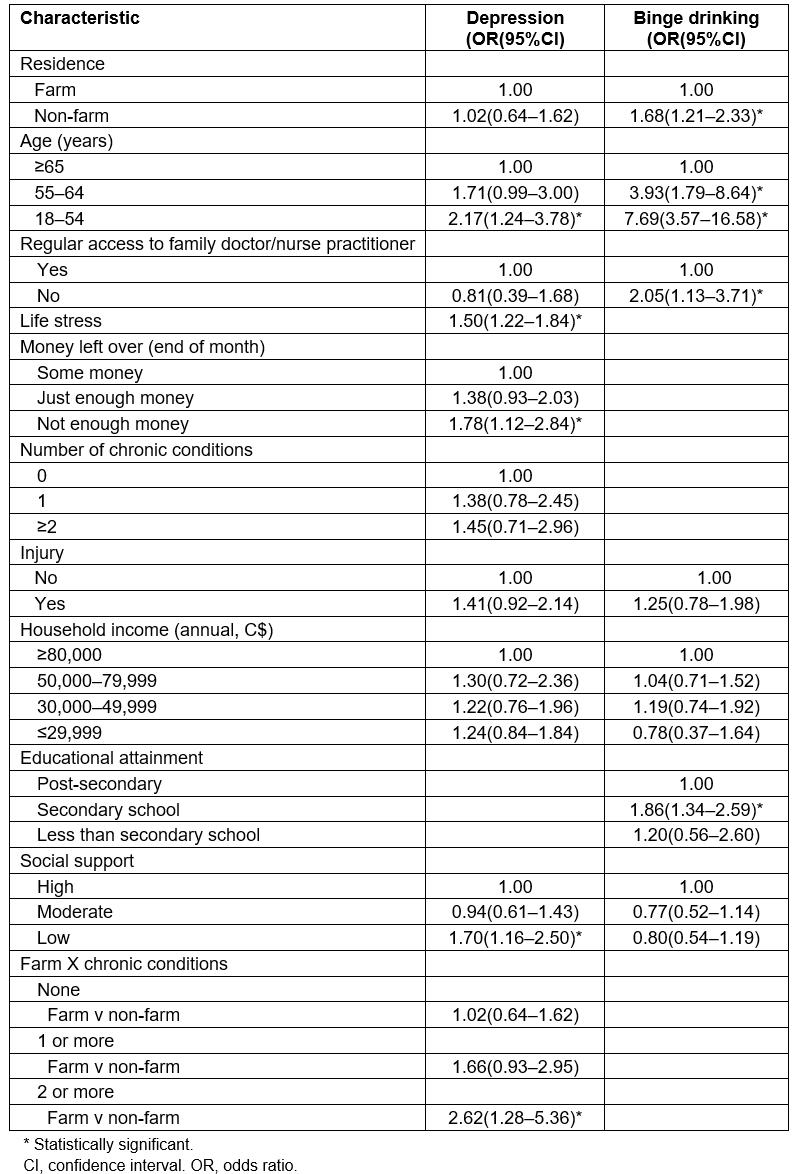
Table 3: Odds ratios and 95% confidence intervals for multivariable adjusted final models for depression and binge drinking in men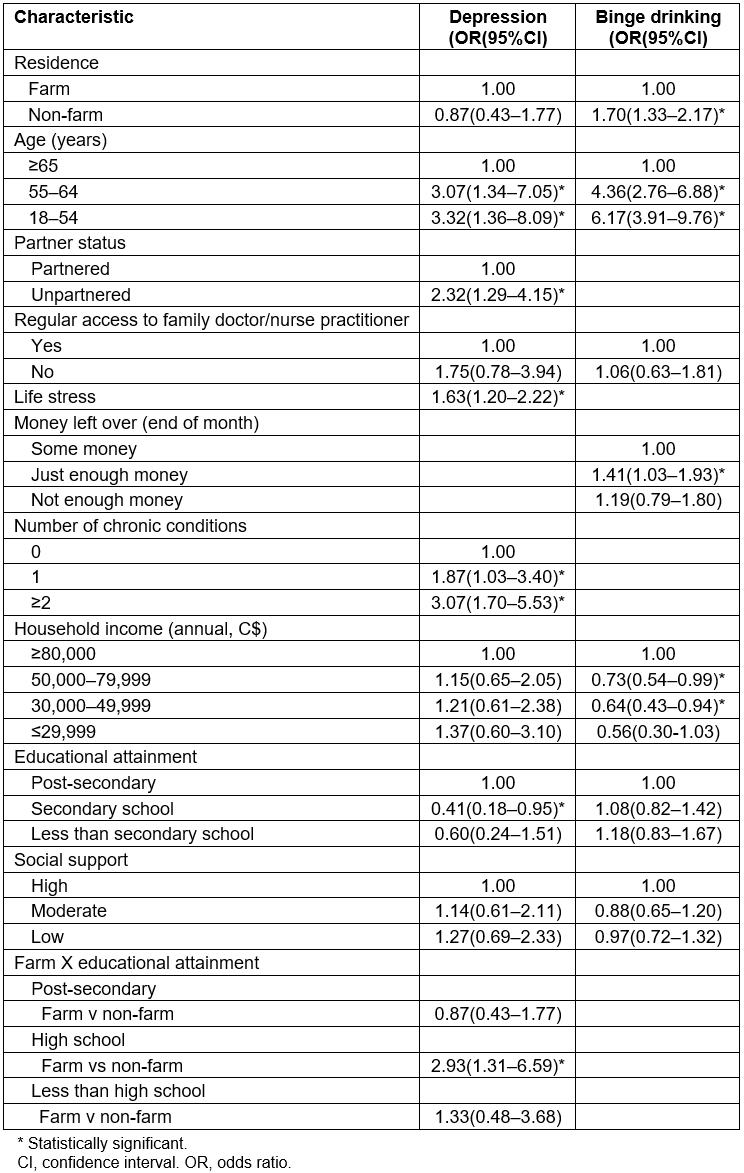
Discussion
The objective of the present study was to examine the correlates of mental health among rural Saskatchewan women and men, positioning farm/non-farm status as a main explanatory variable and depression and binge drinking as measures of mental health. For depression, although the unadjusted results suggested an overall detrimental association with non-farm status, multivariable analysis identified more nuanced findings, with an elevated likelihood of depression observed among non-farm women with two or more chronic conditions and among non-farm men with a secondary school education. The likelihood of binge drinking was greater in non-farm women and men compared to their farm counterparts and remained so in adjusted analyses.
Depression
Canadian research examining the mental wellbeing of farming populations relative to other rural dwellers is scarce. International research comparing farm and non-farm populations in depression and related symptomatology has provided mixed findings, with some showing no difference between groups 10,22, greater depression among farm men than non-farm men but no difference between women11,23, or differences/similarities dependent upon the particular mental health measure used11,12. In the present study, farm/non-farm status was related to depression but only under particular circumstances, which in turn differed by gender. In women, non-farm residents with two or more chronic conditions reported more depression than their farm counterparts; among those with no chronic conditions or one chronic condition, no association between farm/non-farm status and depression emerged. One possibility is that, due to selection, farming women who experienced more severe chronic conditions may have left farming in favor of less physically demanding employment in town. Some research suggests that severity of chronic conditions (unmeasured in the present study), rather than the number of conditions, may be more strongly associated with mental health24. However, if the selection of women with more severe chronic conditions out of farming is an explanation, why this same effect would not emerge in men is unclear. For men in this study, independent of farm/non-farm status, the presence of chronic disease was associated with an increased likelihood of depression. Associations between chronic physical illness and mental morbidity, including depression, have been extensively reported in previous research25,26.
Farm/non-farm status was associated with depression for men in this study, but only in one particular subgroup; that is, non-farm men with secondary school education reported greater depression compared to their farm counterparts; among men with post-secondary or a less than secondary school education, no association by farm/non-farm status was detected. Higher education is generally considered as an important resource for mental health via various pathways, including greater employment opportunities, more favorable work conditions and higher income27. That said, a university degree is not generally viewed as a requirement for farming, thus a secondary school education among non-farm men might be considered as more of an impediment to attaining the health-enhancing resources already described. If so, however, why this association was not also observed among those with less than secondary school education is difficult to explain and requires further investigation.
The remaining correlates of depression observed in this study were quite consistent with previous research in rural populations, including younger age22,28, being non-partnered28, higher stress10,12,29, greater financial strain30 and lower social support12,22,28,30. Other than the nuanced patterns observed in relation to farm/non-farm status described, the predictors of depression were generally similar for men and women in this study, although some associations observed in unadjusted analysis (data not shown) were not maintained at the multivariable stage, such as partner status (women) and financial strain/social support (men). Consistent with previous research13, it was also found that women were significantly more likely than men to report a diagnosis of depression (odds ratio (OR)=2.57; 95% confidence interval (CI) 1.76–3.75), an association independent of farm/non-farm status (data not shown).
Binge drinking
Binge drinking in the present study was more prevalent in non-farm women and men compared to their farm counterparts. The authors could find no previous Canadian research comparing farming and non-farming populations in binge drinking; international research has shown inconsistent results, likely due in part to the diversity of alcohol measures used. In studies from Australia and the USA, no significant differences were reported by farm/non-farm status in binge drinking31 or harmful alcohol use32, respectively. In contrast, Jarman et al reported higher prevalences of frequent binge drinking among farm or ranch owners/employees compared to many other occupations in North Dakota33. In another Australian study, non-farm women reported significantly higher daily consumption levels than farm women, although no differences were found between farm and non-farm men on a variety of alcohol-related parameters34. Several studies from Sweden using alcohol-related hospitalizations and mortality as outcomes have reported lower rates among farmers compared to rural non-farming men35,36.
What might account for the higher likelihood of binge drinking in non-farm compared to farm women and men in the present study? The selection of heavier drinkers outside of farming cannot be ruled out, given the cross-sectional design of this study. Non-farm residents were younger than farm residents in this study, and of a younger age, although one of the strongest correlates of binge drinking in the literature, including in rural settings37,38, was accounted for in the multivariable analysis. Easier access to alcohol for non-farm compared to farm residents may be a factor; some research indicates that, at least in urban settings, living closer to an alcohol outlet is associated with greater risk of excessive drinking39. It is important to note that although the non-farm group was a combination of acreage/town dwellers, the vast majority resided in town. Living farther from drinking establishments, farm residents may be more concerned about drinking and driving than non-farm residents, which could serve as a deterrent to more extreme alcohol use. Binge drinking behavior may also be related to occupation; that is, the demands of farming (eg early mornings, long hours) may make it incompatible with engaging in more extreme alcohol use. Conversely, non-farm dwellers may be more likely to be employed in occupations in which alcohol use is more prevalent, such as in the service industry; construction; and oil, gas and mining occupations40. Unfortunately, the lack of occupation information in the present study prevents further evaluation of this hypothesis. Additional research is required to determine whether observed differences in binge drinking are attributable to occupation, individual characteristics (eg demographic, personality related) and/or community-level determinants that may be differentially distributed by farm/non-farm status. Although not specifically looking at farm/non-farm residence, the results of a recent study set in rural Australia suggest that factors at the individual level (eg age, male sex) may be more important predictors of hazardous alcohol use than those at the area level37. Consistent with this research, in addition to younger age, the present study found that men were significantly more likely than women to report binge drinking (OR=2.70; 95%CI 2.26–3.22), an association that was independent of farm/non-farm status (data not shown).
Other than non-farm residence and younger age, the remaining factors associated with binge drinking in this study differed for women and men. Among women, not having access to a regular family doctor/nurse practitioner was associated with an increased odds of binge drinking (and unassociated in men). One challenge to interpreting this finding is the imprecise wording of the question posed to participants: ‘Do you and your family members in your household have access to a regular family doctor or nurse practitioner?’ Assuming the female participants answered the question with themselves in mind, perhaps women who have regular access to a doctor are more likely than those who don’t to have problematic alcohol use identified, and, based on physician intervention, adjust their drinking behavior. Although there is some support for the efficacy of brief interventions for heavy drinking in primary care settings41, screening for alcohol misuse does not routinely take place in Canada42. Alternatively, heavy drinkers may be less likely than non-drinkers to engage in a variety of preventive health practices including regular check-ups with their family physician43.
The socioeconomic patterning of binge drinking in this study also varied inconsistently between and among women and men. In men, binge drinking was associated with higher household income but was not related to educational attainment; in women, binge drinking was linked to lower education but was unassociated with income. These finding are not that incompatible with the broader research literature, which points to a complicated relationship between alcohol misuse and socioeconomic circumstances44. In Canadian general population samples, men and women with lower income are, on average, less likely to binge drink than those with higher income, perhaps because they have less discretionary money to spend on alcohol and social activities45. However, the opposite socioeconomic pattern occurs when alcohol-related harms are considered, with lower income adults experiencing more than double the rate of hospitalization due to alcohol use compared to their higher income counterparts46. Previous research examining the relationship between education and problematic alcohol use have not produced entirely consistent results47, although a slight preponderance of evidence suggests a higher prevalence of binge drinking among Canadians with lower education45.
Strengths and limitations
The present study had a number of strengths, including a large sample size, which allowed the authors to examine a broad array of factors potentially associated with mental health, to control for confounders, and to test for potential interactions with farm/non-farm status. Limitations were also present. The number of statistical tests conducted may have inflated the probability of type II errors. All measures were based on self-report, including indicators of mental health, which, due to social desirability, may have resulted in depression and binge drinking being underreported. The depression measure was based on a single item and required contact with a health professional; although some research suggests that this measure is a reasonable proxy for a diagnosis of depression based on clinical data48,49, the validity of results would have been enhanced had the authors included a more comprehensive measure of depression, independent of health service use. Binge drinking was operationalized in this study as consuming five or more alcoholic drinks at least once a month; however, four drinks may be a more appropriate cut-off for women14; thus, the prevalence of binge drinking among women in this study was likely underestimated. Given the older average age of participants in this study, the use of other measures of alcohol misuse, in addition to binge drinking, may have been informative. Measurement limitations were also present with respect to the primary exposure of interest, farm/non-farm status. Intended as a proxy for involvement in farming, some misclassification is likely, as some farm residents may not be farming and, conversely, some non-farm residents may own farms or be employed as farm workers. Also lacking is information on multiple job holders; that is, many farmers may work off the farm as well, including women, who in addition typically have primary responsibility for housework and caregiving.
Regarding design, the cross-sectional nature of the data limits the ability to infer causal relationships between exposures and mental health indicators. A healthy worker effect50 is a possible explanation of the lower prevalence of binge drinking in farm compared to non-farm populations and among the subgroups of farm women and men with a lower likelihood of depression. That is, persons having mental health/drinking problems may avoid farming in the first place, or are forced to leave farming for other occupations. On the other hand, some research suggests that farmers are no more likely than those in other occupations to leave their work for mental health reasons51.
The original (phase 1 of the SRHS) response rate was 42%, which may have introduced selection bias into the study18. In phase 2, 63% of the original baseline survey responded to the follow-up questionnaire; drop-outs were more likely to be non-farm residents, have lower socioeconomic status (educational attainment) and more likely to have reported various respiratory outcomes20. Unfortunately, mental health information was not collected in the baseline survey. If the non-farm people who did not respond were also more likely to be binge drinkers and/or be depressed, this may have resulted in an underestimation of the effect between the primary exposure (farm/non-farm) and study outcomes. Finally, just over 97% of the sample indicated being of Caucasian origin, thus preventing the authors from examining ethnicity as a correlate of depression and binge drinking.
Conclusion
Depression and binge drinking represent serious health concerns for adults in Canada. The present study is one of very few recently published quantitative studies of mental health determinants set in rural Canada. The findings of this study suggest that non-farm dwellers in rural Saskatchewan may be more vulnerable to compromised mental health than their farming counterparts. For both women and men, non-farm residence was associated with a higher odds of binge drinking. Further, two subgroups of non-farm residents, women with two or more chronic conditions and men with a secondary school education, were at greater risk of depression. Additional research employing a longitudinal design and enhanced measurement is required to confirm or refute these findings.
Acknowledgements
The Saskatchewan Rural Health Study Team consists of James Dosman, MD (Designated Principal Investigator, University of Saskatchewan, Saskatoon); Dr Punam Pahwa, PhD (Co-principal Investigator, University of Saskatchewan, Saskatoon); Dr John Gordon, PhD (Co-principal Investigator, University of Saskatchewan, Saskatoon); Yue Chen, PhD (University of Ottawa, Ottawa); Roland Dyck, MD (University of Saskatchewan, Saskatoon); Louise Hagel (Project Manager, University of Saskatchewan, Saskatoon); Bonnie Janzen, PhD (University of Saskatchewan, Saskatoon); Chandima Karunanayake, PhD (University of Saskatchewan, Saskatoon); Shelley Kirychuk, PhD (University of Saskatchewan, Saskatoon); Niels Koehncke, MD (University of Saskatchewan, Saskatoon); Joshua Lawson, PhD (University of Saskatchewan, Saskatoon); William Pickett, PhD (Queen’s University, Kingston); Roger Pitbaldo, PhD (Professor Emeritus, Laurentian University, Sudbury); Donna Rennie, RN, PhD (University of Saskatchewan, Saskatoon); Ambikaipakan Senthilselvan, PhD (University of Alberta, Edmonton). We are grateful for the contributions of the rural municipality administrators and the community leaders of the towns included in the study that facilitated access to the study populations and to all of participants who donated their time to complete and return the survey.

