Introduction
The need to maximize the productivity of agricultural lands to meet the demand for food has led to an increasing use of pesticides. In this large-scale use, agricultural workers have high levels of exposure that can trigger health problems as a result of a lack of knowledge of how pesticides can be lethal to health and the consequences of their use1; thus, agricultural workers are one of the groups most affected by suicide and mental health problems2,3.
It is essential to distinguish between some terms involving suicide: suicide ideation, suicide attempt, and suicide itself. Suicide ideation is a risk factor that can lead to suicide because it makes people think of ending their lives without necessarily implying a material fact4. A suicide attempt is an act of attempting to take one's life, but it does not necessarily imply intention to die by suicide. Exposure to agrochemicals is a factor that can lead to suicide in agricultural workers; however, there are different opinions on this topic4. Thus, more studies are necessary to confirm and understand this phenomenon5.
Several studies confirm that the use of pesticides is closely related to adverse effects on human mental health, such as anxiety and depression5-9. These mental disorders can potentially lead people to die by suicide, and has become a public health problem because it is responsible for approximately 250 000 deaths annually, most of which occur in developing countries10. Moreover, a previous review showed that rural workers are more likely than other professions to die by suicide11.
The existing literature on suicide and exposure to pesticides shows a crude reality. An evaluation of 409 suicide attempts of rural workers in China showed that working in agriculture produces mental disorders and depression, which can lead people to suicide12 In Australia, another study argued that the highest suicide rates are among agricultural workers regardless of gender13. On analyzing these previous studies, the need to understand the motivation of agricultural workers to die by suicide in rural areas arises.
Current literature on rural work and suicide focuses on the mental health of agricultural workers in certain countries1 and analyzes the consequences of pesticide exposure for mental illness, cancer, and teratogenicity14. These studies note a higher risk of suicide due to mental disorders produced by constant and acute exposure to pesticides; this reaffirms the need to understand the association between pesticide exposure and suicide in agricultural workers.
Therefore, this study aimed to conduct a systematic literature review to find the association between pesticide exposure and the incidence of suicide in agricultural workers. It is worth highlighting that this research focuses on suicide due to the exposure to pesticides and not the poisoning with pesticides as a means to attempt or carry out suicide.
Methods
The systematic literature review of this research followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol15. This protocol reviews the abstract, introduction, methods, and results in all selected papers in the research bases following a checklist of 27 items. After a previous verification, a documentary flow is described (Fig 1) to construct the final portfolio selected for the systematic literature review.
The databases used in this review were Scopus, Web of Science, and PubMed. Searches in these databases were conducted using the following strings of keywords.
- Rural worker OR Agricultural worker OR Farm worker OR Farmer
- Suicide OR Suicide intention OR Suicide attempt
- Agrochemicals OR Pesticides OR Pesticide exposure OR Agrochemical exposure
The searches in databases initially screened 307 documents (Fig1). However, after excluding duplicates and grey literature and filtering by type of document (articles or reviews) and language (English or Portuguese), 232 documents remain.
After reading the title, abstract, and keywords, we realized that some papers were not related to this study, eg articles where notably agricultural workers or the use of pesticides were not the object of study, resulting in 174 remaining.
Finally, a full read of the text of these articles was conducted, excluding the papers that were not closely related to the research theme. This resulted in 30 articles, and three were added because they were relevant to this study, resulting in a final portfolio of 33 articles.
From the final portfolio, the following data were extracted:
- sample size
- type of crop
- type of pesticide
- effects caused on rural workers’ health
- country of research
- variables studied.
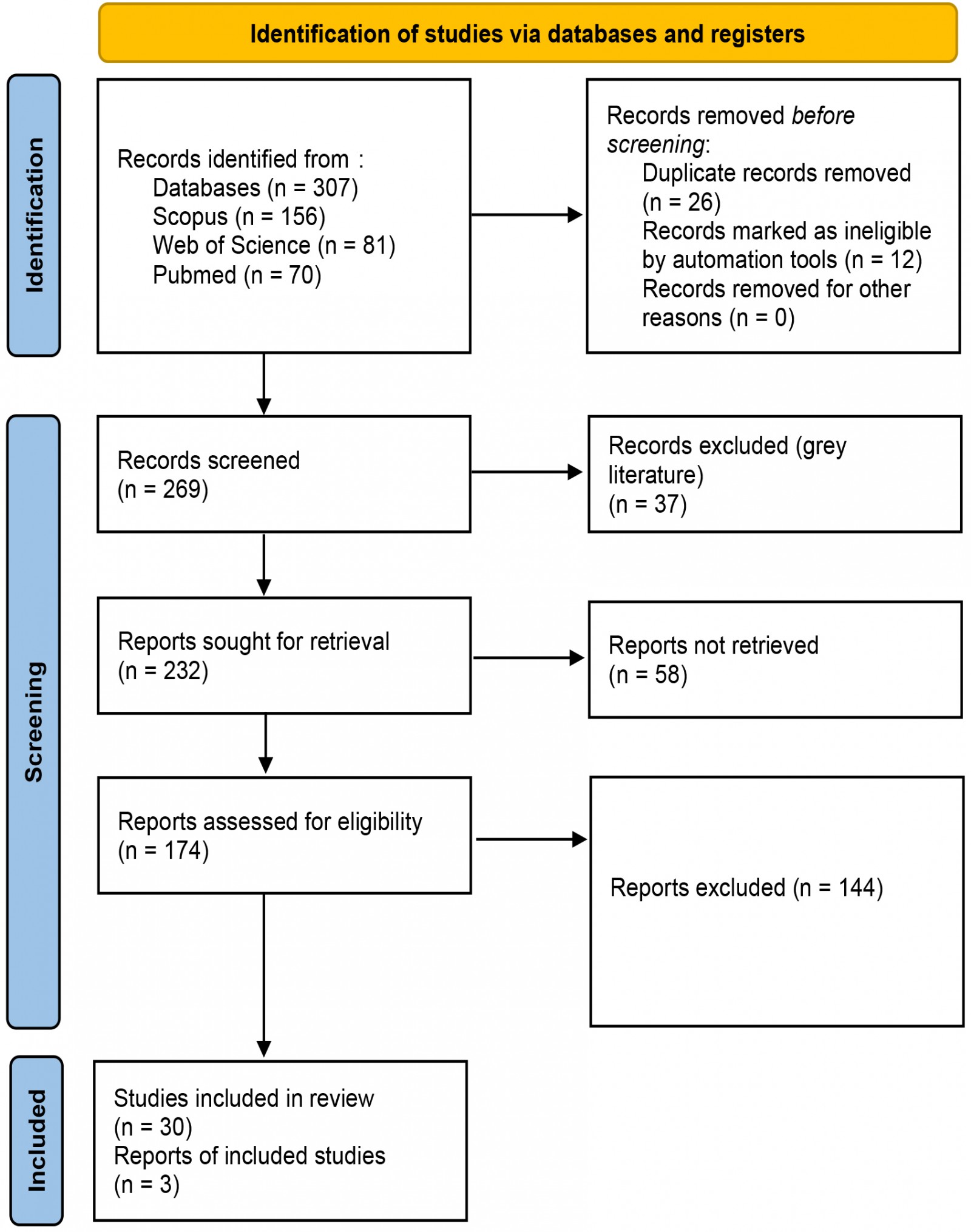 Figure 1: Steps for constructing the final portfolio.
Figure 1: Steps for constructing the final portfolio.
Ethics approval
No approval and/or consent was required, since this study is based on a review of the existing literature.
Results
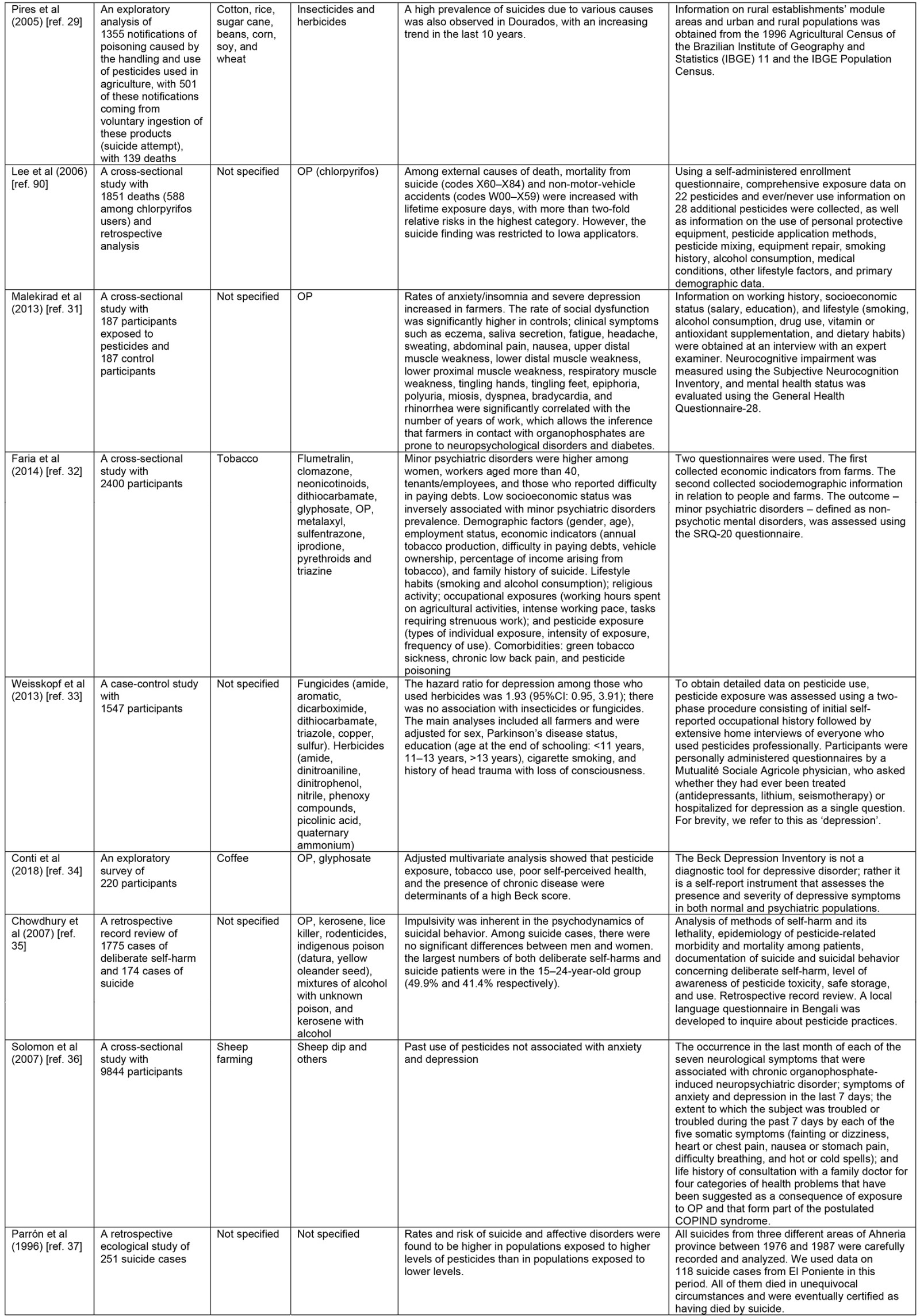
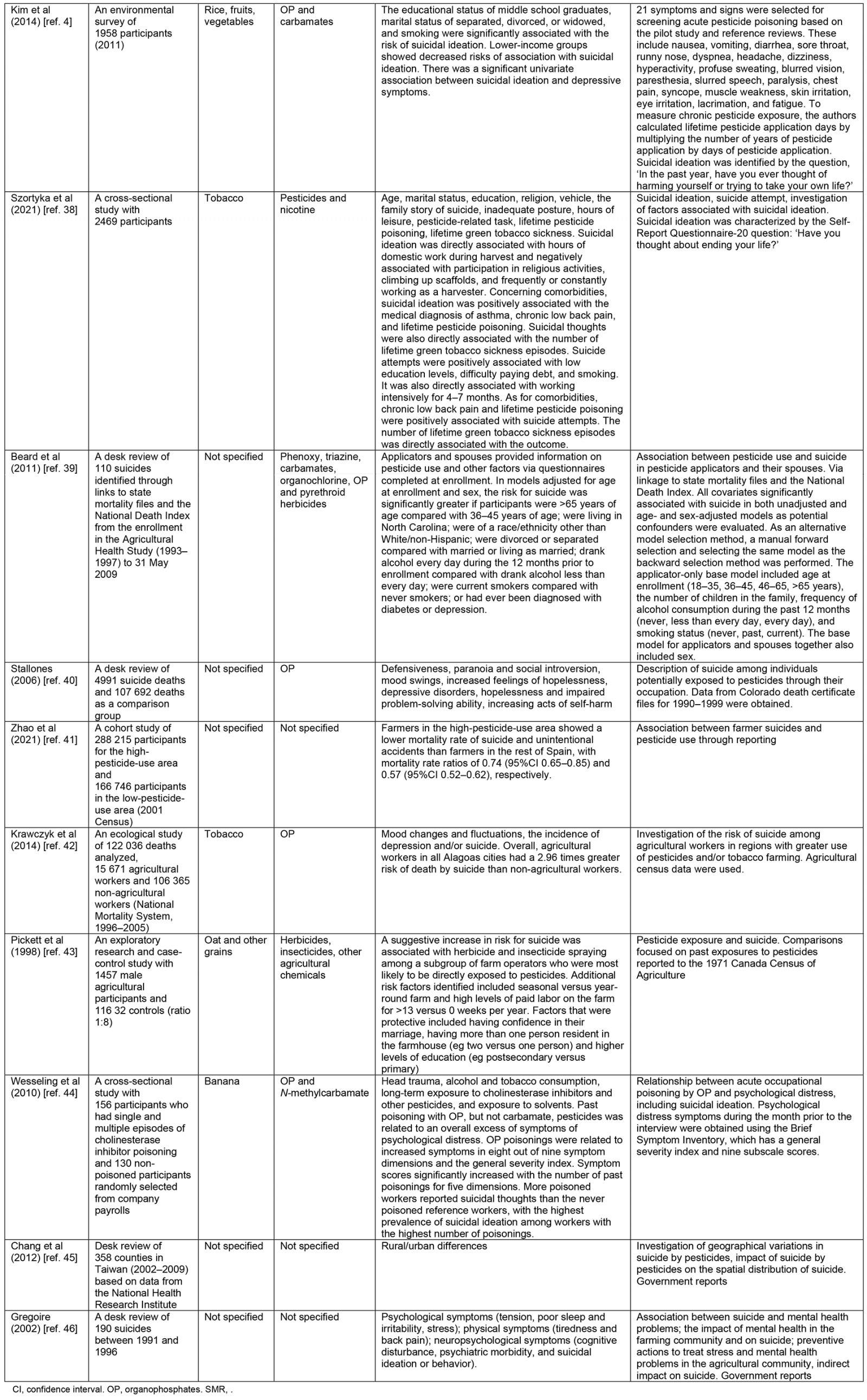
The 33 articles selected for the literature review were analyzed and are described in Table 14,8,16-46.
The country with the highest number of publications was Brazil with nine articles18,20,27-29,32,33,38,42, the US had five articles8,24,30,39,40, the UK had four articles16,19,36,46, Iran17,31 and Spain37,41 had two articles, and another 11 countries had one publication each.
The year with the highest number of publications is 2014, with four4,20,32,42, followed by 200730,35,36, 201023,24,44, and 201617,19,28 with three surveys in each year; then 200216,46, 200521,29, 201331,33, 201822,34 and 202138,41 with two publications in each year. The years 199637, 199843, 200026, 200318, 200640, 20088, 201139, 201245, 201725, and 202027 have one publication each year.
The data sources analyzed in the review surveys are mostly from reports and censuses (13 occurrences). However, the authors proposed their own questionnaires for the research in seven articles. Other tests included the neuropathy questionnaire in two studies; cholinesterase activity tests in two surveys; the Self-Report Questionnaire in four surveys27,28,32,38, being combined with the authors’ own questionnaire27,28 and with the Intoxication Protocol of the State of Paraná and Alcohol Use Disorders Identification Test27; quality of life, stress, depression, and anxiety scales in one survey; the Subjective Neurocognition Inventory combined with a blood glucose test in one study31; the Beck Depression Inventory34; Brief Symptom Inventor44; the Hospital Anxiety and Depression Scale19; the Barrat Impulsivity Scale combined with the Aggression Inventory in one survey22; and the General Health Questionnaire-28 in one survey31. The cholinesterase levels test was applied in four studies18,24,26,44.
The variables influencing suicide are smoking4,27,38,39, low level of education4,38, difficulty paying debts20,38, and frequent alcohol consumption27,39. Concerning the rural workers’ age, studies found a set of varied result. Based on the literature, some age groups are more vulnerable: children from both genders aged less than 15 years28, people aged more than 40 years, and women of any age group20, men and women aged between 15 and 24 years35 and people aged more than 65 years39. Moreover, the marital status of rural workers, predominantly separated, divorced, or widowed, is another factor influencing suicide4,39.
The chemical agents that are more present in the articles are the organophosphates, which were analyzed separately in 13 articles; organophosphates and carbamates appeared in four articles; and other types of pesticides were presented in 12 articles.
Regarding the effects of exposure, depression and anxiety are the most recurrent consequences in the publications (n=18); next is suicidal behavior, in four articles; mental disorders were present in three publications; nausea, tiredness, headache, and pain appeared in three publications; stomach diseases and asthma were present in two publications; the reduction of intellectual capacity in one publication; and three articles did not analyze the consequence of exposure.
Table 1: Analysis of the portfolio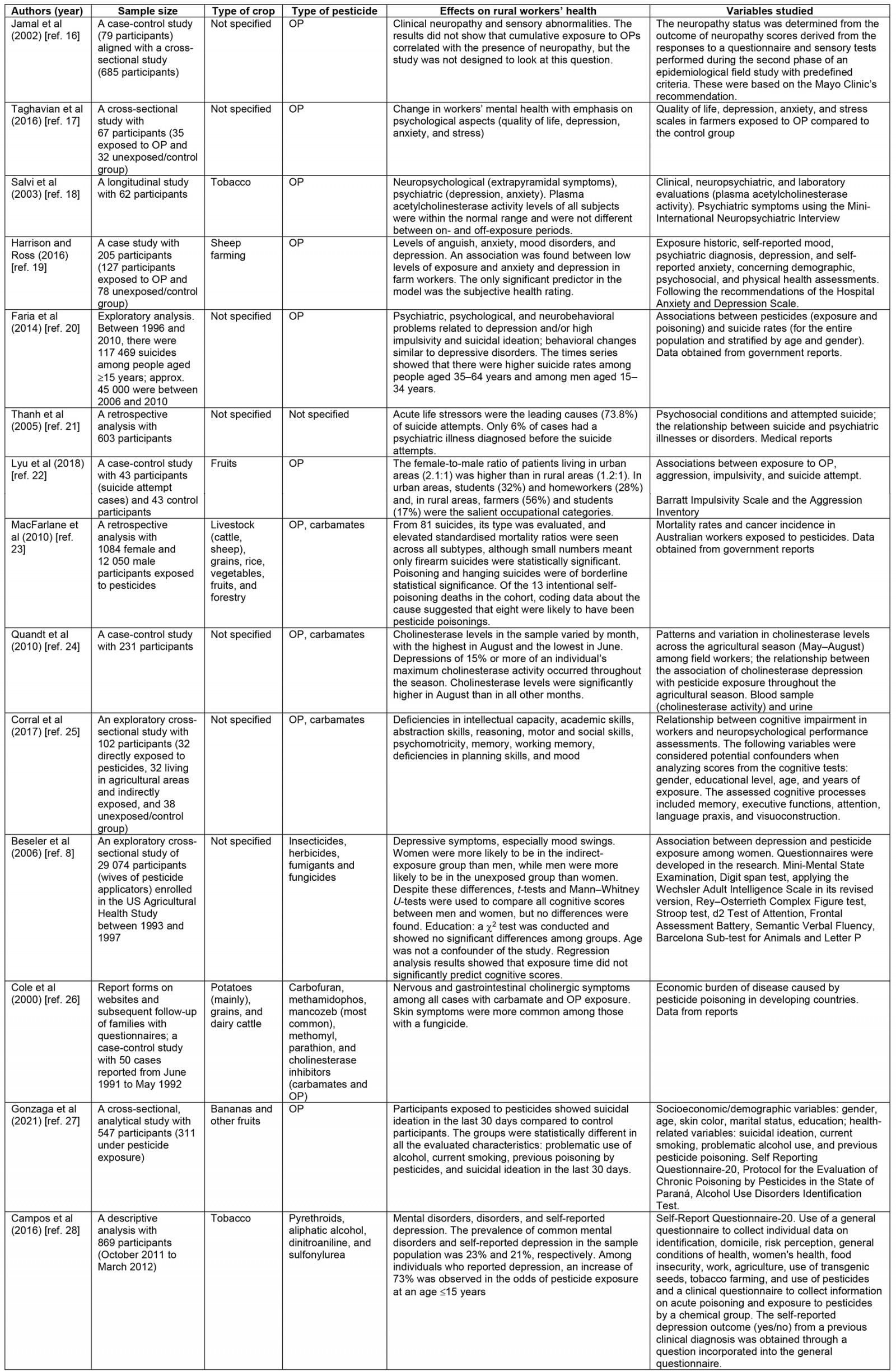
Discussion
The main results of the research show that constant and acute pesticide exposure leads to health disorders. In this sense, organophosphates are the most common type of pesticide in the studies; hence, one might notice a link between the use of organophosphates and suicide (itself, ideation, or attempt). Furthermore, since more than half of the studies did not specify the crop cultivated by agricultural workers, no relation between suicide and cultivated crops could be found.
There is a great variety of data collection instruments in the methods and variables studied; most applied questionnaires to agricultural workers. However, most studies neglected the use of clinical tests that are important for confirming a poisoning with pesticides; these tests may be applied in hematologic or hair tests47.
Moreover, many studies did not consider the most significant possible number of variables related to pesticide exposure and suicide, and only a few articles showed an association between intervening variables such as smoking, alcohol consumption, age group, length of exposure to agrochemicals. However, it was possible to identify some factors determining the profile of agricultural workers ideating, attempting, or dying by suicide.
Profile of agricultural worker and suicide issues
In general, agricultural workers have low educational levels because of the inherent manual labor and physical efforts they must conduct13. However, some factors increase the likelihood of suicide at every level (ideation, attempt, and carrying out). These factors include the consumption of hazardous drinks (alcohol) or smoking.
Gender is a variable that does not show a conclusive relationship; thus, we cannot affirm that gender (male or female) affects the tendency to carry out suicide due to exposure to pesticides. Nevertheless, a recent review11 argues that, in general, male agricultural workers have more risk of suicide than female agricultural workers, but this study cannot confirm this.
Furthermore, marital status is also a factor that influences suicide. In this sense, divorced, separated, or widowed agricultural workers are more vulnerable to suicide than single agricultural workers. Moreover, socioeconomic situation is also a variable that can lead rural workers to carry out suicide; the difficulty of paying debts is a common factor in taking the decision of ending one’s life.
This study found that moderate participation in religious activities is associated with suicide in only one article38. In India48, practitioners of Hinduism were part of the population that died by suicide the most, in addition to other variables, such as low literacy rates and high levels of agricultural employment.
Regarding the age of rural workers, we did not identify a typical age for suicide or attempts. WHO49 describes suicide as the fourth leading cause of death in young people aged between 15 and 29 years. In this sense, two studies conclude that similar ages are risk factors for suicide among rural workers, 15–24 years20 and 15–34 years35.
Analysis by geographic localization
Another factor that may influence suicide issues is the localization of agricultural workers. This section analyzes the geographic distribution of workers to recognize relationships between geographic localization and suicide among agricultural workers.
In this review, the countries with the highest number of publications are Brazil and the US. According to the Food and Agriculture Organization of the United Nations (FAO)50, the countries that consume the most pesticides in the world are the US, Brazil, and then China. Hence, the results of our review demonstrate a significant concern with the issue of suicide among rural workers in these countries, corroborating the FAO data.
Although the US has the second highest number of publications, an article did not find support for moderate use of pesticides and suicide39. This result may be linked to the dose of pesticide used since, in Spain, a study found high suicide rates when there were high doses of pesticide37. The same was found in Brazil, where an area with intensive use of pesticides had a higher number of poisonings and suicides29.
Current literature10 argues that most cases of suicide are in developing countries, especially Brazil, China, and India, countries with intensive use of pesticides and where access to them is easier than in developed countries; however, in this study, there is also a prevalence of studies in the US. It might be an indicator that more attention to suicide should be given, not only in less developed countries. In this sense, another review11 found Australia has an acute problem with suicide among rural workers; thus, it is crucial to understand that the suicide of agricultural workers due to occupational pesticide exposure is a global problem and not exclusively of developing or least-developed countries.
Occupational exposure to pesticides, mental disorders and suicide
In this review, occupational exposure to pesticides was found to be a factor for suicide at every level: ideation, attempt, and commitment. It is worth mentioning that self-poisoning with pesticides is the most used method of suicide among agricultural workers51; however, our purpose was not to study pesticide ingestion as a mechanism to carry out suicide but to study the relationship between occupational exposure to pesticides and suicide.
In this sense, the most common pesticides in our portfolio was organophosphates; thus, there is a potential link between them and suicide. In this regard, since the mid-1980s, organophosphates have been considered a significant risk to human health that can increase human morbidity and mortality52.
Organophosphates are one of the most used pesticides worldwide, and they are compounds that can be lethal to humans; they damage the enzyme acetylcholinesterase, which is crucial for controlling nerve signals in the human body52. Thus, there is a real relationship between the occupational acute exposure of agricultural workers to pesticides, especially organophosphates, and the degradation of the nervous system, making people suffer some mental disorders, such as anxiety, depression, and impulsivity53, which favor the ideation, attempt, and subsequent suicide among agricultural workers.
At the same time, exposure time may be another risk factor. The more time exposed to pesticides, the greater the poisoning and the risk of diseases aggravating the suicidal intention38. In the US, the results of a survey show that in times of high productivity, when pesticide use is increased, there are high levels of pesticide compounds in the blood of farm workers24, representing a risk for human health due to the degradation of enzymes to control nerves. The same occurred in Brazil, with the indiscriminate use of pesticides in times of high productivity, also increasing the risk of neurological diseases53.
For Peres and Moreira54, one of the implications of the expressive use of pesticides resides in the high rates of suicide attempts in Brazil. According to the researchers, the recurrent exposure of rural workers to these products causes nervous system disturbances. Work by Bombardi55 corroborates this finding, emphasizing that the cases of death resulting from intentional exposure to pesticides are related to the development of psychiatric disorders by their users, especially organophosphates, causing the development of neuropathology.
Another factor that may influence suicide among agricultural workers is the access to pesticides, not necessarily for the risk of self-poisoning, but for the risk of informal commerce that can promote the sale of pesticides of untrained people, that encourages an inadequate application and storage of these compounds.
In this regard, Zhang et al56 found that 63.9% of the 5088 farmers interviewed in their study stored pesticides in easily accessible places, and only 4.9% of respondents stated that they stored them properly in a predetermined place. Among those who stored pesticides properly, 89% of respondents confirmed the presence of organochlorines, especially methamidophos, an insecticide with high persistence in the environment and classified by WHO49 as extremely toxic; WHO remarks that the focus should be on more types of pesticides than organophosphates.
Finally, another factor is the limited access to mental health services in rural areas. In addition, rural workers may be afraid to use these services when available because of the stigma of having a mental disorder when asking for help57. In this sense, the barriers to access to health in rural areas, such as professional capacity, understanding of the health of the rural population, and the costs of access to health, must be eliminated58.
Conclusion
This article aimed to conduct a systematic literature review to find the association between pesticide exposure and the incidence of suicide in agricultural workers. Thus, the literature showed a strong link between occupational pesticide exposure and suicide at all levels: ideation, attempt, and commitment among agricultural workers.
The main findings suggest that there is an agricultural worker profile that is more likely to carry out suicide. The factors that influence it are smoking and consuming alcohol, as well as marital status (divorced, separated, or widowed) and financial stressors (difficulty in paying debts). Surprisingly, there is no age group or gender in which a more significant number of suicides among rural workers is concentrated.
Initially, it seemed that this problem is exclusive to developing countries, such as Brazil, India, or China, because of the intensive use of pesticides to increase agricultural productivity. However, the results suggest that it is a global problem since developed countries, such as the US, may have a significant occurrence of suicide among agricultural workers as a consequence of exposure to pesticides.
Organophosphates are the pesticides most used in the cases found in the literature. Organophosphates cause the degradation of acetylcholinesterase, a crucial enzyme for the nervous system, originating mental disorders and illnesses, eg anxiety, depression, or aggressivity that may result in suicide; thus, it is crucial to properly regulate the use and commerce of organophosphates, without neglecting other pesticides that can be equally or even more harmful to human health.
Regarding the methods used in the studies of the portfolio, there is a need for more studies on poisoning with a diversified use of data collection instruments. Despite its importance, the acetylcholinesterase test was used in a few studies and is responsible for quantifying pesticide exposure, and the use of this test has been increasing. Thus, applying this test is encouraged to quantify and confirm an objective relationship between pesticide exposure and suicide among agricultural workers due to the damage to their nervous systems.
Most suicides worldwide occur through self-poisoning (pesticide ingestion); our review showed that exposure to these pesticides produces mental problems, especially in countries with easier access to pesticides that promote informal commerce. Therefore, there is a need for norms to regulate the commerce of pesticides, restricting their access only to trained people and controlling their use and storage. Hence, it is noted that training and empowering agricultural workers in the proper use and storage of pesticides is necessary, as well as communicating about pesticide compounds and their consequences on mental health.
Furthermore, since it is a public health problem, suicide among agricultural workers must have the appropriate attention of governments and society, ensuring their access to mental health services, prompt diagnosis, and adequate treatment and support to avoid suicide among agricultural workers.
This review attempted to be as objective as possible; however, as with every research, it had some limitations because some articles that could be deemed relevant to this topic were not indexed in the databases used or were excluded in the filtering due to subjective reasons. Moreover, the information in some articles could be generalized due to synthesis purposes, and not reflect some details of studies that could contribute to this review.
Finally, we encourage the research community to continue researching suicide among agricultural workers due to pesticide exposure, but with a particular focus on the correlation of secondary variables (gender, age, habits, exposure, and others) and the application of medical laboratory tests to measure the level of poisoning due to pesticides and the degradation of mental health in agricultural workers.
Funding
This work was supported by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) [Finance Code 001], and the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq) [Sponsored by CNPq 309491/2023-1] and Fundação Araucária e Secretaria de Estado da Ciência, Tecnologia e Ensino do Paraná.
Conflicts of interest
The authors declare no conflicts of interest.
References
You might also be interested in:
2022 - Perceived risk and pandemic response awareness in low-capacity public primary health care in Greece
2004 - Consultant supported intermediate care - a model for remote and island hospitals

