Introduction
In the context of global nursing shortages, recruitment and retention of nurses is an increasingly important challenge for the sustainability of healthcare delivery1. Failure to recruit and retain nurses in rural and remote settings is a particularly acute problem2,3. Nurse-to-population ratios are significantly lower in rural and remote areas, further exacerbating the problem4. Nurse vacancies are anticipated to accelerate over the next decade as more of the workforce retires5.
A growing body of literature on rural and remote nursing has explored a variety of individual factors influencing nurses’ decisions to work in rural and remote settings. These include a sense of belonging6, having a rural background, family connections7 and job satisfaction8. Much of the literature describes the difficulty within rural and remote areas to maintain skilled and competent nurses in the face of workforce shortages9, increased workload10,11, the generalist nature of the role12 and the challenges of professional isolation13.
Rural nursing practice has been defined as a unique, demanding and challenging speciality requiring specific personal qualities such as flexibility, versatility and adaptability14. The characteristics of rural nursing include the need for rural nurses to assume the role of expert generalist and function as a jack-of-all-trades whilst working in a broad spectrum of clinical settings and performing many diverse tasks6.
Despite the complexity of factors that influence nurses’ decisions to work in rural or remote areas, much of the research to date has focused on specific factors in isolation. The purpose of this article is to systematically review existing literature on nurses’ experiences to explore the influences on nurses’ decision making to work in rural and remote areas. By doing so, findings from this study will inform strategies to improve recruitment and retention of nurses in rural and remote settings.
Background
Defining ‘rural’ and ‘rural nursing’
The literature is replete with definitions of rural nursing. The word ‘rural’ often conjures up images of the idyllic life in the country15. ‘Rural’ is described as a vague and ambiguous term signifying many things to many people, such as agricultural landscapes, isolation, small towns and low population density16. The literature categorises ‘rural’ using a range of pre-assigned characteristics including land use, population density, demographic structure, environmental characteristics, population characteristics, non-metropolitan area and commuting patterns17. The variation in definitions of ‘rural’ has important methodological implications18 such as assuring the validity, reliability and utility of research19. Definitional complexity around ‘rural’ also impacts understandings of rural nursing20.
Rural nursing is defined by some as ‘the provision of health care by professional nurses to persons living in sparsely populated areas’21. Although there is debate around whether any difference exists between nursing practices in rural and urban health care facilities22, some common features of rural nursing predominate. The term ‘expert generalist’ is often used to describe rural nursing, with suggestions that rural nurses need to be a ‘jack-of-all-trades and master of many’12. Rural nursing is conceptualised as being a ‘long way from anywhere and pretty close to nowhere, being independent or perhaps just being alone’, and the challenges are described in terms of difficulties in separating one’s personal life from one’s professional life, as rural nurses are ‘stripped of their own anonymity while simultaneously charged with protecting their patients’ privacy’23. The implications of living and working in the same community, such as high visibility, lack of anonymity and privacy, result in nurses feeling as though they are living ‘in a fishbowl’24. Despite some consensus around the nature of rural nurses’ work, traditional definitions and descriptions are said to provide limited understanding of how rural practice shapes nurses’ unique approach to managing healthcare needs25. Within the literature debate is ongoing in respect to the difference between rural and remote area nursing with the context of practice in rural areas described as being more divergent than the context of practice in remote areas24. The generalist role of rural nurses increases as the population declines, thus the more remotely nurses are located the greater the generalist nature of the work22,24.
Existing evidence
Much of the recent research in rural and remote nursing has used quantitative designs and has been undertaken in Australia using large online survey repositories26-28. These studies have investigated connections between personality and career choice, and they highlight that persistence, self-directedness, cooperativeness and reward dependence are congruent with the professions’ requirements. Results conclude that individuals have a unique combination of traits that make them who they are, and that recruitment and retention policy should not adopt a ‘one size fits all’ approach26. Myriad demographic, developmental and environmental factors influence an individual’s life and work choices and their psychological profile, which raises a question about whether individuals with the observed temperament and traits are attracted to nursing in rural areas, or whether it is more likely that individuals develop certain character traits as a product of their rural experience and training28.
There has been a tendency to consider rural and remote nursing through cross-sectional studies26,29 rather than longitudinally, which would explore a more informed understanding of rural practitioners’ decisions-in-the-making. For example, the ‘rural pipeline’ describes the passage of medical students from the point of developing their aspiration for a career in medicine, through to retaining general practitioners (GPs) in rural locations, while highlighting key stages in between30. This includes how individuals construct their career choice based on their personal identity and how an individual’s attachment to place, such as the influence of rural upbringing31-33, impacts their career pathway – ultimately influencing their decision to remain part of that workforce. Most studies exploring recruitment and retention focus mainly upon medicine, but extending the concept of the rural pipeline to include other professions such as nursing has the potential to strengthen understandings of rural career choice34.
Rural and rurality are inherently geographical concepts but when a geographic location is imbued with meaning, it becomes place35. It is not possible to separate the experience of health and health care from the place in which it is experienced, and space and place have emerged as important and central themes in nursing research36. This research needs to move beyond considering places for health care merely as geometric points, passive containers or locations of human activity37, and focus conceptually on the dynamics between nursing and place, encapsulating the powerful social and cultural phenomenon permeated with power, symbolism and attachments38. Place matters – as a geographical location, a lived experience, as demarcation of space, and as a site of meaning creation35.
Much of the current research has focused on describing aspects of rural and remote nursing as individual entities, which does not provide insight into the complex dynamic of experiences that ultimately influences nurses’ decisions to work in rural and remote settings. This perspective is important to inform recruitment strategies for students and experienced nurses in the rural and remote setting.
The aim of this study was to explore the influences on nurses’ decisions to work in rural and remote healthcare settings.
Methods
A systematic review with qualitative meta-synthesis was used to answer the research question, ‘What factors influence nurses’ decisions to work in rural and remote healthcare settings?’ The study is reported following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines39.
Search strategies
Search strategies were devised for the following databases: Medline, Journals@OVID Full text and APA PsycInfo. The search spanned from January 1990 to January 2020 in order to capture the early rural nursing theory work21. The following speciality journals were also searched independently: Rural and Remote Health, Journal of Rural Nursing and Health Care and Health & Place. The reference lists of pertinent articles found were also searched. Table 1 summarises the search strategy. All search results were downloaded into RefWorks and duplicates were removed.
Table 1: Medline search strategy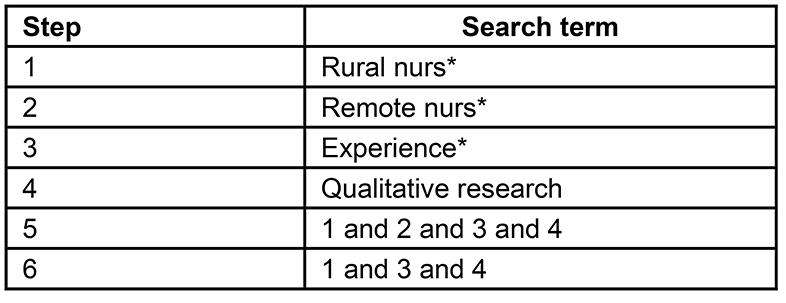
Study inclusion
The publications had to meet the following inclusion criteria: (1) published in the English language; (2) any aspect of experiences of rural or remote nursing; (3) qualitative research. Qualitative studies were targeted as this paradigm is more appropriate to capture the experiences of rural and remote nurses. Inclusion criteria were used to screen the title and abstracts. Full text articles were first scrutinised by SCM to confirm inclusion or exclusion. All screening was conducted by a second independent reviewer, AS, RGK or MB. Consensus was reached where debate existed around retaining or excluding an article.
Data extraction
Data were extracted by SCM, and checked by AS, RGK and MB, for the following characteristics for each retained article: author(s) and year of publication, country, focus/aim, design, method/sample, definition of ‘rural’/’remote’ and study limitations.
Quality appraisal
Retained articles were assessed using the CASP (Critical Appraisal Skills Programme) tool for qualitative research40, which was modified to include a scoring system from each of the CASP questions where ‘Yes’ = 1 and ‘No’ or ‘Can’t tell’ = 0. The maximum score was 10 and the minimum score was 0. All articles were critically appraised and scored by SCM and then independently scored by a second reviewer (AS, RGK or MB). The tool was not utilised to exclude articles from the synthesis but rather to enhance understanding and identify methodological limitations of the primary studies.
Synthesis of findings
Thematic synthesis41 was selected as it relies on an inductive line-by-line coding of text from the primary studies. By staying as close as possible to the experiential accounts of nurses working in a rural or remote setting, the aim was to generate new insights into this phenomenon.
All data were coded by hand by SCM and three key steps were undertaken in the synthesis. First, the results sections of each study were extracted and inductively coded line by line. Verbatim quotations and text were entered into NVivo v12 (QSR International; http://www.qsrinternational.com). Second, the identified master themes (dimensions) and subthemes (domains) were highlighted and organised into tables, and texts with similar content and meanings were grouped together as descriptive themes. As each study was coded, the bank of emergent themes was added to and developed. The third stage went beyond the content of the original studies by identifying and examining relationships between themes to develop an overarching analytical framework. The use of line-by-line coding enabled one of the key tasks in the synthesis of qualitative research to be undertaken: the translation of concepts from one study to another. Every sentence had at least one code applied, and most were categorised using several codes. A draft summary of the findings across the studies organised by the 18 descriptive themes was written by SCM. AS, RGK and MB commented on this draft and a final version was agreed. The analysis informed the development of a model of rural and remote nursing.
Results
The results are presented in Figure 1 using a modified PRISMA 2009 flow diagram39. All independent reviewers agreed on the application of inclusion criteria and 40 full text articles were included.
All retained articles were published between 2001 and 2018 (Table 2). The geographical context of the 40 studies were as follows: Australia (15), Canada (12), USA (7), UK (4), South Africa (1), Ghana (1). The samples in the articles included were predominantly nurses (20), nurses/managers (6), nurse practitioners (2), mental health nurses (2), midwives (1), nurses/GPs (3), student nurses (3), dual role – nurse/midwife (1), preceptors/students (2).
Twenty of the 40 articles (50%) did not include a rural definition. Of the 20 articles that provided a definition, most used population based definitions, geographical classifications, accessibility/remoteness indexes such as the Rural/Remote and Metropolitan Area Classification (RRMA)42, the Weighted Inlier Equivalent Separations (WIES) based on number of hospital beds43, or the Australian Bureau of Statistics whereby hospitals are coded A–E44-46. Several articles offered bespoke descriptions of rural such as ‘rural nursing is carried out by a nurse in a health facility where the support services are predominantly visiting’47 and ‘mountainous terrain where access can be affected by adverse weather’48.
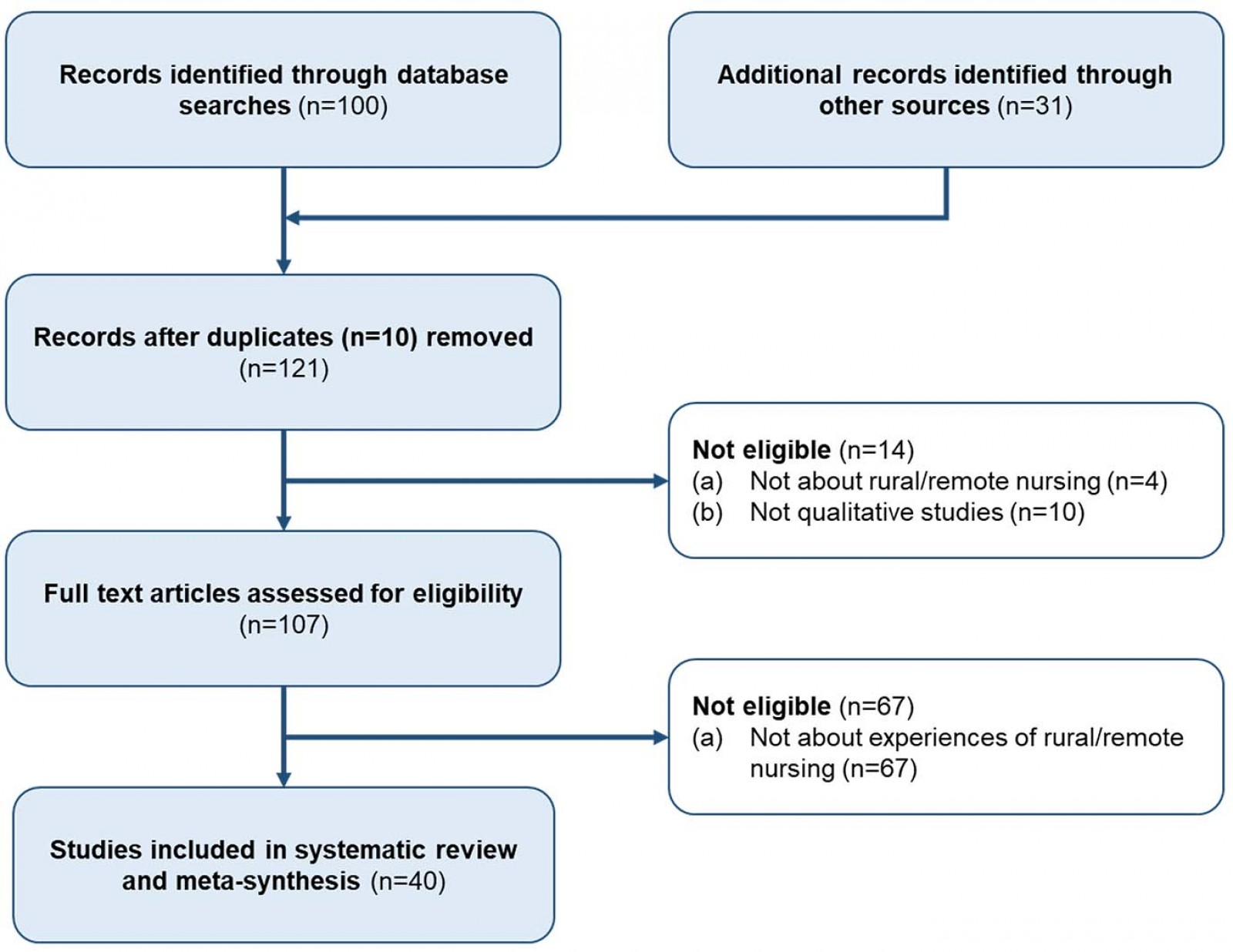 Figure 1: Modified PRISMA 2009 flow diagram.
Figure 1: Modified PRISMA 2009 flow diagram.
Table 2: Data extraction
| Author(s) | Country | Focus/aim | Method/sample | Definition of "rural"/"remote" | Limitations |
|---|---|---|---|---|---|
|
Arnaert et al (2009) [ref. 65] |
Canada |
To explore homecare nurses" attitudes to palliative care in a rural community |
Face to face semi-structured interviews and a focus group discussion with five homecare nurses |
Statistics Canada definitions - population density of 1.2 inhabitants per square kilometre; made up of 18 small municipalities |
The results may not be generalisable to other regions because each rural community has its own unique characteristics. |
|
Baernholdt et al (2010) [ref. 59] |
USA |
To identify how rural nurses and their chief nursing officers define quality care |
Focus group interviews - staff nurses (n=23), chief nursing officers (n=4), rural hospitals (n=4) |
American Hospital Association Statistics - rural hospital = located in a non-metropolitan geographical area with population less than 50 000 |
Study took place in one specific region of one state in southern region of USA, so findings may not apply to all rural areas. Insufficient information given regarding the researcher-participant relationship. |
|
Beks et al (2018) [ref. 57] |
Australia |
To explore the experience of rural nurses in managing acute mental health presentation |
Semi-structured face to face interviews with 13 nurses |
No definition |
Sample size of this study was subject to the response of nurses to the study invitation. Novice nurses were not adequately captured. |
|
Birks et al (2011) [ref. 74] |
Australia |
To report on models of health service delivery in remote or isolated areas of Queensland |
Multiple case study research design including interviews and focus groups. Registered nurses (n=35) |
No definition |
Lack of in depth description of data analysis process. Insufficient information given regarding the researcher/ participants" relationship. |
|
Bish et al (2015) [ref. 60] |
Australia |
To identify factors that influence directors of nursing in their approach to leadership when working in rural Victoria, Australia |
In depth, semi-structured interviews. Directors of nursing (n=5) |
No definition |
Small sample size in one Australian state may limit the transferability of the study. |
|
Boucher (2005) [ref. 50] |
USA |
To explore what qualities a nurse needs to "make it" in rural home care? |
Interviews with experienced rural home care nurses (n=12) |
No definition |
Recruitment strategy unclear. Insufficient details regarding ethics approval. Lack of in depth description of data analysis process. Insufficient information given regarding the researcher/ participants" relationship. |
|
Caldwell (2007) [ref. 14] |
USA |
To reveal the life stories of nurse practitioners in rural Appalachia |
Interviews of life stories and ballad elements of the culture. Nurse practitioners (n=7) |
No definition |
Lack of in depth description of data analysis process. |
|
Conger and Plager (2008) [ref. 72] |
USA |
To describe rural connectedness versus disconnectedness |
Focus groups and individual interviews. advanced nurse practitioners (n=30) |
No definition |
Difficult to ascertain how many of the 30 participants felt connected and how many did not. |
|
Corbett and Williams (2014) [ref. 61] |
Wales (UK) |
To study the interactions between nurses and their older rural patients by considering professional boundaries |
Semi-structured interviews and home-care observations between older adults (n=10) with chronic pain and community nurses (n=4) and carers (n=2) |
No definition |
Recruitment strategy unclear. |
|
De Valpine (2014) [ref. 51] |
USA |
To ensure the unique stories of bush Alaska nurses are preserved and told, to foster a strong bush nursing tradition and to inform recruitment, hiring and retention practices in remote settings |
Semi-structured interviews with long term retained (>15 years) nurses (n=10) |
No definition |
Bristol Bay may not be representative of other bush communities. |
|
Drury et al (2005) [ref. 47] |
Australia |
To describe nursing roles of registered mental nurses working in remote and rural areas of Western Australia |
Face-to-face interviews. Rural mental health nurses (n=5) |
Rural definition - rural nursing is carried out by a nurse who works in a health facility where the support services (medical and allied health) are predominantly visiting and in a community or district nursing service in a non-metropolitan area |
Small sample size taken from one rural region, placing limitation on the extent to which results can be generalised. |
|
Farmer et al (2007) [ref. 75] |
Scotland (UK) |
To consider Scottish maternity units and aim to identify issues in the change process associated with rurality and remoteness |
Interviews with managers, midwives and community members (n=131) in rural maternity units in the north of Scotland (n=6) |
Scottish Executive Classification defining "rural" as settlements of less than 3000 people and "remote" as more than 30 minutes from settlements of 10 000 people or more |
Insufficient information given regarding the researcher-participant relationship. |
|
Farmer and Kilpatrick (2009) [ref. 48] |
Australia and Scotland (UK) |
To investigate the actions of rural health professionals and consider if they were also social entrepreneurs |
Interviews (majority face to face) with nurses (n=21), general practitioners (n=7), primary health care managers (n=4), allied health professionals (n=6) in Tasmania and Scottish Highlands |
No definition |
Inappropriate to generalise the findings beyond the two countries. |
|
Farmer et al (2010) [ref. 76] |
Scotland |
To investigate older people"s health service provision in remote rural Scotland |
Semi-structured interviews with men (n=12) and women (n=11), service practitioners (n=9) and service managers and politicians (n=7) |
Scottish Government definition of rurality in terms of population sparsity and distance from service centres |
Study findings may not typify all of rural Scotland. Lack of urban comparator sites. |
|
Gibb et al (2005) [ref. 68] |
Australia |
To investigate the culture of workplace learning within a study of eight small hospitals |
Focus groups before and after a series of interventions designed to nurture a culture that supports learning (mentoring, generating cohesiveness within the team) with nurses (n=4-8 in each site) |
No definition |
Recruitment strategy a bit vague. |
|
Heilderbeer and Carson (2013) [ref. 70] |
Australia |
To explore what non-resident workers (fly in, fly out) see as the advantages and disadvantages of their modes of work, and whether they face the same or different social/personal and professional barriers to rural and remote practice as their resident colleagues |
Semi-structured interviews with non-resident nurses working in remote locations in Northern Territory, Australia (n=7) |
Population density of less than 0.1 persons per square kilometre |
Insufficient information given regarding the researcher-participant relationship. |
|
Hunsberger et al (2009) [ref. 13] |
Canada |
To investigate whether nurses receive the resources and supports necessary to meet the challenges of rural practice |
Semi-structured interviews managers (n=21) and staff nurses (n=44) in rural hospitals (n=19) |
Advisory Panel of the Canadian Medical Services in Underserved Regions - definition of rural communities = those with a population of 10 000 or less |
Insufficient information given regarding the researcher-participant relationship. |
|
Joseph et al (2013) [ref. 77] |
Canada |
To interpret the meaning of bad weather for front-line healthcare workers in rural long-term care |
Interviews with nurses and personal support workers (n=6) |
Rurality was defined using the Statistics Canada rural and small town (RST) definition of individuals living in towns or villages outside the commuting zone of major urban centres with a population of less than 10 000 |
Authors state that Interpretations were limited by the inability of the re-analysis approach to follow up with the interview respondents on new themes. |
|
Kenny and Allenby (2013) [ref. 43] |
Australia |
To examine issues that rural nurses face in the provision of psychosocial care from a broad general nursing perspective |
Focus group interviews. Rural nurses (n=22) |
Rural hospitals categorised by measuring the level of inpatient activity measured in terms of weighted inlier equivalent separations (WIES). Categorised as B to E |
The views reported within one rural region in Australia may not be reflective of the broader nursing workforce. Findings may not be generalised to every setting. |
|
Kenny and Duckett (2003) [ref. 44] |
Australia |
To explore the issues that impact on the ability of rural hospitals to provide health care |
In-depth interviews with managers, nurses and rural doctors (n=60) in rural hospitals (n=20) |
Australian Bureau of statistics - Australian Government (2002). Large metropolitan teaching hospitals = Code A, rural hospitals = Codes B to E, very smallest hospitals = Code E |
Insufficient information given regarding the researcher-participant relationship. |
|
Kenny and Duckett (2004) [ref. 45] |
Australia |
To identify the critical issues that impact on service delivery in rural hospitals |
In-depth interviews with hospital managers, chief executives, senior nursing staff and doctors (n=60) |
Department of Human Services categorises hospitals according to size related groupings A to E |
Large sample size for qualitative study. |
|
Kenny et al (2007) [ref. 46] |
Australia |
To identify rural nurses" perceptions of key issues related to the provision of effective psychosocial care for people with cancer in rural settings |
Focus groups with nurses (n=19) in rural hospitals (n=3) |
Department of Human Services categorises hospitals according to size related groupings A to E |
All-female sample. |
|
Lauder et al (2001) [ref. 62] |
Scotland |
To describe the care given by district nurses to patients with mental illnesses and the adequacy of relationships between specialist and generalist services |
In-depth interviews with district nurses (n=15) |
No definition |
Findings may not be generalisable to nurses in all rural areas as not all rural areas are geographically homogeneous. |
|
Leipert and Anderson (2012) [ref. 66] |
Canada |
To explore the use of photovoice to foster learning about and interest in rural locations and rural nursing as future practice settings |
Photovoice was used to take photographs that represented challenges and facilitators of rural nursing practice. Nursing students (n=38) |
Rural contexts are defined in Ontario as communities "with a population of less than 30 000 that are greater than 30 min away in travel time from a community with a population of more than 30 000" |
Authors state that students need to be sensitised to the fact that all may not be as it appears in a photograph, that continuous reflection, consideration of complexity and life and professional experiences and knowledge are needed to accurately understand and effectively work in the rural context. |
|
Lori et al (2012) [ref. 54] |
Ghana |
To determine the perceived barriers and motivators influencing final year midwifery students" acceptance of rural postings in Ghana |
Focus group interviews with final year midwifery students (n=49) |
No definition |
Authors state that it is unclear whether midwifery students in a more rural setting perceive the barriers and motivators for rural practice in the same way as those represented in the study. |
|
MacKinnon (2008) [ref. 58] |
Canada |
To describe the work nurses do when providing maternity care in rural/remote settings and to explore how interactions with women, healthcare providers and the rural community influence their work |
Observation and focus group interviews with nurses (n=48) |
No definition |
Authors state that the diversity of rural communities cannot be represented by studying one area in one Canadian province. Caution when transferring findings. |
|
Mills et al (2007) [ref. 42] |
Australia |
To explore rural nurses" experiences of mentoring and their multiple perspectives of "self" |
Semi-structured interviews with rural nurses (n=9) |
Rural/Remote and Metropolitan Areas (RRMA) classification |
Authors state that snowball recruitment attracted one participant who had not had any formal mentoring training. |
|
Mohale and Mulaudzi (2008) [ref. 56] |
South Africa |
To explore and describe the experiences of nurses working in a rural primary health-care setting in Mopani district, Limpopo Province |
In-depth interviews with female nurses (n=11) |
No definition |
Recruitment strategy not fully described. |
|
Montour et al (2009) [ref. 71] |
Canada |
To describe the nature of nursing work from the perspective of rural nurse executives and frontline nurses |
Semi-structured interviews with nurses (n=21) from different hospitals (n=7) |
Population size <100 000. Working definition of rural employed by the Ontario Ministry of Agriculture, Food and Rural Affairs used in the study |
Sample primarily older females with extensive nursing experience. Transferability of study findings limited. Insufficient information given regarding the researcher-participant relationship. |
|
Moszczynski and Haney (2002) [ref. 53] |
Canada |
To investigate stress and coping among northern rural nurses in relation to the transfer of trauma or accident patients |
Focus group interviews with nurses (n=19) from rural hospitals (n=3) |
No definition |
Authors state that the small sample size may have limited the range of experiences described. |
|
Newhouse (2005) [ref. 73] |
USA |
To explore the impact of legislative, strategic and organisational changes on nursing in rural hospitals since 1995 |
Focus group interviews with nurse executives (n=11) |
"Rural hospitals are located outside a metropolitan statistical area which has a large population base with social and economic networks" |
Insufficient information given regarding the researcher-participant relationship. |
|
Pront et al (2013) [ref. 67] |
Australia |
To understand what influences student learning in the rural clinical environment |
Semi-structured interviews with nursing students (n=7) |
No definition |
No in-depth description of recruitment strategy or data analysis. |
|
Robinson et al (2010) [ref. 68] |
Canada |
To better understand experiences and issues related to rural palliative care |
Focus group interviews with nurses, physicians, pharmacists and social workers (n=44) and palliative volunteers or family members of those who had received hospice care (n=20) |
Rural defined by "distance from an urban centre and population" |
Recruitment strategy not clarified. |
|
Rohatinsky and Jahner (2016) [ref. 63] |
Canada |
To explore perceptions, processes and organisational features of mentorship in rural healthcare |
Semi-structured interviews with seven female nurses. Two follow up interviews conducted to verify and confirm emerging concepts |
Rural defined as the local community population is less than 1500, but the facility serves an area of approx. 20 000. The nearest urban centre is 200 km away |
There is limited generalisability with this study as it was conducted in one rural facility with nurses only. Individuals whose relationships and experiences with mentors that were not successful may have chosen not to participate. |
|
Rosenthal (2005) [ref. 6] |
USA |
To describe the lived experience of rural generalist nurses who work in an acute care hospital with less than 25 beds, located in a mountain setting |
Face-to-face interviews with rural nurses (n=8) |
No definition |
The researcher and the storyteller are the same person, therefore only the researcher"s perception of the nurses" stories was represented. |
|
Sedgwick and Rougeau (2010) [ref. 64] |
Canada |
To describe events that influence undergraduate nursing students" sense of belonging during a rural hospital preceptorship |
Individual in-person and telephone interviews with fourth-year nursing students (n=12) |
Population size - rural communities designated as towns with a population of less than 9999 people |
Recruitment strategy unclear. |
|
Woodhouse (2010) [ref. 49] |
Australia |
To determine the understanding of nurses within a shared care model and the degree of interaction evident in their practice in the shared care nursing environment in a rural care setting |
Questionnaire sent to registered nurses with more than 5 years post registration experience in community health, palliative or aged care (n=6) |
No definition |
Small sample. Recruitment strategy unclear. |
|
Yates et al (2013) [ref. 9] |
Australia |
To explore and describe the experiences of working in the dual role as nurse and midwife in rural areas of Queensland, Australia |
Interviews with dual role nurses (n=8) |
No definition |
Authors state that midwives in different rural locations may have different experiences. |
|
Yonge et al (2013) [ref. 55] |
Canada |
To capture the experiences of preceptorship in a rural setting |
Photovoice study with preceptors (n=4) and students (n=4) |
No definition |
Recruitment strategy not fully described. |
|
Yonge et al (2006) [ref. 52] |
Canada |
To examine the experiences of fourth-year nursing undergraduate students and their rural-based preceptors |
Interviews with preceptors (n=26) and students (n=23) |
Statistics Canada defines a rural area as a place having a population of less than 1000 and a density of less than 400 persons per square kilometre |
Quality appraisal and analysis
Initial inter-rater agreement of the application of the quality appraisal was 85.7% (343 items in agreement of 400 CASP items (ie 10 CASP questions × 40 included articles)). The lowest agreement score (15%, 6/40 articles) was for CASP item 6 (‘Has the relationship between the researcher and participants been adequately considered?’). Discussion between reviewers identified differences in how this question was interpreted. Interpretation of the question was therefore discussed at a meeting of all four reviewers and agreement reached. Additional differences in assessment were resolved through discussion until agreement of 100% for all CASP items was reached (Table 3).
Most articles scored highly for quality critique (8–10). Whilst two scored lower – (5)49 and (6)50 respectively – this may have been due to lack of information reported in the article, rather than low quality. Most articles demonstrated clarity in data collection methods, ethical issues and data analysis. Only 10 out of 40 articles provided evidence of some reflexive practice such as the researcher critically examining their own role and potential bias during data collection6,51-53, an appropriate choice of location54, and a good collaborative researcher/participant relationship based on trust and researcher empathy55. Several authors described reflexive techniques such as feedback of emerging themes to the participants, which facilitated achieving credibility by ensuring confidence in the trustworthiness of the data42,51,56-58.
Thematic analysis identified three interrelated dimensions that influenced rural and remote nurses’ retention and migration decision making: ‘person/al’, ‘profession/al’ and ‘place’, with 18 inter-related domains. The dimension of ‘person/al’ contained five domains: a sense of belonging/connectedness, knowledge of rural culture, blurring of personal and professional lives, anonymity and job satisfaction/stress. The dimension of ‘profession/al’ contained eight domains: expert generalist, advanced nurse practitioner, professional isolation, mentorship, education, autonomy and empowerment, role conflict and recruitment and retention. The dimension of ‘place’ identified five domains: terrain and weather, fewer resources, geographical isolation, safety and rural culture. Tables 4 and 5 summarise the rural and remote nursing dimensions and domains.
Key quotations are highlighted below to exemplify the dimensions and domains of rural and remote nursing.
Table 3: Quality assessment summary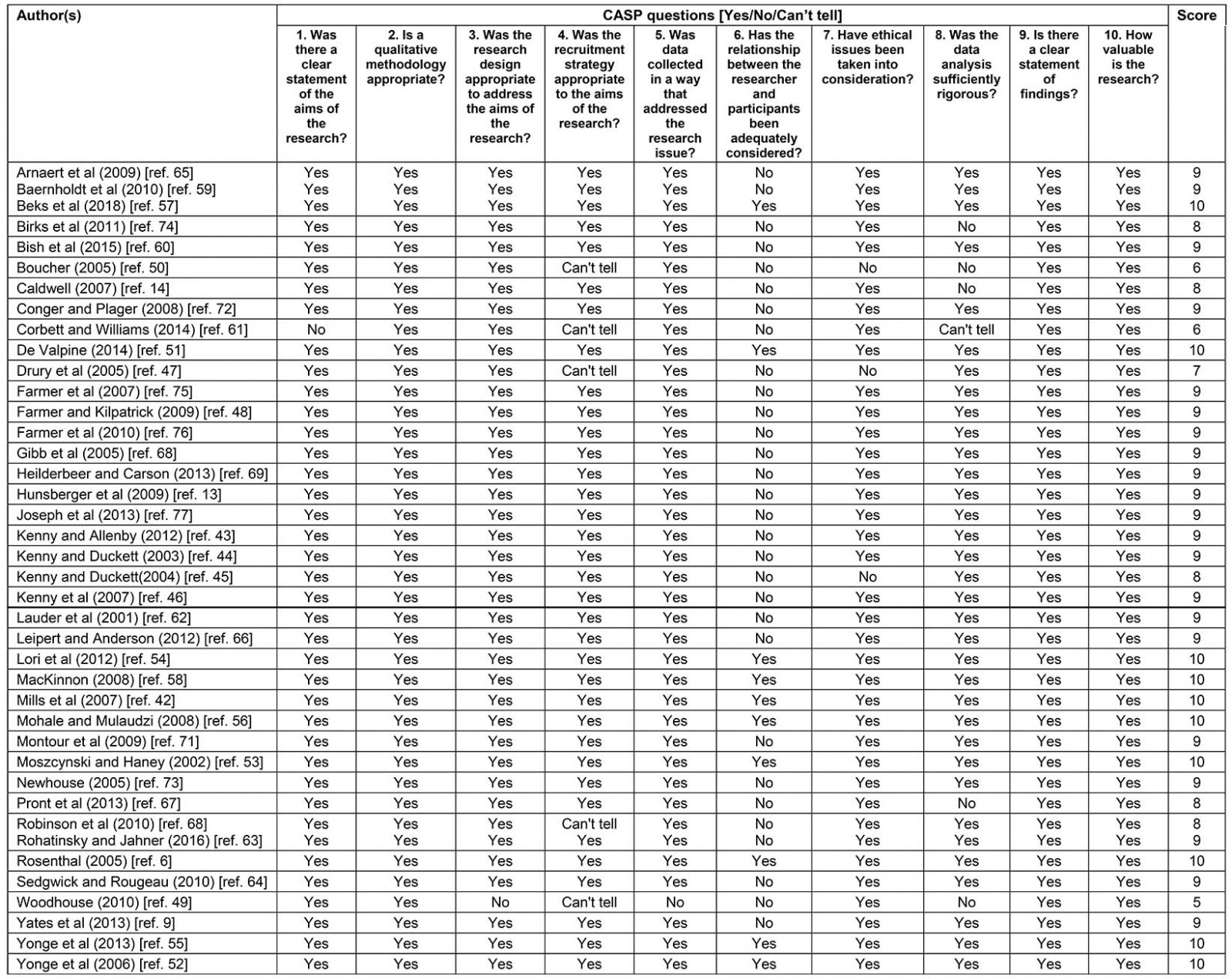
Table 4: Rural/remote nursing dimensions and domains
|
Author(s) |
Person/al | Profession/al | Place |
|---|---|---|---|
|
Arnaert et al (2009) [ref. 65] |
Lack of anonymity, role blurring, emotional isolation, stress |
Professional isolation, more education required, poor communication and inadequate team work. |
Limited resources |
|
Baernholdt et al (2010) [ref. 59] |
Community connectedness can be both a help and a hindrance |
||
|
Beks et al (2018) [ref. 57] |
Rural generalist nurses experienced a lack of confidence when caring for mental health consumers. Frustration as high workload obstructs altruistic practice. Lack of anonymity. Stress. |
Paucity of mental health education for rural nurses. Need for closer collaboration with the community mental health teams. |
|
|
Birks et al (2011) [ref. 74] |
Need for: |
||
|
Bish et al (2015) [ref. 60] |
Rich knowledge of rural life and culture |
Nurturing of professional relationships and empowerment is central to leadership skills |
|
|
Boucher (2005) [ref. 50] |
Qualities needed: flexibility, creativity, willingness to learn |
Need for more focus on mentoring and education |
Challenges of rural nursing: isolation, weather, terrain, distance, rural poverty, rural unemployment, difficult to access health care, and increased costs |
|
Caldwell (2007) [ref. 14] |
Being deeply rooted to family, mountains, culture and people |
||
|
Conger and Plager (2008) [ref. 72] |
Need to develop strong support networks
More education required to prepare advanced practice nurses for challenges of working in rural areas |
||
|
Corbett and Williams (2014) [ref. 61] |
Strong feelings of social and emotional connectedness - "knowing each other" and "feeling connected" are fundamental to the establishment of close relationships between carers and rural patients |
Nurses face challenges around maintaining appropriate professional boundaries |
|
|
De Valpine (2014) [ref. 51] |
An independent sense of family and childrearing. |
An intense appreciation of Native Alaskan culture and environment |
|
|
Drury et al (2005) [ref. 47] |
Challenges with clinical confidence and self esteem |
Professional isolation |
Safety issues |
|
Farmer et al (2007) [ref. 75] |
Perceived "distance" between senior managers imposing change |
Distance to urban units |
|
|
Farmer and Kilpatrick (2009) [ref. 48] |
Engagement in a range of community activities enables physical/psychological health benefits that boost confidence |
Mentoring |
|
|
Farmer et al (2010) [ref. 76] |
Tensions in management approach |
||
|
Gibb et al (2005) [ref. 69] |
Advancing age seen as dis-enabler to education |
Nurses recognised personal benefits of change through embracing learning and mentoring |
Geographical distance, time and cost seen as dis-enablers to education |
|
Heidelbeer and Carson (2013) [ref. 70] |
Higher incomes and more time off with fly in fly out rural nursing |
Difficulty accessing professional development/education |
Harsh climate |
|
Hunsberger et al (2009) [ref. 13] |
Commitment to colleagues, patients and community |
Lack of resources, support and influence to manage negative situations |
Security issues when working at night |
|
Joseph et al (2013) [ref. 77] |
Weather related illness and injury leading to staff absenteeism and increased workloads |
||
|
Kenny and Allenby (2013) [ref. 43] |
Psychosocial care more difficult due to staff and clients knowing each other well outside the clinical setting Psychosocial care is significantly undervalued |
Lack of collegial relationships amongst staff Issues around "culture" of organisationProfessional isolation |
|
|
Kenny and Duckett (2003) [ref. 44] |
Diversity of nursing practice in rural hospitals Lack of university education amongst rural nurses |
||
|
Kenny and Duckett (2004) [ref. 45] |
The rural hospital remains the symbol of the social power of medicine but nurses forced to do things that were outside their scope. Notion of advanced nurse practitioners was an extremely controversial subject |
||
|
Kenny et al (2007) [ref. 46] |
Lack of confidence and emotional exhaustion |
Rural nursing is characterised by diversity multiskilled generalists lacking specialist knowledge |
|
|
Lauder et al (2001) [ref. 62] |
Blurring of personal and professional lives |
Feelings of being unsupported in multiple roles |
Nurses have a unique position within the community. Appreciation of rural culture |
|
Leipert and Anderson (2012) [ref. 66] |
Less stress as slower pace of life Blurring of boundaries between personal and professional life Insider/outsider status |
Facilitators noted as increased autonomy, the generalist role and advances in technology |
Strong sense of community/culture |
|
Lori et al (2012) [ref. 54] |
Although participants voiced a strong desire to help others and to save lives, they also expressed a deep concern for their own quality of life |
Lack of staff |
Concerns about unacceptable housing accommodations, no access to potable water, impassable roads, no transportation, non existent schools, poor support structures and poorly equipped hospitals |
|
MacKinnon (2008) [ref. 58] |
Complexity of rural nursing |
||
|
Mills et al (2007) [ref. 42] |
Emotional impact of interactions in the course of nursing from "the womb to the tomb" |
Expert generalists - "we"re not specialists in anything but have to deal with anything that comes through the front door" |
Sense of close community/culture |
|
Mohale and Mulaudzi (2008) [ref. 56] |
Emotional and physical strain as a result of the shortage of human resources |
Retaining nurses is a problem |
|
|
Montour et al (2009) [ref. 71] |
Ageing workforce - anticipation of a substantial increase in retirements during next decade |
||
|
Moszczynski and Haney (2002) [ref. 53] |
Sadness of stress, anger and difficulty in keeping professional life from encroaching on personal life |
Tension due to the lack of communication and support |
Geographical isolation |
|
Newhouse (2005) [ref. 73] |
Distinctive challenges for rural nurses - patient population, legislation, technology, staff shortages, cultural differences between staff, physicians and patients, nurse-physician conflict and maintaining competency |
Physical isolation |
|
|
Pront et al (2013) [ref. 67] |
Relationships between staff, students and patients meant an intertwining of professional and private lives |
Promotion of learning through supportive preceptorship has the potential to aid retention of nurses in rural areas |
Unpredictable nature of rural environment |
|
Robinson et al (2010) [ref. 68] |
Strong sense of pride in being able to "make it work" for patients |
Dual relationships leading to numerous ethical challenges |
Social solidarity, close-knit relationships, culture and community commitments were strengths of rural communities |
|
Rohatinsky and Jahner (2016) [ref. 63] |
Lack of anonymity |
Expert generalist - multiple hats |
Limited resources |
|
Rosenthal (2005) [ref. 6] |
Lack of anonymity |
Rural nurses need to assume the role of expert generalist and function as "jack-of-all-trades" |
|
|
Sedgwick and Rougeau (2010) [ref. 64] |
Stress |
Fear of being observed or making an error or mistake |
|
|
Woodhouse (2010) [ref. 49] |
Confusion around role, skills, communication and care planning |
||
|
Yates et al (2013) [ref. 9] |
Stress |
Nurses recognised the importance of being a multi-skilled generalist in rural areas Concerns that midwifery skills could be eroded due to diminishing work available |
Experiences of nurses are shaped by location/culture. Limitations of working in rural hospital |
|
Yonge et al (2013) [ref. 55] |
Confidence and personal bonds can be fostered through preceptorship |
Mutual professional development through preceptorship |
|
|
Yonge et al (2006) [ref. 52] |
Students expressed their enjoyment of the "family feel" that coincides with a rural hospital - majority of students requesting a rural placement originated or grew up in smaller towns |
Lack of technology and lack of academic support |
Adverse weather |
Table 5: Rural/remote nursing dimensions summary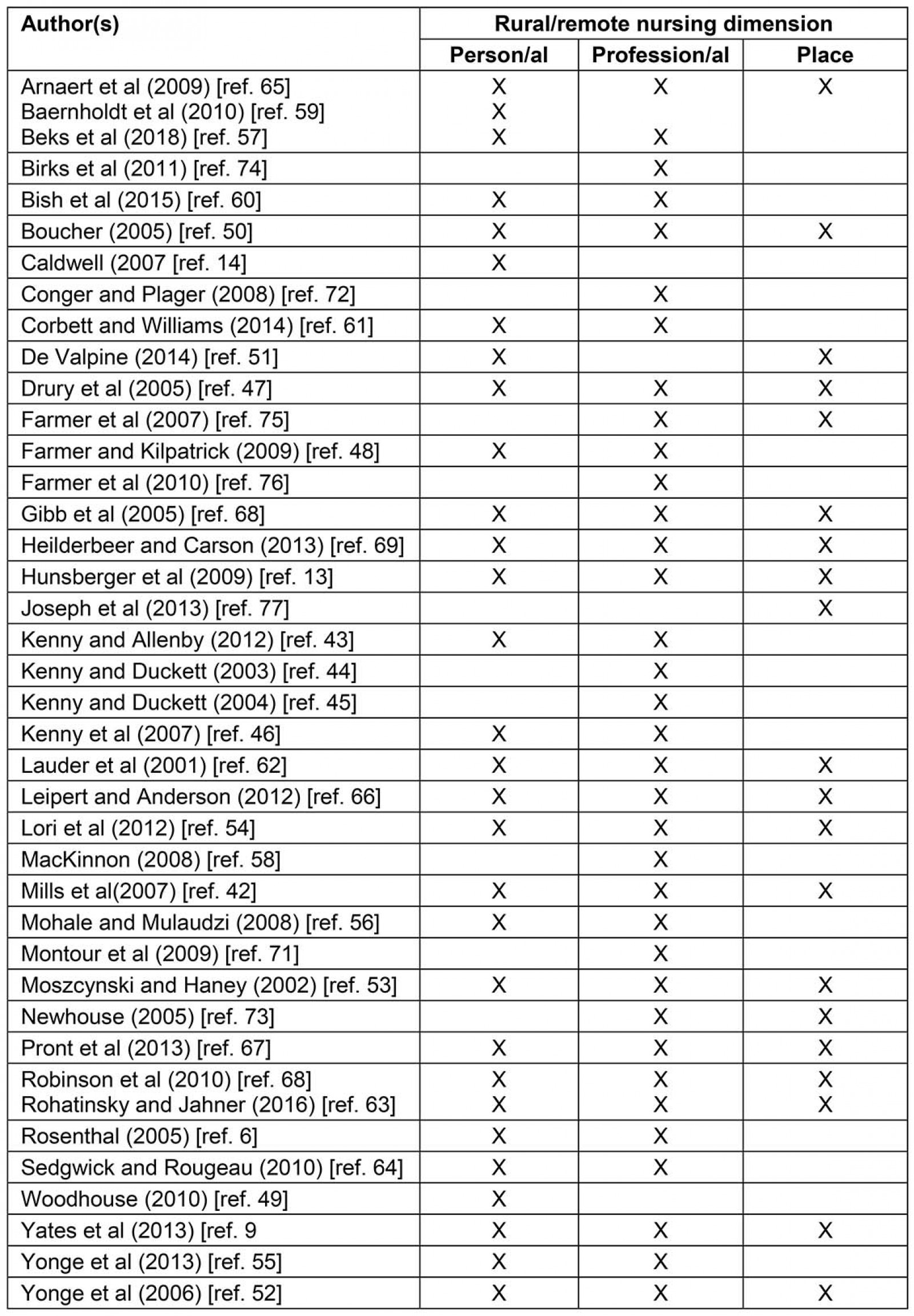
Person/al
Sense of belonging/connectedness: Previous exposure to rural or remote life, or previous work experience in the country, were the most compelling reasons influencing the attraction of some nurses to rural and remote areas6,13,14,42,51,59-64. There was a sense of people returning to their roots:
I’m going back to the rural setting ... I’m a farm girl. I was born and raised in a small community and I'm headed back ... I’m going to be a rural nurse. (Canada)52
Knowledge of rural culture: The culture of rural and remote regions was cited in several articles14,42,43,51,52,59,60 as a major aspect of the nurses’ practice and motivation to stay in the region. The community ethos influenced nurses:
I had met some Alaskan Native people as patients and felt a love for them, appreciating their conduct, learning about their lives. (USA)51
Blurring of personal and professional lives: Several studies pointed towards the advantages and disadvantages of familiarity between patients, professionals and the community13,42,43,46,53,61-63,65-67 and the potential blurring of personal and professional lives:
Patients do like to bring personal information into the conversation perhaps about a neighbour and as patients may know of others being visited by the same nurse they may ask for an update – that is when I become very professional and try to point out that I can’t tell Mrs Jones about their medical situations or what we do for them. (Wales)61
Anonymity: The challenges of maintaining anonymity were highlighted in several articles6,42,50,57,63,65:
I suppose in a rural community … everything that you do has more of an impact. Like, if you have a relationship or if you have a problem here everybody knows about it. It becomes more of a problem because it’s so … well advertised … If you were an anonymous person in an anonymous setting you really wouldn’t care for a start, but probably no one else would care either … It wouldn’t become everybody’s sort of knowledge. (Australia)42
Job satisfaction/stress: Generally, there was a strong sense of pride in being able to ‘make it work’68 for patients through the provision of responsive, creative, highly individualised care9,13,42,46-48,51-57,63-66,69,70. The interplay with a sense of community belonging contributed to enhanced job satisfaction. Rural nurses expressed emotions such as sadness, anger and feelings of hopelessness due to being overburdened56. Having to maintain a broad range of skills was considered as both a stressor and a motivator to continue learning9,13. Seeking mutual social support from colleagues was a frequently used strategy:
I think nurses must get rid of that kind of sadness of stress by talking to each other – we’ve really only got each other – we need to do that. (Canada)53
Profession/al
Expert generalist: The need for rural and remote nurses to be multiskilled was identified as a recurrent theme6,9,42-44,46,47,51-53,57,58,62,63,66,71. Due to the diversity of the work and a lack of resources and facilities often the nurse became a jack of all trades, prepared and willing to undertake many different tasks:
You took care of a lot of the stuff – plane crashes, burns victims, cardiac, kids. (USA)51
We’re not specialists in anything and we can have anything appear at the front door. I feel that we are fighting for survival … you don’t do things enough to be skilled. (Australia)42
Advanced nurse practitioner: In order to address the complexity of the generalist role, several studies supported the view that advanced nurse practitioners provide high quality services in rural settings44,45,47,72-74:
There is definitely work for a nurse practitioner. To have someone with those sorts of skills would be fantastic but, really, we can’t get any nurses. At the moment anyone would do. (Australia)44
Professional isolation: A number of studies cited professional isolation as a part of everyday experience in rural and remote nursing6,13,43,47,52,53,57,58,63,65,70.
I am the trauma team. (Canada)13
… sometimes you just want another midwife to say ‘Oh, what do you think?’ you know. (Australia)9
Professional isolation remained one of the most concerning aspects of rural work. Nurses experienced difficulty finding help when confronted with unfamiliar situations, and the need to become resilient and overcome fears was articulated:
I had to stop crying and realise that maybe I can do this … I can settle down and do this. (Australia)70
Mentorship: Mentoring was described as one strategy used to retain novice rural and remote nurses and to combat professional isolation42,46,48,50,55,62,63,67,69,70,72. The lack of an onsite mentor described as ‘another pair of eyes’ challenged nurses and led to a sense of loneliness and isolation72. For rural nurses, working in a close-knit setting, the support of colleagues and managers is crucial:
Just the ability to be able to sit down and say, I did this really well or I did this really badly and want to talk about it. (Australia)46
Education: Studies considered the significance of education for rural and remote nurses13,42,44,47,50,52,54,57,58,62,63,65-70,72,74 with some highlighting professional isolation as the main factor leading to difficulty in accessing education, resulting in deskilling13,70.
It is hard to maintain skills that you are not using all the time … it makes it a little scary. (Canada)13
Rurality and remoteness were considered a barrier to continuing professional development:
Due to isolation, nurses experience limited access to continuing education, interaction with healthcare professionals, and resources to provide care. (Canada)66
Autonomy and empowerment: Several studies described autonomy and decision making as core characteristics of rural nursing practice, bringing difficult but rewarding challenges47,60,66. These challenges, such as trying to provide proper care with limited resources and professional support, appeal to some nurses:
Autonomy is a facilitator because it can enhance nurses’ problem solving skills and innovations in their ability to find solutions to a lack of resources … and professional support. (Canada)66
Role conflict: Professional conflict was reported in some of the articles6,9,43,45,53,58,62,73,75,76 and the lack of collegial relationships amongst staff in the rural context was identified as a barrier to effective working:
How do we provide great psychosocial care to clients if we can’t provide psychosocial support to each other? ... You’d even see them looking at the roster … they’d say oh no … I’ve got to work with her … (Australia)43
Some nurses believed that they were required to defend the patient care they had provided when dealing with their counterparts in an urban hospital, and cold and judgemental responses from nurses working in larger settings were recounted:
I am often left feeling angry when those guys come and scoop your patients up and spend an hour criticising your care … it is very, very frustrating … Will those receiving him down South respect your efforts, see you as professionally competent … I’ve always felt that the nurses in the North had to be twice as good as the nurses in the South … I guess it’s some sort of geographic insecurity. (Canada)53
Recruitment and retention: The sustainability of rural nursing is threatened when nurses lack resources, support and influence13. Demographic trends, such as the ageing nursing workforce, exacerbated this situation:
It’s only going to get worse ‘cause you figure they’re telling us there’s at least half of us right now that given the next 10 years could retire. Well you’re already short now and you get another half going out the door? (Canada)71
Place
Terrain and weather: The physical geography that challenges rural and remote nursing practice was described in several articles50-53,66-68,70,75,77.
Some nurses considered that:
Getting in and out of the area is difficult. There is no road system … you can’t get out of here …. (USA)51
We have had times when ambulances have been stuck in our laneway or ice storms, that kind of stuff, where you don’t have the availability of quick response or a snowplough to help out. In the winter it can be a detriment. (Canada)77
In the Highlands of Scotland, travelling on poor roads impacted on emergency calls and travel, and for island populations this was further challenged by unpredictable seas:
We are just too remote. If there wasn’t the stretch of water between us and the mainland that might be different, but there is and there always will be. (Scotland)75
Fewer resources: Fewer patient resources were described in some rural and remote communities9,50,51,53,54,63,65,68,70,73,75, including those requiring specialist services such as mental health and drug addiction, which further compounds the challenges of treating a disadvantaged population73. A lack of local support structures resulted in patients being referred to better equipped facilities54.
Poor resources also impacted on nurses’ lives and might preclude them from accepting permanent positions in a rural or remote area:
They gave me this place to live in. It hadn’t been cleaned, had almost no kitchen, the television didn’t work, the washing machine didn’t work, there was no ironing board. It’s a basic level of accommodation (Australia)70.
Geographical isolation: Geographic isolation50,51,53,54,63,65,66,68-70,73,75,77 and the fragility of life were highlighted by nurses:
Life is fragile out here – the isolation. (USA)51
More positively, geographical isolation was also considered a source of restoration as nurses enjoyed the slower pace of life in rural and remote communities, which resulted in less stress:
Remote areas are less contaminated by … garbage … you’ll be in awe of the power and beauty of nature. (Canada)66
Safety: Some nurses cited personal safety as being a concern13,47,51,53,54,66,68,70,77. Nurses described lone working without security personnel in the evening:
There are four of you in the whole hospital and we don’t like people to know that because we are very much at risk. (Canada)13
Rural culture: A desire to have a level of immersion into the culture of rural and remote communities influenced nurses personally60. In several studies the culture was a major aspect of the nurses’ motivation to stay in a rural or remote region6,9,42,48,51,60,62,63,66,68. For example, nurses portrayed an intense appreciation of Native Alaskan culture and environment:
I love the Native population here. I like this community. It’s beautiful, it’s abundant with salmon … a moose rack … a haunch of caribou … (USA)51
Explaining the cultural complexities of rural and remote communities such as the accepted norms and practices is integral to cultivating and growing new novice nurses42.
MacKay’s 3P model
Data synthesis informed the development of MacKay’s 3P model of factors influencing rural and remote nurses’ decision making (Fig2). The model provides a theoretical framework to explore the complex interplay between the person/al, profession/al and place-related dimensions of rural and remote nursing and capture the complex phenomenon of the factors that influence nurses’ decision making to remain or leave rural and remote areas.
 Figure 2: MacKay’s 3P model of factors influencing rural and remote nurses’ decision making.
Figure 2: MacKay’s 3P model of factors influencing rural and remote nurses’ decision making.
Discussion
This systematic review and thematic synthesis highlights the complexity of factors that influence nurses to work in rural and remote locations. Examples are the influence of family ties and connections (personal), appreciating the local culture (place) and accepting the flexibility required to adapt to whatever the immediate healthcare needs may be (professional). Being part of a team, job satisfaction, a rural lifestyle, a sense of belonging and being part of a culture that supports education and learning through mentoring had a positive effect on the retention of rural and remote area nurses. Professional isolation, lack of anonymity, challenges in maintaining continuous professional education, fewer resources and fears for personal safety were the main negative findings of the review. These findings were used to develop MacKay’s 3P model, which provides a graphical representation of three distinct but interrelated dimensions of rural and remote nursing: person/al, profession/al and place. The review also highlighted the fluidity of the domains and dimensions, recognising the interrelated nature of factors affecting nurses’ experience and decision-making to work in rural and remote areas. Despite clear connections between these three dimensions, few articles have explicitly considered this interplay. Around a quarter (11/40) of the articles only focused on one dimension. Of those that considered more than one dimension these were generally treated in isolation. Whilst these connections were not explicitly made within individual articles, the authors’ analysis across the studies has highlighted and described multiple relations. MacKay’s 3P model illustrates the complexity and interplay of the person/al, profession/al and place-related dimensions of rural and remote nursing.
This review found that there are no universally accepted definitions of ‘rural’78. Less than half of the articles included in this review presented a definition of the term ‘rural’. Of those, half used census or other administrative data defining rurality in terms of population distribution across land mass, whereas the other half used bespoke definitions based on a nurse’s role78. There is a need for authors to explicitly report the definition of a rural area used in their research79. Of the 15 Australian articles included in the review, only seven presented a definition of ‘rural’ and only one of these articles considered remote nursing70. The three remote nursing articles included in the review51,70,74 were retrieved using the search term ‘rural nurs*’. By applying the search term ‘remote nurs*’ no qualitative remote nursing research articles were retrieved. This further clarifies that in addition to the paucity of remote nursing qualitative research is definitional complexity around the terms ‘rural’ and ‘remote’. The categorisation of articles within databases did not differentiate between rural and remote – all were classified as rural. Of the three articles considering remote nursing two were set in Australia (remote Queensland)6,9,74 and one was set in USA (south-west ‘bush’ Alaska)51, all focusing on nursing experiences in delivering care in indigenous communities.
Implications for research, policy and practice
Findings from this review suggest three key implications for further research, policy and practice. First, to support further research in this area consensus should be reached around the terms ‘rural’ and ‘remote’. There is a need for more clarity whereby authors should explicitly report the definition of a rural or remote area used in their research. It is methodologically important80; for example, in order to more accurately assess the rurality of a community it may be more appropriate to include both quantitative (ie distance and population size) and qualitative criteria (ie community relationships, individual attitudes). Often ‘remote’ and ‘rural’ are used together without a clear understanding about the distinction between the two. The concept of rural or remote is complex, variable and evolving80. The small but growing literature around remote health recognises that recruitment and retention issues arise as remote populations are smaller, more isolated and more highly dispersed – often relying on visiting services (fly-in fly-out)70. Due to the multidisciplinary and generalist nature of practice in remote settings, policy-makers and planners are mandated to direct resources and programs such as the preparation of specially credentialed remote area nurses to address the health needs of populations in these areas81. Second, policy-makers involved in developing recruitment and retention strategies should consider how the key factors that influence nurses’ decision-making to work in rural and remote areas, identified here, can be incorporated into campaigns to attract and retain nurses in these areas. The review highlights some of the many advantages for nurses working in rural and remote settings that could be emphasised in recruitment approaches or marketing materials. Some describe the opportunities available for them to step up in challenging situations, make leadership decisions and have more than one role. Evidently nurses who choose to work in rural and remote settings do so because of a combination of factors, and an understanding of their experiences and decision-making can help devise effective recruitment and retention strategies for this workforce at a time of global nursing shortages. Finally, the literature has only begun to explore the connections between the person/al, profession/al and place-related dimensions of rural nursing and, whilst this article goes some way to highlight and describe the complex interconnections, further work is needed to fully understand the complexity of nurses’ experiences of working in rural and remote settings and examine the interplay between the factors in MacKay’s 3P model. Specifically, as most articles included a snapshot of nurses’ experiences at a single moment in time, there is a particular need to understand nurses’ experiences over time. In this way the complexity of the decision-making process and implications of decisions made to work in rural and remote settings will be better understood over the course of a career.
Unanswered questions and future research
This article has identified the many factors that influence nurses’ decisions to work in rural and remote areas. A model of factors that influence nurses’ decision-making to work in rural and remote areas has been outlined that can be used by policy-makers to shape targeted recruitment and retention strategies and serve as a framework for future research in this field. However, in the face of global nursing shortages, which have a disproportionately negative impact on remote and rural areas, this review shows that further research examining the interplay between the personal, professional and place-related dimensions of rural nursing is required. (Auto)biographical narratives have been used by health researchers to enable participants to understand the flow of their lives through time and space, and the interrelation between the two82. Using autobiographical (or life history) approaches in rural nursing research may help to uncover nurses’ rationale for their career decisions in the context of the relationships with people and places in which they were made. Through narrative, life stories are appropriate for understanding a lifetime of occupational experiences and for appreciating the personal, professional, social, economic, historical and geographical influences that shape these experiences83.
Strengths and limitations
This appears to be the first systematic review and thematic synthesis to explore the evidence around the dimensions and domains that influence nurses’ decision-making and experiences of working in rural and remote healthcare settings. Studies were generally of a high quality, perhaps reflecting the use of qualitative reporting guidelines such as COREQ-32 (consolidated criteria for reporting qualitative research)84. Notwithstanding the use of the CASP tool40, quality appraisal retains a degree of subjectivity, and although all articles were critically appraised and scored by SCM and then independently scored by a second reviewer (AS, RGK or MB) it is possible that other researchers may have appraised the quality of the studies in a different way. Only English language articles were included, and thus the findings of this review may have limited relevance to countries where English is not widely spoken. Although limited, due to the inclusion of only three qualitative remote nursing articles, this review has highlighted that the dimensions and domains of rural nursing seem to be synonymous with those of remote nursing. There is a scarcity of international qualitative remote nursing research evidence to enhance understanding of nursing in more isolated and remote settings.
Conclusion
This review identifies the factors influencing nurses’ decision-making to remain in or leave areas of remote and rural work. To date, there is a paucity of qualitative rural nursing research undertaken in the UK, a lack of explicit definitions of rural and remote nursing in many studies, and a tendency to examine factors in isolation. MacKay’s 3P model highlights the multiple and complex factors at play that guide nurses’ decisions to remain in or leave rural and remote settings. This three-dimensional model (person/al, profession/al and place) will aid policy-makers to tailor recruitment and retention strategies for rural and remote areas. However, further research that examines the complex interplay of these multiple factors over time is required to inform action to enhance these strategies to address the global shortage of nurses in rural and remote settings.
References
You might also be interested in:
2021 - Grey nomads with diabetes self-management on the road – a scoping review



