Introduction
There is a growing interest worldwide in the fear of childbirth, as shown in bibliometric analyses1 as well as in several meta-analyses2 systematic reviews3-7 and meta-syntheses8,9. Fear of birth could present during pregnancy or after birth1. Fear of birth is increasing and occurs in 14% of women of childbearing age worldwide2, as concluded in a systematic review and meta-analysis of 33 studies from 18 countries with a total of 853 988 pregnant women included. The prevalence of fear of birth ranged from 3.7% to 43% and there was a large heterogeneity, probably based on lack of consensus regarding definitions2. The lack of clear definitions of how to measure and diagnose fear of birth has been acknowledged in several reviews3,4.
A systematic review of 24 scientific papers from nine developed countries comprised data from a total of 862 108 women5. Fear of birth was measured on different scales in the studies. Seven of those studies used the same instrument for measuring fear of birth but yielded a range of fear of birth from 6% to 15%. The most commonly used scale, the Wijma Delivery Expectancy Questionnaire10, has been criticised for its length and lack of cultural transferability6, thus a clinical tool focusing solely on fear of birth is needed5,6.
Fear of giving birth could affect women’s health in various ways. Previous systematic reviews and studies with other designs have shown that fear of birth is associated with perinatal mental health problems, such as anxiety and depression3,4,11, maternal requests for caesarean section4,12,13 and a higher use of epidural3. In addition, women with a fear of birth usually have less positive experiences of birth14,15. Treatment for fear of birth was investigated in a review of 18 studies; it suggested that counselling, psycho-education and prenatal preparation might be effective in treating fear of birth, but the authors admitted that cognitive behavioural therapy and relaxation techniques warranted more research7.
Women’s experiences of fear of birth have been described in a meta-synthesis of 14 qualitative articles8. The main finding was described using the metaphor of ‘being at the point of no return’. The authors concluded that women with a fear of birth need support and acknowledgement of their feelings and experiences – especially in the case of a previous negative birth experience – to regain trust in maternity care8. O’Connell et al9 conducted a systematic review and meta-synthesis of seven qualitative papers investigating women’s experiences of interventions for treating fear of birth. The interventions used in the studies were continuity of midwifery care in terms of team midwifery, psycho-education, art therapy, counselling with midwives and internet-based cognitive therapy. Women’s experiences were mirrored in the overarching theme ‘ownership of childbirth’. The authors highlighted the need for identifying and acknowledging women’s fears9. Few studies have used a salutogenic perspective in terms of sense of coherence16 on fear of birth (eg factors protective for maintaining health and stability when facing stressful life situations). Ferguson et al17 concluded, in a literature review of 15 studies, that women with a high sense of coherence reported better emotional health and were less anxious, depressed and stressed.
The problem of a lack of both definitions and measures regarding fear of birth is well known. Some studies suggest that fear of birth is solely a variation of anxiety18 and should be described by psychological characteristics, due to heterogeneity, but no consensus has been reached. As a response to these shortcomings, one of the health authorities in Sweden19 recently released a systematic review based on 31 scientific papers and concluded that visual analogue scales could be used to identify women with a fear of birth in need of further treatment but also concluded that studies of effective interventions are few and far between. The Fear of Birth Scale (FOBS) is based on two visual analogue scales and is used to identify fear of birth during pregnancy20,21. It has been used in a variety of populations6,22, but few studies have repeatedly assessed women before and after birth as well as the case of a future birth. The aim of the present study was to explore the trajectories of fear of birth and associated factors in a sample of women living in a rural area of Sweden.
Methods
Context of care
For the provision of maternity care, Sweden is divided into 21 independent regions, financed through taxes, with no additional fees to be paid by women. Antenatal care usually takes place within the primary healthcare sector and is community based. Midwives working in antenatal care are usually based in a health centre together with general practitioners, district nurses, child health nurses, physiotherapists and occupational therapists. The antenatal midwife is the main caregiver for pregnant women during the recommended eight or nine visits during an uncomplicated pregnancy. The women are linked through a referral system to obstetricians in case of pregnancy complications23. There is good continuity of caregiver during pregnancy, but not always between other episodes of care, namely antenatal, intrapartum and postpartum. In addition to providing care to pregnant women, antenatal midwives prescribe contraceptives and conduct pap smears for women listed as patients in the health centre. The midwife in antenatal care usually works only during the day.
Intrapartum care is hospital based, within specialist care, which is a separate management system. Midwives who work in hospitals do not usually rotate to antenatal care; they work in two or three shifts or the night shift only, and many rotate between the labour ward and postnatal/gynaecological ward. Rotation areas might differ depending on the size of the hospital. Large hospitals usually have separate labour wards, postnatal wards and gynaecological wards, while smaller hospitals have integrated care. The midwives are responsible for uncomplicated births and work in collaboration with obstetricians in complicated cases or in emergent events. Swedish labour wards are highly medicalised and centralised. The majority of small hospitals in rural areas have been closed for the past 20 years. Alternative birth options, such as homebirths, birth centres or midwife-led models of care, are rare in Sweden. There are also few national guidelines for maternity services23.
Design
This is a cohort study of women recruited in mid-pregnancy. It was conducted in the northern part of Sweden where pregnant women were offered extended services with birth assistance from a known midwife, in addition to antenatal care24.
Setting
The study was conducted at an antenatal clinic in a rural area of Sweden. Shortly before the study started, the local labour ward closed, and women then had to travel 100–120 km to the nearest hospital with a labour ward. The antenatal clinic is based in the local hospital and incorporated within the specialist care area, where one hospital floor comprises a gynaecological outpatient clinic, an ultrasound clinic, the antenatal clinic and a postnatal revisit clinic. The extended services entailed having a known midwife (one of four midwives) for birth assistance during part of the day. The midwives followed a rotation schedule for the on-call service, and one midwife was available from 7 am to 11 pm daily, with some exceptions, such as summer holidays and internal education sessions for the midwives24.
Participants and recruitment
All women who came to their booking visit were allocated a midwife, whom they met with during the majority of their antenatal visits. Women who consented to participate in the study had the opportunity to meet the other midwives both during the visits as well as in parenting classes and informational meetings. The recruitment started in February 2017, and women with a due date from 1 August 2017 to 30 June 2019 were eligible to participate. Women born outside Sweden who understood the Swedish language well enough to communicate by telephone were also invited to participate. This was important at the onset of labour when the midwife was contacted. Women received oral and written information about the study when they contacted the antenatal clinic to book an appointment. There was also information available on the internet and on posters available in the waiting area of the clinic. When a woman went into labour she would contact the midwife on call, and plans would be made for assessment of labour onset. The midwife would go to the labour ward of the woman’s choice and assist during labour and birth. If the woman went on early discharge after birth, follow-up consultations and paediatric examinations were performed in the local hospital24.
Data collection
Data were collected by two questionnaires sent to the women’s home addresses. Reminders were sent by text message after 2 and 4 weeks to those who did not return the questionnaire. The first questionnaire, completed in mid-pregnancy, collected sociodemographic, obstetric and medical information.
Fear of Birth Scale: The variable of interest was response on the Fear of Birth Scale (FOBS). The FOBS starts with this question ‘How do you feel when thinking about the approaching birth?’ The FOBS consists of two 100 mm visual analogue scales with the anchor terms ‘calm’ – ‘worried’ and ‘no fear’ – ‘strong fear’20,21. Women were instructed to place marks on both lines, which are measured and averaged. A cut-off point of 60 or more indicates fear of birth. For this study, FOBS was collected in the first questionnaire completed in mid-pregnancy and twice more after giving birth. The wording of FOBS after birth was ‘How do you assess worry and fear when thinking about the birth?’ and ‘How do you assess worry and fear when thinking about a future birth?’ The anchor terms were similar in all measures. To follow the trajectory of fear of birth, a composite variable was created, where 0 = ‘no fear during or after pregnancy’ (FOBS <60 on all three measures); 1 = ‘no fear in mid-pregnancy’, but FOBS scores 60 or more presented in retrospect or thinking about a future birth; 2 = FOBS score 60 or more in mid-pregnancy, but not after birth (in retrospect or in case of a future birth); 3 = FOBS scores 60 or more on all three measures.
Background characteristics: The first questionnaire collected information about the women’s sociodemographic background (age, parity, country of birth, marital status, level of education). Women were instructed to self-rate their physical and emotional health on four-point Likert scales, ranging from ‘very good’ to ‘very bad’. To further determine women’s emotional health, the 10-item Edinburgh Postnatal Depression Scale (EPDS) was used25, with a cut-off point of 13 or more as suggested when used during pregnancy26. EPDS mainly identifies depressive symptoms, but three of the 10 questions refer to anxiety. As an indicator of personality traits, the Sense of Coherence Scale was used16. The 13 items were summed to produce a total score and thereafter grouped into low (<60), moderate (61–75) and high (≥76).
Birth-related variables: Two months after birth, a follow-up questionnaire was distributed to the participants with a prepaid envelope. The questionnaire asked about the women’s experiences of their antenatal and intrapartum care, for example the number of visits to a midwife and/or to a doctor (obstetrician), the number of midwives met during pregnancy and the women’s opinions about the number of healthcare providers. Women were asked if they had had counselling due to fear of birth and, if so, who provided the counselling. The second questionnaire included questions about gestational weeks at birth, onset of labour, mode of birth, use of epidural anaesthesia, use of augmentation with synthetic oxytocin, self-assessed birth complication, neonatal transfer and if there was a known midwife assisting during labour and birth. The women’s birth experiences were summarised on a five-point Likert scale, ranging from ‘very positive’ to ‘very negative’27. The response alternatives were collapsed into ‘positive’ (1–2) and ‘less positive’ (3–5).
Analysis
Statistical analysis was conducted using SPSS Statistics for Windows, v25 (IBM, http://www.spss.com). Descriptive statistics were used to present data. A repeated-measures ANOVA was performed to explore change over time in the FOBS. Crude and adjusted odds ratios with a 95% confidence interval were calculated between the explanatory variables and the composite variable using a multinomial logistic regression analysis28.
Ethics approval
The study was approved by the regional ethics committee in Umeå, Sweden (dnr 2017/120-31). All women signed a consent form before participation.
Results
The first questionnaire was completed by 280 women and the follow-up questionnaire by a total of 236 women. Only responses of those who completed the FOBS were included in the analysis (n=228). Women not returning the follow-up questionnaire, after two reminders, were more likely to be born in a country outside Sweden (p<0.000) and not to have returned the first questionnaire (p<0.001).
Most of the women were aged 25–35 years, cohabiting with a partner and born in Sweden. The majority of respondents had a high school education, while 37% had a university degree. Women self-rated their physical health as being better than their mental health, and around 12% presented with depressive symptoms. The Sense of Coherence Scale showed that 63% presented with low or moderate sense of coherence (Table 1).
The mean FOBS score in mid-pregnancy was 46.61, with 32.6% of the women scoring 60 or more and being classified as having a fear of birth. The corresponding percentage after birth (in retrospect) was 21.9%, and 26.9% when thinking about a future birth. Table 2 shows descriptive statistics of worry, fear and the total FOBS score, with mean values and standard deviations. The FOBS score showed the highest values in mid-pregnancy, decreasing after birth and increasing again when thinking about a future birth. A one-way repeated measures ANOVA was conducted to compare scores on the FOBS in mid-pregnancy, in retrospect after birth and if thinking about a future birth. There was a significant effect for time, Wilks’ lambda=81, F=24.86, multivariate partial eta squared = 0.186, p=0.000.
The trajectory variable of FOBS shows that 122 women (54.2%) never scored FOBS 60 or more, 30 women (13.3%) did not have high FOBS scores in mid-pregnancy but did so after giving birth. Thirty-three women (14.7%) scored high on FOBS in mid-pregnancy but not after birth. Forty women (17.8%) scored high on all three measures.
Table 3 shows that no background variables were associated with the group of women who did not have a fear of birth in mid-pregnancy but who scored high on the FOBS after birth (group B). Women with a FOBS score of 60 or more in mid-pregnancy but who scored under 60 after giving birth (group C) were more likely to self-rate their physical and emotional health as less good. They also showed depressive symptoms and had a low sense of coherence. Similar characteristics were shown in women with fear during and after birth, with the added factor of having a low level of education (group D).
After birth, 7% of the women reported they gave birth before 37 gestational weeks, the majority followed the recommended eight or nine visits to the midwife and 58% met only one or two midwives during pregnancy. Quite a large number of women (57.5%) had paid a visit to an obstetrician, and 21% received counselling for fear of birth, the majority from the antenatal midwife. More than one in three women had an induction of labour (32%), 35% asked for an epidural and 36% needed augmentation with synthetic oxytocin during labour. The majority (79.7%) gave birth vaginally, 5.5% had an instrumental vaginal birth, 5.1% had a planned caesarean section and 9.7% had an emergency caesarean section. In total, 38% of the women self-reported a birth complication, and 14% of the newborn babies were transferred to a neonatal unit.
Antenatal and intrapartum variables were explored in relation to the four groups of women, based on their FOBS scores during pregnancy and after birth (Table 4). The group of women with low FOBS scores during pregnancy who developed fear after giving birth were compared with the group of women who did not present with fear during or after pregnancy (reference group). There were no background differences between the two groups. However, women who developed fear after birth were more likely to have had epidural anaesthesia, synthetic oxytocin for labour augmentation or an emergency caesarean section as the mode of birth. It was more common that the newborn babies were transferred to a neonatal unit and the odds ratio (OR) for a less positive birth experience was higher (OR 17.04) compared to women in the reference group.
Women with high FOBS during pregnancy but not after birth presented with worse self-assessed health during pregnancy, high EPDS scores and a low sense of coherence (Table 4). Of the variables collected after birth, women in this group were more likely to have had visits to an obstetrician and have had counselling for their fear during pregnancy. No intrapartum variables showed any significant difference when compared to women in the reference group.
Finally, women with a fear of birth both during and after pregnancy were characterized by a low level of education, worse self-rated physical and mental health, more depressive symptoms and low or moderate sense of coherence. During pregnancy, they were more likely to have had visits to an obstetrician and counselling. In addition, they were more likely to have had an emergency caesarean section, self-rated birth complication or a worse birth experience. All of the statistically significant variables remained significant when adjusted for background variables.
Table 1: Background of participants (mid-pregnancy)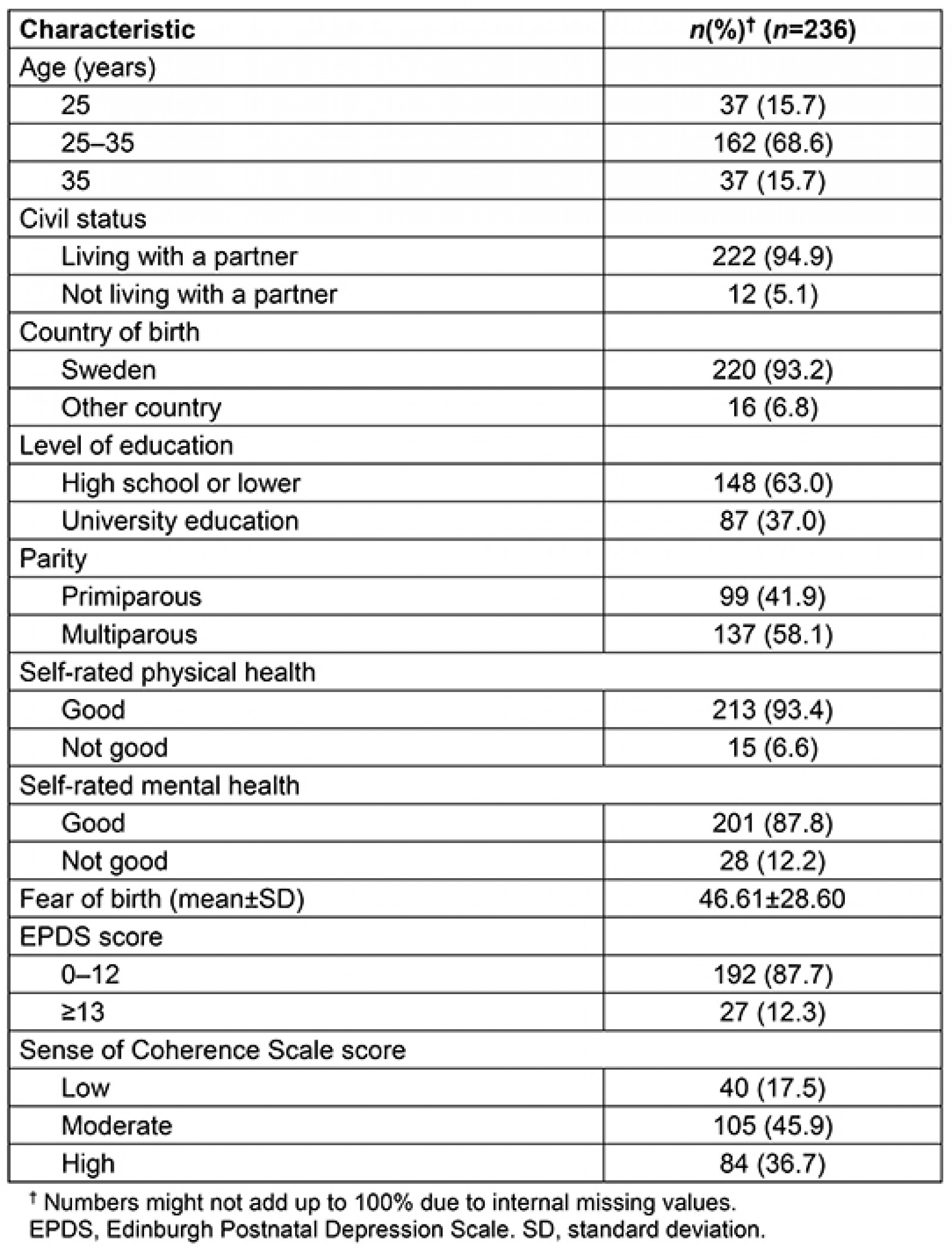
Table 2: Descriptive statistics for the Fear Of Birth Scale in mid-pregnancy, after birth and in case of a future birth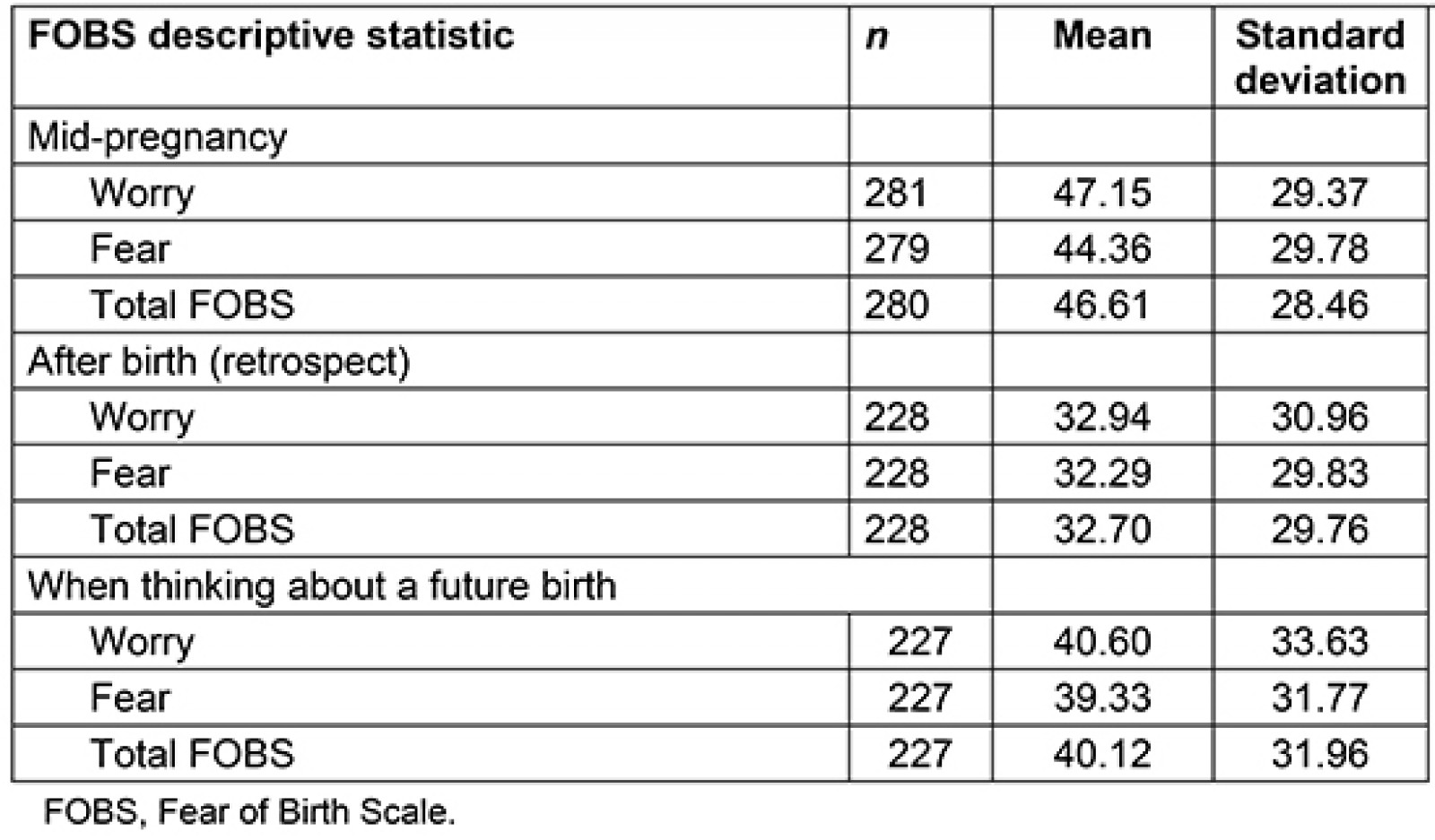
Table 3: Background factors in relation to the trajectory of fear of birth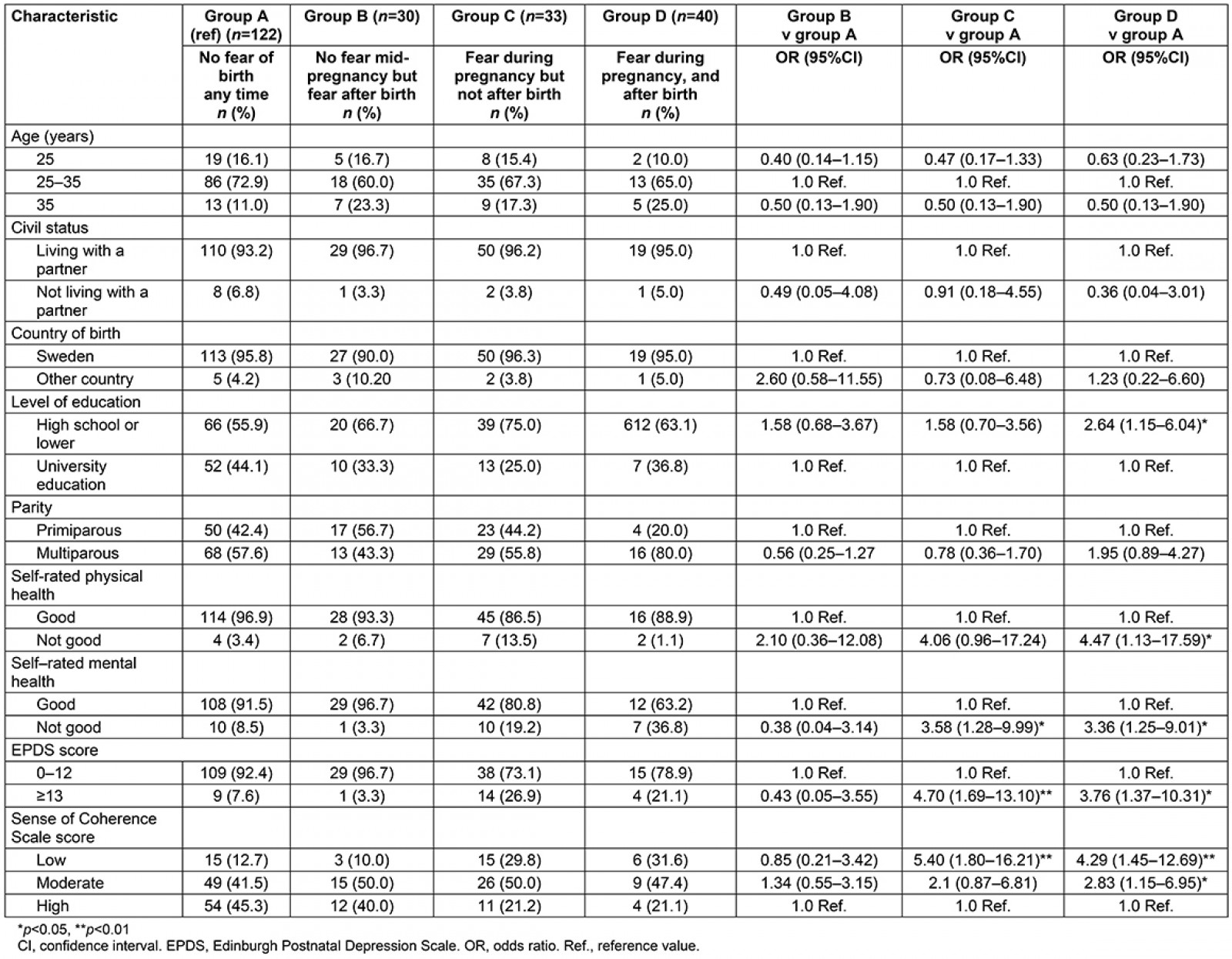
Table 4: Pregnancy and birth related factors in relation to the trajectory of fear of birth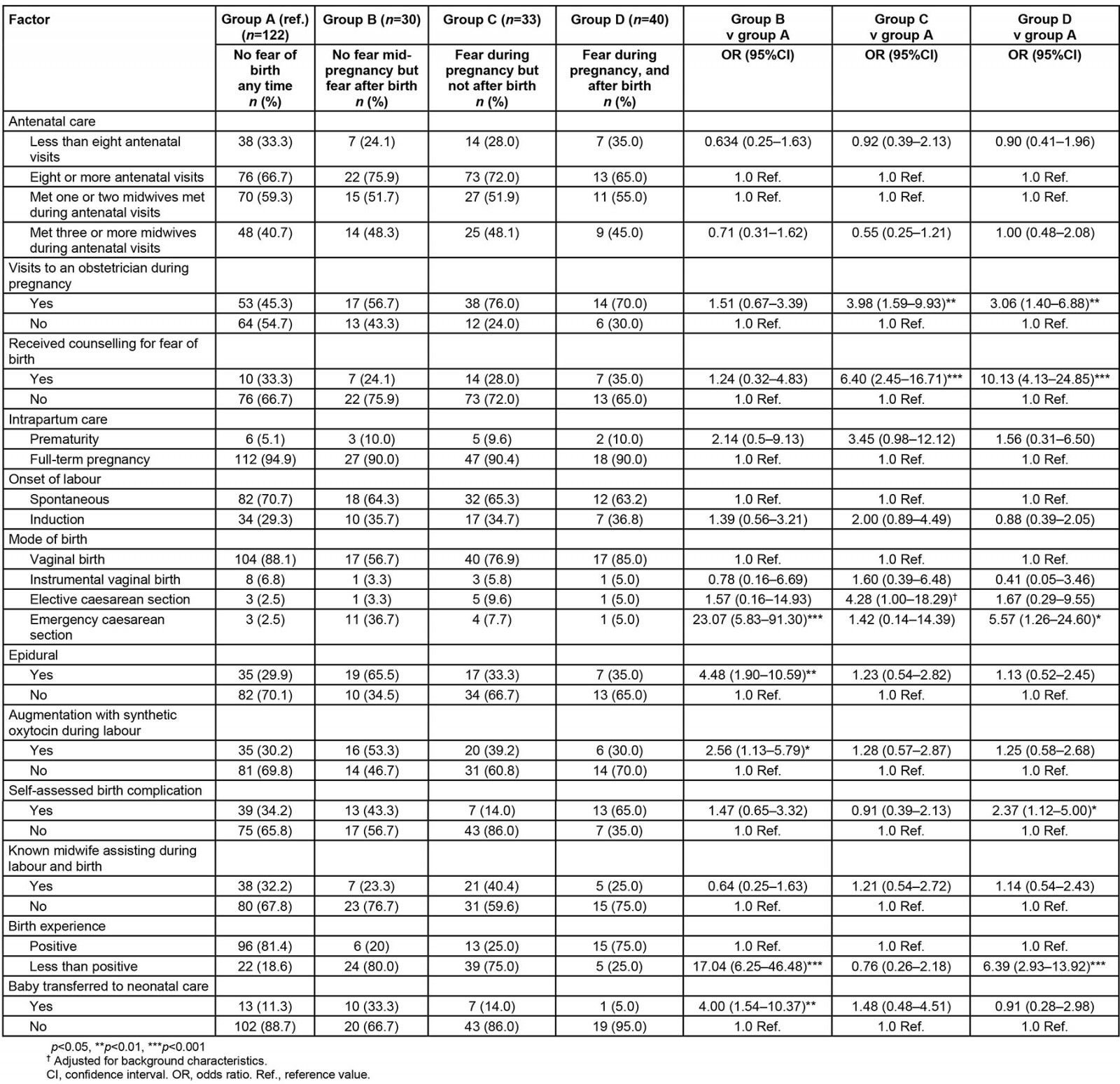
Discussion
The main findings of the present study were that a fear of birth fluctuated over the course of pregnancy and after birth. Factors associated with developing fear after birth were mainly related to the birth event, while reduction of fear was associated mainly with population characteristics and antenatal support. For some women, the levels of fear did not change, and these women were characterised with worse self-rated health and more negative experiences of having given birth.
When the FOBS was measured three times, a statistically significant change in the levels of fear became apparent. A previous population-based study conducted during 2008–2009 in the same area as the present study showed a continuous increase in the fear of birth from 12% in mid-pregnancy to 13.5% in late pregnancy and upward to 15.1% after giving birth. In that study, FOBS was not used, and fear of birth was assessed on a four-point Likert scale. The question was worded ‘Worries and fears are common feelings among men and women when facing childbirth. To what extent do you experience worries and fear?’ The response alternatives were ‘not at all’, ‘somewhat’, ‘a great deal’ and ‘very much’29.
When using the cut-off point of 60 on the three measures, 21.9–32.6% of the women in the present study were classified as experiencing fear of birth. These percentages are higher than those usually found in women who assessed their fear of birth using the FOBS22.
Studies offering treatment for women with fear of birth have shown a similar development of fear as in the present study. One example comes from an experimental study in which women with a fear of birth were offered birth assistance from a known midwife in addition to counselling30. Using the FOBS, the mean value in mid-pregnancy was 72.18. In retrospect, after giving birth, the FOBS mean was 36.75 and, looking ahead to a possible future birth, the mean value of FOBS was 45.27. Of note in this study, all women were diagnosed with fear of birth before entering the study, which can explain the difference in the mean scores compared to the present study. Another example comes from a randomised controlled trial where women with fear of birth were offered internet-based cognitive therapy or counselling with midwives. The result showed a decrease in FOBS scores over time, but no difference between the groups31.
In the present study, there was no measure of FOBS in late pregnancy, which limits the trustworthiness of the findings. Another important notion is the lack of reasons for women’s fear of birth. Many women wrote comments in the margins of the questionnaire that they were most afraid of giving birth in the car or on the road after the closure of the local hospital’s labour ward. Long distance to hospital has previously been acknowledged as an important factor creating uncertainty and fear32,33, resulting in more caesarean sections on maternal request and unassisted freebirths.
Women who developed fear in retrospect, after not being fearful during pregnancy, were more likely to have had a birth characterised by use of epidural and augmentation, an emergency caesarean section, a baby transferred to a neonatal unit or a less positive birth experience. All these factors are associated with fear of birth, as shown in many studies3,14,27.
The women who had FOBS scores of less than 60 after birth, while having presented with fear during pregnancy, had more mental health problems and a lower sense of coherence compared to women without fear. It is not known if they received any treatment for their mental health during pregnancy. No birth-related variables showed any statistically significant result when the group was compared to women without fear. One explanation could be that these women were satisfied with the number of children they now had and regarded the fear of birth as a problem solved. Another explanation could be that they actually were ‘cured’ by having had counselling and visits to an obstetrician. The midwives who provide antenatal care and counselling worked closely with a male obstetrician who was really compassionate in helping women with their fear of birth. Unfortunately, there was limited information in the questionnaires about what mattered most when it came to being ‘cured’. A previous study29 showed that women ‘cured’ of fear had a more positive birth experience, especially regarding feelings of control and satisfaction with information about the progress of labour.
Women who reported FOBS scores of 60 or more, both during pregnancy and after giving birth, showed some similar background characteristics with the women who were ‘cured’ of their fear of birth. They also demonstrated antenatal and birth factors similar to the women who developed fear after birth. A posthoc analysis revealed that women in this group with constantly high FOBS scores reported a mean value of 84.68 on the first measure of FOBS. This score decreased to 62.16 in retrospect and then increased to 83.41 (1.27 units less than at first) when thinking about a future birth. On the other hand, those who were ‘cured’ showed a 42.55 unit reduction from the first to the last measures. In the previously mentioned study30 with birth assistance from a known midwife, the same pattern was shown, with a 26.9 unit reduction in mean scores, and the levels of fear did not reach the original measures30. Based on these findings, it might be of importance not only to classify women based on the cut-off point of 60 or more on the FOBS, but also to take the actual level of fear into consideration.
Having a known midwife was not associated with the trajectory of fear in the present study. However, in the previously mentioned study where the counselling midwife also provided intrapartum care, 29% of women who actually had a known midwife assisting during labour and birth reported that their fear of giving birth disappeared30.
Women’s perception of their birth experience was a major contributing variable in those developing fear after birth and also when thinking about a future birth. Previous studies have also shown that women with a fear of giving birth are more likely to have a less positive birth experience27,29,34,35. On the other hand, studies of women with fear of birth who received intrapartum care from a known midwife showed that they were nearly five times more likely to have a positive birth experience (83% v 52%)36.
Despite the growing body of studies focusing on fear of birth, it is still not known for certain what actually works in reducing fear of birth. A recent review suggested that counselling, psychoeducation and prenatal preparation might be effective7. However, the latest Swedish governmental investigation concluded that the effect of interventions to treat fear of childbirth could not be estimated because there have been too few studies19.
Strengths and limitations
The study is compromised by its observational design, and by not including women who did not speak Swedish. There were some differences between participating women and non-participants, but no detailed information about reasons for not entering the project, due to the self-recruitment. Some of the differences, such as being born outside Sweden, which could imply difficulties in communicate in Swedish, could be explained by the project criteria. A total of 391 pregnant women in the area actually gave birth during the study period. The authors have information from birth records for 266 women in the project and 125 not in the project. A total of 110 women in the area were born outside Sweden (28%). However, the authors have no information about women’s actual language skills. The self-recruiting process makes it difficult to access eligibility, but it has been assumed that the 83 foreign-born women not included in the project were not Swedish-speaking at all. With this assumption, around 308 women would then have been eligible and the project reached 86% of those. This calculation must be viewed with caution as women might have had other reasons than language abilities for not participating. The women not responding to the follow-up were also more likely to be born in a country outside Sweden (p 0.000) and also more likely not to have completed the questionnaire in mid-pregnancy (p 0.000), suggesting that the midwives sometimes overestimated women’s language skills.
The different trajectories of fear showed similar birth characteristics as previous studies21,31, which strengthens the credibility.
Another limitation might be that anxiety was not measured distinctly, as it is known that fear of birth and anxiety are closely related18. However, the EPDS covers both depressive symptoms (seven items) and anxiety (three items), but in the present study EPDS was analysed as a total score. Other studies have shown that co-morbidities (eg anxiety, depressive symptoms and fear of birth) are fairly common11,37.
One strength of the study was the organization of care. Prior to the study, all antenatal care was offered in a community-based health centre. As the project offered continuity with a known midwife, and the midwives worked both in primary care and specialist hospital-based care (care during labour and birth) it was important to have the midwives working in one organisation only. This has been successful, and currently all antenatal care in the area is provided in the local hospital. The midwives (and the women) have excellent access to gynaecologists, obstetricians and ultrasound examinations during the day. This organisation benefits pregnant women (who usually are healthy) but also provides the opportunity for development of midwifery care, when all midwives work together. It is also easier for the midwives to help each other in case of sick leave or planning holidays.
Conclusion
Fear of birth usually seems to change over time and is mainly associated with women’s emotional wellbeing, circumstances surrounding the actual birth and the birth experience. Support during pregnancy could change the trajectory of the fear of birth. Women with high levels of fear rated their health lower and had a more negative birth experience. Further research is needed in how to best help women overcome their fear of birth. Possibly qualitative studies would be fruitful as women show their keenness to elaborate on responses about this topic.

