Introduction
Urban and rural areas have particular characteristics that affect the health and mortality of their inhabitants – the disparity in mortality between urban and rural areas has been widely described in the literature1. Urban areas are associated with high levels of physical and social factors that are potentially detrimental to maintaining good health, such as air pollution, stress, and fear of crime2. On the other hand, rural populations face challenges related to limited access to health services and poor nutrition. Furthermore, considering that their livelihoods depend on agriculture, they are particularly vulnerable to migration pressures3.
The mortality rate in urban and rural areas has been studied mainly in developed countries. In the US, in 2019, the adjusted mortality rate in large metropolitan areas (>1 000 000 inhabitants) was 664.5/100 000 inhabitants, while rural areas amounted to 834/100 000 inhabitants4. Other studies have shown that the urban–rural gap is independent of gender and age5. Although several studies have been performed, the urban–rural mortality status is inconclusive, especially in developing countries. This is a topic that needs more research.
In Mexico, the number of inhabitants in urban areas has increased considerably from 43% in 1950 to 79% in 20206. These percentages will increase in the future, since it has been estimated that by 2030 much of the population growth in Mexico will be urban, with 83.2% of the national population concentrated in this area7. This dynamic will have a considerable impact on social development, prompting decision-makers to consider, among other aspects, the development of an efficient health system.
The leading causes of mortality in Mexico include cardiovascular diseases, diabetes mellitus, cancer, and accidents, all of which represent 66% of all deaths8,9.
Continuous monitoring of mortality and inequality rates in Mexico, including the gap between urban and rural areas, is necessary to reduce them. Until now, research on urban and rural mortality in Mexico has been scarce. With these considerations, the objective of this study is to describe the adjusted mortality rate in these areas and analyze its trends from 2000 to 2019.
Methods
Data
The analyzed areas have been classified as rural and urban by INEGI (National Institute of Statistics and Geography). This institute differentiates urban and rural residences by the number of inhabitants: a rural residence has fewer than 2500 inhabitants and an urban residence has more than 2500 inhabitants. According to the INEGI, currently, there are 185 243 rural areas and 4189 urban areas in Mexico. The mortality data in urban and rural areas of residence were also obtained from the publicly available INEGI database. All mortality data – cancer (ICD10 COO-D48), cardiovascular disease (ICD10 I00-I99), and external causes, including accidents, suicide, homicide, surgical complications, sequelae of external causes of morbidity and mortality and supplementary factors (ICD10 V01-Y98) – were analyzed from 2002 to 2019. Data on urban and rural populations from 2005, 2010, and 2015 were obtained from the census or population counts reported by the INEGI10-12. The population was estimated by linear interpolation for the rest of the years.
Analysis
Adjusted mortality rates were estimated for urban and rural areas of residence by direct method, using the world standard population and expressed by 100 000 inhabitants. Mortality rates were grouped by gender, age groups (<20, 20–39, 40–59, ≥60 years), and socioeconomic region (SR), which range from 1 to 7 in Mexico. The level of wellness in the region increases as the SR number increases, 7 being the SR with the highest level of wellness. These SRs have been classified by the INEGI by considering the following criteria: infrastructure, housing quality, housing equipment, overcrowding, health, education, and employment. These socioeconomic regions group the 31 federal entities and Mexico City, being made up of the following states: SR1: Chiapas, Guerrero; SR2: Campeche, Hidalgo, Puebla, San Luis Potosí, Tabasco, Veracruz; SR3: Durango, Guanajuato, Michoacán, Tlaxcala, Zacatecas; SR4: Colima, Mexico, Morelos, Nayarit, Querétaro, Quintana Roo, Sinaloa, Yucatan; SR5: Baja California, Baja California Sur, Chihuahua, Sonora, Tamaulipas; SR6: Aguascalientes, Coahuila, Jalisco, Nuevo León; and SR7: Mexico City.
The difference between urban and rural areas was performed by the Student’s t-test. Trend analysis was performed with a logarithmic regression and tested with the Student’s t-test. The annual percentage change (APC) was estimated with the following formula, APC = (em – 1) × 100, where em is the inverse of the natural logarithm of the slope of the logarithm regression rates. A p-value of ≤0.05 was considered statistically significant, and NCSS v12 (NCSS; https://www.ncss.com) was used for the analysis.
Ethics approval
This is a retrospective study that uses public domain data, so the ethical committee approbation was not required.
Results
From 2002 to 2019, the numbers of deaths in the urban and rural areas of Mexico was 7 990 400 and 2 355 111 respectively. In the same period, the estimated population in urban areas increased from 75 250 603 in 2002 to 97 633 305 in 2019, while that in rural areas increased from 24 544 799 in 2002 to 27 084 065 in 2019.
Mortality rate
Overall, residents of urban areas presented higher mortality rates (622.1/100 000 inhabitants) than rural residents (549.5/100 000 inhabitants) – the same pattern was observed for both genders (Table 1). In the case of males, the mortality rates in urban and rural areas were 737.8 and 634.4/100 000 inhabitants respectively, and in the case of females, they were 520.9 and 467.5/100 000 inhabitants respectively. In both areas, males presented the highest mortality rates (Fig1).
All age groups showed the highest mortality rate in urban areas, except for 20–39 years, which showed higher mortality rates in rural areas (165.5/100 000 inhabitants). The age group with individuals ≥60 years presented a higher mortality rate than the rest of the age groups in both areas of residence (urban=3506.9/100 000; rural=2910/100 000) (Fig2).
Concerning the main cause of death, residents of urban areas had higher mortality rates than rural residents for cancer (urban=87.0/100 000; rural=66.6/100 000) and cardiovascular diseases (urban=157.7/100 000; rural=133.9/100 000) (Fig3). For the external causes, there was no significant difference between areas (Table 1). Cardiovascular causes had the highest mortality rates in both areas.
Regarding the SRs of Mexico, the adjusted mortality rate was higher in the urban areas of almost all socioeconomic regions of Mexico, except in SR 7 where mortality was higher in rural areas (Fig4). The SR that presented the highest mortality rate in the urban area was SR 5 (654.5/100 000) while the SR that presented the highest mortality rate in the rural area was SR 2 (404.5/100 000).
Table 1: Trends in adjusted mortality rate by residence, age, gender, and main cause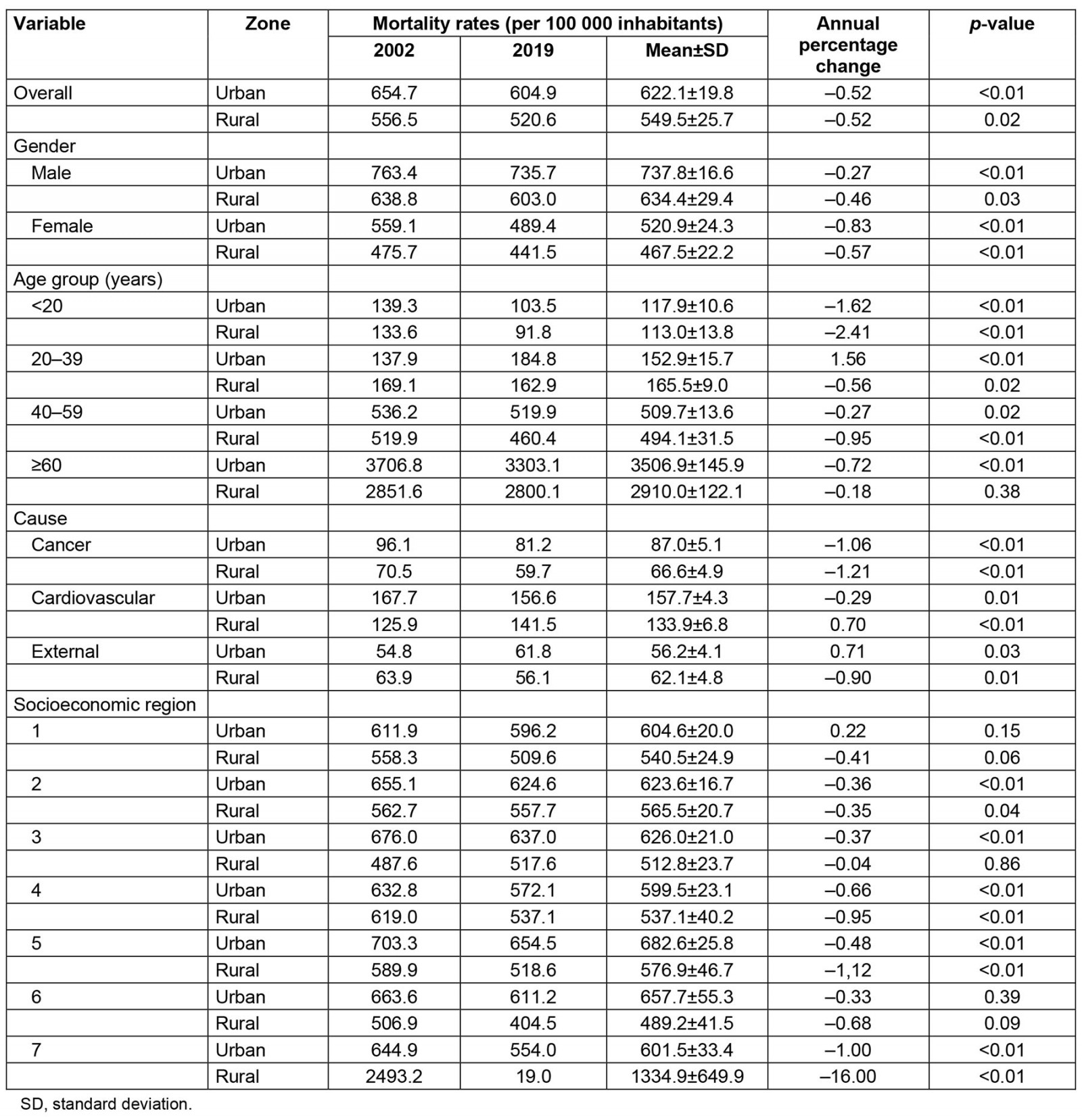
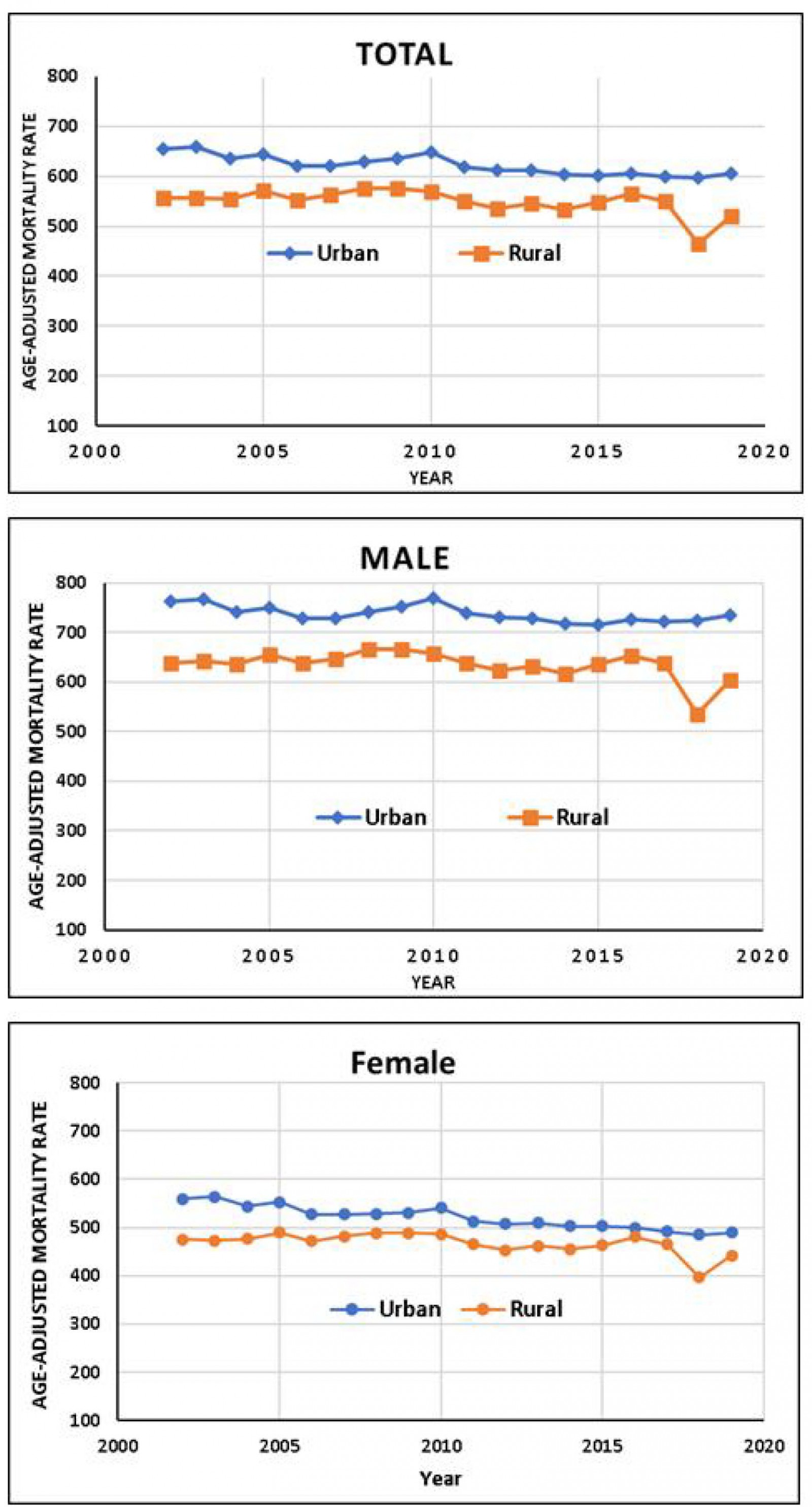 Figure 1: Annual adjusted mortality rate in urban and rural areas of Mexico according to gender (2002–2019).
Figure 1: Annual adjusted mortality rate in urban and rural areas of Mexico according to gender (2002–2019).
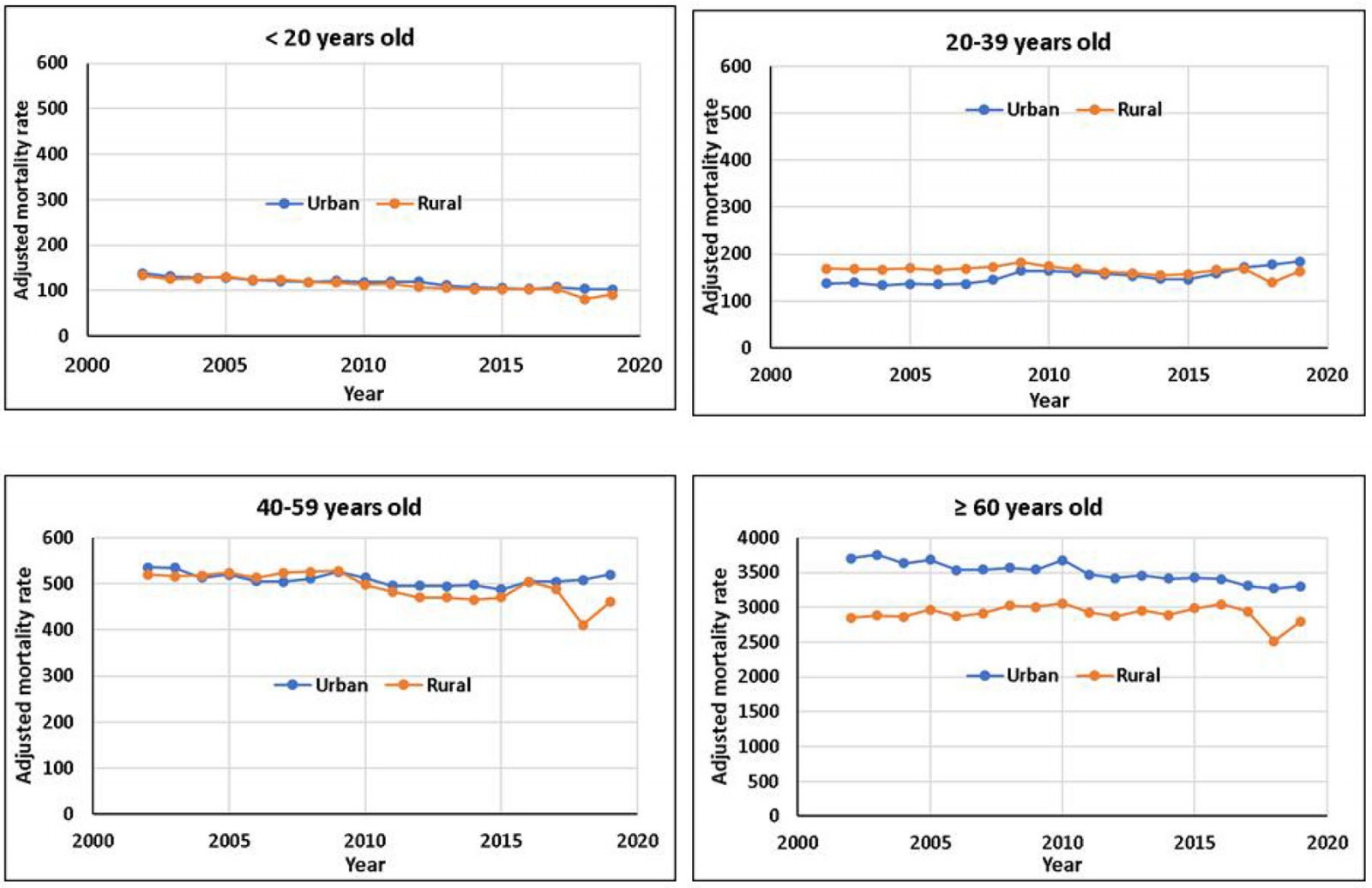 Figure 2: Annual adjusted mortality rate in urban and rural areas of Mexico according to age group (2002–2019).
Figure 2: Annual adjusted mortality rate in urban and rural areas of Mexico according to age group (2002–2019).
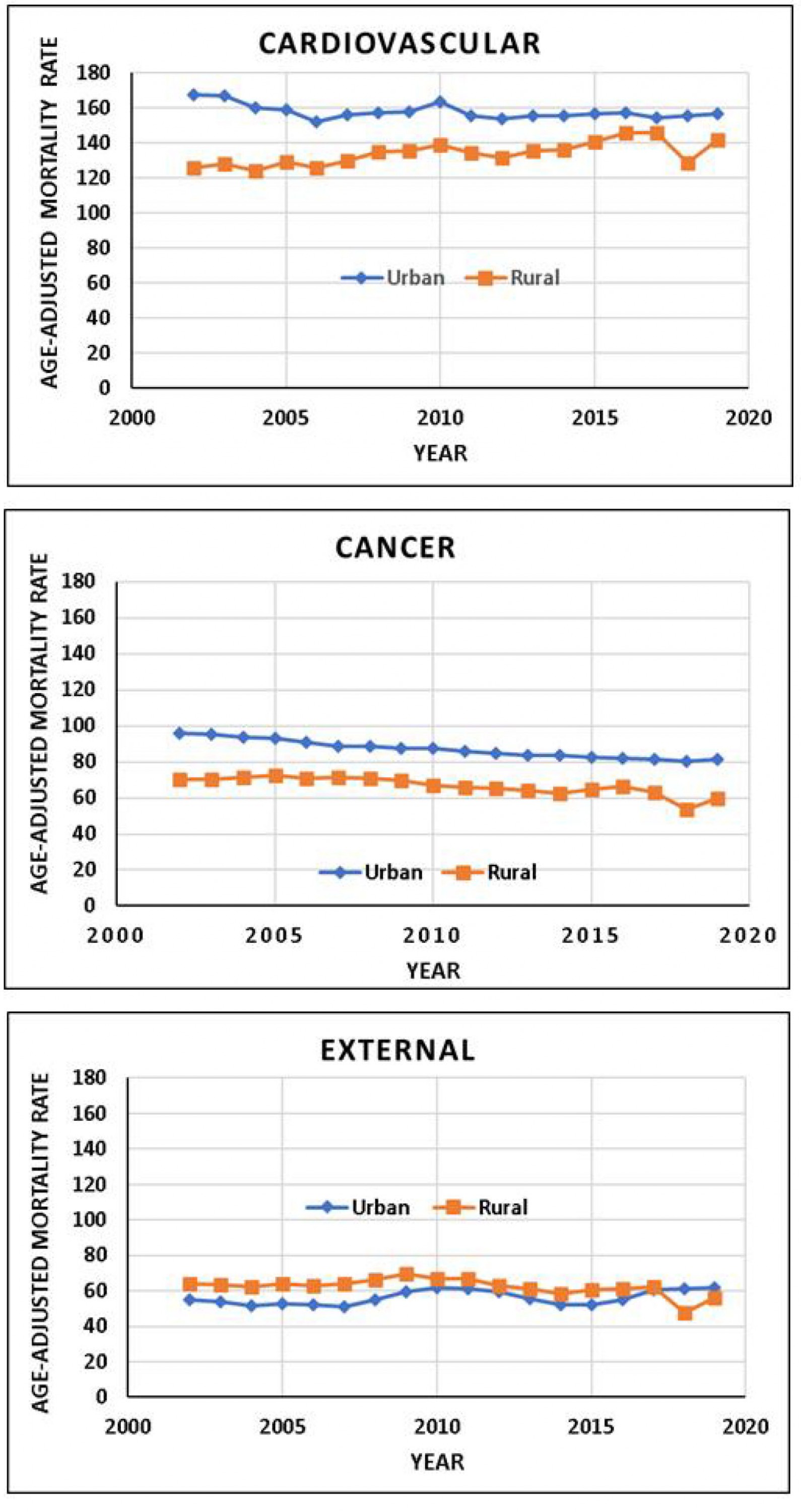 Figure 3: Adjusted mortality rate in urban and rural areas of Mexico according to main cause of death (2002–2019).
Figure 3: Adjusted mortality rate in urban and rural areas of Mexico according to main cause of death (2002–2019).
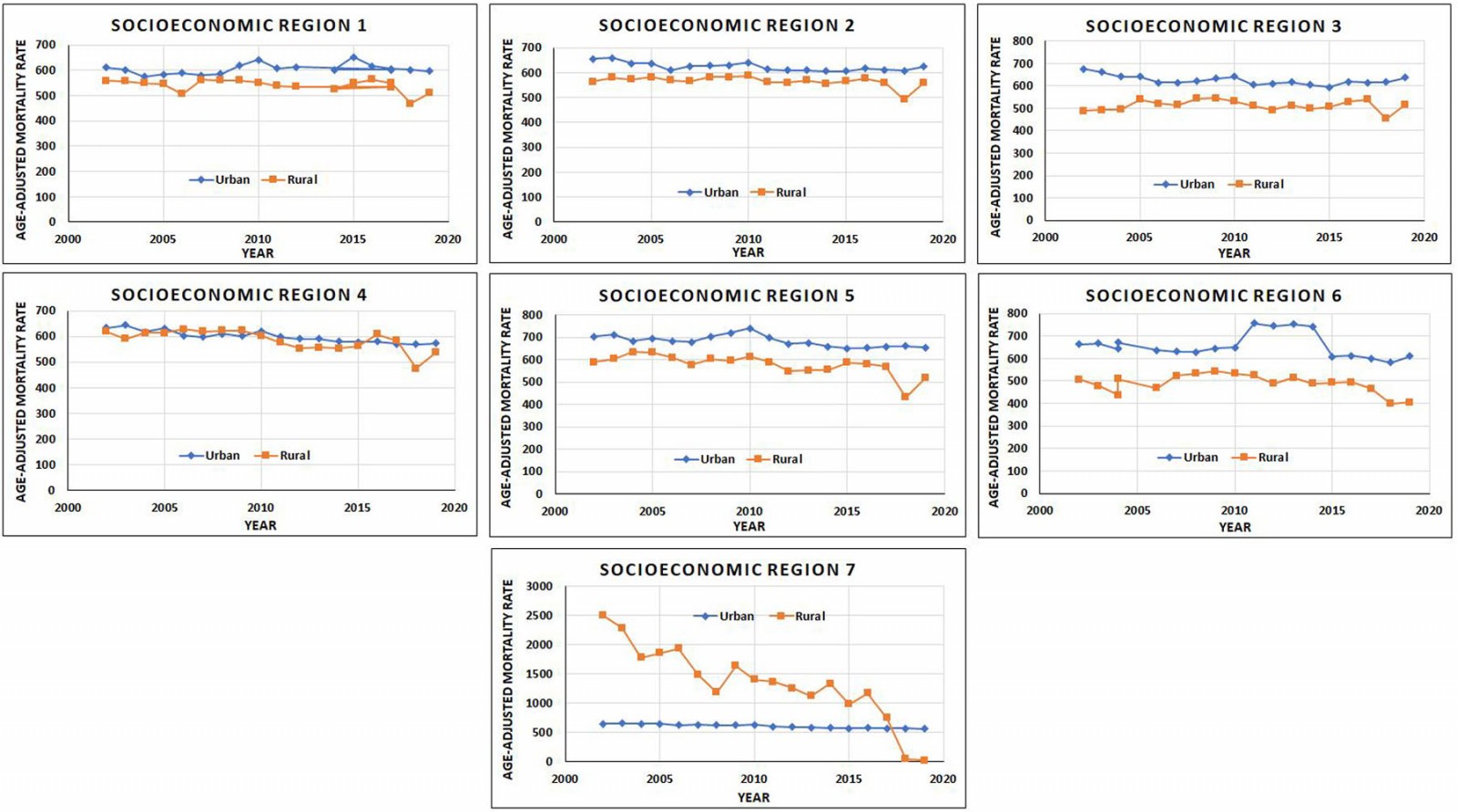 Figure 4: Adjusted mortality rate in urban and rural areas of Mexico according to socioeconomic region (2002–2019).
Figure 4: Adjusted mortality rate in urban and rural areas of Mexico according to socioeconomic region (2002–2019).
Trends
Overall, a significant decrease in the mortality rates was observed in both areas of residence (p<0.05), from 654 to 604.9/100 000 inhabitants for urban residents and from 556.5 to 520.6/100 000 inhabitants for rural residents (Table 1). The APC in both areas of residence was the same, –0.52%. Furthermore, males and females showed a significant decrease in mortality rates in both areas of residence. The higher APC for males was in the rural area (APC= –0.46) while for females, the higher APC was in the urban area (APC= –0.83).
All age groups showed a significant decrease in mortality rates in both areas of residence. The exceptions were the age group 20–39 years in the urban area, which presented a significant increase in mortality rate (APC=1.56), and the age group ≥60 years, which presented no change in the rural area with a non-significant APC. A higher decrease was observed in the group of <20 years in the rural area (APC= –2.41).
According to the main mortality causes, cancer showed a decrease in mortality rates in both areas of residence, the rural area having the highest trend (AP= –1.21). Cardiovascular deaths showed significant increases in the rural area (APC=0.70), while the urban area presented a significant decrease (APC= –0.29). By contrast, external causes showed an increase in mortality in the urban area (APC=0.71) and a decrease in the rural area (APC= –0.90).
Some areas of the SRs of Mexico showed a significant decrease in mortality rates. The SRs that showed a significant decrease in mortality rate in their urban areas were SR2 (APC= –0.36), SR3 (APC= –0.37), SR4 (APC= –0.66), SR5 (APC= –0.48) and SR7 (APC= –1.00). On the other hand, the socioeconomic regions that showed a significant decrease in the mortality rate in their rural areas were SR2 (APC= –0.35), SR4 (APC= –0.95), SR5 (APC= –1.12), and SR7 (APC=16.00) (Table 1).
Discussion
This is the first study that describes world-adjusted mortality rates and their trends in the urban and rural areas of Mexico. Globally, variations in mortality rates between urban and rural areas among different countries are attributed to several factors, including the environment, the individual, and health conditions. On the one hand, it was found that mortality for all causes is higher in urban areas, a result contrary to other studies in countries such as the US (urban=712.9/100 000; rural=847.7/100 000)13, Lithuania14 (urban=1112.1/100 000; rural=1205.8/100 000), and China (30% higher in rural area)15, where mortality is higher in rural areas. On the other hand, mortality rates in Ireland2, England, and Wales (35–54% higher in urban areas)16 are greater in urban areas. The authors of the studies where rural mortality is higher than in urban areas concluded that this gap has been persistent in the last years, and more programs and resources should be allocated to reduce it.
Contrary to other reports, mortality rates in urban and rural areas of Mexico were not affected by age; urban areas showed the highest mortality rate in all the analyzed age groups. The major gap between urban and rural areas was observed in older individuals. This pattern has been observed in Germany, England, and Wales, where a transition from urban to rural mortality has been observed in individuals aged 80 years and older (relative mortality >5% in rural areas). The authors attribute this transition to different capabilities among the different areas to respond to arising health issues across older ages17.
Concerning the main cause of death, mortality is variable among countries: in this study, cancer and cardiovascular disease mortality was higher in urban areas. This result is different from the one reported in China (44% more likely to die in rural areas)18 and the US (rural=164.1/100 000; urban=142.8/100 000)19, but similar to that in South Korea20. In Lithuania, no significant differences were reported in urban and rural areas in 2018 for cancer as a cause of death14. In the case of external causes, mortality was higher in rural areas; these results are similar to those reported in Lithuania where males presented higher mortality in rural areas (rural=152.0/100 000; urban=114.4/100 000).
While SR5 and SR6 presented the highest mortality rate in the urban areas, the causes are not clear; most of the states that form these regions are characterized by industrial activity, they are in the north of the country, and they have a desert climate. Curiously. SR7, which has a major level of wellness, presented a higher mortality rate in the rural than in the urban area. This has only been observed at the country level, where developed countries – those with a higher level of wellbeing – have a higher mortality rate in rural areas than in urban areas. SR7 is the capital of Mexico and is characterized, in addition to a higher level of wellness, by high levels of pollution and high population density (6163 inhabitants/km2).
Mortality differences between urban and rural areas have been described with contradictory results. In some countries, mortality is higher in urban areas, while in others, it is higher in rural areas. Several causes contribute to this discrepancy, including the sociodemographic characteristics of the country’s inhabitants, a healthy or an unhealthy environment, and the definition of precise borders of urban and rural areas.
Overall, different mortality rates result from the sum of various factors, acting for or against: in the case of access to health services, rural residents often encounter barriers that limit their ability to obtain the care they need21. Another factor is environmental pollution, which is frequently expected to be higher in urban areas, due to the high population rate and anthropogenic activities. Some cases, however, show contrary trends, as seen in a study carried out in China between 2006 and 2015, where high levels of air pollution with PM2.5 particles were found in rural areas, due to the use of coal stoves, which was associated with a high mortality rate from lung cancer22.
Although more studies are needed, we think that higher mortality in Mexico’s urban areas could be partly explained by migration from rural to urban areas. These migrants tend to gradually adopt lifestyles that are prejudicial to health, such as those where there is lack of physical activity, alcohol and tobacco consumption, and a diet rich in sugar and fat, all of which are risk factors for cardiovascular disease. In addition, some migrants could settle in informal districts that are poorly attended by public services, with deficient sanitization, drinking water, and limited infrastructure.
Both urban and rural areas showed a significant decrease in mortality rates, independent of gender and age. Like the gap in urban and rural mortality, this decrease could be due to multiple factors: in rural areas, this decrease could be due to an increase in connectivity between urban and rural areas, which facilitates the access to hospitals or health centers when needed. Data from the Consejo Nacional de Evaluación de la Política de Desarrollo Social (CONEVAL) (National Council for the Evaluation of Social Development Policy) in showed that rural areas increased their access to road traffic from 2010 to 202023. Another factor that could contribute to this decrease is the increase of individuals covered by public health programs. According to the population census reported by INEGI, the affiliation to some health services mainly, IMSS (Instituto Mexicano del Seguro Social/Mexican Social Security Institute) and ISSTE (Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado/Institute of Security and Social Services of State Workers) by Mexicans increased from 40.8% in 2000 to 73.5% in 202011,12. Concerning the decrease in mortality rates in urban areas, this could also be due to an increase of individuals associated to Mexican public health services.
Finally, the limitations of this study include the lack of mortality data based on subclassifications among rural and urban areas; for example, rural remote and large megacities. Another limitation is the lack of data based on ethnicity; in Mexico there are more than 65 Indigenous ethnic groups (9.4% of the population), with traditions and customs that may have an impact on their health. Another potential limitation is a possible error in the data register – this could explain the sudden mortality decrease in 2018.
Conclusion
In Mexico, there is variation in mortality between urban and rural areas, urban areas having higher adjusted mortality rates. The gap is independent of age and cause of death. Mortality in both areas significantly decreased during the study period.
Funding
No funding was received for this research.
Conflict of interest
The authors declare no conflicts of interest.
References
You might also be interested in:
2012 - Physician in practice clinic: educating GPs in endocrinology through specialist-outreach
2010 - Prevalence, awareness, treatment and control of hypertension in an elderly population in Greece
