Dear Editor
It is increasingly important for health professionals to promote interprofessional education (IPE) in rural clinical settings1. Health professionals and students can create positive IPE experiences in rural learning environments, and evidence of positive outcomes is accumulating1,2. IPE means that students can learn in the same place and in cooperation with people from multiple professions. However, we observed that an incorrect educational style was adopted, although the title of the educational course included ‘interprofessional education’. In the course, individual professionals from different disciplines (eg nurses, medical social workers and pharmacists) working in vertically segmented organizations were invited to a lecture hall of an urban university to talk about their work experiences from their perspectives to medical students. We replaced this incorrect strategy with more appropriate educational practices in rural areas.
Interprofessional rapport-building is important to promote IPE in rural areas3, highlighting the importance of the following exploratory study. The present research strongly supports the message that shared space, adequate time and balance of disciplines are important elements to sustain IPE and retain health professionals in rural areas3. Although the study was conducted outside Australia, our results were similar.
The research settings were mountainous rural areas in Japan with poor traffic access, each of which had a population less than 11 000 inhabitants and was located at a distance of more than 80 km (1.5 hours’ travel time by car) from a major urban city with a population of approximately two million people. Semi-structured interviews were conducted with 29 physicians, nurses (including public health nurses), physical therapists, occupational therapists, registered dietitians, medical social workers and medical office workers. Their ages ranged from 26 to 61 years, averaging 38 years, and their years of experience ranged from 0.1 to 22 years, averaging 10 years. The authors contacted each interviewee by email or telephone to obtain appointments. Each interview took place in a pre-arranged private room within the participants’ institutions. Each interview lasted approximately 60 minutes, and the questions focused on issues concerning the implementation of IPE in rural areas. The recorded content was transcribed verbatim, encoded, divided into meaningful categories and aggregated.
Participants gave mostly positive responses to IPE; however, we identified the following four problem categories: lack of network development, lack of long-term local government plans, difficulties in making time for learning, and hierarchies among health professionals (Table 1).
The study showed that health professionals in rural areas support interprofessional collaboration and IPE, which may contribute to retaining health professionals in rural clinical settings. Doctors in rural areas actively cooperate to promote community-based medical education, despite heavy educational burdens4. The present research showed similar trends among other health professionals in rural areas. This study agrees with previous research5 promoting IPE in rural areas, as it provides future health professionals many learning opportunities and contributes to their personal development. This article presents international data that contribute to global perspectives on IPE.
Table 1: Four problems in interprofessional development identified by study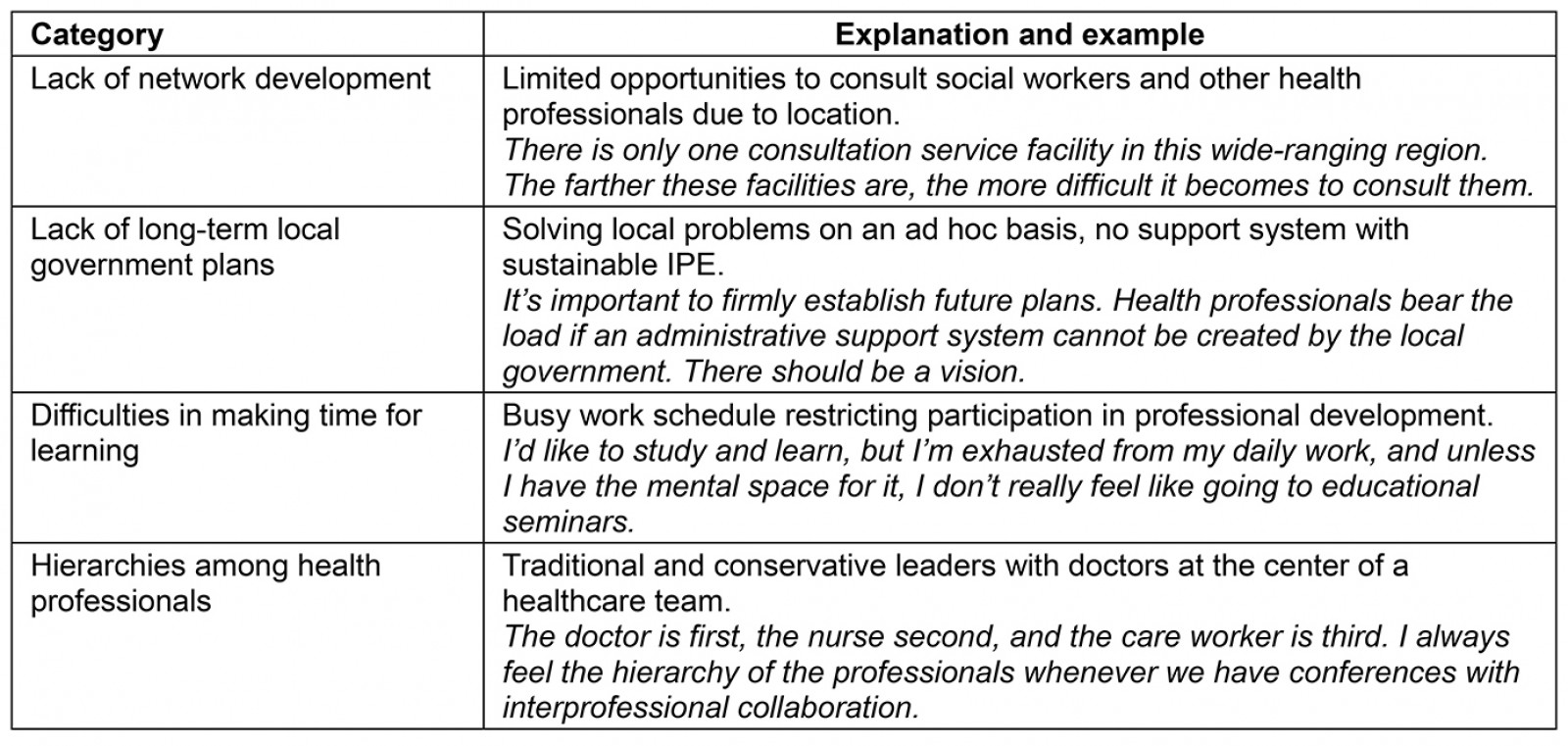
Acknowledgements
We thank all the health professionals who participated in our research.
Kotaro Matoba and Hideki Hyodoh, Hokkaido University, Sapporo, Japan
Manabu Murakami, Hokkaido University, Sapporo, Japan
References
You might also be interested in:
2022 - Home visits in rural general practice: what does the future hold?
2013 - Core clerkship in internal medicine at a rural community hospital in Israel
2010 - Health handicaps and advantages of the rural population in Hungary
