Introduction
Emergency departments (EDs) offer a form of first-contact, primary medical care focused on managing a range of urgent, acute illnesses and injuries1-3. They are not intended for non-urgent primary care type problems (patients not arriving by ambulance or who are self-referred and have a medical consultation time of less than 60 minutes)3-5. However, attendances for these presentations at EDs are accepted even though care could be managed in general practice without adverse outcomes3,6-11. Indeed, many primary-care-type presentations may be managed better by community-based services, including outpatient clinics, general practices and mobile centres12-14. Further, ED utilisation presentations that could be managed elsewhere increase ED congestion, the cost of care and fragmentation of care15-17.
Much is known about patient perspectives on the choice of which primary medical care service to attend. Several competing factors may influence health-seeking behaviour, such as financial status, lifestyle and sociodemographic profile18. The availability, accessibility and affordability of community-based services can significantly impact the utilisation of ED services6. When services cannot be accessed when needed or are expensive, people choose hospital EDs to meet their needs19. People with chronic and complex health conditions often become frequent users of hospital care in the absence of well-coordinated, community-based care20,21. The resulting uncoordinated health service provision incurs higher costs, consumes ED resources and often does not adequately address important underlying social and health issues22.
The benefits of general practitioner (GP) services can only be fully realised if the care is timely, available, accessible and appropriate. Evidence suggests that, if primary services could function to address people’s needs, then the use of EDs would more closely match the acute role for which they are designed23. It is argued that improvements in the design and availability of GP services need to be supported by more concerted efforts to raise public awareness that alternative primary care solutions exist within the community that they can efficiently and effectively utilise24. For example, opening up a parallel GP ‘urgent care centres after hours (evenings, weekends and holidays) can significantly reduce ED presentations25. Similarly, incentivising GPs to improve access to after-hours care reduces some less urgent visits to the ED26.
Despite the widespread acknowledgement of negative consequences of the less appropriate use of ED for primary-care-type presentation, causes of such visits are not clearly understood27, especially in rural and remote areas. While the ED workload and patient perspectives have been explored, less is known about healthcare providers' perspectives. This article reports a study of healthcare providers' perspectives in the ED, private general practices, and an Aboriginal Community Controlled Health Organisation (ACCHO) in a remote Australian city where ED workload and patient perceptions have also been researched28.
Methods
Context and settingHealthcare services in Australia are provided through a complex combination of national and state-funded agencies that operate at state, regional and local levels. Further, the combination differs a little by state. Hospitals in general are funded by both the federal and state governments and managed by state governments. Through different service and funding models, the federal government funds general practice and ACCHOs. In rural Queensland, state-run public hospitals also contribute to primary care medical services through small hospitals offering ‘urgent’ and some acute care services, acting as low-volume EDs that stabilise and transfer patients to larger hospitals. In some communities, these services are provided by the same doctors (rural generalists and GPs) who staff community GP clinics that the federal government funds. The federally funded public health networks offer local coordination of primary care services across funding sources, and jurisdictional management.
The city of Mount Isa is located in remote Queensland, 883 km from the nearest major city, Townsville. It was established because of the vast mineral deposits in the area, and the local mining industry produces lead, copper, silver and zinc. Mount Isa has a population of approximately 22 000, which includes a significant Aboriginal and Torres Strait Islander population29. GP services are available between 7 am and 8 pm on Monday to Friday and between 9 am and 5 pm on weekends, at three practices. An ACCHO offers primary care services from 8 am to 5 pm on four days of the week. Mount Isa Base Hospital is a medium-sized (80 beds) regional hospital with a 24-hour ED that manages approximately 30 000 presentations per annum30.
Methodology
A qualitative approach used focus groups and semi-structured interviews to explore health staff perceptions about factors associated with ED presentations for primary-care-type presentations.
Participants
Potential participants were recruited by an email invitation describing the purpose of the project and the expectation in time commitment should they decide to participate. Each respondent received a follow-up phone call to arrange a meeting, and this was confirmed by email. Privacy and confidentiality were maintained by referring to participants by ID code. Three focus groups were held for 14 respondents, and individual semi-structured interviews were offered for those who could not attend the focus group meetings. The following questions and probes were used in both focus group and individual interview processes and were developed with the assistance of the project steering group, which included senior medical, nursing and management staff:
- How often are you involved in providing care for patients who come to the ED for primary-care-type presentations?
- Why do you think patients come to the ED for primary care rather than to a GP or medical centre?
- What are your thoughts on the strategies specific to primary care services that may help to overcome these problems
- What are your thoughts on strategies specific to the ED that need to be implemented to reduce utilisation of ED for primary care presentations?
- Would you like to add anything else?
Formal written consent was obtained. The recruitment of healthcare providers was discontinued when thematic saturation was achieved. Each focus group session and the individual interview lasted approximately 30–45 minutes. All discussions and interviews were recorded and transcribed verbatim.
Analysis
All de-identified interview transcripts were entered into the NVivo qualitative data analysis software v10 (QSR International Pty Ltd; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home). The data analysis was guided by Braun and Clarke’s approach for inductive thematic analysis31. Line-by-line analysis was conducted, with data coded for similarity and relevance to the research questions. Primary codes were developed (AN, YF), and codes were cross-checked by two other researchers (SK, IS) for validity. There was a difference of opinion about text elements; the codes and text were discussed until consensus was reached. Memos and field notes were consulted, and primary codes were aggregated into larger themes or axial codes. A model was developed to represent these axial codes. Data were cross-checked to ensure that the codes accurately represented the emergent themes. Overarching themes were agreed upon, and these themes were used to go back to the literature to confirm the findings and their theoretical relevance in the broader health and health services literature.
The use of narratives and participants' quotes has been minimised to promote the anonymity of the participants, which is particularly critical when conducting a study in a remote health precinct.
Ethics approval
This project was approved by Townsville Hospital and Health Service human research ethics committee (HREC/17/QTHS/73). Western Queensland Primary Health Network commissioned the study through James Cook University. Interview participants gave written informed consent.
Results
Focus groups were conducted with ED staff, GPs, Queensland Health Nurse Navigators, Aboriginal and Torres Strait Islander Health Workers and Indigenous Liaison Officers. Three focus groups and 10 one-on-one interviews were conducted. There were five GPs in the first focus group, four ED practitioners in the second focus group, and the third group included four Aboriginal and Torres Strait Islander Health Workers and one Aboriginal and Torres Strait Islander Liaison Officer. The plan was to undertake a fourth focus group with the ED staff but, due to availability issues, individual interviews were conducted instead. In total, the qualitative data comprised the views of 24 healthcare providers.
The analysis identified three themes: access and logistical barriers, rational decision-making and self-perceived urgency (Table 1).
Table 1: Perceptions of healthcare providers on emergency department utilisation for primary-care-type presentations in Mount Isa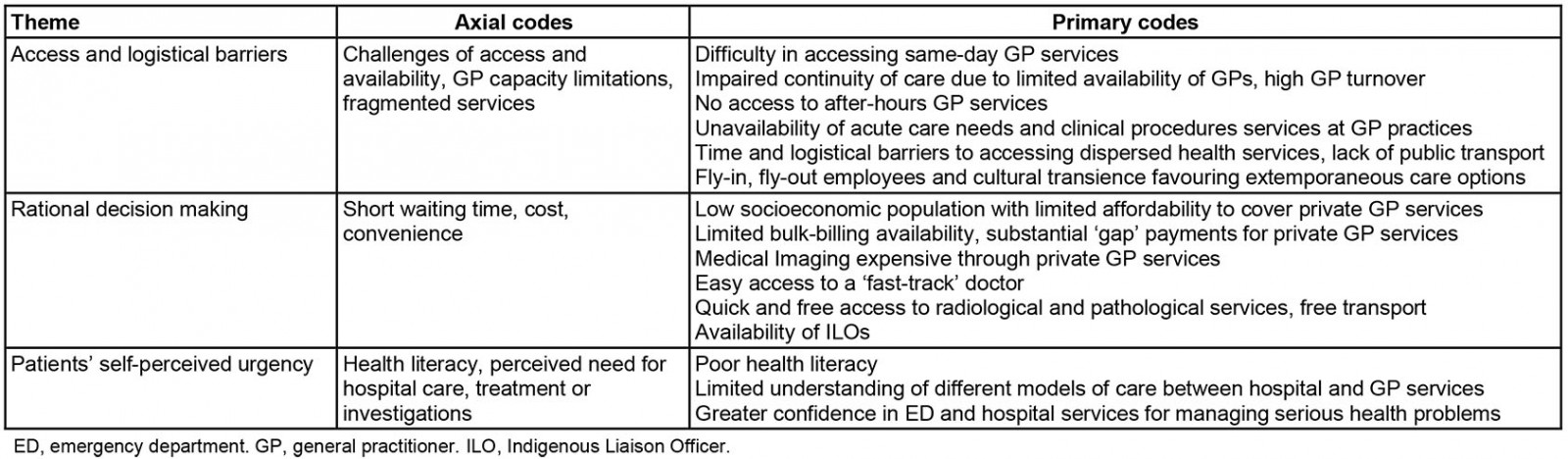
Access and logistical barriers
When reflecting on the factors influencing ED utilisation, providers frequently mentioned access and logistical issues. The general agreement was that many patients attending the ED needed to be redirected to GP services. GPs thought that some of their patients chose to attend ED rather than GP clinics. As one of the participants commented:
More of them (patients) than I would like [attend the ED] … particularly out of hours. (ED provider)
The participants discussed the absence of a 24-hour GP service. The three private GP clinics do not offer either sole or collaborative after-hours services. The ED provides walk-in medical services that do not require an appointment, an attractive option for some patients. There were some differences in perception between GPs and ED staff, with GPs believing that they were available if regular patients called, questioning whether patients attending the ED had tried to obtain an appointment. On the other hand, the ED staff and Nurse Navigator participants reported that many patients claimed they could not obtain appointments, particularly for families, visitors and new residents, with appointments booked out for several weeks ahead and minimal same-day availability.
The role of the ED in providing a second opinion was regarded as a valid reason for presentations in a small community. Furthermore, there was agreement that the ED ‘fast-track’ service was efficient – patients triaged as category 4 and 5 were seen by a senior medical officer to rule out more urgent/serious problems. While this managed patient load more rapidly, it was so efficient that it potentially reinforced future ED presentations for less urgent presentations. Further, the ability of the ED to offer a ‘one-stop-shop’ service that included consultation, investigations and treatment, all at no direct cost, was another unintended perverse incentive. On the other hand, some procedures, such as catheterisations, are not available in GP clinics, so the ED fills an important service gap.
An important association seemed to exist between patients attending the ED and having a regular GP. Regular GP patients were less likely to attend the ED, suggesting that improved awareness of local services may reduce ED attendance for GP-type presentations. All participants shared concerns about the potential for fragmented care, particularly for those with longer term or complex problems, disabilities and vulnerabilities.
Options for improving services included co-location of joint extended-hour GP services adjacent to the ED. An alternate approach was to stop using the ‘fast track’ and refer those appropriate patients directly to the GP, requiring increased availability of GP services. In addition, the option of a mobile clinic to support home-based primary care was suggested with support from the multidisciplinary team. Further suggestions included developing an Aboriginal and Torres Strait Islander super clinic with transport support and more access to walk-in clinics with flexible primary health care options such as mobile GP services.
Rational decision making
Participants perceived that going to the ED patients was rational decision making, seeking optimal and prompt healthcare services based on local access, availability and affordability. Despite many ED attendees being employed, the hospital health professionals group perceived more patients had limited ability to pay for private GP services, including investigations, and limited transport options. Hence attending a private GP clinic was regarded as both less convenient and less affordable. The higher socioeconomic population may be less concerned about cost but still influenced by the convenience, rather than need, of an ED service that is always open, has short waiting times and provides timely investigations and treatments or medical certificates. These may be strong incentives that make the ED a preferred choice. GPs identified that patients find the coordinated ‘do it now’ ED approach (e.g. for blood tests, X-rays and referrals) reassuring, whereas the approach of primary care is less invasive, with fewer investigations, referrals (and therefore lower cost to the healthcare system) and based on more deliberate review over time. Some GPs believed that lack of engagement with patients might be a factor in why some patients presented to the ED:
… the [patients] that you just don't have enough time with and don't feel like you're across, I think they're the ones that tend to access it [ED] more. Yeah, the ones you don't have enough time with. (GP)
Patients’ self-perceived urgency
All healthcare providers acknowledged that the poor health literacy levels and a lack of understanding by some patients about the appropriate use of ED services compared to GP services significantly impact the care pathways chosen:
There are patients who think it's normal for them to present to the ED for their cold and coughs and UTIs [urinary tract infections] … they probably don't understand the health system … they've done it before … maybe the treatment and reception that they got in the ED was very receptive to their presentation and made it easier for them to present in the ED … which encouraged them to do that over and again … (GP)
An emphasis from all the participants was placed on the need for community-based education and awareness-raising on the intended roles of ED, GP and other primary healthcare services. This was further explored in regards to the fragmented and duplicated services across the North West region of Queensland. Targeted and sustained strategies to increase understanding of the role of primary care and the ED were identified.
Participants highlighted the need for improving communication and collaboration between the ED and the local primary health network by utilising a GP liaison role. The Aboriginal and Torres Strait Islander Health Worker and Indigenous Liaison Officer focus group reported that many Indigenous patients would attend the ED if they felt unwell:
… if they're sick, they want to go to the hospital. They know if they're sick. (Aboriginal and Torres Strait Islander Health Worker)
Participants in the Aboriginal and Torres Strait Islander Health Worker and Indigenous Liaison Officer focus group and the Nurse Navigator focus group felt that patients who did not prioritise their health have complex lives, and were not ready to engage in primary care, were frequent users of the ED.
Disagreement between views of ED and GP providers on ED utilisation for primary-care-type problems
The interviews also highlighted some similarities and differences in ED and GP providers (Table 2).
Both ED doctors and GPs agreed that pathways between general practice and the ED, referral both in and out, were poorly defined and required strategies to address this issue. While there was agreement that the local ED service was dealing with a disproportionally high number of clinical presentations that did not require the resources available at an ED, there was some disagreement among health professionals working in a range of primary healthcare services about the drivers of primary care presentations and how to address this.
The differences between ED and GP groups are perhaps the most intriguing. ED doctors saw themselves as mostly there for emergencies but dealt with whatever was presented, and they heard consistent reports from patients that no GP appointments were available. However, they regarded less urgent presentations as distractions from their main role. They discouraged ED follow-up for presentations and advised patients to see a GP, but had limited influence over future patient decisions.
Even though the number of GPs in the community was lower than the national average, at about 1 per 2000 population, there was resistance to increasing the number of GPs, particularly by establishing an all-direct-billing practice adjacent to the hospital. If implemented without broad support from the medical community, there were concerns that such a development may further disrupt the continuity of care, as this may involve a simple relocation of the ED ‘fast-track’ service that would not necessarily solve the problems of costly investigations and availability of appointments.
Table 2: Differences in perceptions of healthcare providers on emergency department utilisation for primary-care-type problems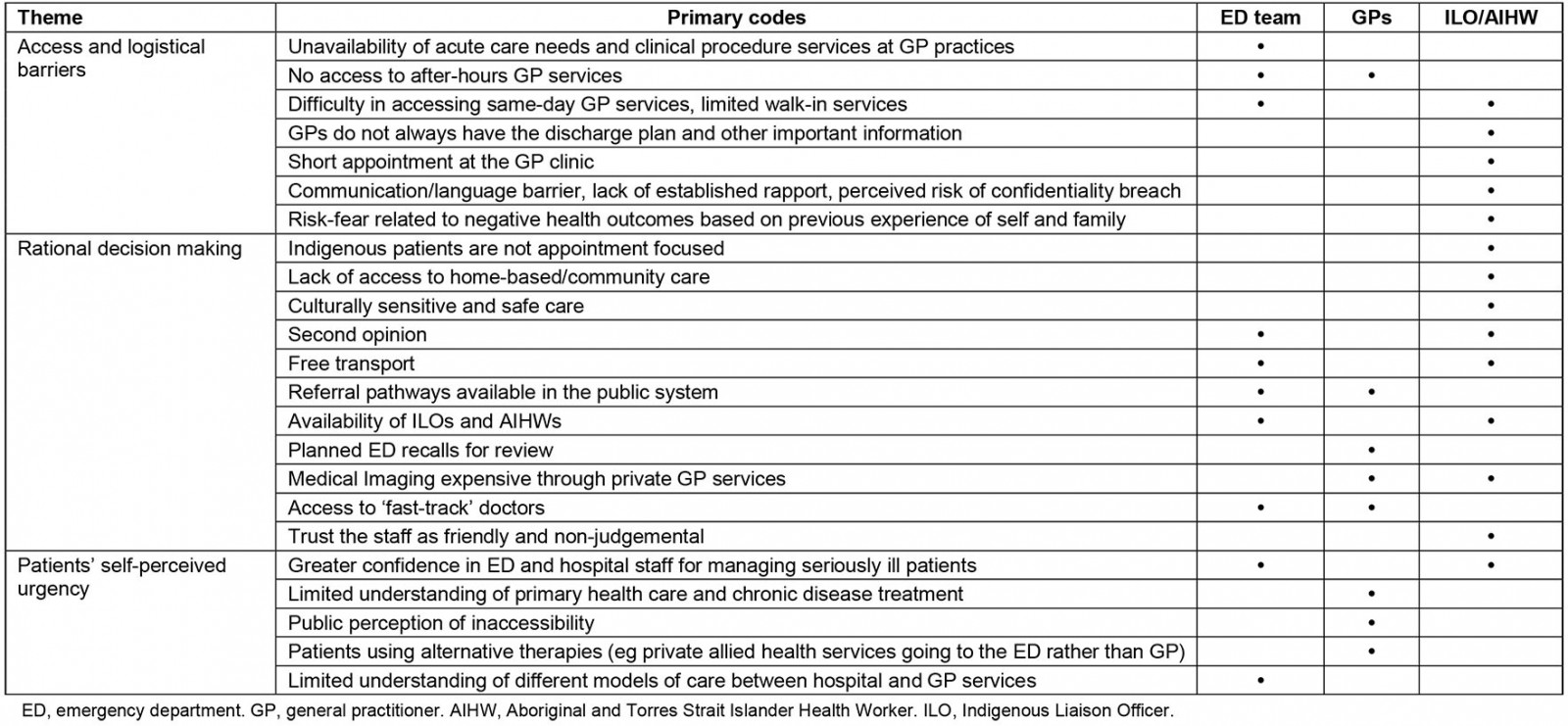
Discussion
This study increases understanding of the providers’ perspectives of ED use for primary-care-type presentations. Both ED doctors and GPs agree that pathways between general practice and the ED, referral both in and out, could be made clearer as, ideally, the two services are complementary rather than competitive. However, both recognised some uncertainty about how best to direct presentations that may sound appropriate for GP assessment but require more urgent investigation and management.
This work extends findings from the previous studies that have investigated the perspectives of only ED staff on the concept of ‘inappropriate’ ED attendances concerning large urban hospitals, such as in New Zealand32, Turkey33, Ireland34 and Iran35. The Irish study included the perspectives of paramedics bringing patients to EDs. The present study’s findings align broadly with these other studies but add the views of GPs and Aboriginal and Torres Strait Islander Health Workers, who provide alternative and complementary services. The context is also that of rural and remote Australia, where the proportion of Indigenous Australians is high, and the funding and configuration of healthcare services are different. Furthermore, for Indigenous Australians, access to Indigenous Liaison Officers who can provide emotional and cultural support and help with health literacy issues is a key factor in service access decision making36. The absence of Indigenous Liaison Officers in general practices may also contribute to ED utilisation.
One strategy to reduce ED utilisation for primary care issues may be effective workforce strategies that could support increasing the medical workforce, including sessional hospital appointments for rural generalists to increase the availability of GPs and the coordination of service provision across hospitals’ community boundaries37. These combined roles are regarded as more attractive to recent graduates, many of whom pass through the local hospital during training but observe that opportunities to continue practising an advanced skill are limited in the local hospital, which has adopted a ‘specialist-delivered’ model of care seen in larger urban centres.
Another important strategy is to address the cost and convenience of both consultations and investigations38. In the high cost environment of a remote community, most GP consultations and investigations ordered by GPs are charged at a higher rate than when ordered at a public hospital. The primary health network may have a role in negotiating or supporting a different fee structure to remove cost as a disincentive to attending GP clinics. Further, hospital-ordered investigations are often conducted at the time of the consultation at the same site, a much more convenient arrangement than in general practice. Another strategy may be to invest in a community education program to improve understanding of what each service can provide. However, until accessibility and affordability factors are addressed, this may be less likely to succeed, and many patients will continue to make what are to them quite reasonable choices.
The study offers views of a range of health professionals engaged in primary health care. The influence of context – location, demography and health service configuration – may be unique to this community, and convenience sampling limits the generalisability of findings across other Australian communities. Nevertheless, this research highlights opportunities for intervention to reduce ED utilisation for primary care presentations. Future research is required to evaluate interventions such as improving communication, information-sharing and coordination between ED and GP providers, a triage system that directs patients to the more appropriate service and clearer patient pathways for pre- and post-ED care.
Conclusion
In one large, remote mining community with a unique combination of population demographics and health service configuration, the challenges of managing emergency medicine attendances for problems that could be managed in general practice are similar to those reported elsewhere. This study shows that ED staff have similar perspectives to colleagues in ED departments serving larger populations, but adds the perspectives of GPs in both private practice and Indigenous medical services. A small proportion of patients whose presentations suggest suitability for GP management require more urgent management. There is scope to improve coordination of services across funding sources and jurisdictional differences. The present research highlights opportunities for intervention to reduce ED utilisation for primary-care-type problems. Future research should build on these findings, particularly the need for greater coordination between ED and GP providers for effective communication and information sharing to develop appropriate interventions and assess their effectiveness.
Acknowledgements
We are thankful to Professor Isabelle Skinner, Associate Professor Katie Panaretto, Rhonda Fleming and the staff at Mount Isa Hospital for their help and support with the project. The research team would like to thank all participants who generously shared their time and experiences with us.



