Introduction
Into whatever houses I enter, I will go into them for the benefit of the sick. (Hippocratic Oath, c. 400 BC)
The image of a doctor entering someone’s home carrying a black leather bag is one of the most traditional representations of medicine in the western world. Modern-day primary care and house calls have evolved from the origins of bedside medicine in ancient Greece, as documented in the writings of Hippocrates1. Interestingly, the Dutch term for ‘general practitioner’ (GP) is Huisarts, which literally translates as ‘home doctor’2. Is this quintessential element of general practice – that of visiting patients in their own home – going to become a thing of the past?
A decline in house-call rates has been documented in Europe, Australia and North America over the past 90 years3-9. Prior to the Second World War, doctors were more likely than patients to have access to transportation, and house calls made up almost 40% of a GP’s workload10. Following the decline in house calls between the 1930s and 1950s in the USA, their proportion of the workload constituted only 10%5. A 27% reduction in house calls was noted in England and Wales between the 1980s and 1990s4. In Australia, rates declined by over 50% in the 10 years between 1997 and 20078. Many of the studies documenting this decline took place between the 1980s and 2000s4,8,9, and up-to-date data on current rates are lacking. In addition, many of these studies examined house-call rates in urban or mixed settings3-5,8,11-13 with fewer focusing on rural areas14-16.
Systematic reviews and meta-analyses have tried to synthesise and evaluate the benefits of home visits. The variety of inclusion and exclusion criteria, and the heterogeneity of interventions, makes comparison and interpretation challenging. As such, the evidence for house calls is unclear and inconsistent.
Findings from systematic reviews have demonstrated no favourable effect from preventative house calls to older patients17, no benefit to patients in terms of mortality or functional status18, and, in contrast, that multifactorial preventative home visits can prevent admission to institutional care in an older population19.
The results of combined systematic reviews and meta-analyses have also demonstrated inconsistent results: home visiting programs can reduce mortality and admission to long-term care in older patients20, multidimensional geriatric assessment (including house calls) can improve functional status and mortality in the ‘younger’ older population (aged less than 77 years)21, preventive house calls to a younger elderly population have a positive effect on mortality and decline in functional status22 or no consistent evidence of improved mortality or independent living23. It is perhaps the necessary, but somewhat reductive, evaluation of house calls in terms of mortality, institutionalisation and functional status that may be overlooking their other important benefits.
A German qualitative study of general practitioners (GPs) showed all participants recognised the importance of house calls to an elderly population for detecting changes in health status, reviewing medications and assessing their home situation24. GPs reported they gained valuable insight into a patient’s environment – their compliance, abilities and family dynamics – and that this information contributed to better quality of care and aided complex decision-making around hospitalisation24. Further qualitative research describes how healthcare providers24,25, patients26,27 and relatives 26,27 felt house calls provided better, more patient-centred care, promoting trust in their doctor and improving the doctor–patient relationship.
Other studies have shown how clinic-based assessments of elderly patients miss two additional clinical problems and underestimate the severity of these problems compared with seeing that patient in a home setting28,29. The most clinically important problems identified when visiting a patient with dementia at home were found to be patient safety issues and caregiver stress – vital components of holistic geriatric assessment29. House calls can allow patients who are socially vulnerable, immobile or lacking transport to access health care7. In the palliative setting, they provide meaningful continuity of care and allow end-of-life care in the patient’s own home7, a key marker of end-of-life care success26.
House calls have been criticised as time consuming and poorly reimbursed when compared to seeing a patient in a clinic setting7,24. However, house calls are most often utilised by elderly patients3,6-8,14-16, a population for whom in-office assessment is often less suitable5,30. The elderly population across Europe is set to increase over the next 30 years, and globally there will be an increase in the old-age dependency ratio31. This population has increasing multimorbidity, which is associated with increased healthcare utilisation and cost32-34. There is also a shift in healthcare toward earlier discharge and management of chronic conditions in the community35,36. The growth of this cohort with complex community healthcare needs necessitates careful consideration of what constitutes cost-effective healthcare delivery.
Research across the world has shown common reasons for house calls. Studies from the UK4, Denmark11, Greece12, North America5, Canada37, Israel15 and Ireland3,38 reveal similar themes – respiratory illness, infection, cardiovascular complaints, musculoskeletal problems and palliative care are the most common. However, there is a lack of published information characterising the reasons for house calls in a rural setting15.
To facilitate the debate on the place of house calls in the future of general practice, this study aimed to provide an up-to-date assessment of the rate and the characteristics of house calls in a rural general practice setting.
Methods
Study design
A descriptive observational study was undertaken.
Sampling and recruitment
A total of 22 GP training practices in the north-west of Ireland were invited to participate in the study. These practices were chosen to enable comparison with a similar cohort studied in 2009 by Stewart and Stewart14.
Data collection
Data were collected on every house call in each practice over a 2-month period (May-June 2019). The data collection tool was completed retrospectively at the end of each week. This was undertaken by the GP trainer and data controller in each participating practice to comply with general data protection regulations. Irrevocably anonymised data was collected on gender, age category, who initiated the visit, whether it was routine, urgent or emergency, the medical reason for the visit, the reason the patient could not come to the practice, the treatment given or outcome of the visit, and whether the call took place within or outside of normal working hours. Data for out-of-hours house calls were obtained from discharge summaries sent to the practices the following day by the local out-of-hours service.
Data analysis
Microsoft Excel was used for data storage and analysis. GraphPad v8.4.1 (GraphPad Software; http://www.graphpad.com) was used for statistical analysis. Binary variables were calculated using the χ2 test.
Ethics approval
Ethics approval was granted by the Irish College of General Practitioners Research Ethics Committee.
Results
Eighteen of the 22 training practices invited to participate consented to take part in the project. Four practices withdrew prior to commencement of data collection, citing changes to workload or resourcing, leaving 14 training practices who completed the project. These 14 practices had approximately 30 000 ‘public’ patients in their practices (patients eligible for means-tested free GP care). Data were received on 547 house calls. Of these, 443 were done within normal working hours (0800–1800, Monday–Friday), 100 were done out of hours and four were unclassified and excluded from initial analysis. The rate of house calls within normal working hours was calculated at 87 house calls/1000 patients/year, which translates to a raw proportion of 1.44%. Using the N-1 χ2 test, this rate was compared to the rate calculated in the 2009 study (143/1000/year; raw proportion 2.43%), also for house calls done within normal working hours14. When compared, the difference between these two proportions was 0.991% (95% confidence interval (CI) 0.759–1.22%; p<0.001). Therefore, direct comparison of the 2009 rate (143/1000) to the 2019 rate (87/1000) shows a statistically significant reduction of 40% over a 10-year period. Additional analysis categorising the four unclassified calls as within working hours also produced a statistically significant reduction.
Analysis of the 443 house calls within normal working hours (Fig1) showed that 86.2% of patients were aged over 65 years, with 45% of those aged over 85 years. There was a statistically significant difference in house-call rate according to gender, with 58.6% (95%CI 0.54–0.64%; p<0.001) of visits being to females. Fifty-three percent of house-call requests were made by a relative (Fig2), with 15.1% requested by the patient themselves, and 6% initiated by the GP. In the majority (55%), the patient was too immobile to travel to the GP surgery for assessment (as opposed to being ‘too unwell’ or having ‘no transport’). The most common medical reason for a house call was infection related (34%) (Fig3) and, within that category, respiratory infection was identified most frequently. Palliative care and pain-related presentations represented 11% each of total house calls. Procedures such as urinary catheterisation and phlebotomy were the primary reason for the call in 10% of cases. Most calls (52.1%) were deemed urgent (to be seen within 24 hours). In terms of the main outcomes of the house calls, 88.3% of patients were managed in the community, with only 11.7% referred on to hospital. Overall, 45.8% of patients’ management involved a prescription from the GP and 17.1% required no further intervention (Fig4).
Analysis was then undertaken on 100 house calls done outside of normal working hours (1800–0800 Monday–Friday, and 24 hours Saturday and Sunday). In general, the medical reasons for the calls were broadly similar to those within normal hours, as shown in Figure 5. Significantly more patients were found to be too unwell to travel (44% out of hours compared to 30% within normal hours, 95%CI 0.34–0.54%; p<0.05). Significantly more medication was administered by GPs out of hours (25% v 10% in normal hours, 95%CI 0.17–0.35%; p<0.001), and, while not reaching statistical significance, fewer prescriptions for the pharmacy were issued out of hours than within normal hours (37% v 5.8%, respectively).
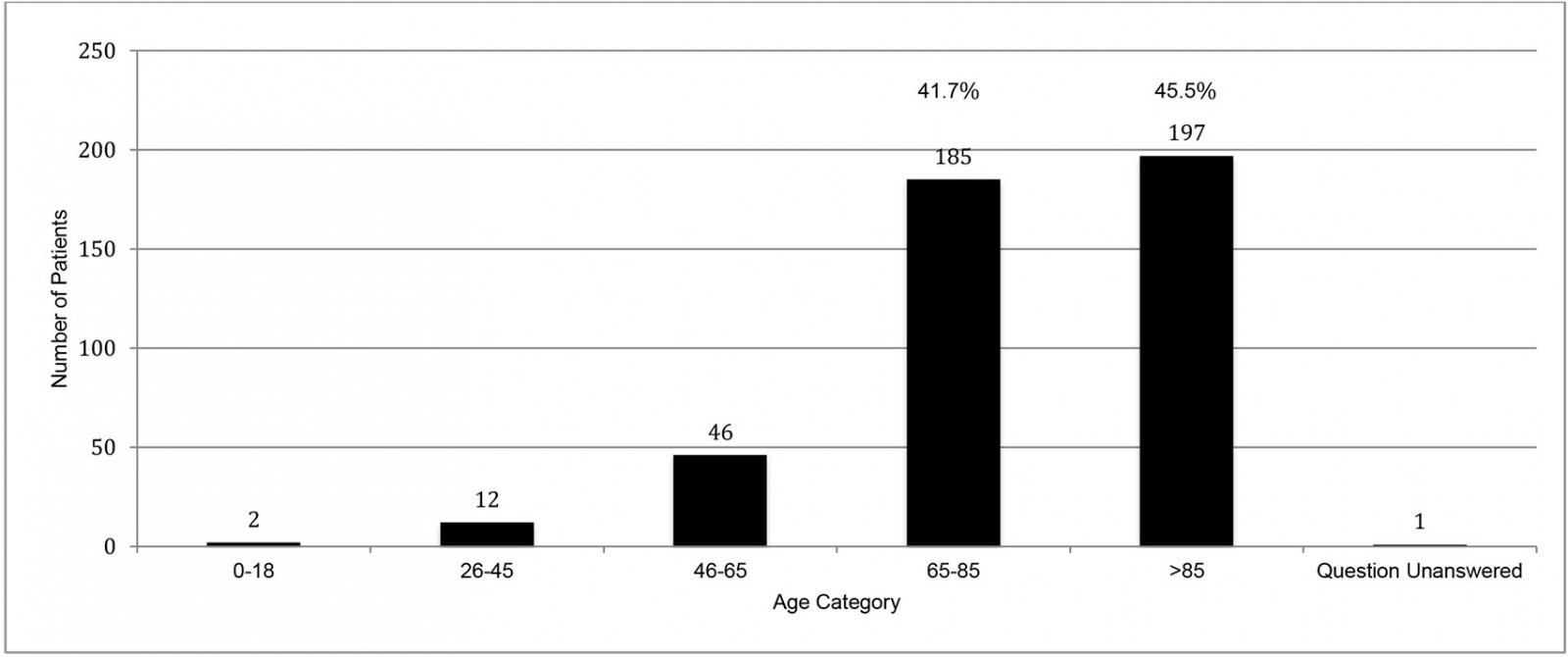 Figure 1: Age of house call patient for 14 GP training practices for in-hours house calls (n=443) in County Donegal, north-west Ireland, May–June 2019
Figure 1: Age of house call patient for 14 GP training practices for in-hours house calls (n=443) in County Donegal, north-west Ireland, May–June 2019
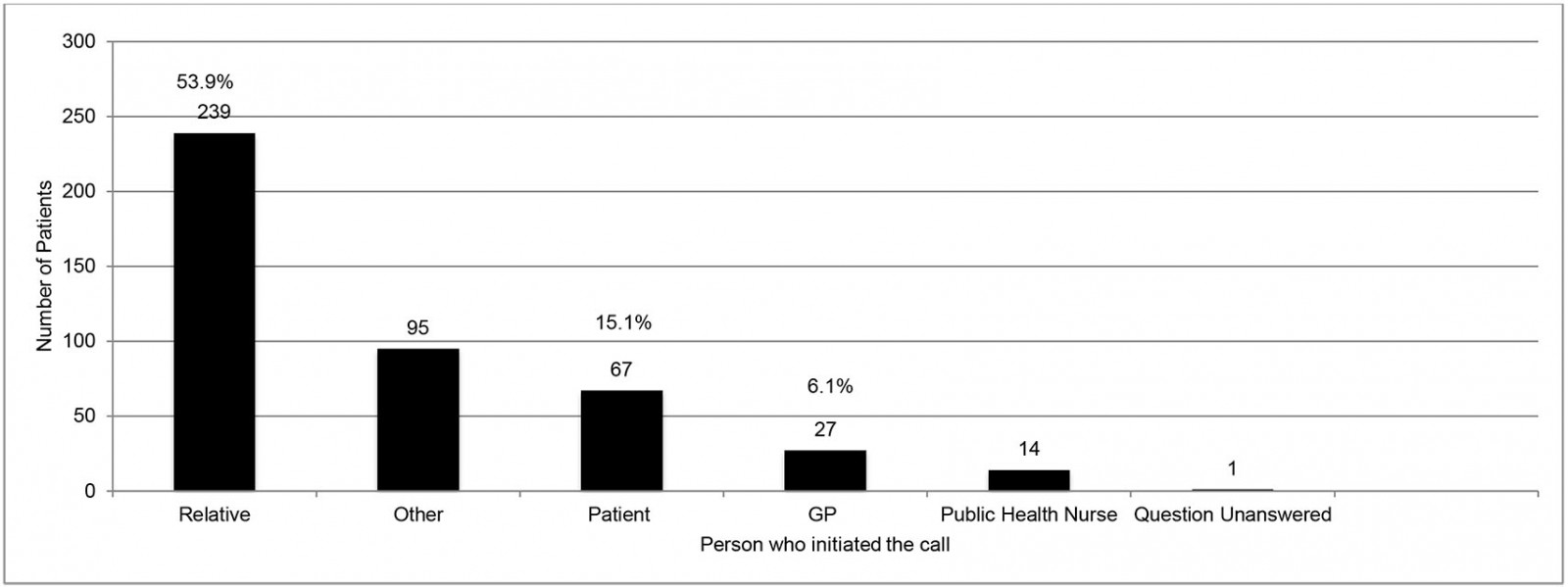 Figure 2: Initiator of house call for 14 GP training practices for in-hours house calls (n=443) in County Donegal, north-west Ireland, May–June 2019
Figure 2: Initiator of house call for 14 GP training practices for in-hours house calls (n=443) in County Donegal, north-west Ireland, May–June 2019
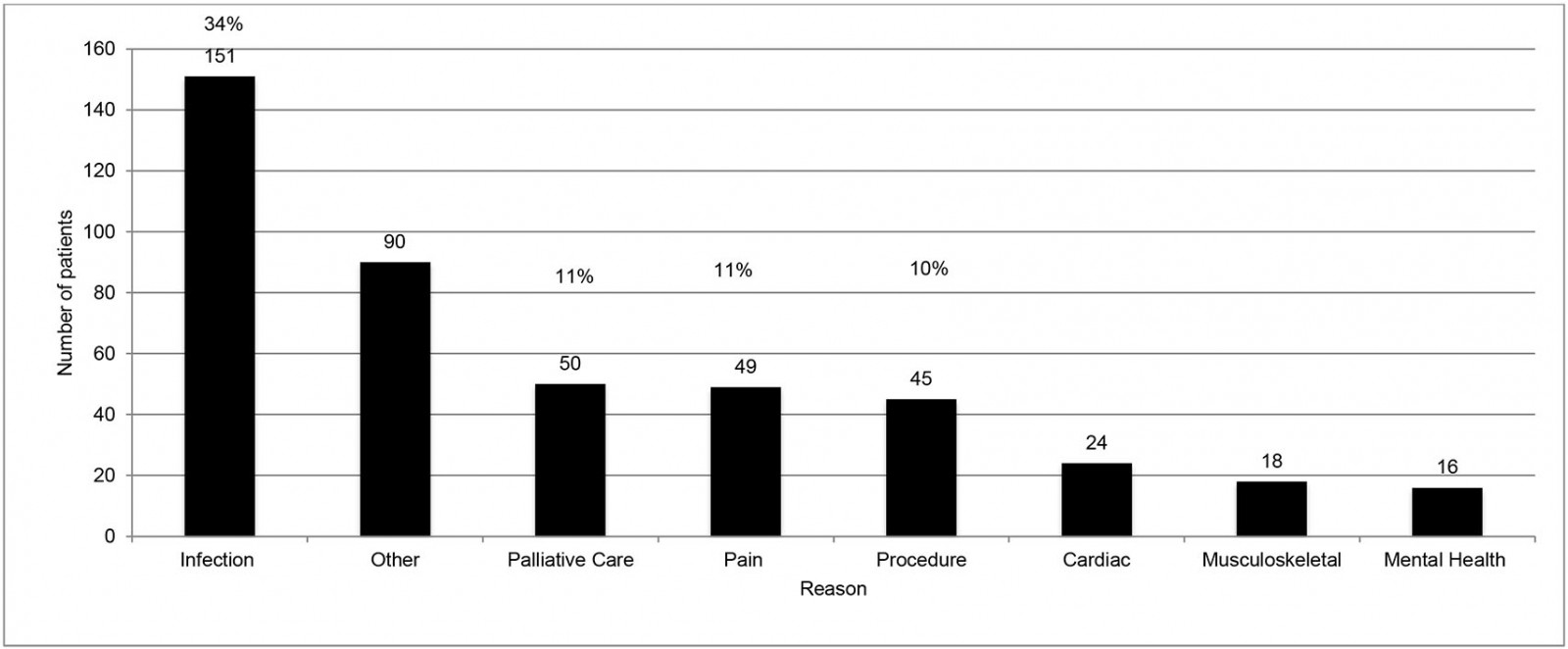 Figure 3: Reason for house call for 14 GP training practices for in-hours house calls (n=443) in County Donegal, north-west Ireland, May–June 2019
Figure 3: Reason for house call for 14 GP training practices for in-hours house calls (n=443) in County Donegal, north-west Ireland, May–June 2019
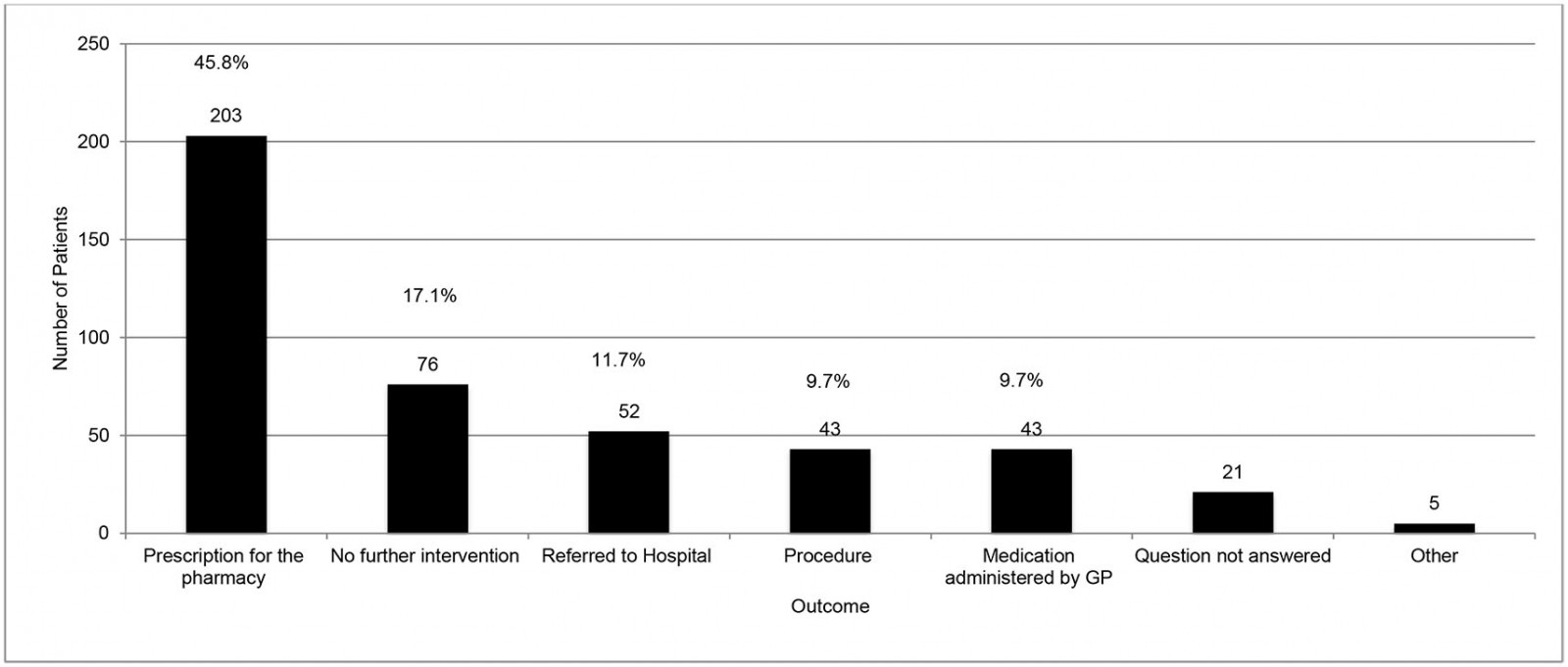 Figure 4: Outcome of house call for 14 GP training practices for in-hours house calls (n=443) in County Donegal, north-west Ireland, May–June 2019
Figure 4: Outcome of house call for 14 GP training practices for in-hours house calls (n=443) in County Donegal, north-west Ireland, May–June 2019
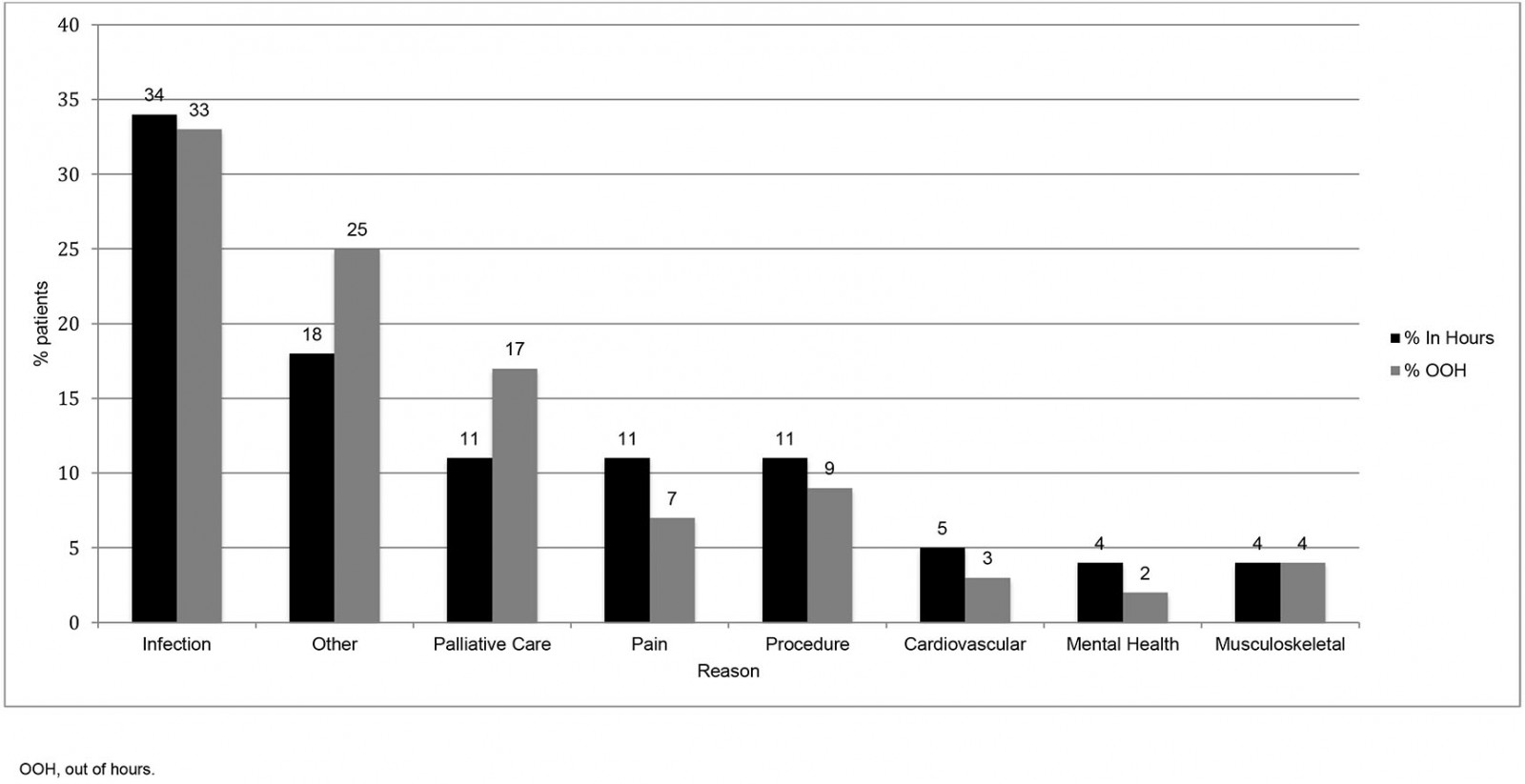 Figure 5: Working-hours and out-of-hours house call by reason for 14 GP training practices (n=543) in County Donegal, north-west Ireland, May–June 2019
Figure 5: Working-hours and out-of-hours house call by reason for 14 GP training practices (n=543) in County Donegal, north-west Ireland, May–June 2019
Discussion
Despite the traditional link between rural general practice and house calls, this study demonstrates a statistically significant decline of 40% in the rate of house calls over the preceding 10 years. It confirms that the vast majority of house calls in rural settings are to people aged over 65 years, which is consistent with other rural studies14-16. In addition, it provides data on the reasons for these calls, demonstrating that infection-related, palliative care and pain-related presentations are the most common. Importantly, this study shows that the vast majority of house-call presentations are managed in the community by the GP. These data will facilitate the debate around the place of house calls in 21st-century general practice.
Strengths and limitations
This study sampled a large cohort of patients. The population in the north-west of Ireland (County Donegal) is approximately 160 00039. There are just over 93 000 patients with a medical card in this region, entitling them to means-tested free GP care40. The house-call data here represent approximately 30 000 patients, which is approximately one-third of the population in this area with these entitlements39. Feedback on the data collection tool was that it was quick and easy to use, and the completeness of data collection sheets supported this. The category ‘other’ was selected in several sections but, helpfully, explanatory material was often recorded as free text. A more extensive pilot study may have revealed that further options such as pronouncement of death or stroke/transient ischemic attack needed to be included as reasons for house calls, but this information is now available for future research in this area.
The number of out-of-hours house calls recorded was fewer than expected, suggesting that recording of information on this subset may not be as complete as that for normal hours. In the north-west of Ireland, data from out-of-hours house calls is sent to practices the following day and so this may not always have been included in the practice’s weekly house-call tally. For this reason, data relating to out-of-hours house calls needs to be interpreted with caution.
Comparison with existing literature
In keeping with the literature on house-call rates worldwide3-5,7-9, a significant decline in a rural setting has been demonstrated here. This 40% decrease in house calls in a decade shows a similar trend to that in an urban Irish setting (22% decline over 4 years)3 and in the Netherlands (48% decline over 13 years)13. A more recent large Australian study demonstrated a 51% decline in a decade (1997–2007)8.
Political and health system changes like the abolition of distance-related payments for house calls in Ireland41, and GPs in the UK voting to remove the contractual responsibility for house calls42, could affect local and short-term house-call rates, but the consistent and widespread findings across the world suggest that this is a robust trend. In this context, it is important to ask why the house-call rate is declining. Literature discussing the decline cites GP workload resulting in lack of capacity42, more urgent calls being passed to emergency services24, concerns for personal safety43 and inadequate reimbursement9,24,36 as possible factors. However voices recognising the value of house calls and reluctance to give them up have also been heard44,45.
Implications for research and/or practice
These findings have important implications for general practice going forward. Most house calls were for elderly patients; in fact, 85% of all calls were for those aged over 65 years and 45% for patients over 85 years. The Irish population aged over 85 years is set to double in the next 10 years46 and there is a similar trend seen across Europe, with the population over 80 years predicted to reach 11.4% by 205031. This increase is not unique to Europe and can be seen worldwide, even in regions with high birth rates31. If the health system loses capacity or skill set to deliver house calls, it may be suggested that the needs of this growing elderly cohort of patients will no longer be served as well as they could.
This study provides data on the reasons for house calls, with the commonest reasons (infection, palliative care and pain) being for presentations typically managed by GPs. This, supported by the finding that only a small proportion of calls required onward referral, reinforces that GPs are ideally placed to carry out such calls, particularly when 55.5% required medications to be administered or prescribed (Fig4). This finding is relevant when considering whether delegation of house calls to other healthcare providers presents an efficient use of resources for patient and provider45.
Investigating why the house-call rate is falling (by nature or by design?) is a necessary area of future research to address the deficiencies in the current literature described above. Central to decisions about service provision is the identification of when, where and for whom house calls are an effective use of resources. This requires both quantitative and qualitative methodologies involving GPs and patients, as well as other relevant stakeholders. A future study collecting demographic data on the general practitioners who provide house calls (e.g. age, years in practice) could facilitate an analytical observational study. This study’s finding that most house calls were requested by a relative indicates this group might be an information-rich cohort for further qualitative exploration. Qualitative research on the impact of house calls on both patients and their caregivers would be extremely valuable and of great interest.
Conclusion
This study has shown a statistically significant decline in the rate of house calls in rural general practice in the past 10 years. These calls were mainly to elderly patients, and the majority were managed by the GP in the community. The juxtaposition of a decline in house calls with the projected expansion of the population that most uses them demands us to now decide if house calls are worth saving, before it is too late.
Acknowledgements
We acknowledge Peter McCrystal for statistical support and data analysis.
References
You might also be interested in:
2009 - Challenges faced in implementation of a telehealth enabled chronic wound care system
2008 - National Centre of Rural Medicine in Norway: a bridge from rural practice to the academy

