Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory disease, of autoimmune etiology, which generates functional limitation, disability, and deterioration of quality of life if there is not adequate and timely management. The use of disease-modifying drugs (DMARDs) as angular therapy decreases disability and improves prognosis. Therefore, favoring the start of effective treatment and its adherence generates higher remission rates, lower costs derived from health care and, finally, better quality of life among those affected. A transcendental aspect that motivates drug adherence is a good doctor–patient relationship, and this requires the promotion of culturally sensitive care through the understanding of the knowledge and practices in health of the community.
RA, hypothesized to be of American origin1,2, is the most prevalent inflammatory arthropathy worldwide, estimated to affect 0.5–1% of the global population3,4. In contrast, in indigenous peoples of the USA, Australia, and New Zealand the prevalence is 0.6–6.8%5. The Latin American Group for the study of Rheumatic Diseases in Indigenous Peoples (GLADERPO) estimates the prevalence in Argentina, Venezuela, and Mexico to be 0.5–3.2%. A COPCORD study in Colombia that did not include the indigenous population estimated it at 1.49%6. The COPCORD Misak study is currently underway, which will inform of the prevalence of rheumatic diseases in this community7.
The political constitution of Colombia of 1991 recognizes the fundamental right to health care in view of the country’s ethnic and cultural diversity8. In 1993 the currently used General System of Social Security in Health Care (GSSSH)9 was established under the guiding principles of universality and solidarity in health care. In 1999, the WHO recognized the important contribution of traditional medicine in health policies and strategies10. Accordingly, in 2001 Colombia agreed to the participation of indigenous peoples in the GSSSH11 and in 2007 the country endorsed the provision of ‘differential activities’ such as managing health resources, legal support, hospital accompaniment, bilingual guides, home visits and practices used by the traditional healers12.
This regulatory framework gave rise and sustained an emergent culturally sensitive healthcare model in the Misak community, which exceeds the experience of other indigenous peoples13,14. This healthcare model is defined as ‘the ability to react appropriately to the attitudes, feelings, or circumstances of groups of people sharing a common and distinct racial, national, religious, linguistic or cultural heritage’15. This means articulating differences and similarities between traditional and biomedical practices and knowledge of RA in the Misak people and, based on them, promoting intercultural objectives. This must overcome the tendency to just train traditional healers while excluding their expertise and, in contrast, focus on real interculturality that recognizes a patient as the ultimate decision maker who determines when, and how, the health system becomes relevant16.
Studies about medical pluralism from a medical anthropological perspective along with explanatory models (EMs) laid the groundwork of this study. An EM is a useful description of why and how a thing works or an explanation of why a phenomenon is the way it is. EMs do not claim to be a complete description of the absolute about a phenomenon, nor do they even claim to, necessarily, be fully accurate. The description/explanation does, however, need to fit well enough to a sufficient portion of all the knowledge, observations and theoretical circumstances known about a phenomenon, so that the EM becomes useful to make changes in a way that relates to the reality of the community. In this case, EMs are defined as notions about disease episodes and their management used by those involved in the clinical process, and every participant has its own EM. Kleinman distinguished five main structural points that make up an EM: etiology, pathophysiology, mode of onset of symptoms, course of sickness, and treatment17. Patients and their families inform the understanding of the disease and, building on this understanding, they choose and evaluate different treatment strategies18. For example, in the EM of the Mapuche people of Chile, the concept of RA is a warning from the afterlife sent as an indication that a dream revelation has been ignored. It often thought of as a disease-causing evil spirit that takes the shape of a hair, rod, or insect, and must be sucked out by the shaman to expel it19.
Indigenous approaches to care and biomedicine provide different perspectives. The role of medical anthropology in this medically plural context is to enable or facilitate a dialogue between these two approaches to improve care for patients with rheumatic diseases such as RA20. These interactions should be viewed through the prism of pedagogy of relational contact, defined as respectful communication with consideration for human dignity and subjectivity, empathic and sensitive to intellectual and emotional life21,22. It is in this context that the present study was developed.
Population and methods
Design
This qualitative study used ethnographic methods aimed at understanding the social context in the daily life of the individuals, as well as the intentionality of their actions undertaken within coexistence and interaction with others. Ethnographic refers to the description of attitudes, cultural know-hows, and therapeutic practices employed by the Misak in the treatment of RA.
Study population
The study population was patients with RA according to the 1987 American College of Rheumatology criteria23 who attended the Mamá Dominga Hospital; some patients with disabilities were visited at home. Similarly, researchers interviewed 12 traditional healers and 5 health professionals (4 general practitioners and a rheumatologist) providing medical services to patients with RA in the community.
The Misak are a community of approximately 22 000 persons inhabiting the Guambia reservation in the Department of Cauca, Colombia24. They call themselves Piurek (‘children of water’) (according to the Misak myth). The concept of Mother Earth lies at the heart of their worldview, together with idea of the pishimisak (protective elder spirits). Ninety one percent live in rural areas with farming as the main economic activity. Sixty five percent speak the local language known as nam trik wam; 18% of the population is illiterate. The highest authority is the Cabildo Indígena25. The Misak are a receptive community, a community that show a tolerant attitude and accept new ideas, criticisms, and influences, in this case regarding proposals related to health care. Many professionals from different fields of knowledge return to the reservation after receiving academic training; among them are healthcare professionals who come back to manage and provide health services. The community has been served since 1994 by the Mamá Dominga Hospital, a primary healthcare institution, and the Casa de Plantas – Sierra Morena, a traditional medicine care center. Both institutions provide inpatient and outpatient services and are located 2 km apart, so the local population has access to both types of treatment (Fig1).
 Figure 1: Location of the Mamá Dominga Hospital (a biomedical care center) and the Casa de Plantas –Sierra Morena (a traditional medicine care center) in the Guambia Reservation, Cauca, Colombia.
Figure 1: Location of the Mamá Dominga Hospital (a biomedical care center) and the Casa de Plantas –Sierra Morena (a traditional medicine care center) in the Guambia Reservation, Cauca, Colombia.
Data collection and analysis
Data were collected for two consecutive years (2017 and 2018) by a group composed of physiotherapists (one of them of Misak origin), an anthropologist, and a rheumatologist, through observation, a field diary, and open interviews. Interviews were recorded with an MP4 recorder, transcribed, and translated into Spanish in their entirety for the thematic analysis. An interview script was designed to explore the EMs.
Different triangulation efforts were conducted to ensure the rigor of the findings: methodological triangulation (observation, interview) and investigator triangulation (multidisciplinary researchers).
The process involved reading the transcripts on several occasions and taking field notes of the observations to reconstruct the narratives of the participants. The thematic analysis identified the themes and subthemes along with the emerging themes as per the study objectives26. An interdisciplinary group (rheumatology, physiotherapy, and medical anthropology) performed the analysis to establish the convergence of the identified themes. The team then reviewed the analysis and reached agreements as to its interpretation, ensuring the reflexivity of interpretation.
Ethics approval
The ethical principles underlying this investigation are governed by the Declaration of Helsinki and the Resolution 008430 of 1993 by the Ministry of Health of Colombia27. The authors obtained the authorization from the ethics committee of the Universidad del Cauca, internal code ID:4152, an endorsement from the indigenous authority (the Cabildo), as well as individual informed consent forms from all participants. Each interviewee was assigned a code to meet the ethical criterion of confidentiality.
Results
This study describes attitudes, cultural knowledge, and therapeutic practices of the Misak people concerning RA, as an important aspect to motivate a rapprochement between the community and health professionals, and to strengthen an emergent culturally sensitive healthcare model that is present in the Misak community. The model is made up of these elements: a receptive indigenous population; health professionals equipped with cultural competencies rooted in university academic training; healthcare centers that subscribe to the local worldview – figuratively speaking, an amalgam of biomedical and traditional knowledge in line with the state policies and the indigenous law (Fig2).
Researchers interviewed 20 RA patients, 12 traditional healers and 5 health professionals (4 general practitioners and a rheumatologist) who have been serving the Misak population for at least 6 months and agreed to participate in the study. The participating traditional healers had a mean age of 46 years and most of them only attended primary school, while health professionals had a mean age of 27 years and were self-defined ethnically as mestizos. The group of patients with a medical diagnosis of RA had a mean age of 50 years (range 28–74 years) and 80% were women.
The main three themes around which the results of the study are built are: (1) training of the traditional healers, (not as a product of formal academic curriculum, but recognized by the community); (2) the EM of RA constructed by patients and the traditional healers; (3) challenges between the community and the biomedical EMs.
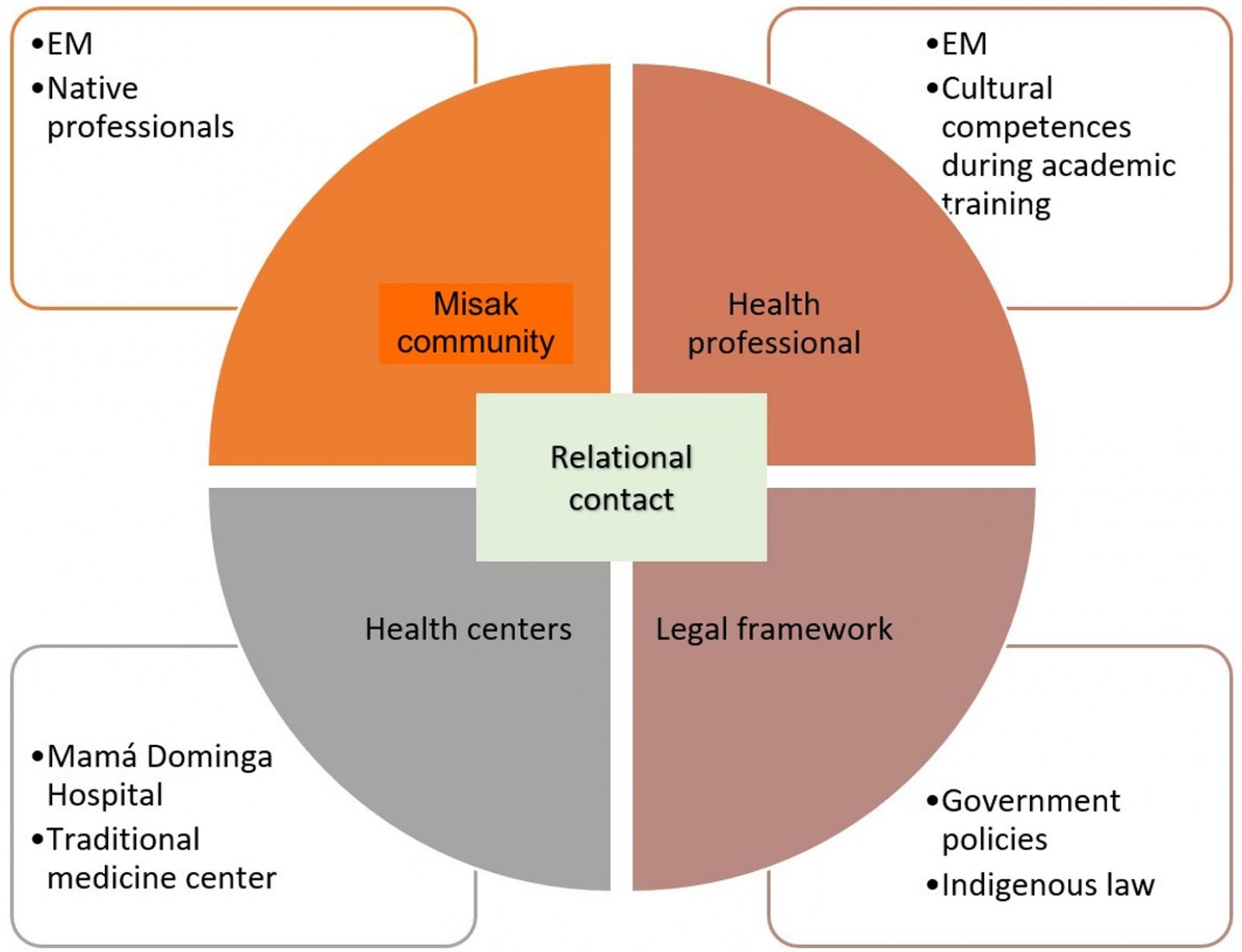 Figure 2: Culturally sensitive healthcare model of the Misak indigenous community.
Figure 2: Culturally sensitive healthcare model of the Misak indigenous community.
Traditional healer training
The traditional healers agreed that their knowledge is acquired through ‘gifts’ granted in dream revelations during childhood and reinforced through teachings passed on through generations, along with the advice and guidance of other healers. These gifts are inspired by the elder spirit and must be practiced selflessly. According to this tradition, there are several types of specialties in native health care, including sobanderos (traditional healers who treat dislocated bones, fractures, sprains and muscle pain, through therapeutic massage), midwifes, sentidores (traditional healers who perform cleansing rituals), and pulsadores (traditional healers who treat scared children). The healers attach great importance to the influence of nature spirits:
I have 14 years of experience in this area and so far all patients I have seen have turned out well, because one has that positivity in caring for patients and that energy is transmitted to the person. (traditional healer, interview 4)
Explanatory model of rheumatoid arthritis in the Misak community (patients and traditional healers)
The Misak community has a consensus between patients and the traditional healers, as described below.
Etiology of RA: From its origins, RA has been construed as a cold-related disease. The healers propose that habits and factors leading to the disease are bathing in cold water while being ‘hot’, building houses near rivers, lagoons, or wet spots, eating cold food, having a poor diet and ignoring ancestral meal choices, overexerting at work, wearing boots constantly, having poor postnatal care, bathing while menstruating, living under stress, walking through places inhabited by the spirit of the disease, inheriting the disease, and touching the dead.
We who come from the countryside are used to wearing rubber boots, which get hot and then people would wash their legs without cooling down first, which causes pain, and pain over time becomes RA. We also have bad eating habits. (traditional healer, interview 11)
Another cause is for not building the houses well, previously they were built on the hills, and now they are built on the banks of the rivers, and that wind from the rivers penetrates the body especially in the morning and the person absorbs it and that is the cause of rheumatoid arthritis. (traditional healer, interview 5)
Many people wash their legs without cooling after removing their boots, causing pain in the legs, which over time becomes RA. (traditional healer, interview 11)
Today we do not value ancestral foods such as mauja, corn, quinoa, ollucos, cabbage, milk, and mothers say that you have to eat hot foods like these, and cold foods in a balanced way, to avoid generating this disease. (traditional healer, interview 4)
Diagnosis: The traditional healers identified conditions of bones, nerves, veins, liver, eyes, nails, and especially tendons, which become rigid and cannot be moved; they pay attention to weight loss, general malaise, fever, and exacerbated night-time pain when moving, associated with inflammation and joint deformities.
Treatment: A distinctive characteristic of the Misak community’s EM is the agreement between the traditional healers and the patients, which translates into patients choosing the therapeutic approach offered by the traditional healer, either as the first or the only treatment option. The healers recommend the use of ‘hot’ medicines, in the form of plants, to cure a ‘cold’ disease, and that patients seek union with the elder spirit during rituals that start with a ‘refreshment’ (an initial part of a ritual including offering prayers and having revitalizing drinks) followed by massages and baths with one or more plants such as marijuana, coca, pine, eucalyptus and rue, chosen because of their analgesic properties, and calendula or sarsaparilla for their anti-inflammatory and anxiolytic properties. The plants are used in infusions, steamed, or added to drinks per patient needs to manage the general symptoms of RA. The elder spirit is said to guide the healer through their dreams, teaching them to use the plants correctly. According to the healers, treatment is fast and efficient, and the diseases are cured when ‘one has faith’. Some patients are encouraged to do physical workout routines to complement the treatment.
Differences between the community and biomedical explanatory models
The care of patients with RA in the community, by traditional healers or general practitioners, does not have a single starting point, nor does it run in a linear fashion; it fluctuates between one and the other at the initiative of the patient, but rarely by referral. Recently, biomedical groups referred cases of musculoskeletal pain such as some appendicular syndromes to the traditional doctor, with the purpose of motivating bidirectional referral of patients with diseases such as RA. However, up to now, traditional healers have sent people to healthcare professionals only when they have with acute and severe manifestations of extra-articular compromises of RA, generally configuring a poor prognosis among those affected (Fig3).
While the EMs of Misak and traditional healer patients coincide, the biomedical EM requires that, through the pedagogy of relational contact, it be made available to the community effectively to overcome conceptual and communication barriers. Some biomedical groups report that meeting spaces with traditional healers are limited and that this is partly a consequence of rejection attitudes learned during their academic training. This is one of the aspects to continue transforming through curricular designs with social projection of higher education institutions, in favor of generating humanized healthcare paths, with social responsibility.
Health professionals also reported that they seek tactics to improve adherence by doing educational talks, explaining the disease and the treatment plan to the patients with charts and diagrams, using interpreters as necessary, to address the community’s concerns about being unable to work. Unfortunately, most patients start seeking advice from a rheumatologist when it is too late, or it is more likely that they will need to switch to biological DMARDs, for which they must travel to Popayán city, capital of the department of Cauca, 60 km away.
Mapping out the EM of the Misak community to find common ground with the biomedical EMs amid their differences is an opportunity to bring about changes needed to provide more sensitive, consistent, and timely health care to improve clinical outcomes in this population:
That is why our plan was to partner up with a strategic biomedical group and the Mamá Dominga Hospital, liaise with the community to hear it, interact with patients, with the traditional healers, earn their empathy and trust, and obtain data for the health authorities and the health workers to make decisions. (rheumatologist)
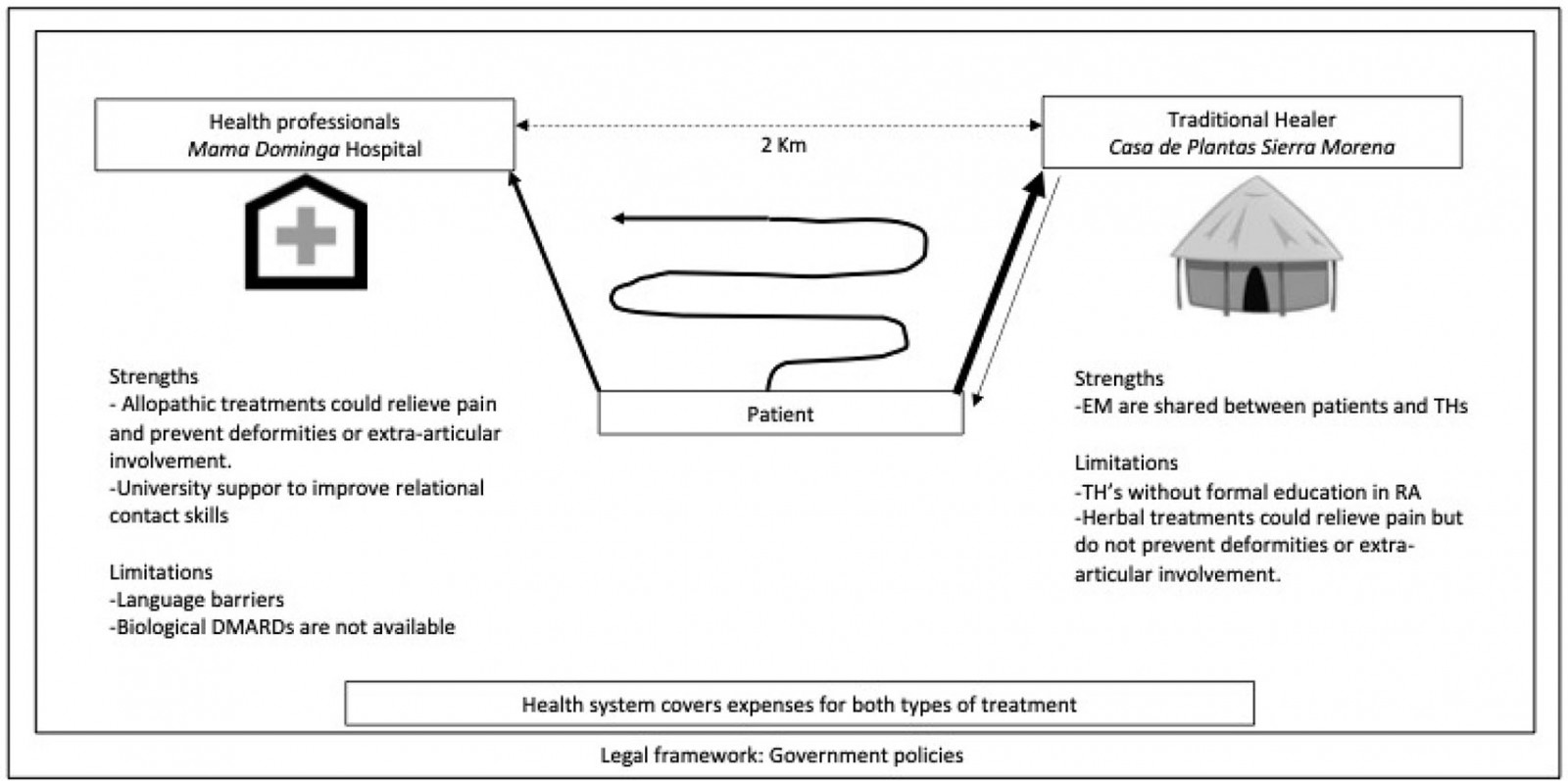 Figure 3: Care of patients with rheumatoid arthritis in the community fluctuates between traditional and allopathic medicine by the initiative of the patient. Usually, patients prefer traditional healers and go to Casa de Plantas – Sierra Morena; sometimes traditional healers go to patients to offer treatments.
Figure 3: Care of patients with rheumatoid arthritis in the community fluctuates between traditional and allopathic medicine by the initiative of the patient. Usually, patients prefer traditional healers and go to Casa de Plantas – Sierra Morena; sometimes traditional healers go to patients to offer treatments.
Discussion
This study has helped to work out the details of the Misak community’s EM of RA included in an emergent, culturally sensitive healthcare model that is present in the Misak community.
The Misak community’s EM is shared by traditional healers and the patients, which translates into patients choosing the therapeutic approach offered by the traditional healer more than allopathic treatment. The EM of the community tends towards concrete knowledge, whereas the biomedical EM is more abstract28. Biomedical EMs define a disease in terms of meeting a basic threshold value of symptoms and other clinical data (for example the 1987 American College of Rheumatology criteria), whereas the EM of the community appears in this case to be based on a conception of RA that is based on abstract cultural theories (Fig4). A traditional healer is allowed to practice only if the community recognizes their vocation, while a health professional’s choice of profession is an individual decision and is endorsed by the academic institutions.
As opposed to the main constituents of an EM, the etiology and pathophysiology of RA from the biomedical standpoint are products of the interplay of inherited and non-inherited genetic, hormonal and environmental vulnerability factors (eg smoking and periodontal disease)29-31. In this regard, the traditional healers believe that RA can be a hereditary disease, due to factors related to daily life aspects such as work duties, life cycles, and environmental impact (eg exposure to cold). Although there are no scientific data supporting the association between thermic changes and RA, there is evidence of bidirectional control between the immune system and the nociceptive system, so there’s a field to explore between innocuous cool and noxious cold and inflammation32,33.
As far as the disease course and the diagnosis are concerned, the identification of clinical features by the traditional healers correlates with the biomedical model. However, the Misak situate the disease topographically in the tendons rather than in the joints; these deformities are frequently found late for a definitive diagnosis, a scenario that the biomedical approach seeks to avoid34. At the same time, the Misak traditional healers mention the presence of general symptoms, but fail to identify the diversity of extra-articular manifestations of the disease and related complications owing to late or interrupted treatment35. Concerning treatment, the Misak consider biomedical medications to be ‘cold’ substances that relieve but do not cure. This contrasts with the approach taken by traditional medicine practitioners, who seek to cure a ‘cold’ disease through the use of ‘hot’ medicines, which are plants.
Caring for patients with RA in the community, either by the healer or a general practitioner, lacks a single starting point and develops in a non-linear fashion; the patients themselves decide which treatment to take, rather than being referred from the traditional healer to the health professional or vice-versa. However,
the geographic proximity between Mamá Dominga Hospital and Casa de Plantas – Sierra Morena favors the possibility of gestating meetings between traditional healers and health professionals, and between patients and the therapeutic options that both centers offer, in order to establish joint protocols or ‘paths’ of care in RA, as they prefer to call them, taking advantage of the Colombian legal framework that promotes the empowerment of indigenous people regarding the responsible use of GSSSH resources for ‘differential activities’ in their health care.
While the EMs of the Misak patients and the healers concur, the biomedical EM differs in diagnostic and therapeutic determinants. Health professionals who work at Mamá Dominga Hospital have gained culturally sensitive communication skills during their work with the community; however, these need to be further strengthened after their academic training. This is one of the aspects that is being strengthened through the curricula of some socially conscious higher education centers, designed to open paths of humanized health care, full of awareness and historical responsibility36,37.
In 2015, the Colombian Ministry of Health established the report of RA patients to the High-Cost Account (Cuenta de Alto Costo), an organization to trace high-expenditure diseases38. Biological therapies, joint replacements, osteoporosis and fractures, disability and incapacity, caregivers and morbidity and mortality from cardiovascular causes, infections and cancer generate a high cost of care39. These health expenses are facilitated by barriers to access to care, late diagnosis, lack of opportunity for treatment and poor adherence to it, which are prevalent among native peoples in this case40. An example of this are the challenges faced by the indigenous communities of Australia, Canada, New Zealand, and the USA, whose access to health care is limited by co-pays and invisible costs, long distances, cultural barriers, and a large proportion of those populations being uninsured41. Latin America faces the same challenges and needs studies to identify the sociocultural, economic, and geographical factors that affect healthcare conditions42.
In this respect, the present study promotes cultural competencies, defined as a set of academic and interpersonal skills enabling the health professionals to deepen their understanding and appreciation of the cultural differences and similarities between human groups. This improves the interrelation between EMs in what concerns disease management. It should be emphasized as part of the academic training in view of global migratory processes by offering creative solutions, working together with trust, mutual respect, and relational contact to tackle inequalities and fight for international recognition of the right to health care for indigenous peoples43-45. These changes can optimize the use of national resources through cooperation in therapeutic decisions in a bid to improve clinical outcomes, and, in the particular case for Colombia, to help bring peace to a country that strives to put an end to over 50 years of armed conflict.
Interdisciplinary community studies in different extramural settings are an important tool for the early identification of diseases such as AR, with its clinical, economic, and social implications.
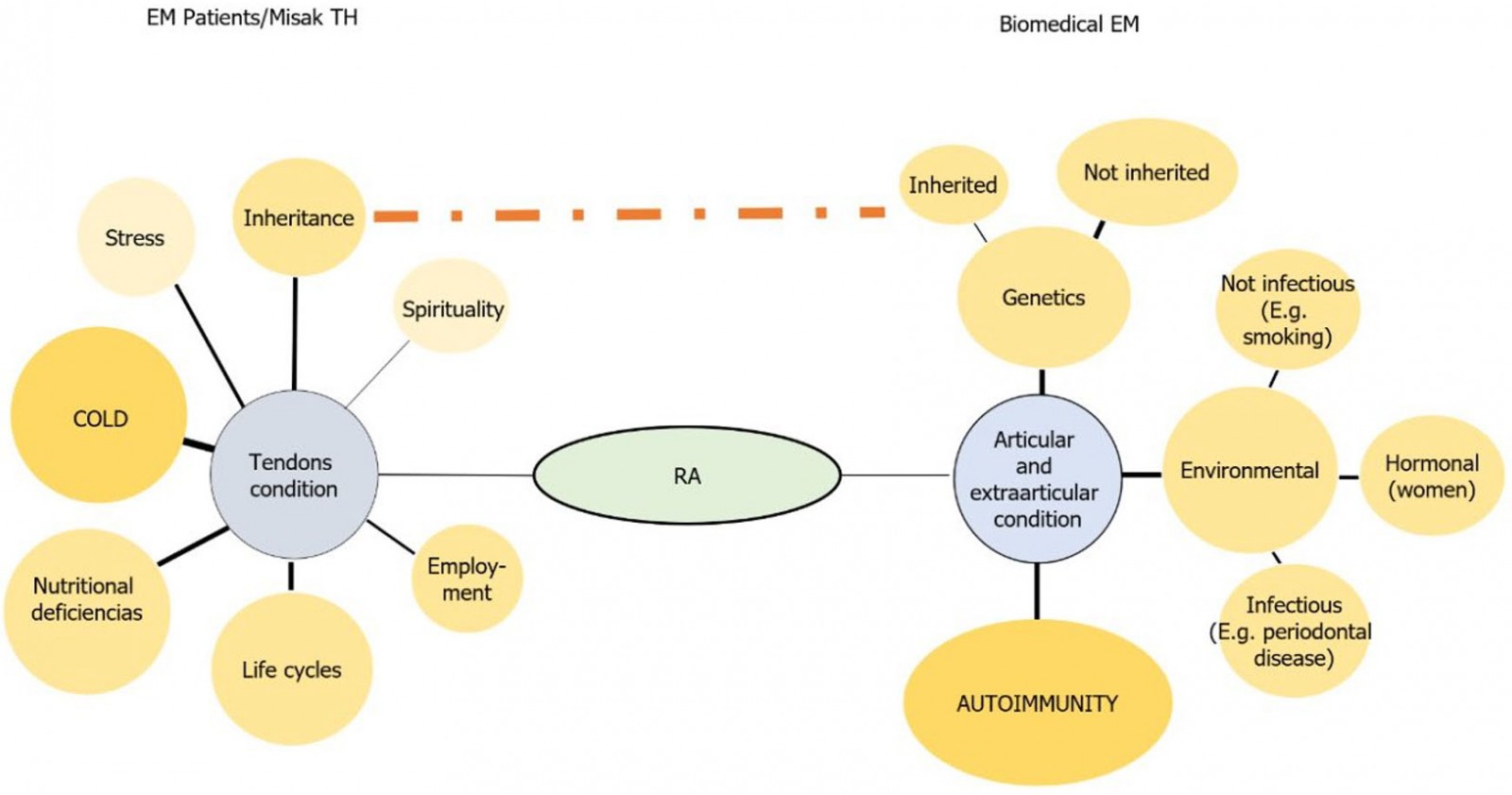 Figure 4: Etiology, pathophysiology, and diagnosis of rheumatoid arthritis in the explanatory models of patients and the Misak traditional healers, versus the biomedical explanatory model.
Figure 4: Etiology, pathophysiology, and diagnosis of rheumatoid arthritis in the explanatory models of patients and the Misak traditional healers, versus the biomedical explanatory model.
Strengths and limitations
This study describes an emergent, culturally sensitive healthcare model promoting intercultural care involving health professionals such as rheumatologists, physiatrists, physiotherapists, and orthopedists. The components that favor the sustainability of this model over time are described, such as members of the indigenous community becoming healthcare professionals outside their usual context and returning to practice the medical profession in their communities.
The study does not specify the number of patients who were attended exclusively by the traditional healers, biomedical physicians, or both, nor does it specify the type of DMARD treatment they received because they didn’t remember them, and a review of the files of each one was not carried out. Researchers in this study didn’t have access to laboratory tests and didn’t specify the adherence to a treatment plan, traditional or biomedical, before switching to a different approach. Finally, it was outside the scope of this study to describe the clinical characteristics of the disease in the subject population, a feature that can influence their decision to choose one or another treatment.
Acknowledgements
We acknowledge the Universidad del Cauca, the indigenous authorities of the Misak reservation council, Mamá Dominga Hospital, Casa de Plantas-Sierra Morena and the study participants.
References
You might also be interested in:
2021 - Why do some medical graduates lose their intention to practise rurally?
2009 - Childhood obesity and elevated blood pressure in a rural population of northern Greece






