Introduction
Access to health care in developing countries is scarce and subject to many barriers such as lack of medical equipment, high poverty rates, and poor infrastructure1. Recently, the implementation of short-term medical service trips (MSTs) from high-income countries has become a possible solution to providing for the healthcare needs of these countries2. A typical MST lasts from 1 day to 4 weeks and goes to a developing country, establishes a temporary clinic, and offers outpatient services to local communities. Treatment generally takes place during single visits where follow-up care is often not available. Due to the logistical challenges of transporting diagnostic equipment, MST clinics mainly use inexpensive portable tests that provide immediate results to inform treatment plans. New methods to effectively deliver care given these constraints are of great interest to global healthcare organizations.
Point-of-care ultrasound (POCUS) imaging shows promise as a diagnostic tool in developing countries because it is relatively inexpensive and has a broad range of applications3. Moreover, it is safe and accurate, provides immediate results within the clinical scope of physicians on MSTs, and aids clinical decision-making in remote mobile clinics. Providers have widely incorporated portable ultrasound machines into MSTs; it has been reported that up to 40% of trips have them3.
However, despite widespread use, few studies have examined how often ultrasound imaging is used and whether its use changes the medical management of patients. Furthermore, to the best of the authors’ knowledge, there are currently no studies regarding the appropriateness of ultrasound exams on MSTs, and no criteria have been developed by the American College of Radiology (ACR)4. A prior study conducted in Nicaragua showed the promise of ultrasound imaging in MST clinics; however, further work must be done to explore ultrasound use in these settings5. Accordingly, the purpose of this study was to determine the usefulness of portable ultrasound imaging during a short-term MST to rural Guatemala. Specifically, the primary objective was to determine how often ultrasound results changed the medical management of the patients and to assess the most common indications for ultrasound imaging. The secondary objective was to assess how appropriate each POCUS examination was in accordance with established ACR appropriateness criteria.
Methods
A multidisciplinary group of physicians set up a mobile clinic in Antigua, Guatemala, during a 3-day MST in December 2019. This was a retrospective observational study, analyzing the collected data. As the collected data contained minimal identifying data, a waiver of consent was obtained.
In the months preceding the trip, the organizing agency advertised their upcoming health clinic through local community leaders. The trip to Guatemala used the city of Antigua as a centralized location. The group then traveled to the communities of La Trinidad, Santa Catarina Barahona, and San Miguel Dueñas to provide care in a rural setting. All patients who arrived were eligible for care and subsequently included in the dataset. Patients were seen in a single-visit outpatient setting. Medications were distributed as needed. All patients who had indications for ultrasound had their suspected diagnoses and treatment plans recorded before receiving a POCUS. Indications for ultrasound reflected the common clinical use in normal practice settings, such as visualizing heart function or quantifying hepatomegaly. Additionally, ultrasound was used instead of other imaging modalities, as resources were limited. The premedical students and medical students helped prepare each patient for the scan. Examinations were performed solely by a US-licensed emergency medicine physician with credentials in emergency ultrasonography and with over a decade of experience. US-trained diagnostic radiologists were available for consultation by web-call as needed. A highly trained US-licensed cardiologist was available on site for cardiac consultation. Following ultrasound imaging, each patient’s updated clinical diagnoses and treatment plans were recorded.
The collected data were retroactively analyzed to determine how frequently patients had indications for ultrasound imaging, what the main indications for ultrasound imaging were, how often treatment plans were changed following ultrasound imaging, and how appropriate each study was according to ACR appropriateness criteria. Indications for ultrasound imaging were grouped by organ system (cardiac, genitourinary, gastrointestinal, and musculoskeletal). Patients were considered to have a change in medical management if they had a change in diagnosis or treatment instructions or addition or withdrawal of pharmacotherapy. POCUS examinations that ruled out a suspicion but did not diagnose a cause were defined as ‘excluded diagnosis’ and considered a change in management.
Inclusion criteria
All adult patients (age ≥18 years) were included in the data analysis.
Exclusion criteria
Patients aged less than 18 years were excluded from the data analysis. All ultrasound tests were compared to the ACR appropriateness criteria to determine if the performance of ultrasound would be considered best practice in the USA given full availability of medical equipment. Ultrasound scanning was characterized as ‘usually appropriate’, ‘may be appropriate’, or ‘usually not appropriate’ as per the ACR appropriateness criteria.
Ethics approval
This study was approved by the Baylor College of Medicine (IRB approval H-47069)
Results
During the 3-day MST, 205 patients were examined. Of these patients, 24 (12%) underwent POCUS imaging (average age 51.9 years). Seventy-one percent of the patients who received POCUS imaging were female. The use of POCUS imaging confirmed the pre-test suspicion in 11 (46%) patients, changed the medical suspicion and management in 5 (21%) patients, and excluded the leading diagnosis subsequently changing management in 8 (33%) patients (Table 1). The most common indication for ultrasound testing was suspected cardiac disease (11 patients, 46%) followed by suspected gastrointestinal (8 patients, 33%), genitourinary (2 patients, 8%), and musculoskeletal (2 patients, 8%) conditions (Table 2).
For gastrointestinal diagnoses, the POCUS confirmed the majority of cases (6 patients, 75%), and changed the diagnoses on the others (2 patients, 25%). For diagnoses that were confirmed, ultrasound was used to rule out anatomical abnormalities, which, combined with the clinical picture, were used to arrive at a more accurate diagnosis. The most common confirmed diagnosis of gastric pain was gastritis, for which proton pump inhibitors were prescribed. An example of a changed diagnosis was the presentation of generalized stomach pain, for which an enlarged post-voiding bladder was visualized, shifting the leading diagnosis to urinary retention and infection.
For cardiovascular disease, POCUS was used to visualize the heart and valvular flow. While altering the leading diagnoses and subsequent management, POCUS did not provide the etiology of many cardiovascular cases. In total, POCUS resulted in mostly excluded diagnoses (8 patients, 73%). A smaller subset of cardiac indications resulted in a confirmed diagnosis (3 patients, 27%). There were no changed cardiac diagnoses. The excluded cardiac diagnoses presented with a manifestation of shortness of breath or chest pain, for which no abnormalities were visualized on the heart. Depending on the severity of the symptoms, several patients with chest pain were referred for further work-up. An example of a confirmed diagnosis was the presence of a prolapsed mitral valve.
All ultrasound tests were indicated given the available equipment during the MST. Comparing the clinical presentation to the ACR’s appropriateness criteria for ultrasound use, 14 (58%) tests were consistent with ‘usually appropriate’, nine (38%) were deemed ‘may be appropriate’ and one (4%) was deemed ‘usually not appropriate’ (Fig1).
Table 1: Confirmed and changed diagnoses using ultrasound examination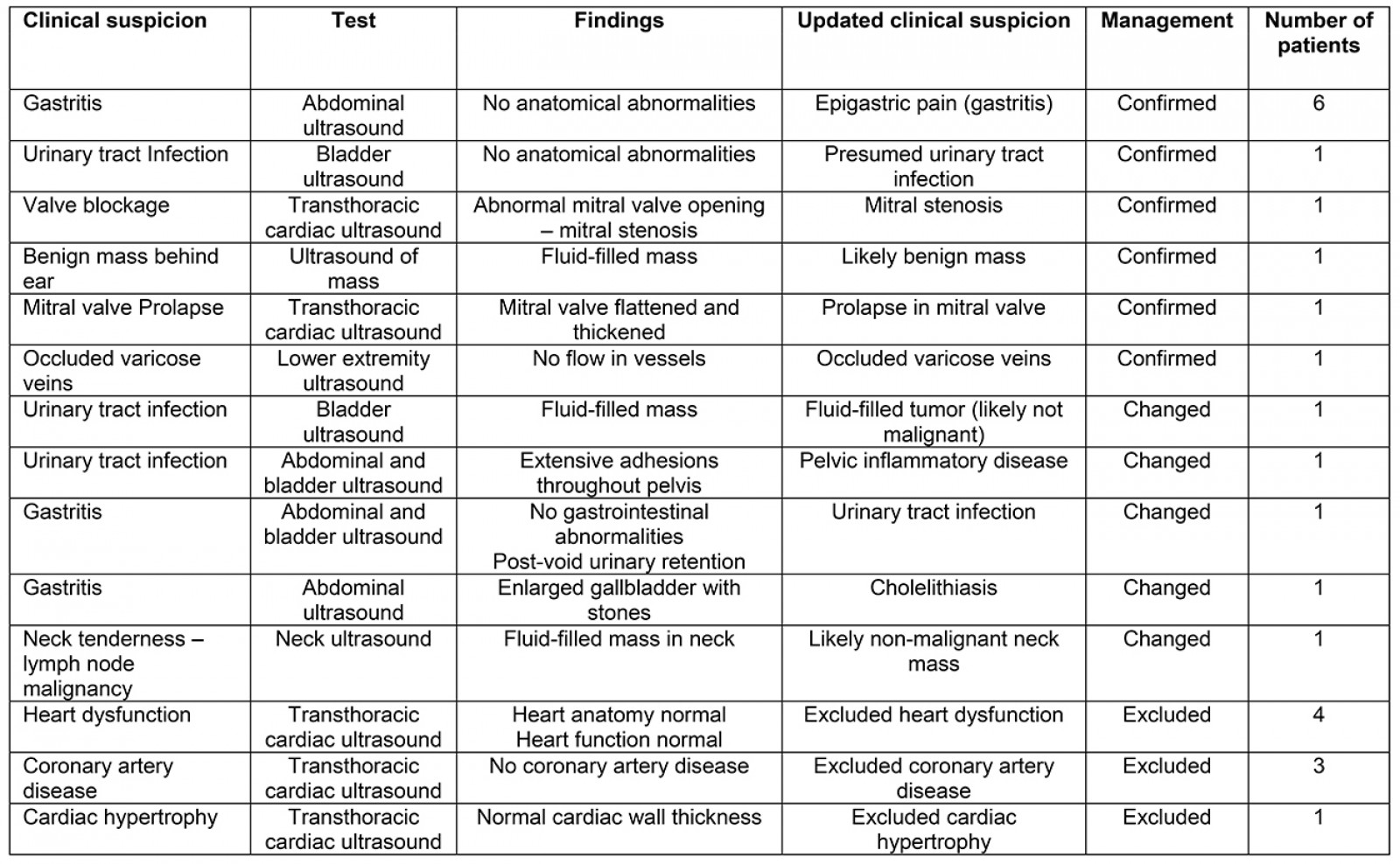
Table 2: Management changes by organ system 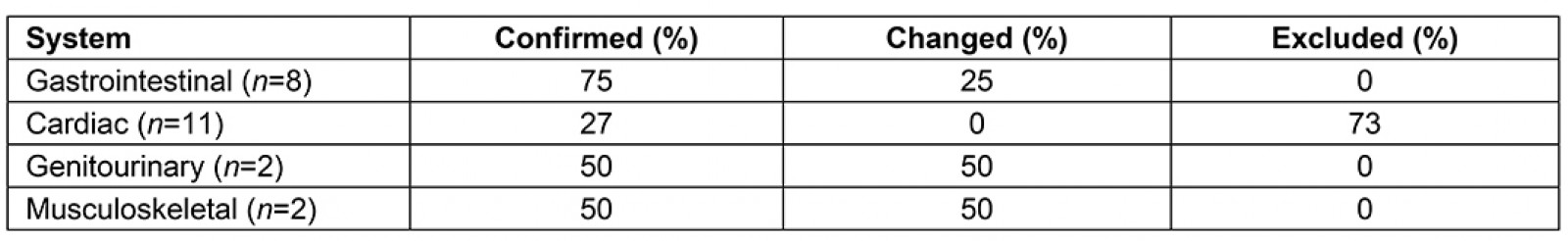
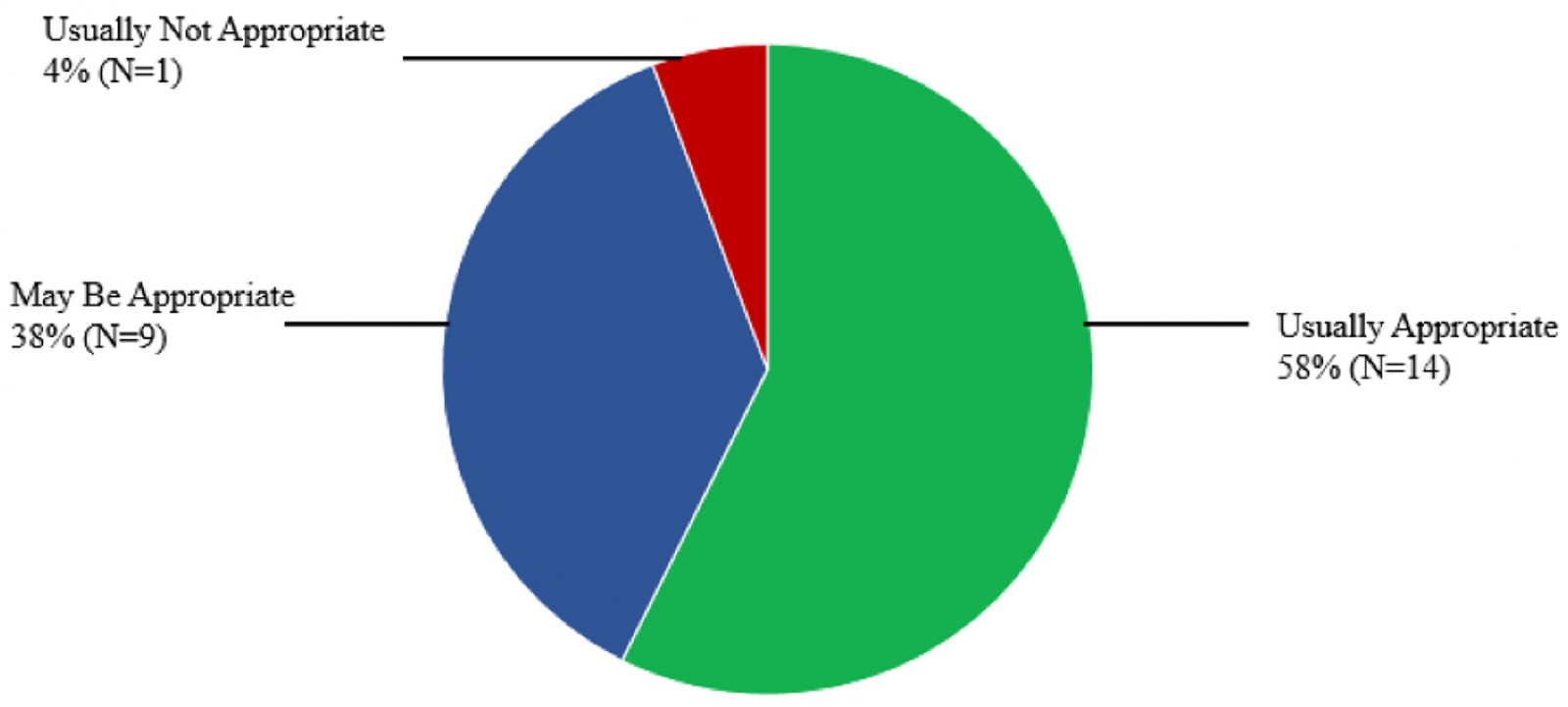 Figure 1: Radiology appropriateness designations for performed ultrasound examinations.
Figure 1: Radiology appropriateness designations for performed ultrasound examinations.
Discussion
Portable ultrasound integrated into outpatient care helped physicians more accurately diagnose diseases in the patients seen during the MST as compared to physical exams alone. While the majority of patients seen in the rural outpatient clinic did not have indications for ultrasound testing, a small yet substantial portion of patients had issues that warranted POCUS testing. Of the patients who received POCUS testing, over half had management changes resulting from the use of the POCUS.
Ultrasound was particularly effective in guiding clinicians to properly treat gastrointestinal diseases. Often the presenting symptoms were non-specific. By visualizing the anatomy of the abdomen, the ultrasound provided clues to the underlying pathology and required treatment. Moreover, ultrasound was vital in excluding potentially life-threatening conditions with non-specific presentations such as the presence of an ectopic pregnancy or appendicitis in instances of abdominal pain.
Ultrasound was likewise helpful in diagnosing cardiac problems, as it allowed for visualization of heart chambers and valves. For many of the patients who underwent POCUS imaging for cardiac indications, traditional physical examinations alone did not provide enough information to confidently treat patients. The POCUS was useful in confirming or excluding the presence of valvular diseases and other cardiac abnormalities. In 73% of the patients with suspected cardiac disease, the suspected diagnoses were excluded upon visualization of normal heart function, although this raises the question of how to provide follow-up care for indications that were not determined. Moreover, several disease states, such as cardiomegaly, can be suspected through the use of POCUS, but determining the etiology cannot be done in the MST setting6.
Physicians on MSTs have limited diagnostic equipment available, especially in rural regions7. The present study’s results showed that, in over half of the POCUS tests performed in the present study, ultrasound imaging was deemed ‘usually appropriate’ according to ACR appropriateness criteria. Ultrasound is generally the best practice for initial work-up of chest pain as it can be useful in evaluating suspected valvular disease or determining the presence of pneumothorax8,9. As such, the ultrasound was a great tool for physicians evaluating chest pain and shortness of breath in the rural outpatient setting. Moreover, many of the gastrointestinal indications were deemed as ‘may be appropriate’ as an abdominal CT with contrast is considered best practice for diagnosing generalized pain. However, POCUS is one of the several modalities that are suggested if CT is not available. The single case in which POCUS imaging was deemed ‘usually not appropriate’ was an evaluation of neck tenderness. In this instance, radiographic imaging was the only modality deemed appropriate by the ACR. Currently, there are no guidelines guiding clinicians as to best practices for ultrasound use, despite how widely they are used10. The establishment of appropriateness criteria for MST specific ultrasound use will help guide providers to proper treatment giving the available diagnostic equipment.
During the duration of this MST, patients were provided for by pre-medical students, who handled initial processing; medical students and residents, who assisted in acquiring the relevant histories; and practicing physicians, who performed physical examinations, conducted ultrasound tests, and determined treatment plans. One of the reasons for the growth of MSTs is the ability to incorporate trainees from all levels into the care of patients. Due to the heightened need in the countries that are served, all levels of interactions serve a distinct purpose in the care for the patient.
Recently, there has been an increasing interest in quantifying the use of ultrasound on MSTs as many organizations employ them on their trips. A study assessing an MST in Nicaragua found that POCUS changed management for 36% of patients5. Moreover, a study in Nigeria found that 46% of scans detected an abnormality11. In conjunction with the present study’s data, these results are promising; however, more work is needed. One promising avenue to explore is the parallels between MSTs and disaster medicine. Notably, sonography has long been used in disaster triage, and insights can be gained by paralleling the two12. More specifically, it has been found that POCUS can diagnose many abdominal and cardiac conditions rapidly and conclusively13,14. MSTs can use the gained knowledge of disaster triage to provide guidelines on proper POCUS use.
While MSTs serve as a temporary solution to the medical needs of rural under-served communities, there is a focus on permanent implementation. Historically, there has been a focus on supplying medications1. However, with MSTs finding value in ultrasound, efforts should increasingly focus on finding ways to bring ultrasound machines to communities, and training local doctors in their use. Notably, ultrasounds have already found their bearing within rural communities due to their ease of use and real-time feedback15. However, such implementation is not without challenges. There is a barrier to education dissemination in many rural parts of Central American countries16. Additionally, the cost of ultrasound machines may be costly for resource-limited communities. A possible solution is utilizing the longstanding relationships that medical service organizations have built with local communities to bring ultrasound equipment that will remain at the site and then educating local doctors in its use. Training of local doctors in POCUS would likely improve their ability to determine which patients could be treated locally, compared to which patients would require travel to a higher level of care.
This study had several limitations. Although the results are promising, the number of enrolled patients was low. Moreover, there was a significant selection bias such that every adult patient who received treatment was included. There is also an issue in blinding, as the physicians who made the initial diagnoses were the same ones who performed POCUS testing and updated the diagnoses. However, in the resource-limited communities, using the same individual for both diagnoses was necessary to effectively offer a diagnosis in a single-visit encounter. A final limitation is that there was no follow-up of patients, limiting the ability for definitive confirmation of several etiologies.
Conclusion
The results of the present study suggest that the use of portable ultrasound imaging improves physicians’ ability to diagnose diseases and manage patients seen during MSTs. Ultrasound is particularly useful in determining the cause of cardiac and gastrointestinal problems and provides a low-cost solution to the growing demands for care in developing countries. Moreover, ultrasound can be useful in excluding potentially life-threatening conditions that would require transfer to more advanced care. Further studies should analyze MST data from several locations to expand the size of the study populations and further assess the appropriateness of ultrasound imaging in a variety of settings.
Acknowledgements
Thank you to Scientific Publications, Research Medical Library at MD Anderson Cancer Center for help editing the manuscript.
