In the spirit of reconciliation, the writers acknowledge the Traditional Custodians of Country throughout Australia and their connections to land, sea, waterways, and community. We pay our respect to their Elders past and present and extend that respect to all Aboriginal and Torres Strait Islander peoples today.
Introduction
This scoping review was undertaken to obtain conceptual clarification about how racism and cultural safety are understood by interdisciplinary health professionals in the aged care sector in regional, rural and remote areas. The gaps in the literature identified in this review will be used to inform future research that examines cultural safety in the aged care sector in the Australian context1. The structure of the review was guided by Page et al2, Arksey and O’Malley3 and Aromataris and Munn4.
Racism can be described as the maintenance or exacerbation of inequality among ethno-racial groups based on a belief in superiority of certain races over another and the ‘expression of such prejudice’5. This definition incorporates three facets of racism: individual ideologies (internalised racism), interactions between persons (interpersonal racism), and the structure of society (systemic racism) as concepts that are concomitant in practice5. Institutional racism, with entrenched political, economic, social and cultural systems, can include the neglect by organisations to provide a professional service of acceptable quality to consumers due to their cultural or ethnic origin6. The idea of power vested in the dominant societal group is linked to colonialism and British utilitarian philosophers such as John Stuart Mill7. Mill asserted that societal cohesion would fail when members of that society comprise those from different faiths and cultures. Utilitarianism in a colonial context extended to assimilation or the subjugation of the conquered people, where every aspect of their lives was controlled by government7,8. Countries where settler colonisation occurred also used racial science and racial superiority to justify the dominance of Anglo-Celtic ethnicities. Structures and institutions created during and after settler colonisation are tied to racial forms of exclusion whereby First Peoples and other racial minorities are constructed as ‘different’7.
In Australia, racism is a factor impacting significantly on the health of First Peoples and other racialised minorities and must be addressed as a component of health inequity9,10. Internationally, racism, historical and present trauma, and settler colonialism are catalysts for ‘compromised individual well-being and degraded physiological processes’ in a landscape of community and family dysfunction11. Institutional racism in Australian health care can be addressed by acknowledging First Peoples’ sovereignty ‘over all aspects of their land, lives, and futures’12. This means recognising that First Peoples’ ways of knowing about health and wellbeing are different from non-First Peoples’ perspectives, and that this lack of knowledge and understanding about different worldviews manifestly affects the way First Peoples are treated within the Australian health system, both as individuals and in service provision for entire communities13. Cultural safety, according to Cox and Best14, connects ‘interpersonal and institutional racism’ and is a necessity to improve the experience of First Peoples’ engagement with health professionals and health systems.
This scoping review uses the definition of culturally safe practice from the Australian Health Practitioner Regulatory Authority15: the ‘ongoing critical reflection of health practitioner knowledge, skills, attitudes, practising behaviours and power differentials in delivering safe, accessible and responsive healthcare free of racism’. In her study conducted in New Zealand, Ramsden16 asserted that the need for cultural safety also extended to those who experienced discrimination due to ‘socioeconomic status, age, gender, sexual orientation, ethnic origin, migrant refugee status, religious belief or disability’.
The health impacts of racism are well documented in the lower life expectancy, burden of disease and elevated levels of psychological distress experienced by First Peoples17. Despite the importance of cultural safety for mitigating racism, little is understood about how health professionals understand racism in the context of providing culturally safe care. There is evidence to suggest that the ability of health professionals to integrate cultural safety into their practice is intrinsic to dismantling racism and to improving the health of First Peoples and other marginalised groups18-20. Utilising international research, this scoping review aims to, in the context of regional, rural and remote areas:
- explore how interdisciplinary health professionals in the aged care sector understand and respond to racism
- investigate how interdisciplinary health professionals in the aged care sector understand and provide culturally safe care.
The term ‘First Peoples’ is respectfully used to refer to Aboriginal and Torres Strait Islander Peoples of Australia, and Indigenous Peoples of Norway and North America.
Methods
A preliminary search of PROSPERO, MEDLINE, the Cochrane Database of Systematic Reviews, and JBI Evidence Synthesis was conducted and no current or in-progress scoping reviews or systematic reviews on the topic were identified.
This review consisted of Australian and international literature published in English, including published primary studies; systematic, integrative and narrative reviews; meta-analyses; theses; policy documents; guidelines; position statements; and government literature. Literature published from 1990 onwards was included, reflecting the commencement of discourse on cultural safety in academia20.
An initial limited search of MEDLINE (Ovid) as well as CINAHL (EBSCO) was undertaken to identify articles on the topic. The text words in the titles and abstracts of relevant articles, and the index terms used to describe the articles, were used to develop a full search strategy. A research librarian provided guidance on the development of a strategy to optimise search results, including advising on the creation of appropriate search strings, which were trialled and refined by the research librarian and first author prior to use. The full search strategy for Scopus is included in Table 1. Ovid (MEDLINE), CINAHL Plus with Full Text, Scopus, Proquest Nursing and Allied Health Database, and Informit were utilised in the full search. The most recent search of all databases was undertaken on 9 May 2022.
All identified records (386) were collated and uploaded into EndNote v20, and duplicates (10) were removed, leaving 376 papers. The articles were then imported into JBI System for the Unified Management, Assessment, and Review of Information21. A pilot test followed, with three reviewers undertaking title and abstract screening of 25 articles against inclusion and exclusion criteria. The primary author (reviewer 1) then undertook the title and abstract screening, and the results were reviewed at a team meeting. The primary author undertook full-text screening. Included and excluded articles following full-text screening were again reviewed at a team meeting with all reviewers. Divergent viewpoints on the relevance of articles at all stages were resolved through team discussion, collaboration and close adherence to the scoping review inclusion and exclusion criteria. Articles for full-text screening were exported into Microsoft Excel.
Title and abstract screening and full-text screening were performed by three reviewers on 376 papers, and 234 papers were excluded. Full-text screening was performed on 142 papers. The reason for exclusion of 132 papers during full-text screening was duplicated papers (n=10), article content not addressing review aims (n=19), a focus on acute care settings (n=7), a focus on urban settings (n=6), ineligible context (n=15), and ineligible phenomena of interest (n=75). Figure 1 shows the screening process in flowchart form.
Data were extracted from full-text papers included in the scoping review by using a data extraction tool developed by the reviewers informed by Peters et al22. Headings included:
- first author, year and country
- type of paper
- methodology
- geographical location
- study aims/purpose
- study population
- key concepts informing results and discussion.
The development of this tool was iterative as features of the included studies became apparent and additional columns needed to be added. The final extraction tool was reviewed and agreed on at a team meeting. The storage and management of data occurred in a Microsoft Excel workbook. The data in the Excel workbook included authors, year of publication, location where the study took place, study population, study aims/purpose, methodology and key concepts informing results and discussion22. There was no need to contact authors to request missing or additional data. A title and abstract search of the reference lists of papers included in the review identified no additional papers. Any lack of concordance between reviewers during the review process was resolved through collegial discussion.
Table 1: Full search strategy for Scopus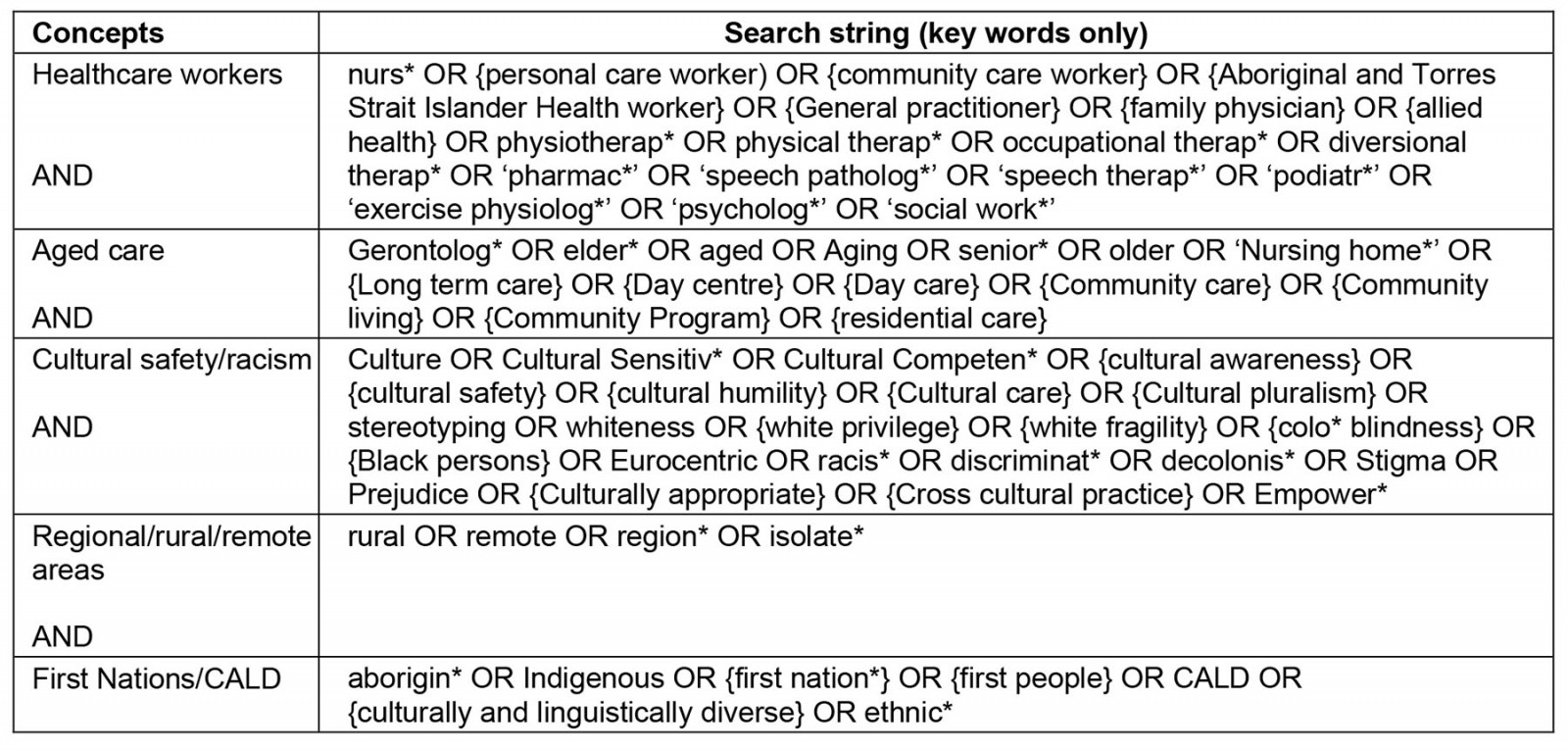
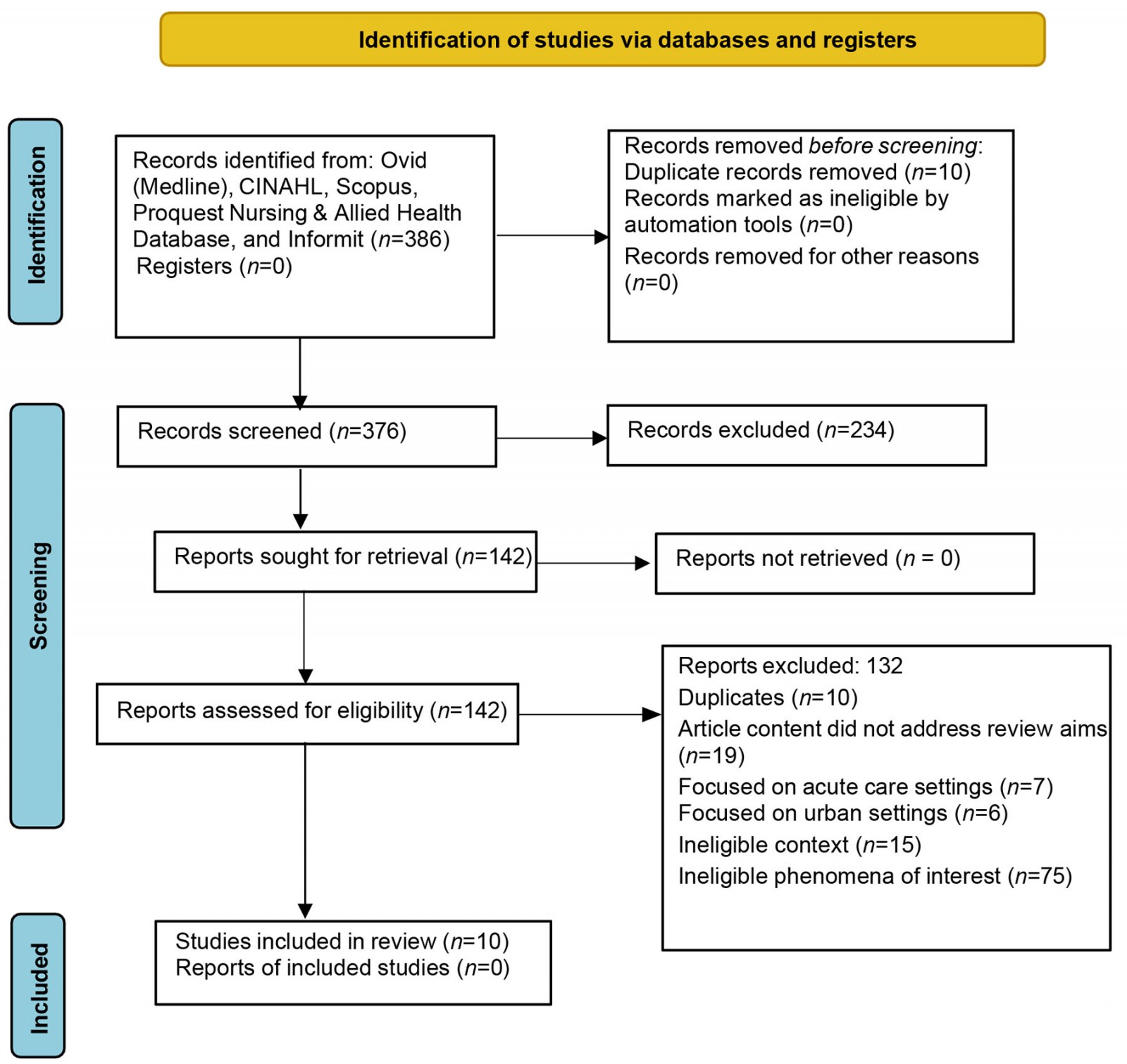 Figure 1: Search results and study selection and inclusion process.
Figure 1: Search results and study selection and inclusion process.
Ethics approval
Ethics approval was not required for this scoping review because it used publicly accessible documents and did not collect information of a personal, sensitive or confidential nature from participants.
Results
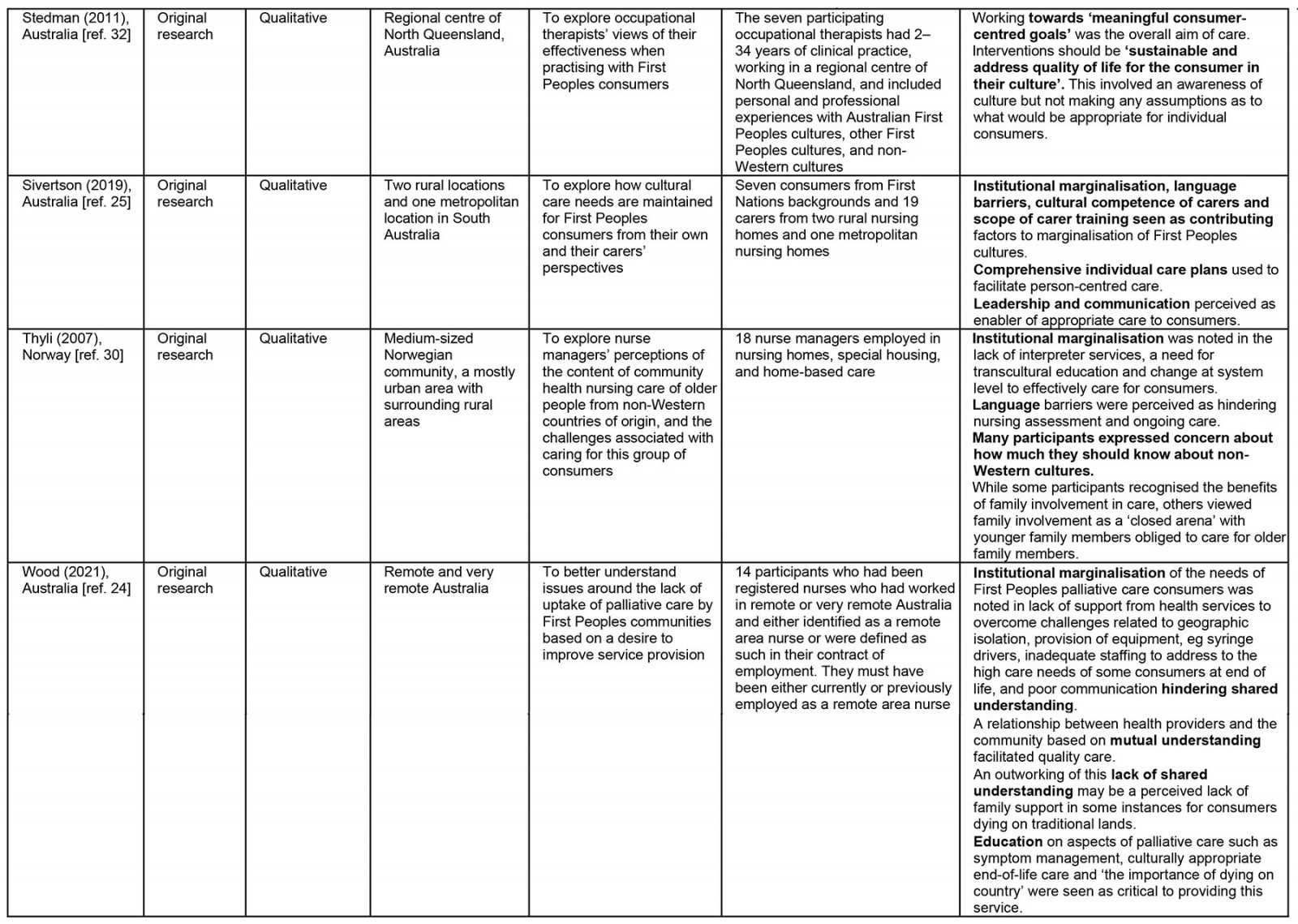
Ten papers were included in the review. The included papers were based on work undertaken in Australia23-26, Canada27, the US28-30, Norway31 and England32. The papers focused on residential and community-based aged care services in regional, rural and remote areas. All papers included perspectives of how cultural safety and racism are understood by nurses and other healthcare workers.
Qualitative research studies comprised seven papers22-26,29,31. Of the remaining three papers, one utilised a mixed-methods approach32, one was a program evaluation28, and one was a narrative discourse30. The qualitative papers collected data through open-ended interviews and participant observation (n=1), focus groups (n=1), telephone interviews (n=1), semistructured interviews (n=2), and structured and open-ended questionnaires (n=2). The mixed-methods study (n=1) used a postal survey followed by telephone interviews.
Sample sizes of participants were small, ranging from seven to 37 participants, as is appropriate for qualitative inquiry. A broad range of perspectives were present in the included papers, including of consumers, carers, family members and various health disciplines. Participants came from a variety of cultural backgrounds; however, the experience of First Peoples dominated the papers included in the scoping review.
Three papers described research undertaken in more than one type of geographical location25,31,32. For example, Sivertsen et al25 interviewed consumers from two rural nursing homes and one metropolitan nursing home. Four papers reported on research focusing on palliative care services23,24,28,29 delivered in rural and remote environments, and one paper reported on occupational therapy services in a regional community26. The decision to include these papers was made following team discussion after considering the relevance of each paper to the scoping review objectives. The results of the review, including the main findings, are presented in Table 2.
Table 2: Characteristics of the included articles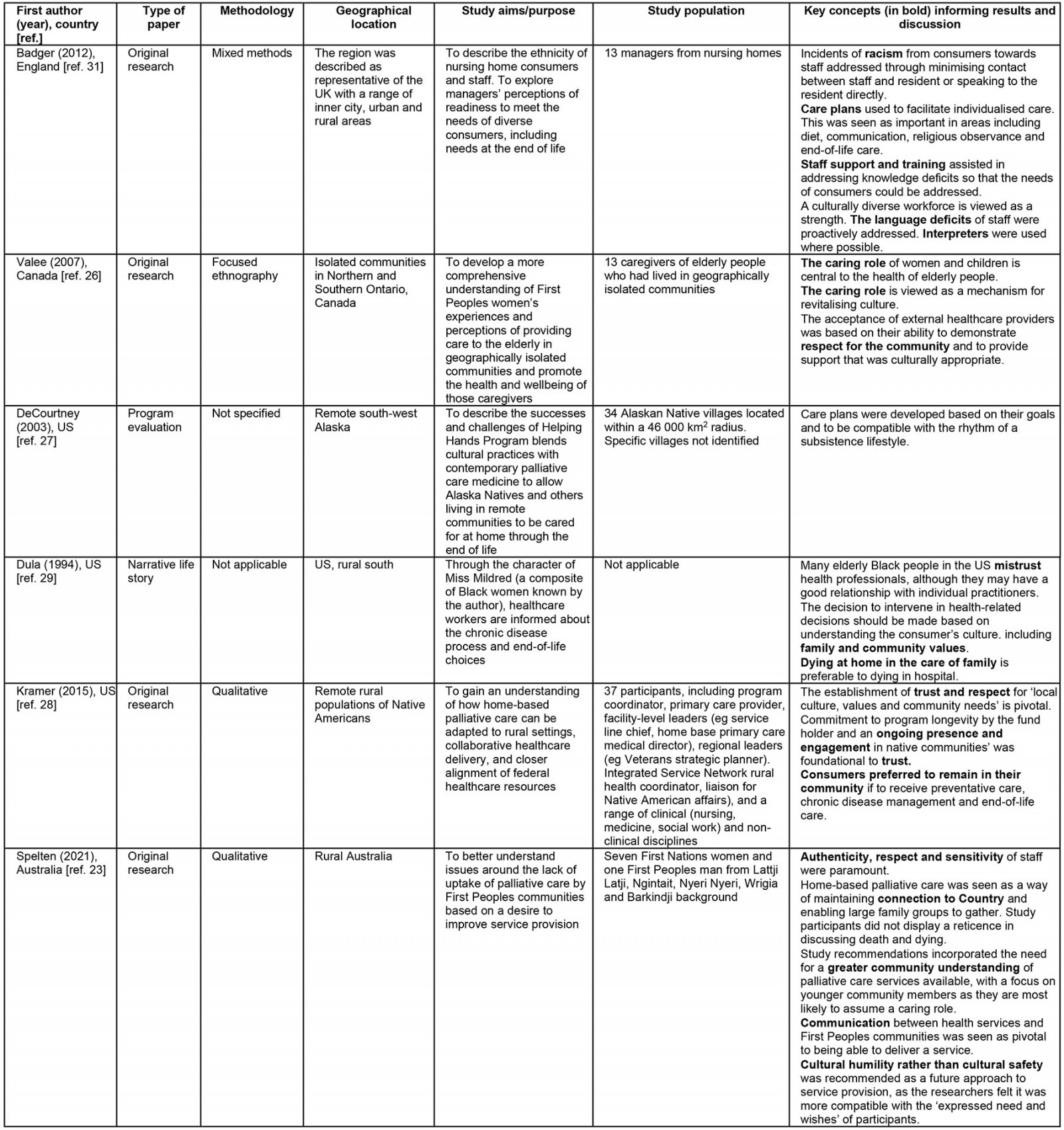
Synthesis of results
Table 2 presents key concepts or themes from the chosen articles as they pertain to the two aims of the scoping review, as well as new insights on relevant topics associated with racism and cultural safety. The first author constructed these themes by reading the included studies numerous times and highlighting relevant information. Once an adequate understanding of the papers was obtained, information was organised in a spreadsheet, colour coded by concept or topic area and reviewed by the authors. The spreadsheet themes are summarised in Table 2. The information from this table informs the results and discussion sections of this article2.
Five themes were distilled from the articles. These are the language of racism in aged care, the evolving use of terminology around cultural safety, the use of care planning to support the cultural needs of consumers, and cultural safety in end-of-life care. One further theme was identified that spanned both racism and cultural safety, that effective communication is pivotal for staff–consumer rapport.
Language of racism in aged care
Badger et al32, in a paper from England, was the only paper to use the word ‘racism’. Racism was used to describe the behaviour of consumers and/or family towards ‘black’ or ‘overseas trained staff’ employed in residential aged care facilities, a feature that also distinguishes it from other papers included in the review. Two options for addressing these incidents were reported. Either the staff member was not allocated to that resident, or the lack of option of allocating a ‘white’ staff member was explained to the resident. One manager noted that racist behaviour in elderly people was common32.
These incidents were, however, viewed as infrequent, and relationships improved once a rapport was built between the staff member and the resident. A direct approach where the views of the resident were challenged was not described; rather, an approach where you ‘work around it’ was employed32. This involved ‘having a word with the resident’ and saying ‘well it’s either that [being cared for by a Black or overseas staff member] or nobody’ (p. 1731).
Sivertsen et al25, in a paper from Australia, were cautious in their use of language, identifying institutional marginalisation rather than racism5, a lack of cultural competency among carers and poor scope of education as barriers to cultural safety. Institutional marginalisation was described by Sivertsen et al25 as a lack or an absence of emphasis on First Peoples cultures in daily activities in an aged care setting.
This created a perception among First Peoples staff and carers of ‘invisibility’ (p. 8) to facility management and leadership25. Wood et al24 described what may amount to institutional racism differently from Sivertsen et al25, citing a lack of equipment and a lack of capacity to access equipment such as infusion pumps and fridges to store deceased persons as primary concerns in delivering end-of-life care in First Peoples communities in remote Australia5.
While the words ‘racism’ or ‘racist’ were not used to describe these activities, Dula30, in a US context, described ‘colored folks not getting the same care that white folks get’, highlighting that issues of ‘whiteness’ are readily identified by those who are marginalised by cultural norms in health care. Issues of trust between White health professionals and African Americans are based on a history of slavery and ongoing systemic racism. Lack of trust has impeded the development of rapport and effective communication between White health professionals and African American consumers30.
Evolving use of terminology around cultural safety
Cultural safety was referred to by three Australian studies included in the review. In these studies, cultural safety was referred to in the context of the needs of consumers, and the provision of care. Stedman and Thomas26 and Spelten et al23 recognised an evolution in terms from ‘cultural safety’ to ‘cultural humility’. Cultural humility acknowledges that understanding another culture completely is not attainable, but the focus should be on ‘self-awareness, reflection, support and the reparation of power imbalances between health professionals and consumers and their families’33. Other terms indicate a multiplicity of cultural care models such as cultural awareness24, cultural competency26, cultural sensitivity27,32, cultural appropriateness26 and transcultural care31. Numerous papers employed multiple terms. Extant literature may make it confusing for practitioners to derive a consistent understanding of cultural safety.
An Australian paper by Sivertsen et al25 spoke of lack of cultural competency; however, other papers framed this concept differently. For example, training of staff was recognised as important to provide a solid awareness of diverse cultural and religious needs32. Wood et al24, also in an Australian context, attested that cultural awareness education was necessary to provide appropriate end-of-life care. In a paper from Norway, Thyli et al31 identified ‘deficiencies in multicultural competency’ (p. 48) as an issue for study participants. Nurses expressed concern at how much extra knowledge was required to care for people from non-dominant cultural backgrounds and advocated implementation of appropriate training. However, organisational issues were identified, including a lack of financial and human resources. Managers were viewed as not being cognisant of the complexities and challenges of caring for people from diverse cultural backgrounds.
Care plans were viewed as crucial to facilitating individualised care, including the cultural needs of consumers in residential aged care environments. Care plans contained information on diet, religion, specific cultural practices such as observance of personal care regimes, and end-of-life care. In England, Badger et al32 provided the example of assisting African Caribbean consumers to follow culturally appropriate skincare regimes. In programs based in the community, individualised care plans aim to support consumers’ goals and the community’s lifestyle. In villages serviced by the Bristol Bay Area Health Corporation in Alaska (US), hunting, fishing and food gathering are vital components of a seasonally based subsistence lifestyle. Care plans were developed to account for the movement of communities to different locations28. For care plans to be effective, they should be available to all staff, including nurses and aged care workers involved in the care of the patient28. Reluctance to discuss cultural matters due to the confidential nature of topics and a fatigue experienced by First Peoples in explaining cultural matters was perceived as a barrier to providing person-centred care28.
Occupational therapists collaborating with a diverse consumer base in a range of organisations in North Queensland in Australia did not describe using care plans; they did, however, emphasise setting consumer-centred goals that aim to maximise quality of life in the context of the consumer’s culture26.
Cultural safety in end-of-life care
Several studies in different countries highlighted a preference for First Peoples remaining within their community and being cared for by family when ill or approaching end of life23,24,27,28,31. Most often, women assumed the role of carers. In Ontario, Canada, the Circle of Caring, for example, describes the interplay between healers chosen by the elderly person to care for them during ill health and the cultural values that they enact in their role. A critical component of a healer is to pass on traditions associated with the caring role27.
The extended family provides practical, emotional and financial support to the healer(s). The women interviewed in this study expressed that the value of the caring role survived the suppression of cultural practices and the fracturing of families and communities as children were sent to ‘residential school’27. Outside the inner circles of caring occupied by healers, family and the First Peoples community, the outer circle is occupied by the non-First Peoples community. This outer circle includes healthcare workers who provide support. The metaphor of a ‘door’ opening describes accepting people from the non-First Peoples community, such as healthcare providers, and services into the Circle. This acceptance was primarily dependent on the respect shown for the collectivist values of the First Peoples community and the capacity to provide culturally appropriate support, such as the integration of traditional and contemporary healing methods27. Sometimes, the door would be opened due to necessity rather than choice, but it could also be closed if the person showed a lack of respect for the Circle of Caring and attempted to impose their own values. Respect encapsulated equality, sincerity, patience and understanding towards the women within the Circle27.
A paper by DeCourtney et al28 discussed the establishment of a culturally sensitive palliative care program in remote Alaskan communities. The program was established specifically for ‘Alaska Natives’28. The paper detailed the trauma experienced by members of the focus groups interviewed in their study regarding not being able to provide culturally safe end-of-life care to loved ones28. Some elderly participants recalled not being able to care for or be present for the deaths of loved ones while children and adolescents, as they were at boarding schools28. Other participants acknowledged they felt ‘ashamed’ at ‘outsiders’ looking after them28. Some reported confusion about why their grandchildren, who had received formal training as personal care attendants, were paid to care for them28. Adolescents were also able to volunteer to provide support to terminally ill elders. Each volunteer, or ‘peer helper’, was given a journal to record traditional knowledge and experiences imparted by the elder during conversations with the volunteer. The information collected in these journals was viewed as a significant cultural contribution to the community and a way of linking to traditional ways of living and being28.
In Australia, home-based palliative care services explored by Spelten et al23 were perceived as a way of family attaining assistance with personal care and pain management. This meant that the carers could focus on the cultural and spiritual needs of their family member and relationships with family and community. Remote area nurses asserted in Wood et al24 that a lack of family support and guidance could be a barrier to providing palliative care ‘on Country’. The reasons for this perceived lack of support were not provided in detail, but family dynamics were mentioned as a reason.
As in studies conducted in Canada and Australia, Thyli et al31 recognised the role of family in caring for elderly people at home in Norway. Some participants described families as ‘closed arenas’ (p. 48). The meaning of this term was not explained. Nurses noted a tension between the traditional role of young women remaining at home as carers and the different expectations of their adopted country (Norway) regarding education and workforce participation. There was a feeling that these circumstances would cause increasing alienation, isolation and loneliness for older generations cared for at home. Nurses were also concerned about potential ‘health problems’ for carers. The exact nature of the health problems spoken of were not clarified further, but a link was made to the patriarchal nature of some non-Western cultures compared to the equality and autonomous nature of Norwegian society31.
To rebuild relationships, healthcare providers must embrace providing culturally safe health care as defined by each community in the context of continuing provider presence and engagement; for example, facilitating care where possible for older people with chronic illness and/or who require palliative care who live in their own community on traditional lands23,24,27,28.
Effective communication builds staff–consumer rapport
Four papers emphasised that relationships between healthcare professionals and those receiving care, and their families and communities, should be underpinned by values such as trust, authenticity, respect and sensitivity24,28,29,31. Displaying these values was particularly important according to Kramer et al29, considering the historical participation of North American health providers and other government organisations in activities that discriminated against and marginalised First Peoples. From the healthcare provider perspective, ‘stigma’ and ‘suspicion’ need to be overcome to build effective relationships with First Peoples29. The benefit of effective relationships, according to a research participant, ‘you can’t put a price on, that relationship, because now their kids, you know, and their grandkids will have a different opinion of the VA [Veterans Affairs] and the government’ (p. 8)29.
Thyli et al31 in Norway reported that an absence of professional interpreters negatively impacts the assessment process for new consumers. This absence was attributed to a lack of understanding of the process of booking an interpreter, and a view that senior management rather than frontline clinical staff should be organising interpreters31. The inability for nurses and consumers to communicate continued to create impediments to the provision of care and negatively impacted the psychological wellbeing of consumers31. Family members of consumers from the African continent, Asia, Eastern Europe and the Middle East were relied on to convey the needs of the consumers. In some circumstances, if consumers attended an appointment at the community health centre, staff from areas such as administration and catering were used as interpreters31.
As a contrast, Badger et al in England reported a proactive attitude by many managers towards resolving language and communication problems32. A diverse workforce was viewed as a strength by many managers once the initial difficulties were overcome. A team approach was employed with staff interpreting for new employees until their English skills improved. This enabled new employees to attend training sessions and develop relationships with colleagues and consumers32. One manager observed that while inexperienced staff refined their spoken English skills, they become more observant of changes in resident behaviour and honed non-verbal communication skills. Other facilities required staff to have an English Language Teaching System score of 7.5 or 8.0 before commencement of employment32. Badger et al32 also observed from interviews that families were perceived as crucial in establishing communication mechanisms between consumers and staff, with resources such as cards with words and phrases in the consumer’s language and English made by family. Staff were also used as interpreters when interpreting services were not available at a facility32.
Language barriers between nurses and consumers created difficulties in forming a ‘connection’ according to an Australian paper by Sivertsen et al25. A negative impact on the quality of care and a deficit in the cultural safety of consumers was also reported, particularly when the English language skills of the carer and resident were not strong and there was a lack of First Peoples employed at the facility with competency in the resident’s language25.
Rather than describing communication between consumers and nurses, Wood et al24 emphasised that communication between health services, staff, the consumer’s family, and the community are enablers of quality care provision in parts of remote or very remote Australia. The liaison role of cultural brokers was seen as essential in ensuring mutual understanding between all stakeholders involved in the care of the consumer. Wood et al24 concluded that if the relationship with health services and staff was positive, then community members were more likely to ask for and accept assistance when offered.
Discussion
The literature reviewed suggests that health professionals in the aged care sector in regional, rural and remote areas do not use the language of race and racism and may use alternative terms. This may be explained first by a lack of understanding of concepts such as implicit bias and institutional racism. Second, there may be a reluctance or discomfort by health professionals in applying these terms to colleagues in their own or other professional groups. There is a lack of clarity on how cultural safety is understood; however, individual care plans that include cultural needs are viewed as instrumental in providing high-quality care to the consumer. Consumers also indicated a preference for end-of-life care on Country with their family and community. Effective communication based on values such as respect and trust are vital for building relationships between consumers, families, communities and individual health professionals and organisations.
A question of terms
The literature featured alternative terms such as ‘institutional marginalisation’ to describe racism25. An unwillingness to use ‘racism’ and ‘racist’ results in lack of reform to address personal and institutional racism in aged care contexts. Johnstone and Kanitsaki34 note euphemisms that disguise ‘cultural racism’ in health such as ‘cultural barriers’, ‘language barriers’, ‘cultural insensitivity’ and ‘cultural miscommunication’. Cultural racism focuses not on ‘skin colour’ but on language, religion and norms and customs34. Concepts of ‘otherness’ and an ‘us/them’ discourse are still employed and have impacted older immigrant Australians from non-English-speaking backgrounds34.
Implicit bias may be a factor in health professionals working in aged care using alternative terms rather than labelling behaviour as racism or racist. Implicit bias comprises unconscious thoughts and feelings that are therefore difficult to acknowledge and address. These thoughts and feelings may evolve over time into intractable views never subject to self-critique or critique by others35. In a Western context, reframing implicit bias as an issue of ‘Whiteness’ provides additional insights. Whiteness is a system of power relations grounded in racism where those categorised as White are privileged over non-White people33. In attempting to neutralise Whiteness as an issue, racial colour-blindness claims not to see race when interacting with others8. Racial colour-blindness enables implicit bias to be unexplored and individual and interpersonal racism to be unchallenged. In a health context, this means that the individual needs of the patient can be disregarded, including the need to provide culturally safe care as defined by the consumer and their family. This approach also ignores the depth and breadth of the problem of Whiteness being an ontology and epistemology established as the societal norm7 and therefore the foundations on which systems such as health are constructed.
Structural and institutional racism
The literature contained examples of structural racism impeding access to information and the development of mutual understanding between consumers and health professionals35. An example is the absence of approved interpreters and translators in health organisations at no cost31. In the Australian healthcare system, institutional racism, according to Phan36, can manifest as suboptimal levels of ‘culturally appropriate practice and ignorance of First Peoples concepts of health and wellbeing’ by staff and management. This arguably reflects the linguistic homogeneity that is a component of Mill’s colonialism where the English language is the cultural norm7. Apart from fomenting culturally unsafe environments, communication barriers can result in increasing social isolation and mental illness34. In Australia, Strickland37, in the context of an apology to ‘Aboriginal and Torres Strait islander peoples’ for past harms and injustices, highlighted that professional racism embedded in the practice of individual nurses and midwives, and institutional racism in healthcare organisations remains a contemporary issue that must be acknowledged and addressed to build a ‘strong foundation towards culturally and clinically safe nursing and midwifery practice’ (p. 3).
Education, but to what standard?
Not recognising the entrenched nature of racism in health organisations diminishes the perceived need for comprehensive and meaningful education on cultural safety. It could also be argued that the entrenched nature of racism in health organisations indicates that cultural safety training has not been effective. Cox and Best14 refer to an approach of ticking the boxes to demonstrate action on diversity and equity, with no understanding of ‘underpinning theories, models, and their application in practice’. This superficial approach to cultural safety may explain why education has proved ineffective and also serves to reinforce the status quo where individual and organisational racism remain unchallenged. The United Nations38 and WHO39 guide discourse globally on the historical and contemporary impacts of racism on the overall wellbeing of populations. WHO provides support to national and local jurisdictions and aims to raise awareness of evidence and participatory approaches to combat racial discrimination40. The UK41, Canada42, Australia43, the US44 and Norway45 have laws and professional standards that guide the practice of nurses (and other health professionals) that encompass the provision of culturally safe care. In Australia, Aged Care Quality Standard 1 requirement 3b asserts that aged care services and the care they provide to consumers must be culturally safe46. But at present there are no Australian national standards in the aged care sector for cultural safety education servicing the aged care sector. However, the Australian Commission for Quality and Safety in Healthcare has conducted a national survey on the features of effective cultural safety training, which may inform the development of future programs in health. Features of high-quality cultural safety training identified in the survey pertinent to this scoping review include ‘clearly naming racism and the impact on health outcomes, delivering training in partnership with First Peoples, identifying systematic improvements needed to foster an environment of cultural safety and asking participants to posit how they can implement their learnings in practice’47. Further, Fredericks48 contends that education must include exploring Whiteness or ‘white race privilege’ so that White healthcare practitioners are also included as raced peoples with relationships to racism. This approach views racism as a systemic problem affecting all of society, ‘one embedded in our history, institutions, policies, way of life and psyches’ (p. 12). Exposing White race privilege is imperative to individuals understanding and unlearning racist ways of thinking and acting48,49.
Care plans and cultural safety – what comes first?
There were numerous definitions of cultural safety used in the literature, arguably creating confusing nomenclature around cultural safety, which is a barrier to conceptual understanding and practical implementation in Australian health care14,50-52. Care plans were viewed as instrumental to understanding individual needs, including those related to culture25,28,32. Australian literature advises that service providers should ensure that ‘individual consumer interests, customs, beliefs and cultural backgrounds are valued and nurtured, and links are maintained with family and community’53. This reflects the perspectives of First Nations Australian consumers on what constitutes culturally safe aged care54.
A cultural support plan as an adjunct to care plan should include strategies for how a consumer’s expressed needs and preferences are met in a culturally safe way43. Despite legislation and quality standards in Australia, adherence to requirements to develop, utilise and revise patient care plans in a meaningful way are highly variable46. Further, there was a perception that care plans were used as mechanisms to obtain funding, rather than as a means of providing effective care to consumers.
Areas for further research
This scoping review highlights areas for further research. While there is widespread agreement in the literature regarding the presence of racism in the health professions and in organisations, the literature does not clearly illuminate what health professionals understand to be racist thinking or behaviour and how it is responded to in practice.
Likewise, there appears to be limited information on health professionals’ understanding of cultural safety and how to provide culturally safe care. Although there is evidence that health professionals recognise the importance of individualised care, they do not seem to link this with the concept of cultural safety.
Work has begun in Australia to develop a consensus through a national anti-racism framework55 and standards for cultural safety training in aged care; there is also opportunity to consider how these should be applied or adapted to residential and community aged care to best meet the needs of a diverse consumer base and workforce.
Limitations
An examination of the methodology and rigour of the included studies is not a focus of a scoping review. Therefore, this scoping review may include literature excluded in other types of reviews. This scoping review included a small number of studies undertaken in regional, rural and remote areas of Australia, the US, England, Canada and Norway. Results may lack generalisability to other countries and geographical contexts.
Conclusion
Health professionals in the aged care sector in regional, rural and remote areas do not readily use terms such as ‘racist’ and ‘racism’ to describe their own or colleagues’ behaviour. This may be explained by implicit bias or ineffective education. A lack of interpreters, equipment and appropriate cultural safety education is indicative of institutional and structural racism. There is a lack of clarity on how cultural safety is understood by health professionals; however, individual care plans that include cultural needs are viewed as instrumental in providing high-quality care to the consumer. Consumers also indicated a preference for end-of-life care on Country with their family and community. Effective communication based on values such as respect and trust are vital for building relationships between consumers, families, communities and individual health professionals and organisations. There is broad scope for further research into how health professionals understand racism and how it affects their work. Further research is also needed to ensure that cultural safety training is effective in a residential and community aged care workforce and a diverse consumer base that includes First Peoples and people from communities that are culturally and linguistically diverse.
Acknowledgements
Four authors acknowledge that they are non-First Nations Australians with Anglo-Celtic ancestry.
Funding
The authors declare that there is no financial support given towards this research. The first author is the recipient of a Sturt Scheme Scholarship through Charles Sturt University.
Conflicts of interest
The authors declare no conflicts of interest.

