Introduction
Although many effective antihypertensive drugs are available, suboptimal blood pressure (BP) control remains a common challenge internationally1,2. In an effort to identify the reasons that explain the gap between evidence-based medicine and actual clinical practice, the investigation of patient knowledge and attitudes can provide a better understanding of possible patient-related barriers2-7. Investigating hypertension management from the patient perspective (‘through patients’ eyes’) can have a great impact on designing effective interventions aiming to improve medication adherence 4,6,8.
Treated but uncontrolled hypertension is a worldwide issue, so exploring the perspective of patients from different cultures and contexts could contribute to a more comprehensive understanding of issues associated with suboptimal medication adherence. However, studies looking into hypertension management ‘through patients’ eyes’ in Greek population are scarce, especially in primary healthcare settings4,9. According to the findings of a pilot study in general practice, patient satisfaction with BP management was found to not always reflect actual BP control, while some knowledge gaps possibly affecting patient compliance were identified9. Moreover, in a qualitative study in outpatient hypertension centers, patients had expressed concerns regarding the use of medicines and their adverse reactions, suggesting that a more personal relationship with the doctor could facilitate adherence to the treatment4. To the authors’ knowledge, there is no previous large-scale study addressing potential barriers of hypertension management among primary healthcare patients in a rural setting in Greece. The aim of this mixed-method, multi-centered study was to investigate patients’ knowledge and attitudes towards hypertension management and their perceived level of control in order to identify possible barriers in effective BP control in general practice.
Methods
Study design
An advertisement of the study was posted on the website of the Hellenic Society of Greek General Practice, describing its aim and inviting general practitioners (GPs) to join the research group. Twelve GPs responded and participated as researchers in their own rural practices, situated in five different prefectures of Greece, from the regions of Central Greece, Thessaly, Macedonia and Thrace.
Physicians were asked to invite to the study all hypertensive patients among the first 20 patients that would visit their practices for any reason for 20 consecutive working days. The study was conducted during the spring of 2017 (1 March – 31 May 2017). According to the inclusion criteria, the participants were patients who (a) had diagnosed hypertension and received BP-lowering medication, (b) were aged over 18 years, (c) were physically and mentally able to participate in an interview, (d) had adequate understanding of the Greek language and (e) provided signed, informed consent.
Blood pressure measurement
Hypertension control was defined as achievement of systolic BP less than 140 mmHg and diastolic BP less than 90 mmHg10. For the evaluation of the control status of the patients, BP was measured according to the 2013 European Society of Hypertension/European Society of Cardiology guidelines for the management of arterial hypertension10. Patients remained seated for at least 5 minutes before the BP measurements. The BP was measured at least twice at 2-minute intervals on the right arm, supported at heart level, using an Omron automatic digital blood pressure monitor (Omron HEM-757, Omron Healthcare). A standard cuff (12–13 cm wide and 35 cm long), was used, but a larger and a smaller size were available for use when necessary. The average of the two BP readings was used for analysis. If the measurements differed by 5 mmHg for either systolic or diastolic readings, subsequent measurements were taken at 5–10-minute intervals. The average of these two BP readings was used as the BP value for those patients.
Questionnaire
A pre-tested 42-item printed questionnaire was constructed for the purposes of the study. It consisted of five sections examining demographics (age, gender, higher educational level, marital status, professional status), risk factor activities (smoking, alcohol consumption, physical activity), knowledge and attitudes toward the management of hypertension, antihypertensive medication, and comorbidities and other medication. Two open-ended questions were asked: thoughts regarding the participant’s BP management and antihypertensive medication, and if there was something that the participant found challenging regarding their daily adherence to treatment. The participants were requested to write their responses. Time taken to complete the questionnaire was approximately 15–20 minutes.
Data analysis
Continuous variables were summarized with mean, standard deviation (SD) and range of minimum and maximum values or median and interquartile range (IQR), when they were not normally distributed. Categorical variables were presented with frequencies and the corresponding percentages. The comparison of BP control with gender was performed with a χ2 and the results presented with odds ratios (OR) and corresponding 95% confidence intervals (CI). All analyses were performed with the Statistical Package for the Social Sciences v21.0 (IBM; http://www.spss.com) and reported p-values were two-tailed at 5% significance level.
The open-ended questions were analyzed using thematic content analysis11. Analysis began with open coding describing each section within the data. Using comparison across the written answers, the open codes were refined into major themes, which provided a coding frame for analysis. Ideas and categories were generated after performing line-by-line analysis and were tested and further explored in subsequent questionnaires until saturation was reached. After compiling a list of meaning statements, emerging clusters of meaningful units were examined. The final themes were agreed upon after two researchers (ZT and SB) reached consensus.
Ethics approval
The research protocol was approved by the Ethics Committee of the Medical School of Aristotle University of Thessaloniki (approval reference: 8/22-02-2017). All patients gave written informed consent prior to their participation in this study.
Results
Description of participants
A total of 613 hypertensive patients were recruited (response rate 91%). The most common reason for non-participation was lack of time (98%). Mean age was 71.5 years (SD 9.4, range 34–100), and 39.5% (242) were male. The demographic and clinical characteristics of the participants are presented in Tables 1 and 2, respectively.
Table 1: Patients’ demographic and lifestyle characteristics (n=613)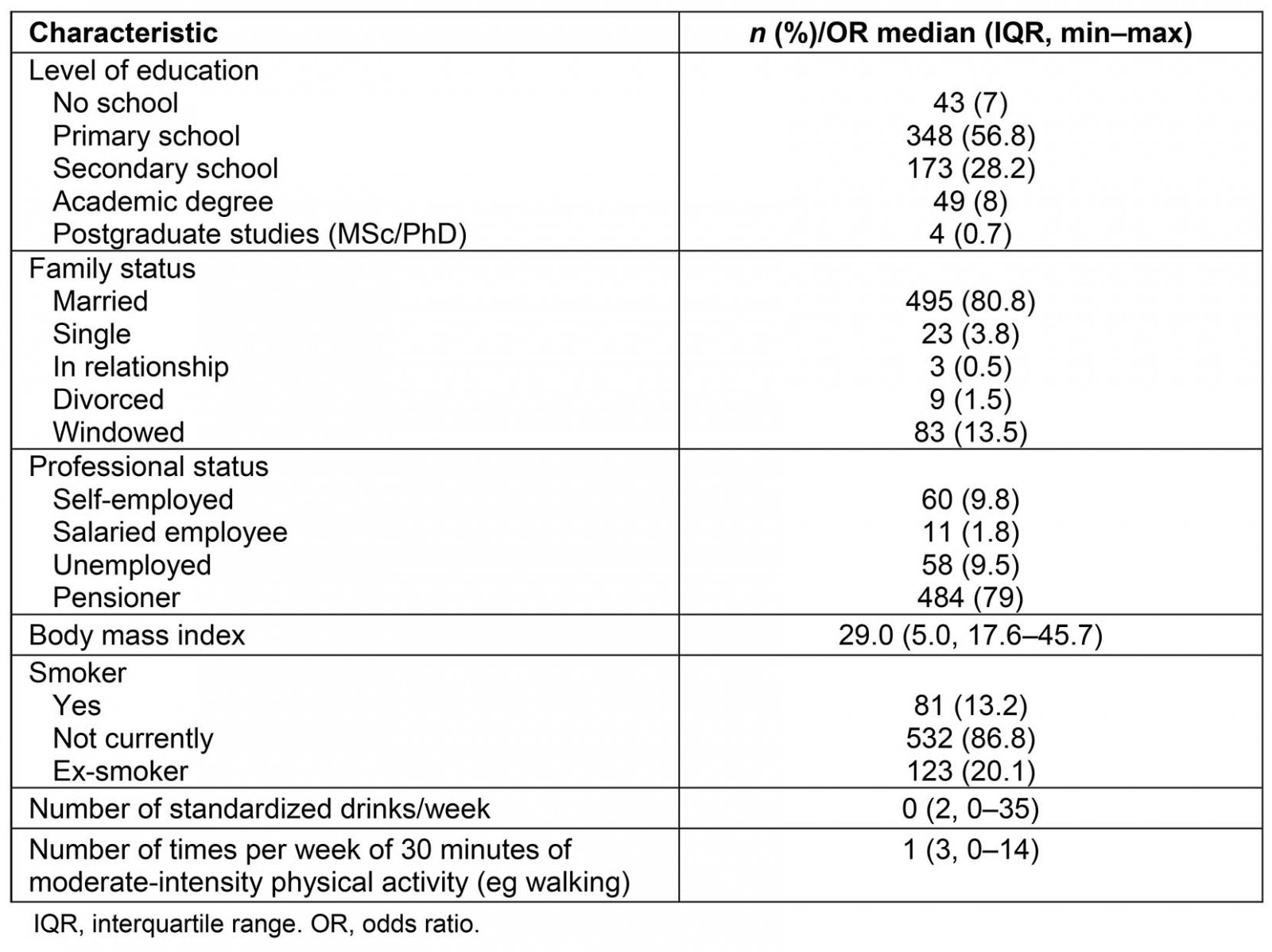
Table 2: Patients’ clinical characteristics: medication and comorbidities (n=613)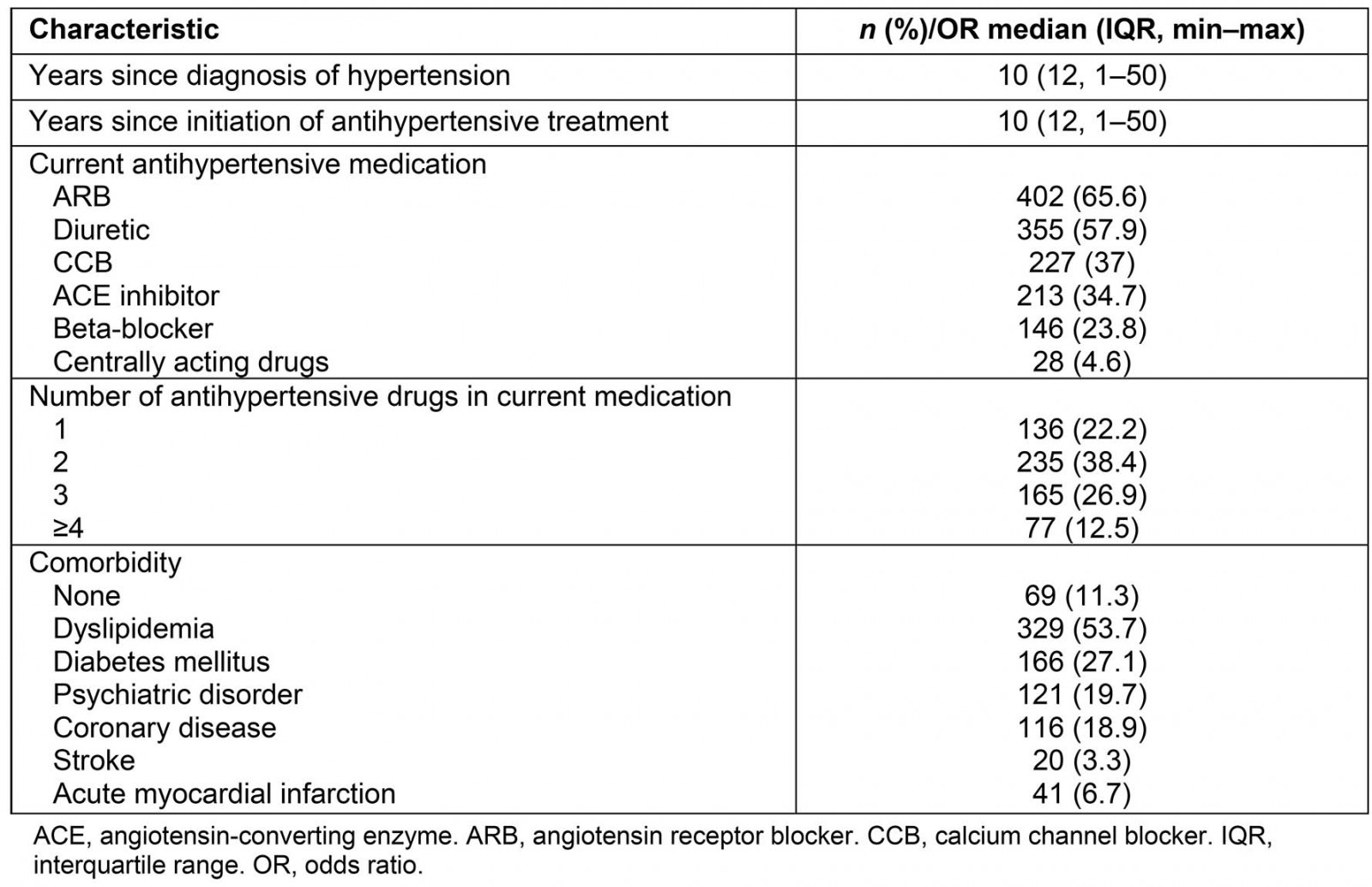
Perceived level of control and knowledge of hypertension management
The percentage of patients with uncontrolled BP was 41.3% (n=253). Interestingly, 67.6% (n=171) of patients not achieving BP control considered their BP controlled, 18.6% (n=47) considered it uncontrolled, while 13.8% (n=35) declared they didn’t know. Among the 359 patients with controlled BP, 82.5% (n=296) knew their BP was controlled, while 7.5% (n=27) perceived that they hadn’t achieved control and 10% (n=36) declared they didn’t know.
The target level for systolic and diastolic BP was unknown by 46.8% (n=287) of participants. Patients’ measurement of BP had a median value of two times per week (ΙQR 2, range 0–21). The measurements usually took place at home (548 (89.4%)), and for 22 (3.6%) at pharmacies. Daily adherence to the hypertensive medication was declared by 566 participants (92.3%).
Table 3 presents the perceived and actual hypertension control, as well as the knowledge of target BP levels by gender. It was shown that the odds of actual BP control were 1.44 times higher in women than in men (p=0.030), while there was no significant difference in perceived BP control (p=0.406) or knowledge of target BP levels (p=0.088) between women and men.
The physicians responsible for the management of hypertension were GPs for 56.5% (n=351) of the participants, cardiologists for 29.3% (n=182), internists for 10.3% (n=64) and physicians of other specialties for 2.4% (n=15). The participants had visited a physician for the management of hypertension, including their visits for medication prescription, an average of four times during the past year (IQR=2, range 1–16).
Table 3: Perceived and actual hypertension control, and knowledge of target blood pressure levels by gender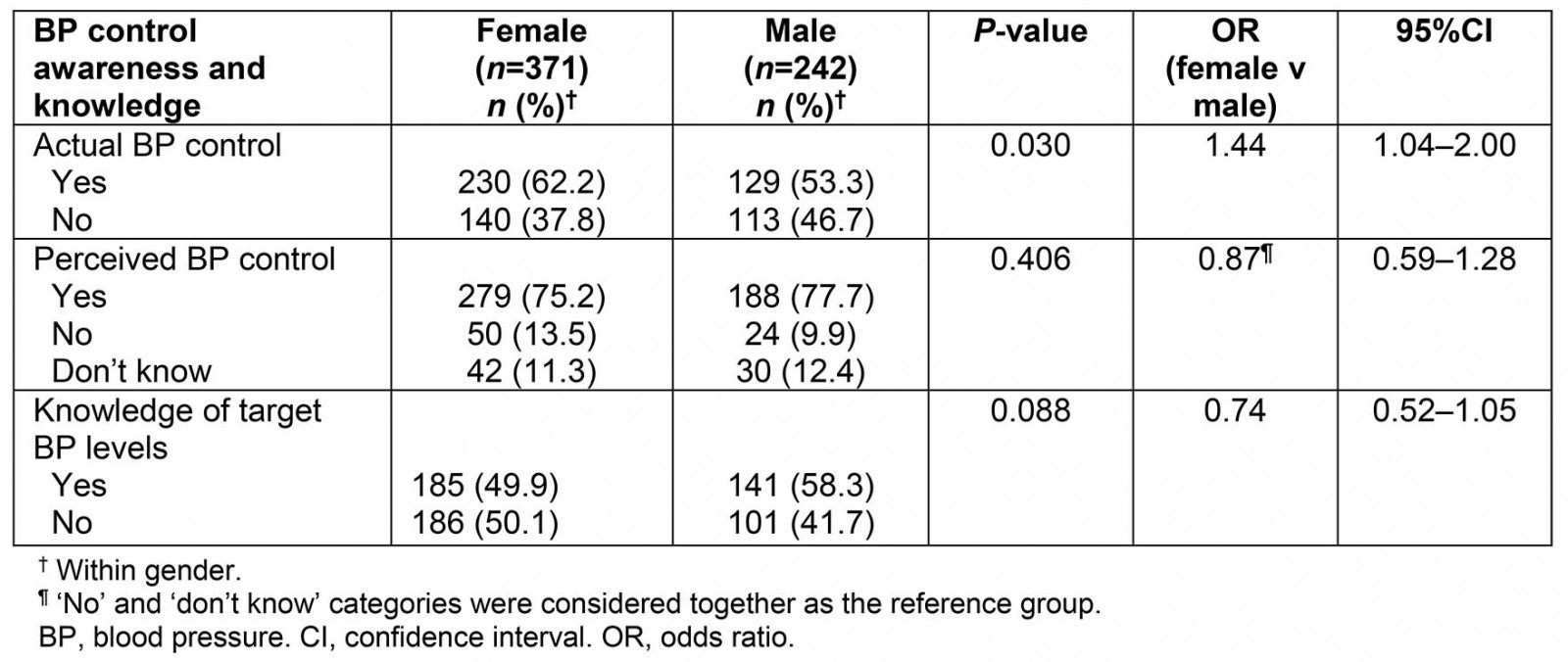
Patient-related barriers to blood pressure control: qualitative analysis
The identified issues possibly affecting adherence, satisfaction with treatment and contributing to suboptimal BP control were described in six themes.
Knowledge gaps: The unawareness of the importance of daily antihypertensive medication consumption in achieving hypertension control was revealed in a number of participants. As a result, some patients did not take a number of pills when their BP measurement was normal, ignoring that this behavior would lead inevitably to poor hypertension control.
On a day that the BP is ok, I don’t have to take my pills. (participant 53, male, 69 years)
When this unawareness was reinforced by lack of knowledge on the safety of the prescribed medication, it led to another argument for the ‘benefits’ of poor daily adherence to the treatment plan.
I take lots of pills daily, that’s why I miss some of them on purpose, because I don’t want to put extra burden on my body. (participant 469, male, 52 years)
Moreover, some hypertensive patients didn’t know that although high BP is often associated with few or no symptoms, it should be treated daily with antihypertensive medication. They also ignored that only BP measurements could be reliable in revealing whether the BP is within the targeted levels.
I take my pills when I feel that I have raised BP. I can tell when I need them, because my cheeks turn red and I have headache. (participant 94, female, 63 years)
Intolerance of adverse events: Adverse events are expected in a number of patients that are treated with antihypertensive medication. For some patients these can be so intense that they could affect their adherence to the treatment plan.
I cannot stand the swelling in my feet. (participant 107, male, 85 years)
I have to urinate so often. (participant 191, female, 57 years)
Patients may misinterpret some irrelevant symptoms or medical conditions as adverse events of their antihypertensive medication, with consequences in their adherence to the treatment plan.
I often suffer from vaginitis, because of my antihypertensive medication. (participant 185, female, 60 years)
Negligence: A notable number of patients mentioned that they sometimes, unintentionally, forget to take their daily dose.
I often forget to take my pill. (participant 325, female, 55 years)
Unmet individual preferences: Individual preferences could play an extremely important role in the acceptance of a treatment plan and the achievement of daily adherence. Some issues that could be of major importance for a patient may have not been considered by physicians. Size of the pill is one of these issues and was mentioned by a few patients.
The size of the pill is a problem … It is too big. (participant 163, female, 59 years)
Surprisingly, disliking the pharmaceutical company that produces and distributes the medication was also mentioned as a reason of poor adherence to the antihypertensive medication.
I don’t want to take a pill from this pharmaceutical company. I have read some awful things about it. (participant 401, male, 69 years)
Financial barriers: Financial barriers should also be taken into consideration. A few patients raised their concerns about the price of the antihypertensive medication and the out-of-pocket payment for getting a prescription.
The pills are too expensive. (participant 609, female, 74 years)
I cannot afford to regularly prescribe them. (participant 12, male, 69 years)
Overtreatment of hypertension: Overtreatment of hypertension could lead to abnormally low blood pressure. A few patients were found to confront the situation themselves by missing some doses or even discontinuing their medication instead of consulting their physician.
When I take my pills, BP drops low, I feel dizzy. (participant 591, female, 79 years)
Discussion
This multi-centered, mixed-methods study in patients from rural primary healthcare practices has revealed a significant disconnection between perceived and actual BP control, knowledge gaps about optimal BP control values, as well as attitudes and concerns that could be barriers for adherence to medication and therefore to effective BP control. The main barriers revealed by qualitative analysis were knowledge gaps, intolerance of adverse events, negligence, unmet individual preferences, financial barriers and overtreatment of hypertension.
The disconnection between participants’ perceived and actual BP control, often with overestimation of BP control rates, is expected to have a negative impact on the achievement of optimal BP control. Knowledge gaps relating to BP control values for almost half of the participants, as well as the often asymptomatic nature of hypertension, could explain partly this disagreement. This finding is in accordance with a previous Greek study in a rural population9, and with the more recent Chinese HAPPEN survey, where although 85% of the patients believed that BP targets were achieved, only 31% of them were actually controlled12. Moreover, it is in line with an American study that reported that patients’ perception of their BP control does not reflect their actual readings, except for the majority of those with controlled BP6. Unawareness of the effectiveness of current antihypertensive treatment is a barrier to the achievement of BP control that physicians should take into special consideration, because it could contribute to lack of treatment intensification. Physicians should bear this barrier in mind and try to address it by informing their patients about the importance of regular BP measurements at home, in order to accurately check their actual BP control.
Another important barrier was the participants’ knowledge gaps regarding the management of hypertension. Lack of awareness of optimal BP control values in half of the participants, as well as the description of attitudes of low adherence to medication when the BP control is achieved in a number of patients, seem to be international challenges, because they have been described in previous studies2,6,9,13,14. The existence of such knowledge gaps underlines the need for the development of well-informed and autonomous patients, with appropriate personalized education by their physicians, in order to contribute actively and consciously to the control of their chronic diseases. In well-trained and empowered patients, even the phenomenon of negligence –reported in the themes associated with poor adherence to medication – is expected to decline. Patients have been often reported forgetting to take their medications2,15. However, whenever impaired memory function is suspected, special precautions should be advised to patients’ carers, because dementia has been recognized as a key barrier to medication adherence among the elderly population16.
The finding that women were significantly more likely to have controlled BP should be interpreted with caution, although it is in accordance with a number of recent European and Asian studies17,18. A recent large-scale study in the UK that analyzed data from the Health Survey for England presented comparable control in both genders19, while another cross-sectional observational study in 12 European countries reported that female gender was associated with an increased risk of having uncontrolled hypertension20. Apart from possible behavioral and cultural differences that could partly explain these differences, a growing body of research suggests gender dimorphism in the pathophysiology of hypertension and pharmacological response to cardiovascular drugs21. Further efforts are required to explore possible gender differences in mechanisms responsible for hypertension, obtaining gender-specific data from clinical trials in order to determine the best treatment options in everyday clinical practice that will increase the control rates of hypertension in both genders22,23.
Although reported daily medication adherence in the present study was very high, the themes that have emerged with the qualitative analysis uncovered a number of issues regarding patients’ concerns, problems and expectations that physicians ought to discuss with their patients. Intolerance of adverse events, financial barriers, even unmet individual preferences about the size of the tablet of the prescribed medications, should be addressed in an effort to raise adherence to treatment plans. Previous research is supportive of the importance of patient expectations1,4,24, outlining the necessity of eliciting each patient’s needs and worries by practicing patient-centered medicine.
To the authors’ knowledge, there is a scarcity of data on the agreement between patients’ perceived and actual BP control. To that end, this study may provide an important insight into hypertension management. Furthermore, it is one of the few studies conducted in rural areas of Greece aiming to add a precious qualitative insight in patient-related barriers in BP control.
Some limitations of this study should be taken into consideration for the interpretation of the findings. First, the selection of the GPs as researchers in their own practices may have resulted in the reluctance of some patients to declare honestly their adherence to medication, possibly explaining the very high percentage of daily medication adherence stated. On the other hand, a written question on what they think about their BP management and antihypertensive medication by their physician could have provided to a number of patients the unique opportunity to reveal concerns and perceptions that they had been reluctant to bring up in the past. Another limitation of the study could be that the assessment of BP control was performed using office measurements. However, although it is suggested that it is preferable to measure BP at home, the methodology of office measurements of BP has often been used for research purposes25-28.
Conclusions
This multi-center, mixed-methods study in patients with treated hypertension revealed a number of patient-reported issues with antihypertensive medication, which may have an impact on medication adherence and blood pressure control. The presented findings suggest that GPs should be aware of the possible disconnect between their patients’ perceived and actual BP control, with frequent overestimation of BP control rates. Moreover, the level of knowledge on targeted BP level and BP management should be investigated for each patient and individually addressed by the physicians. General practitioners should focus on covering their patients’ knowledge gaps and on empowering them to get more actively involved in the management of their chronic condition. Simultaneously, physicians should aim to elicit each patient’s attitudes, concerns about adverse events, individual preferences, as well as possible financial barriers and negligence, in an effort to actually see the antihypertensive treatment ‘through their patients’ eyes’ and eliminate possible barriers to medication adherence. The provision of patient-centered care remains the gold standard for elimination of patient-related barriers in medication adherence and for achieving higher levels of BP control.
Acknowledgements
The authors gratefully acknowledge all the GPs that contributed to collecting the data for this study. In particular, we would like to thank: Α. Mposkariova (Health Centre of Kassandria, Chalkidiki), G. Atmatzidis (rural practice of Proti, Serres), T. Kerasidou, E. Chartaba and B. Naziri (Health Centre of Soufli, Evros), D. Tsiora (rural practice of Eucarpia, Serres), V. Gislis (rural practice of Maurommati, Karditsa) and L. Roganaki (rural practice of Mitropoli, Karditsa).
References
You might also be interested in:
2015 - Exploration of Aboriginal and Torres Strait Islander perspectives of Home Medicines Review
2012 - 'It's a regional thing': financial impact of renal transplantation on live donors





