Introduction
Population aging is a global phenomenon characterized by an increasing proportion of older adults in the population, attributed to decreasing mortality and birth rates1. Brazil is rapidly becoming an aged country – of more than 213 million inhabitants, nearly 30 million are older adults (aged 60 years or more). Nearly 4.5 million (15%) Brazilian older adults live in rural areas. Despite the advances in primary healthcare coverage in Brazilian rural areas, provision of adequate health services for rural populations is particularly challenging. The economic and political crisis and Constitutional Amendment 952 have further restricted investments in the Brazilian Unified Health System3. This situation constitutes a threat to integrality and equity in health care, compromising investments in the Family Health Strategy, which is a user’s first contact with the health system. This scenario can compromise recent efforts to expand coverage and maintenance of health teams in rural and remote localities.
Most literature on aging has been produced in rich countries and in urban areas. Since the determinants of aging can be affected by local conditions, particularly the reduced supply of health services, it may not be appropriate to apply results of urban studies to help propose and implement measures to improve the health care of older adults living in rural areas. In Brazil, urban space is determined by municipal law, and rural space is defined by the exclusion of the urban area. Taking this classification, according to the 2010 Census 84.4% of Brazil’s population at that time were living in urban areas and 15.6% in rural areas4-6.
Knowledge about the occurrence of falls, frailty, sarcopenia and vulnerability among older adults in rural areas of Brazil is less than that available about their urban counterparts7-9. Longitudinal cohort studies that accompany older adults from rural areas can measure the occurrence of diseases as well as assist health service managers in proposing measures that could improve the health services offered according to the needs of rural inhabitants. Thus, this study aims to present the methods used to design a prospective cohort study with older adults from a rural area in the far south of Brazil (EpiRural Cohort Study), as well as to describe the cohort profile.
Methods
Study area
Rio Grande is a municipality in the south of Rio Grande do Sul state, Brazil, with an area of approximately 2708 km2. It has one of the largest ports in Brazil and, in 2017, its estimated population was 209 378, almost 95% of whom lived in urban areas4,5. The rural part of the municipality of Rio Grande is geographically delimited by the water bodies Laguna dos Patos, the Atlantic Ocean and Laguna Mirim, where traditional communities live mainly from fishing and family farming, including livestock, rice and soybean. The study area was chosen to:
- locate the study in the same municipality as that of the EpiRural Cohort Study, designed and developed by researchers from the Federal University of Rio Grande
- investigate and monitor patterns of morbidity, mortality and use of health services in a poorly studied population.
Study population
The eligible population for the EpiRural Cohort Study comprised older adults (aged ≥60 years) living in the rural area of the municipality of Rio Grande.
Baseline survey
The baseline survey was originally a cross-sectional study conducted from April to October 2017. A systematic random sampling process was used to select 80% of households. For each census tract, a number between 1 and 5 was drawn, with the drawn number corresponding to the household in each group of five consecutive households that was skipped. This procedure ensured that four out of five households were sampled in each census tract. All individuals aged 60 years or more who lived in the selected households were eligible. Individuals living in long-stay institutions, nursing homes and prisons were excluded.
The baseline questionnaire included questions about demographic and socioeconomic characteristics (gender, age, ethnicity, religion, marital status, education, family income and occupational status) and lifestyle (smoking, alcohol consumption), as well as about health conditions (self-rated health, past medical history of hypertension, diabetes, stroke, osteoarthritis and lung disease), falls and medication use. The Katz Index of Independence in Activities of Daily Living (ADL)10, the Lawton Instrumental Activities of Daily Living Scale (IADL)11, the Patient Health Questionnaire (PHQ-9)12, the Measure of Older Adults Sedentary Time (MOST)13, the short version of the Brazilian Food Insecurity Scale (EBIA)14 and the Eating Behavior Questionnaire (adapted from the SABE Study)15 were also applied. Weight and height were self-reported by the individuals (Table 1).
Table 1: Summary of variables collected at baseline (2017) and first follow-up (2018/2019), EpiRural Cohort Study, Rio Grande, Rio Grande do Sul, Brazil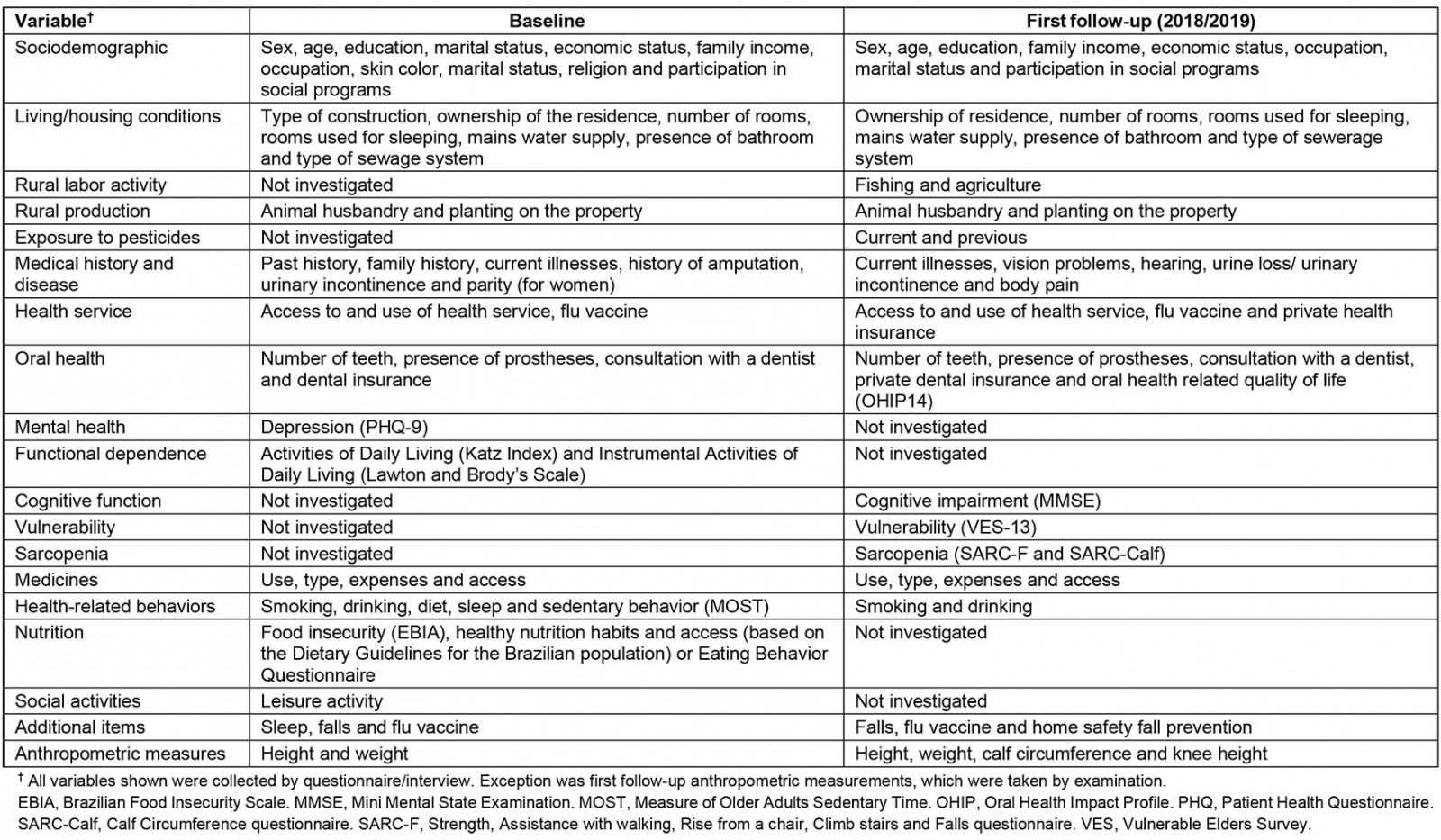
First follow-up
From September 2018 to March 2019, the research team undertook the first annual follow-up visit at each participant’s home. The questionnaire included the same information as the baseline instruments. In addition, the following were administered: the Oral Health Impact Profile (OHIP14)16; the Mini Mental State Examination (MMSE)17; the Vulnerable Elders Survey (VES-13)18; the Strength, Assistance with walking, Rise from a chair, Climb stairs and Falls (SARC-F) questionnaire19; and the Calf Circumference (SARC-Calf) questionnaire20. Knee height, weight and calf circumference measurements were performed. Body weight was measured with an Ohron digital scale, knee height was measured with a portable metal children’s anthropometer and calf circumference was measured with a non-stretch Cescorf tape measure.
Data collection instruments used at baseline and first follow-up comprised an electronic questionnaire using REDCap (Research Electronic Data Capture)21. Both data collections were performed by a team of trained interviewers who had completed secondary school. All measurements were collected by professionals who had been trained according to Lohman’s techniques22 and were standardized as proposed by Habicht23.
Death monitoring
Deaths are being continuously monitored from a monthly report of death certificates or by consulting the Mortality Information System (SIM) at the Municipal Epidemiological Surveillance System. Causes of deaths are being coded according to the International Classification of Diseases, 10th revision (ICD-10)24.
Data analysis
Data were analyzed using Stata v13 (StataCorp; http://www.stata.com). Baseline and first follow-up were described according to sociodemographic, behavioral and health characteristics. The research team then compared the profiles of respondents and non-respondents from the first follow-up (sex, age, smoking, alcohol consumption, diagnosis of hypertension, diabetes, stroke and self-rated health). Pearson’s chi-square χ2 test was used for both analyses.
Ethics approval
The baseline and the first follow-up studies were approved by the Research Ethics Committee of the Federal University of Rio Grande, as per opinion numbers 51/2017 and 154/2018, respectively. Confidentiality of the participants’ individual information was ensured. Participants signed an informed consent form. Caregivers or legal guardians signed the form on behalf of elderly people with disabilities where required.
Results
Baseline
The research team sampled 763 households with 1130 older adults; 1029 individuals participated in the baseline study (8.9% lost to follow-up and refusals).
First follow-up
From the original cohort, 862 individuals were followed (83.8%) in the first follow-up, 2018/2019 (Fig1). Respondents did not differ from non-respondents regarding sex, age, smoking, alcohol consumption, diabetes and stroke. A larger number of non-hypertensive individuals were lost to follow-up (Table 1).
Table 2: Respondents and non-respondents at first follow-up (2018/2019), EpiRural Cohort Study, Rio Grande, Rio Grande do Sul, Brazil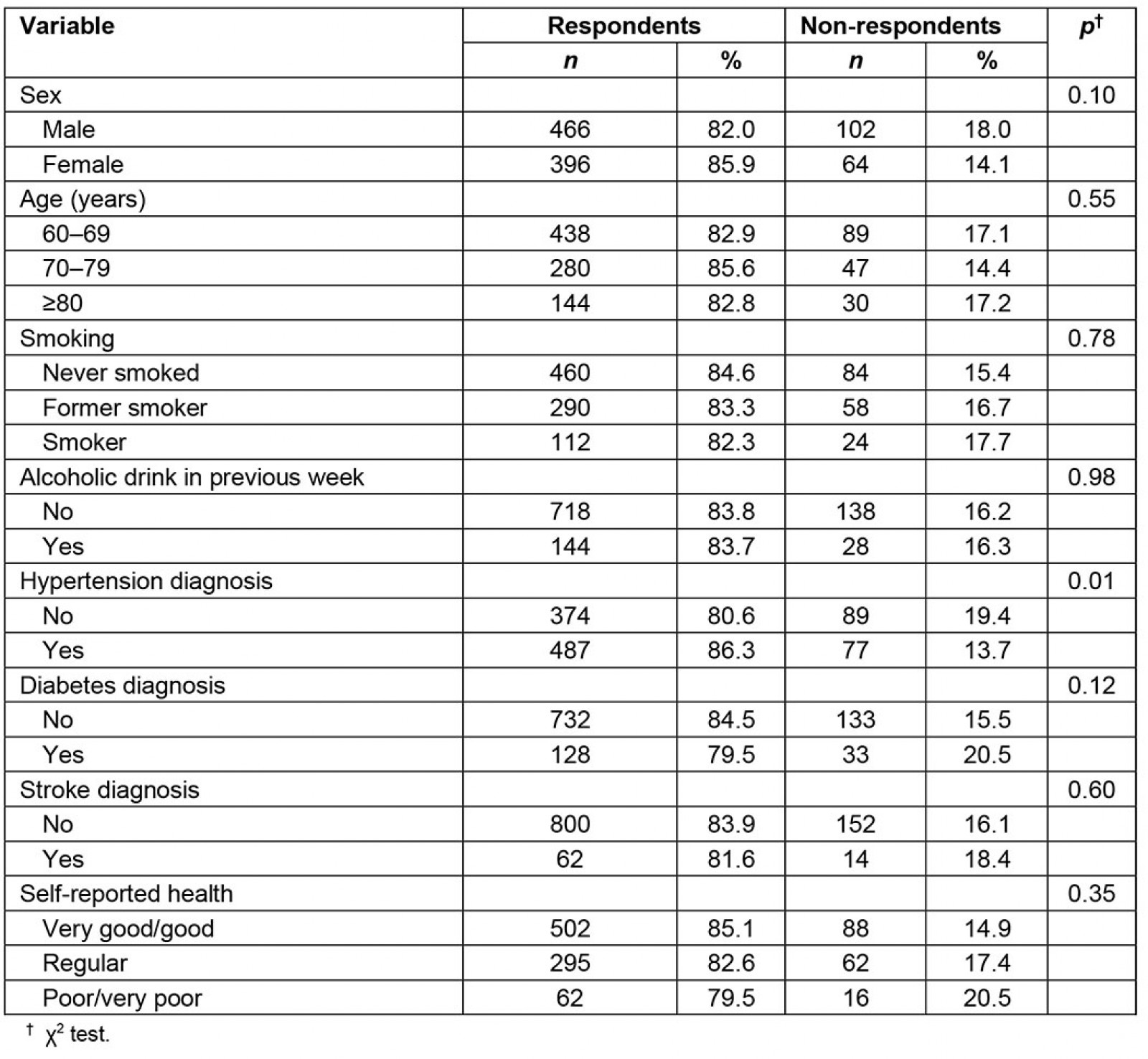
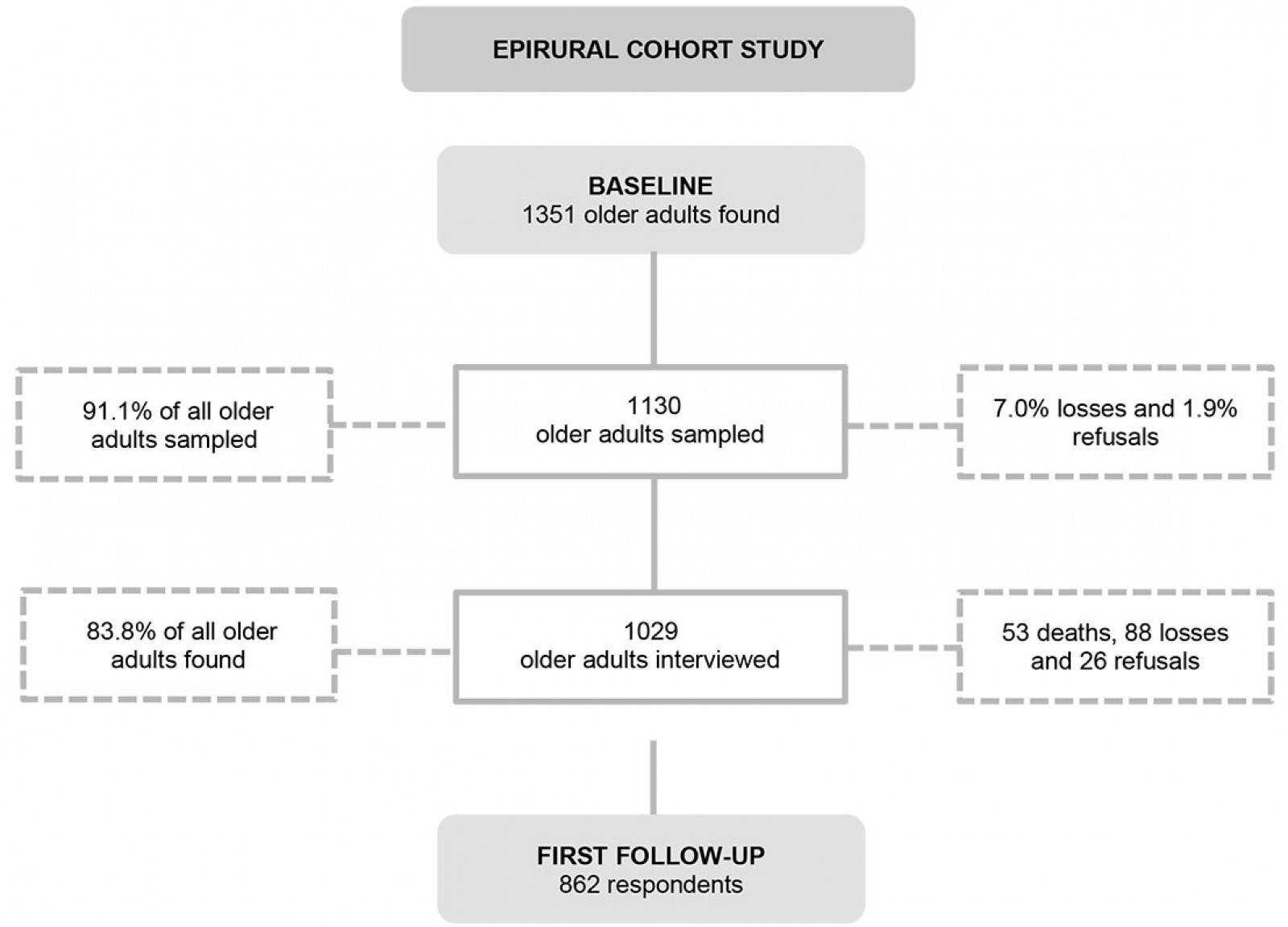 Figure 1: Flow diagram indicating the number of elderly identified, sampled, losses and refusals of the EpiRural Cohort Study, 2017 and 2018/2019
Figure 1: Flow diagram indicating the number of elderly identified, sampled, losses and refusals of the EpiRural Cohort Study, 2017 and 2018/2019
Cohort profile
In the baseline study, most individuals were males (55.2%) and aged 60–69 years (51.4%). Almost 23.0% were living alone, 15.0% were working, about 13.2% were smokers and a 16.7% had consumed alcoholic beverages in the previous week. The prevalence rates of hypertension, diabetes and stroke were 54.9%, 15.7% and 7.4%, respectively. About 60% classified their health as very good/good (Table 3).
Between the baseline and the follow-up study, the proportion of individuals aged 60–69 years decreased to 44.3% and those aged 70–79 years increased to 36.1%. Those who had consumed alcoholic beverages in the previous week and had hypertension increased to 19.4% and 59.0%, respectively. Male-to-female ratio, living alone, working, smoking, diabetes diagnosis, stroke and self-reported health were similar between baseline and first follow-up (Table 3).
Table 3: Baseline and first follow-up characteristics of EpiRural Cohort Study in 2017 and 2018/2019, Rio Grande, Rio do Sul, Brazil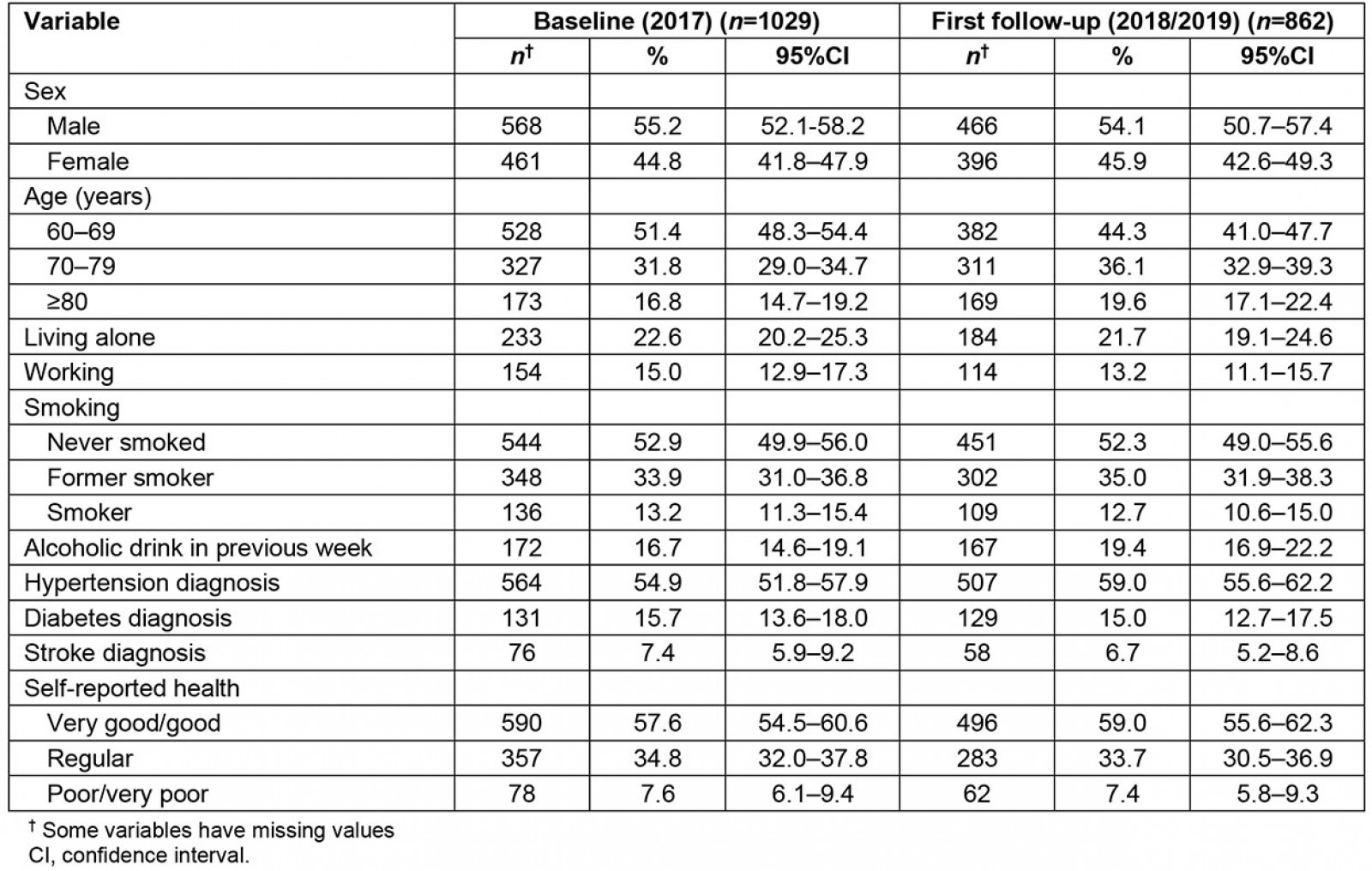
Discussion
This article describes the design and profile of a prospective cohort study with older adults from the rural area of the municipality of Rio Grande, Rio Grande do Sul state, Brazil. To the best of the authors’ knowledge, the EpiRural Cohort Study is the first Brazilian rural older adults cohort. Most Brazilian longitudinal studies assessing older adults have been conducted in urban areas such as Bagé25, São Paulo15,26 and Florianópolis27.
Prospective cohort studies with rural populations are scarce. In Latin America, two cohort studies carried out in small rural towns in Chile (the San Francisco Project Cohort Study (PSF) and the Growth and Obesity Chilean Cohort Study (GOCS)) are noteworthy. The PSF population comprises individuals aged 30–79 years and aims to study and monitor cardiovascular risk factors, while the GOCS is a cohort study with children born in 2002–2003 that assesses the association between early postnatal growth and adiposity recovery time. PSF and GOCS are successful experiences of longitudinal studies carried out in rural areas of Latin America28,29.
In China, a country with almost 40% of its population living in rural areas30, two rural cohort studies that evaluate chronic non-communicable diseases (NCDs) in people aged 18 years or more were reported in the literature. The authors of those studies described that they measured outcomes such as stroke, coronary heart disease, diabetes, BMI and other common chronic NCDs. They also measured blood pressure, lung function and carried out imaging and blood exams31,32.
In the EpiRural Cohort Study, most NCDs have been measured. However, self-reported information about most morbidities has been used, and lung function, imaging and blood exams have not been performed (Table 1).
Data collection is organized and supervised by master’s and doctoral students, who also perform the data analysis. Thus, the EpiRural Cohort Study is a useful tool for professional training while also producing scientific knowledge about the health of rural older individuals.
The authors have published 10 manuscripts with the baseline data. The findings are about access and use of healthcare services, depression, falls, food insecurity, functional dependence, obstructive apnea syndrome, sedentary behavior, smoking, urinary incontinence and oral health (Table 4)33-42. Manuscripts with the findings of the first follow-up have been submitted to a number of international scientific journals.
All the results were reported through meetings with primary healthcare managers and health professionals of the rural area of Rio Grande. Also, the main findings were described in a technical report handed over to the coordinators of family health centers of the rural area of Rio Grande and to the municipal health department. The authors are also sharing the findings with the community on Facebook and Instagram (@epirural.riogrande).
This study has strengths and limitations. The sampling process enhances internal validity as the numbers/proportions of permanently inhabited households, men/women and age strata are similar to those reported by the Brazilian Institute of Geography and Statistics in the 2010 census. Follow-up rates are acceptable despite the challenge of conducting home interviews in rural localities. Losses to follow-up are mainly due to change of address. Sometimes the research team was unable to locate cohort members even after asking for help from neighbors and/or primary care health professionals. Moreover, some routes or localities were known by different names, and they were described better in our field diary to prevent more losses. In the second follow-up the research team will use a global positioning system device to record and locate households. The team is also working to improve data quality about sarcopenia through the measurement of hand grip strength with a dynamometer and walking speed. The use of self-reported diagnosis of hypertension and other morbidities is subject to recall bias. Thus, blood pressure measurements and other clinical tests were included to minimize this limitation. About 5% of cohort members died in a 12–18-month time interval. As an older adults cohort, future study will have to include new members to become a dynamic cohort study.
The EpiRural Cohort Study welcomes collaboration to enhance knowledge about rural older adults. Researchers interested in collaborating and/or further information are invited to contact the authors.
Table 4: Summary of main publications of EpiRural Cohort Study, Rio Grande, Rio Grande do Sul, Brazil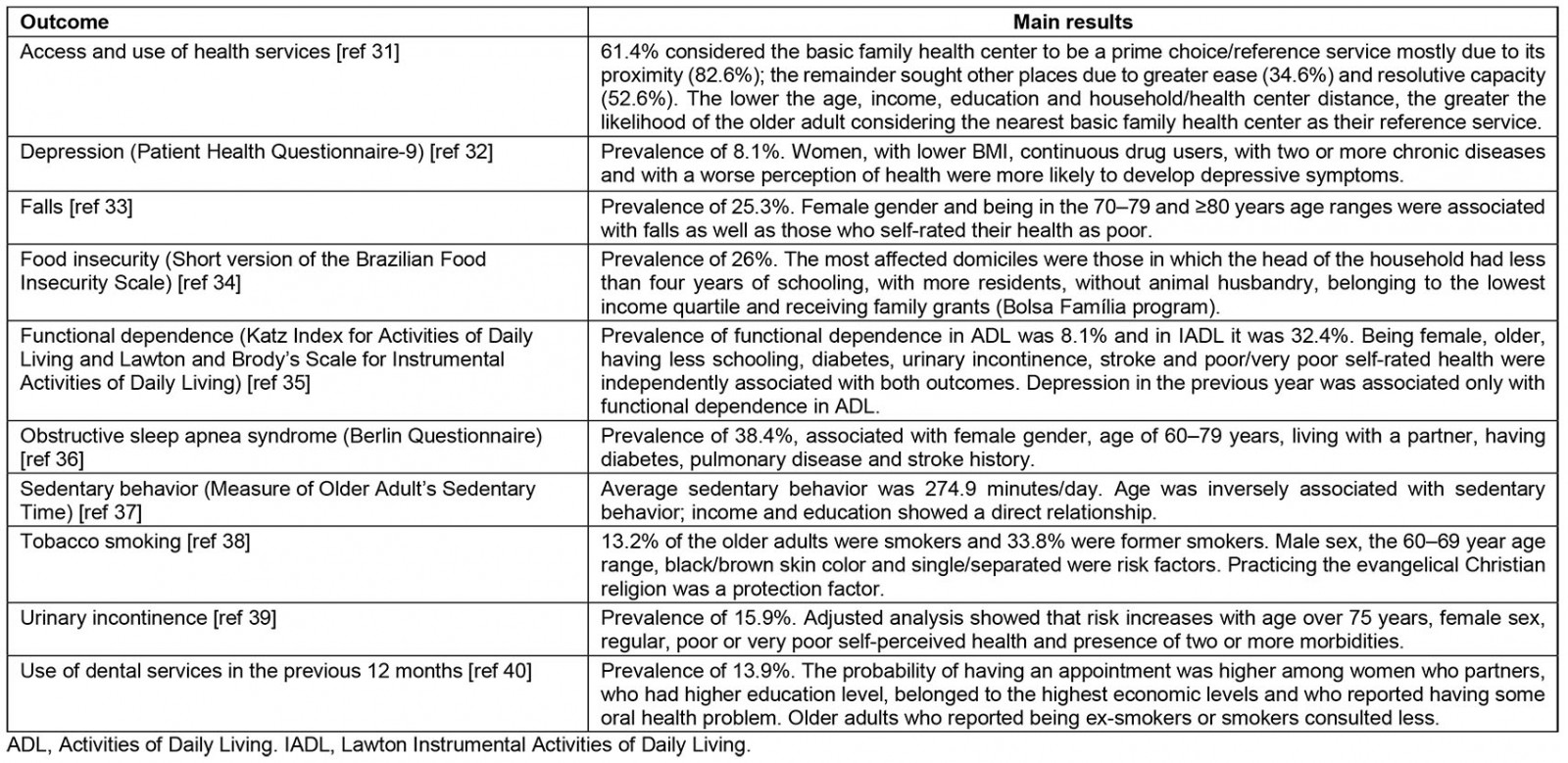
Conclusion
This article shows that the EpiRural Cohort Study is providing knowledge about the health of older adults living in a rural community in southern Brazil. The main findings and methodological issues are also reported, as well as the strategies adopted to overcome the challenges. The authors expect that the report will encourage researchers and health professionals to improve the knowledge about the health of rural older adults in developing countries.
Acknowledgements
The authors acknowledge the Research Support Foundation of Rio Grande do Sul (FAPERGS) and Coordination for the Improvement of Higher Education Personnel (CAPES).
References
You might also be interested in:
2018 - Rural medicine ‘cooking up’ longitudinal integrated clerkships
2016 - Can a 'rural day' make a difference to GP shortage across rural Germany?




