Introduction
Australia in the 21st century is a time of population ageing and a revisioning of what it means to be older, evidenced as increased longevity, high levels of disposable income and embracing of active healthy lifestyles1,2. While new models of ageing are emerging that highlight productivity and capacity, there continues to be a growth of chronic illness in the Australian population, specifically diabetes mellitus (type 1 or 2), where the incidence of this condition has tripled over the past 25 years2. This scoping literature review explores the characteristics and behaviours of a subset of Australia’s older population: grey nomads, many who live and travel with diabetes. Grey nomads are people older than 55 years, who travel in caravans or motorhomes for extended periods of time around Australia3-5. Grey nomads are challenging the established view of ageing in Australia by their lifestyle choices, which include social and economic contribution, independence and furthering of personal fulfilment6,7. Some evidence suggests that grey nomads experience health issues while in rural locations and that there is a significant burden on an already under-resourced rural health services8,9. Specifically, this review seeks knowledge on grey nomads self-management of diabetes while travelling, with the aim of understanding their experiences and identifying support services that facilitate improved self-management. This scoping review is guided by the six-step process recommended for methodological soundness by Levac et al10.
Background
The phenomenon of an ageing Australian population is a dominant challenge to Australian society, government and fiscal wellbeing11,12. Australia's ageing population is attributed to ongoing low birth rates, an increase in life expectancy2 and is consistent with demographic changes in most developed countries13. From 2020 and beyond, Australia has fewer children under 15 years, and an increase of people aged 65 years and older2. Population demographics influence demand for support, services and infrastructure and exert a significant and evolving pressure on government fiscal policies and planning14.
Much of the planning and understanding of future health service requirements is grounded in prevailing views of population cohorts and aims to match population needs with services and infrastructure12.
Of relevance to this article is the pervasive view of post-retirement as a time of dependence and burden, which has evolved from the characteristics of the pre- and post-war generations. However, this view fails to recognise the positive and changing social script of ageing occurring in the 21st century, epitomised by the grey nomads who travel independently seeking destinations and experiences for extended periods of time, often despite personal limitations of health and finances7.
Australians are embracing the grey nomad lifestyle in rapidly increasing numbers, and this cohort is estimated to be 28% of the Australian domestic tourism population15. The COVID-19 pandemic has seen the overseas tourism market, valued at over A$65 billion, grind to a halt in Australia16-20. It is likely in the post COVID-19 era that domestic tourism including the grey nomad population will rapidly increase, along with a concomitant demand for services in rural and remote locations of Australia21. Grey nomads are known to have an incidence of chronic disease consistent with that of the general population22, and understanding the characteristics, social and health needs of this mobile group of older travellers is imperative to fostering continued healthy ageing on which local, state and national government planning and service provision can be based. Of specific interest to this review are the experiences and capacity of grey nomads with diabetes to self-manage when in remote locations, where services and support are often limited.
Methods
Scoping review
Scoping reviews are relatively new to the field of literature reviews and have seen increasing popularity as they serve the combined purpose of summarising current health knowledge, clarifying a specific research question and identifying gaps in the literature10. The method was first proposed by Arskey and O’Malley23 and has been clarified and strengthened by a number of authors10,24,25. The methodology, now recommended as a six-step framework10, has framed the processes of this review.
- Identifying the research question and aim
- Identifying relevant literature
- Selecting studies
- Charting the data
- Collating, summarising and reporting results
- Final consultation
Valaitis et al26 state that methodological rigour of a scoping review is enhanced with a research team from diverse disciplines26. To enhance the rigour of this study, the research team included nurse practitioners, diabetes nurse educators, nurse researchers, a medical student, a pharmacist and community representatives, all bringing their diverse understanding and perspective of the research topic. The review process commenced with a clear identification of the topic of interest under a population, concept and context framework, which guided the scope, processes and objectives of the review.
Identifying the research question and aim
The population of this review were Australian grey nomads with diabetes who travel independently in their own caravan or motorhome for extended periods of time. The concept and context of interest were self-management of diabetes while travelling, and travelling in rural remote areas of Australia. Flowing from the now identified framework, the developed research question of this scoping review was:
What are the self-management behaviours of grey nomads with diabetes when preparing for and travelling through rural and remote locations of Australia?
Identifying relevant literature
Key words are an integral part of developing a search strategy that explores the literature and in this review included ‘grey nomads’, ‘diabetes mellitus’, ‘self-management’, ‘rural and remote locations’. Key words inform the development of search terms, which were separated into three search concepts and variants (Table 1).
After key words and field limiters had been identified, the search commenced. Separated by the three search concepts, the search included the healthcare specific databases of Medline, Cumulative Index of Nursing and Allied Health Literature (CINAHL), Scopus and Ageline. The population of this study for concept 1 (grey nomads) was a straightforward search with limited search results. However, concept 2 (phenomenon of interest: diabetes and self-management) identified a large number of articles. After all relevant literature had been identified, the research team reviewed the studies for final inclusion. Figure 1 identifies the search process and outcomes.
Table 1: Distribution of retrieved articles by concept, theme, subthemes and authors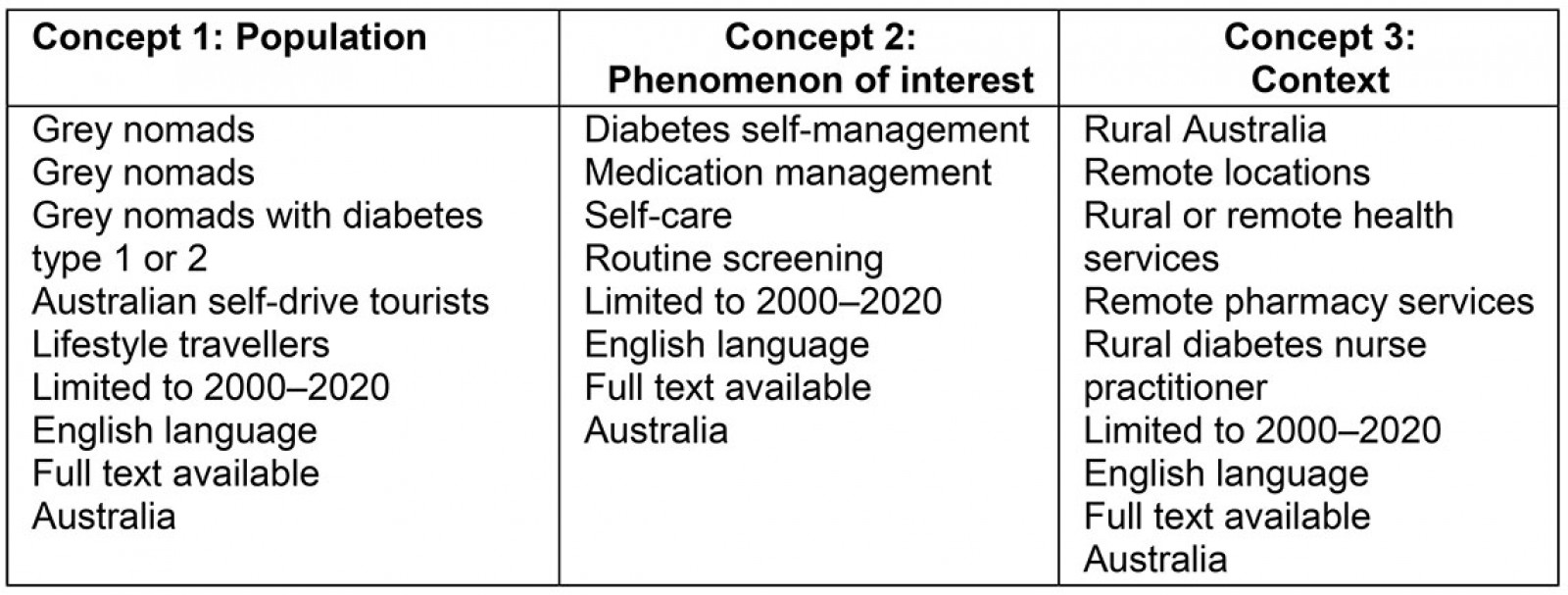
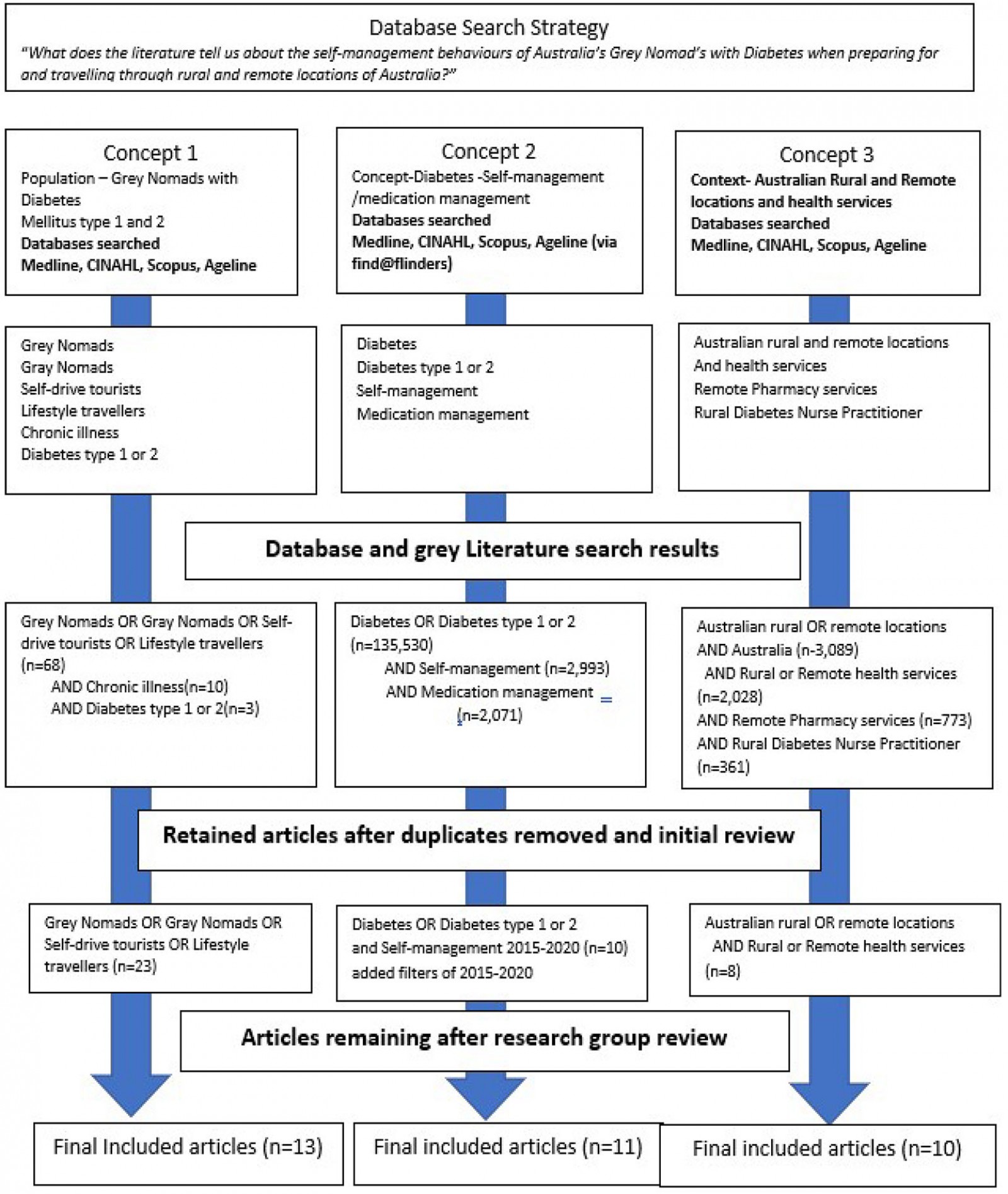 Figure 1: Search strategy and outcomes
Figure 1: Search strategy and outcomes
Selecting studies
On completion of the search, 41 articles were identified for inclusion. Consistent with the methods of a scoping review framework, the identified articles were sent to members of the research team to review. Of the 41 articles retrieved, seven were excluded based on limited relevance to the identified research concepts. The remaining 34 articles were scrutinised for clarity of content23,26. Table 2 displays the distribution of the articles across the concepts and themes. Note that some articles spanned more than one concept.
Charting the data
Mapping of the data is a crucial step in the analysis of the included literature. In this review, it was guided by the process described by Rosas and Kane for enhanced representational validity and reliability27. Concept mapping provides the methods for rigorous reduction, organisation and interpretation of large volumes of data28 into a display of the interconnectedness of the parts of the overall concepts. Where very large numbers of articles on a topic exist, coalescence of concepts is a synergistic process that makes sense of the vast and disparate data obtained. The analysis of the data of this review was aided by the use of NVivo v12 (QSR International; https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home), where themes and subthemes were identified and coded across all retrieved articles (Table 2).
Collating, summarising and reporting results
Concept 1 described the grey nomad population, their characteristics and motivation. Concept 2 focused on self-management of diabetes and identified aspects considered to be barriers to diabetes self-management. Concept 3 contextualised the Australian rural and remote locations. This provided insight into the unique and relevant context that had a major impact on grey nomads’ capacity to self-manage their diabetes, as it was an environment where healthcare services were limited, and help was often not accessible.
Results
Who are the grey nomads?
All articles provided a definition of ‘grey nomads’ as travellers aged more than 55 years who were travelling for extended periods of time independently in a recreational vehicle, caravan, motorhome or campervan. This cohort, constituting 2% of the total Australian population4,22 frequently stayed in some of the most remote locations within the vast Australian hinterland3-5,7,9,22,29-33.
Grey nomads were considered heterogeneous and mostly heterosexual white Anglo-Australian couples who were retired from the workforce. It was also reported that most grey nomads lived with at least one chronic health condition including diabetes4,9,32,34,35.
Grey nomads did not consider themselves as ‘tourists’, but as lifestyle travellers who sought personal freedom and valued the ethos of privacy, individualism and environmental responsibility4,9,32,34. Many sought warmer climates in the colder months, often travelling long distances to very remote areas where campsites chosen offered privacy, isolation, self-sufficiency and a closeness with nature30,32,34. The journeys undertaken by grey nomads varied in length from a few weeks to many months or years. Pickering found experienced grey nomads considered themselves to be in a state of ‘continual and continuing journeying’, interrupted briefly with stays at home32.
Grey nomads were found to generally travel for long periods, seeking experiences rather than destinations, with an estimated 20% of grey nomads travelling continuously for more than 2 years7,30. Australian grey nomads’ motivation was attributed to a desire to seek life- and health-enhancing experiences7,30,32, avoiding organised tours or resort style accommodations. They frequently sought rural and remote locations and aspired to healthy lifestyles and choices1. While grey nomads’ motivation was often seen as travel for health2,30,32, studies identified an incidence of chronic illness that aligned with the broader Australian population3,22,29. Despite the estimated incidence of chronic disease in the grey nomad population, a pre-existing illness was not considered a barrier to adopting the lifestyle and it was estimated that 8% of the grey nomad population lived and travel with diabetes33.
Grey nomads and health
Compounding the presence of chronic disease, extended travels by grey nomads often exhausted their physical capacity in environments where healthcare support and services were limited and the impact of transient populations added a significant burden to local communities and services3,9,22,33. Grey nomads were found to hold a belief that their lifestyle kept them active, healthy and exerted a positive influence on their mental health22. However, Halcomb et al identified that approximately 8% of the study population returned early from travel due to ill health22. Other studies described grey nomads seeking health services from local providers3,9,33. This finding concurred with the experiences of diabetes educators in rural or remote areas5. While the grey nomad journey offered the opportunity for a healthy lifestyle, grey nomads were found to have a higher than recommended consumption of alcohol, higher levels of obesity and a lower-than-average quality of life score across both the physical and social relationship domains22.
Grey nomad preparation for travel
Many grey nomads spent long periods of time planning their trip, destinations, equipment and the supplies required4,32. However, planning for health and healthcare requirements was found by a number of studies to be limited or inadequate3-5,9,22,30,31,33. This inadequate preparation resulted in high utilisation of local health services and was most evident in the lack of adequate medication to last the trip9,22,33. Healthcare summaries were rarely carried5 and the use of technology for health information transfer was suboptimal due to poor uptake of such technology in the grey nomad population22. Conversely, some studies identified that grey nomads were aware of the need for health preparedness and sought advice from their local healthcare practitioner prior to travel, which included a health summary and adequate medications for the journey3.
The need for preparedness was evident in the findings of Obst et al that 21–32% of grey nomads experienced a medical emergency while travelling31, and a lack of access to healthcare services in remote locations often led grey nomads to seek assistance from local emergency services, which often struggled to accommodate the influx of transient older populations4. The capacity of grey nomads to manage their chronic conditions was challenged by poor access, fragmented health care, limited resources for medications and a reliance on self-awareness to identify deteriorating health conditions3,5,35.
The sparse literature concerned with grey nomads with diabetes failed to answer the question of this review and it was identified that the choices and destinations grey nomads made, coupled with the incidence of chronic disease, placed the responsibility and self-management of health and health care almost solely with the grey nomad. Thus, it was important for grey nomads and healthcare professionals to have a clear understanding of the characteristics and tools required for effective self-management. This need was especially important for people with diabetes where care and management were constant and lifelong, and where poor self-management can lead to the early development of associated complications and comorbidities. Information technology, e-health and electronic records may have a role in the preparation for travel for grey nomads with diabetes.
Diabetes self-management
Diabetes is known to contribute to 10% of deaths in Australia and, when inadequately managed, results in out-of-target blood glucose levels, an increase in related complications, poorer quality of life and a higher risk of diabetes-related death2,36. Central to the management of diabetes types 1 and 2 was the capacity of individuals to self-manage their condition, including managing their diet, lifestyle modifications, blood glucose monitoring and medications. Self-management, lifestyle and behavioural choices are key factors in successful diabetes management36-41. Reviewed articles identified essential elements of diabetes self-management as a capacity to problem solve, collaborative goal setting, motivation, time management, eHealth literacy, social support decision-making, appropriate resource utilisation, forming a partnership with a healthcare provider and taking necessary actions36,38-42. It was the relationship between healthcare providers and patient that was consistently identified as a cornerstone for the development of self-management skills and empowered patients through a well-developed capacity to ‘identify, access and make use of appropriate resources’ and thus control and manage their condition37,41,42. While the necessary skills and attributes for self-management are well known, many papers described barriers to self-management that included a lack of communication and support from healthcare providers, insufficient education, financial issues, the influence of the chronicity of the condition on mental health and a lack of motivation to self-manage36-43.
Barriers to diabetes self-management
The importance of the healthcare provider–patient relationship in the development of self-management skills was clear in many of the reviewed concept two studies. Specific findings of poor relationships included having limited time with healthcare providers where questions could be asked and information exchanged, a lack of access to services, a dominance of healthcare providers’ views leading to an unbalanced relationship where the patient felt devalued, decision-making was not collaborative, initial education provided at diagnosis was found to be limited, and ongoing education was sparse with some providers found to be reluctant to refer patients to self-management education programs37,39,42. Dao et al identified that some people lacked understanding of the seriousness of diabetes and the potential consequences of poor management, which led to apathy with treatment and poor motivation for self-care39.
The barriers to self-management have currency for grey nomads with diabetes, who are frequently away or out of contact with their healthcare provider, often for months or years at a time33,35. The capacity for grey nomads to develop meaningful relationships with healthcare providers along their travel routes was limited by not only the time spent in a location, but also access to services in areas of remote Australia where services were already limited and stretched4,9,22,33. These findings raise the question of how well grey nomads were managing their diabetes while travelling and who was providing the support and education required for effective self-management. With the advent of information technology and e-health, self-management of grey nomads with diabetes could be enhanced and more supported.
Rural and remote Australia and healthcare services
Disparities between health services in metropolitan and rural areas have been well documented: people living in rural or remote areas have significantly reduced access to healthcare services and overall health status34,44,45. The disparities have been attributed to geographic remoteness and small populations with low socioeconomic status, which leads to longstanding service provision issues of ‘workforce shortages and maldistribution, difficulties with recruitment and retention, and inadequate access to and availability of appropriate services’44. Adding to the difficulties are resource limitations where delivery of quality care is hampered by a lack of equipment, space and expertise45.
Traditional models of care provision are based on population size, which results in many smaller communities being without on-site services, or there are long distances to reach appropriate care44,45. Seasonal variations in population add further complexity and burden35,43, as small communities are not equipped for the influx of grey nomads, and recruitment of additional staff to meet the demand is difficult4,9,33,34. Grey nomads travel to locations with sparse and stretched healthcare resources, often with the expectations that healthcare services will be available3, and have described healthcare experiences of lack of access, long waits for appointments and lack of investment by healthcare providers due to their short-lived residence in a community4,9,33. Fragmentation of care was reported to occur when there is a need for multiple healthcare providers and when medical history, treatment plans, access to past results, medications and links to health records were unavailable3. Spending long periods of time in a discontinuous health environment has the potential for serious health repercussions: access, continuity and engagement with healthcare providers are cornerstones of self-management in diabetes. This highlights the need for rigorous trip planning and the innovative use of resources that enhance engagement and continuity of care.
Table 2: Review concepts, themes and subthemes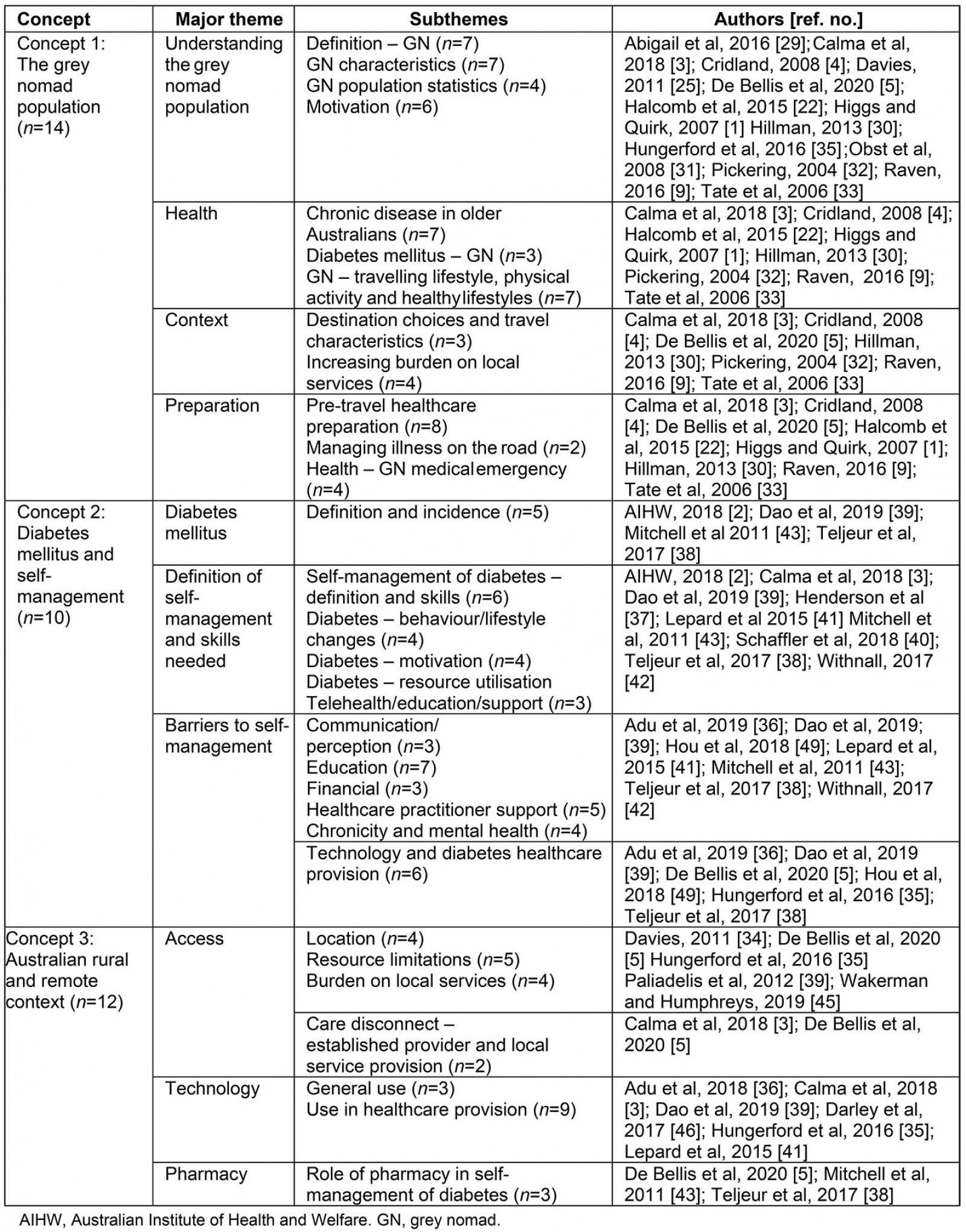
Discussion
The review found that grey nomads were a significant mobile population, many of whom had chronic health conditions including diabetes. Self-management was identified as important in preventing the complications of diabetes, especially when travelling in rural and remote regions of Australia. Many barriers have been identified, including a lack of access to equipment, medications and services in rural and remote areas. Although preparation for travel was generally done well by grey nomads, the reviewed studies identified that health preparation was overlooked. Grey nomads were often underprepared to self-manage their diabetes according to rural and remote diabetes educators5, and it is suggested that information technology and e-health could contribute to better self-management of diabetes for grey nomads, by enhancing access to their own general practitioner or diabetes nurse educator. Furthermore, rural, and remote pharmacists, as well as registered nurses, could have a role in providing information, education, medications and services to grey nomads with diabetes.
Virtual communication programs and cloud-based repositories of information have overcome the confines of rural and remote regions and the limitations of geographic isolation35,46. Telemedicine, social media, the internet and virtual communication have added a significant and important avenue for increasing continuity of care for grey nomads with diabetes as they travel away from their healthcare provider into regions of inadequate services. Early studies of grey nomads use of the internet and social media found that grey nomads were reluctant to embrace technology-based communication4,32. More recent studies, however, have found that grey nomads use of the internet, SMS and virtual communication for information gathering and staying connected with family and friends was rapidly increasing35,46. The COVID-19 pandemic has seen a rapid increase in the provision and uptake of telemedicine and is a promising new resource for continuity of health care in the grey nomad population. Digital technology has added new sources of support for people with diabetes via tools that have been found to enhance self-management, with alerts for medications, recording of blood glucose levels and providing encouragements to enhance motivation that overcome constraints such as access and time36,47. Digital technology and a willingness to communicate using information technology, evident throughout COVID-19, enables stronger communication with established supports, irrespective of location. However, the plethora of information now available online requires a capacity to appraise the information obtained, and not all who can access the internet have such capacity39. Thus, the importance of dedicated and managed e-health sites is imperative to ensure continuity and reliability of care and advice.
Although there is a rapid uptake of digital information seeking, De Bellis et al found the local pharmacy was often the first port of call when grey nomads with diabetes needed assistance5. Community pharmacies are the most frequently accessed and accessible health support, with over 458 million individual patient visits recorded annually48. The Seventh Community Pharmacy Agreement supports consumer access to Pharmaceutical Benefits Scheme subsidised medicines, the National Diabetes Services Scheme and community pharmacy programs across Australia. Pharmacists can offer advice on medications, diet, foot care, blood glucose monitoring and equipment issues49. Rural and remotely located pharmacists offer an important resource in the support and management of grey nomads with diabetes. Further research into electronic resources, information and education for grey nomads themselves, as well as healthcare professions, can be recommended to help grey nomads self-manage their diabetes while on the road.
Conclusion
This review aimed to answer the question ‘What are the self-management behaviours of grey nomads with diabetes when preparing for and travelling through rural and remote locations of Australia?’ The review has explored and mapped the major concepts of who grey nomads are, the sentinel aspects of diabetes self-management and the impact of being rural and remote on services and support for grey nomads with diabetes and their self-management. The literature determined the grey nomad population had a similar distribution of chronic illness, including diabetes, but very little was known about how they self-manage their condition when in remote locations where healthcare services were limited. The emerging roles of digital technology, increased and expanded use of telemedicine and the developmental opportunity for pharmacists offer new and innovative avenues to support grey nomads with diabetes while travelling.
